Short report 1
Hemostatic dressings in civil prehospital practice: 30 uses
of QuikClot Combat Gauze
Stéphane Travers, Hugues Lefort, Eric Ramdani, Sabine Lemoine, Daniel Jost,
Michel Bignand and Jean-Pierre Tourtier
To report the use and describe the interest of hemostatic
dressings in a civilian setting, we provided medical
prehospital teams with QuikClot Combat Gauze (QCG) and
asked physicians to complete a specific questionnaire after
each use. Thirty uses were prospectively reported. The
wounds were mostly caused by cold steel (n = 15) and were
primarily cervicocephalic (n = 16), with 19/30 active arterial
bleedings. For 26/30 uses, hemostatic dressing was
justified by the inefficiency of other hemostasis techniques.
Those 30 applications were associated with 22 complete
cessations of bleeding, six decreases of bleeding, and
ineffectiveness in two cases. The application of QCG
permitted the removal of an effective tourniquet that was
applied initially for three patients. No side-effects were
reported. The provision of hemostatic dressings in civilian
Introduction
Prehospital medical rescuers can face difficulties with
controlling external bleeding by conventional means (e.g.
standard gauze field dressing, elastic bandages, direct
pressure, tourniquet), and uncontrolled external hemorrhaging remains a leading cause of preventable death in
trauma [1].
During the 2000s, several types of topical hemostatic agents
were developed to better deal with these situations. Among
these, QuikClot Combat Gauze (QCG) is a flexible, nonwoven (50-50 rayon/polyester) gauze impregnated with
kaolin, an aluminum silicate with a hemostatic effect caused
by the activation of the intrinsic clotting pathway [2].
These devices have been studied and used widely by
Western armies in Iraq and Afghanistan [2,3]. However,
their use has seldom been described in a civilian setting.
resuscitation ambulances was useful by providing an
additional tool to limit bleeding while rapidly transporting
the injured patient to a surgical facility. European Journal of
Emergency Medicine 00:000–000 Copyright © 2015
Wolters Kluwer Health, Inc. All rights reserved.
European Journal of Emergency Medicine 2015, 00:000–000
Keywords: emergency medical services, hemorrhage, hemostatic dressing,
wounds and injuries
Fire Brigade of Paris, Emergency Medical Department, Paris, France
Correspondence to Stéphane Travers, MD, Fire Brigade of Paris, Emergency
Medical Department, 1 place Jules Renard, 75017 Paris, France
Tel: + 33 622 246 434; fax: + 33 156 796 754;
e-mail: travers.stephane@gmail.com
Received 13 March 2015 Accepted 31 July 2015
using them only in cases of failure of the usual hemorrhagecontrol measures (e.g. direct pressure with standard gauze
field dressing, elastic bandages, tourniquet).
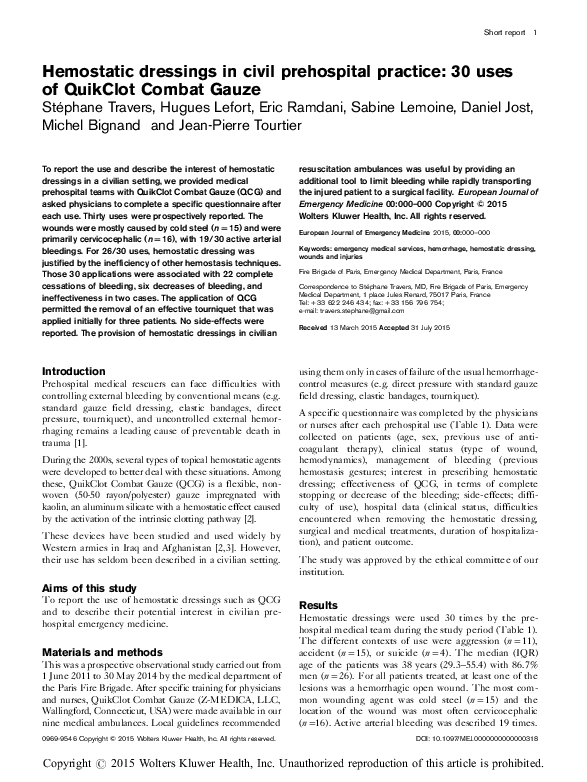
A specific questionnaire was completed by the physicians
or nurses after each prehospital use (Table 1). Data were
collected on patients (age, sex, previous use of anticoagulant therapy), clinical status (type of wound,
hemodynamics), management of bleeding (previous
hemostasis gestures; interest in prescribing hemostatic
dressing; effectiveness of QCG, in terms of complete
stopping or decrease of the bleeding; side-effects; difficulty of use), hospital data (clinical status, difficulties
encountered when removing the hemostatic dressing,
surgical and medical treatments, duration of hospitalization), and patient outcome.
The study was approved by the ethical committee of our
institution.
Aims of this study
To report the use of hemostatic dressings such as QCG
and to describe their potential interest in civilian prehospital emergency medicine.
Materials and methods
This was a prospective observational study carried out from
1 June 2011 to 30 May 2014 by the medical department of
the Paris Fire Brigade. After specific training for physicians
and nurses, QuikClot Combat Gauze (Z-MEDICA, LLC,
Wallingford, Connecticut, USA) were made available in our
nine medical ambulances. Local guidelines recommended
0969-9546 Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved.
Results
Hemostatic dressings were used 30 times by the prehospital medical team during the study period (Table 1).
The different contexts of use were aggression (n = 11),
accident (n = 15), or suicide (n = 4). The median (IQR)
age of the patients was 38 years (29.3–55.4) with 86.7%
men (n = 26). For all patients treated, at least one of the
lesions was a hemorrhagic open wound. The most common wounding agent was cold steel (n = 15) and the
location of the wound was most often cervicocephalic
(n =16). Active arterial bleeding was described 19 times.
DOI: 10.1097/MEJ.0000000000000318
Copyright r 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
�Uses of QCG by medical teams of the fire brigade of Paris from 06/01/2011 to 05/03/2014
N°
Age
Sex
Cause
Cause/
weapon
1
26
M
Suicide attempt
Razor
2
30
M
Suicide attempt
Subway
3
4
49
74
F
M
Suicide attempt
Accident
5
22
M
Wound
localization
Bleeding
Actions
before QCG
No
Arterial
Bandage
No
No
Venous
None
Head
Neck
No
No
Yes
No
Arterial
Arterial
Bandage
Bandage
Upper limb
No
Yes
Arterial
Anticoagulant
Shock
Upper limb
No
Lower limb
Fall
Car
Aggression
Knife
6
36
M
Aggression
Glass
Neck
No
Yes
Arterial
Pressure
point
Bandage
7
21
M
Aggression
Knife
Neck
No
No
Venous
Bandage
8
45
M
Aggression
Knife
Head
No
No
Unknown
Bandage
9
35
M
Accident
Knife
Perineum
No
No
Unknown
Bandage
10
27
M
Aggression
Fire arm
Lower limb
No
No
Arterial
11
34
M
Aggression
Knife
Neck
No
No
Arterial
Pressure
point
Bandage
12
50
M
Accident
Car
Perineum
No
Yes
Arterial
Bandage
13
72
M
Accident
Saw
Lower limb
VKA
No
Venous
Bandage
14
34
M
Aggression
Knife
Lower limb
No
No
Arterial
Tourniquet
15
16
17
46
76
24
M
F
M
Accident
Accident
Aggression
Car
Fall
Knife
Head
Head
Upper limb
No
ASA
No
No
No
No
Arterial
Arterial
Arterial
None
Bandage
Bandage
18
36
M
Aggression
Knife
Neck
No
No
Arterial
Bandage
19
32
F
Accident
Glass
Upper limb
No
No
Arterial
Bandage
20
75
F
Accident
Knife
Neck
No
Yes
Venous
None
21
22
23
27
41
50
M
M
M
Aggression
Accident
Accident
Knife
Fall
Saw
Head
Head
Upper limb
No
No
No
Yes
No
No
Arterial
Arterial
Venous
Bandage
Bandage
Tourniquet
24
25
M
Accident
Knife
Upper limb
No
Yes
Venous
Tourniquet
25
26
37
49
M
M
Accident
Suicide attempt
Glass
Knife
Aead
Abdomen
No
No
No
Yes
Arterial
unknown
Bandage
None
27
92
M
Accident
Knife
Head
No
Yes
Arterial
Bandage
28
29
82
78
M
M
Accident
Aggression
Fall
Knife
Head
Neck
VKA
No
No
Yes
Arterial
Unknown
Bandage
Bandage
30
39
M
Accident
Glass
Lower limb
No
No
Unknown
Bandage
Intererst of QCG
(according to the
physician of the
prehospital team)
Avoid tourniquet or
pressure point
Avoid tourniquet or
pressure point
Spare time (scalp)
Other actions were
ineffective
Other actions were
ineffective
Other actions were
ineffective
Other actions were
ineffective
Other actions were
ineffective
Other actions were
ineffective
Avoid tourniquet
Other actions were
ineffective
Other actions were
ineffective
Avoid tourniquet or
pressure point
Tourniquet removed after
QCG
Spare time (scalp)
Spare time (scalp)
Other actions were
ineffective
Other actions were
ineffective
Avoid tourniquet or
pressure point
Other actions were
ineffective
Spare time (scalp)
Spare time (scalp)
Tourniquet removed after
QCG
Tourniquet removed after
QCG
Spare time (scalp)
Other actions were
ineffective
Other actions were
ineffective
Spare time (scalp)
Other actions were
ineffective
Avoid tourniquet or
pressure point
Complete stop of the
bleeding after
introduction of QCG
Difficulties of
using QCG
Perfusion (ml)
Vasopressive drugs
Hospital
department
Transfusion
Surgery
Duration of
hospitalization
(days)
Outcome
Complete stop
No
< 500
No
ICU
No
Yes
1
Return home
Complete stop
No
700
No
ICU
No
Yes
78
Return home
Complete stop
Complete stop
Yes
No
1500
1900
Yes
Yes
ICU
ICU
Yes
Yes
Yes
Yes
7
1
Dead
Dead
Incomplete stop
No
2500
Yes
ICU
Yes
Yes
7
Return home
Complete stop
No
1500
No
ICU
No
Yes
3
Return home
Complete stop
No
0
No
Surgery
No
Yes
4
Return home
Incomplete stop
No
< 500
No
ED
No
Yes
2
Return home
Incomplete stop
Yes
< 500
No
ED
No
Yes
2
Return home
Complete stop
No
< 500
No
ICU
No
Yes
12
Return home
Complete stop
No
650
No
Surgery
No
Yes
1
Return home
Incomplete stop
No
2000
Yes
ICU
Yes
Yes
14
Complete stop
No
< 500
No
ICU
No
Yes
2
Dead
Return home
Complete stop
No
1000
No
ICU
No
Yes
3
Return home
Complete stop
Complete stop
Complete stop
No
No
No
< 500
< 500
< 500
No
No
No
ICU
ED
ICU
No
No
No
Yes
Yes
Yes
1
12
2
Return home
Return home
Return home
Incomplete stop
No
750
No
ICU
No
Yes
3
Return home
Complete stop
No
< 500
No
ICU
No
Yes
2
Return home
Complete stop
No
1000
Yes
ICU
No
No
1
Dead
Complete stop
Complete stop
Complete stop
Yes
No
No
1000
< 500
< 500
No
No
No
ICU
ED
Surgery
No
No
No
Yes
Yes
Yes
3
2
3
Return home
Return home
Return home
Complete stop
No
500
No
ED
No
Yes
3
Return home
Complete stop
No stop
No
No
< 500
4000
No
Yes
ED
Dead
No
No
Yes
No
1
0
Return home
Dead
Complete stop
No
1500
Yes
ICU
Yes
Yes
4
Return home
Incomplete stop
No stop
No
Yes
0
> 2500
No
Yes
ED
ICU
No
Yes
Yes
Yes
8
2
Return home
Dead
Complete stop
No
500
No
Surgery
No
Yes
2
Return home
ASA, acetysalicylic acid; ED, emergency department; F, female; M, male; QCG, QuikClot Combat Gauze; VKA, vitamin K antagonist.
2 European Journal of Emergency Medicine 2015, Vol 00 No 00
Copyright r 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Table 1
�Hemostatic dressings Travers et al. 3
The use of QCG was justified by the ineffectiveness of
other hemostasis techniques (e.g. direct pressure or
pressure with a standard gauze field dressing and elastic
bandages) in 26 of 30 cases and involved an inaccessible
area for pressure or tourniquet in 14 cases. In seven
patients, the hemostatic dressing was used for a scalp
wound during the initial phase of patient management.
QCG application was associated with the complete cessation of bleeding in 22 cases, the decrease of the
bleeding in six cases, and ineffectiveness in two cases. In
three patients, the use of a hemostatic dressing permitted
the removal of an effective tourniquet initially applied by
a witness while maintaining hemorrhage control.
No complications or side-effects were reported during
the prehospital phase or during hemostatic dressing
removal after arrival at the hospital. Difficulties in QCG
application have been reported by the operator in four
cases, including two cases in which the thin and narrow
nature of the wound made it difficult to introduce the
hemostatic dressing closer to the vascular breach, and two
cases where the operator had difficulty maintaining the
bandage during transportation.
Discussion
Hemostatic dressings have been shown to be more efficient than standard dressings in terms of reduction of
bleeding and survival in animal models with hemorrhagic
lesions with high and low pressure, probably because the
topical hemostatic agent (kaolin, in the case of QCG)
improves the creation of a thrombus in the vascular breach
when used in association with the compression [3,4].
Their utilization has been advocated by several authors,
including the PHTLS Executive Council, on the basis of
numerous animal studies [4–6], and hemostatic dressings
were used widely by several Western armies during
conflicts in Iraq, Afghanistan, and Gaza [3,6–8].
However, other authors point out the difficulties with
analyzing data accumulated during combat situations and
emphasize that the use of these devices has seldom been
described for civilian injuries [3,9].
This case series of 30 uses is, to our knowledge, the first
to describe the prehospital utilization of QCG in a civilian
context.
We chose QCG among numerous available hemostatic
dressings because this device is still recommended as the
first-line hemostatic agent by the Tactical Combat
Casualty Care Committee and was also selected by the
French Military Health Service. According to several
practitioners who had experience with its use in
Afghanistan, one of its interesting specificities is its roll
form, which enables the realization of a packing in
the wound.
Doctors and nurses who used QCG in our department
described complete cessations of bleeding after its
application in two-thirds of the cases, whereas other
measures to control a hemorrhage were ineffective or
impossible to use.
In several previous studies [4,7], the interest in hemostatic dressings was related to their effectiveness in open
wounds located in inaccessible areas for pressure or a
tourniquet, such as the groin or perineum, and their
effectiveness in certain situations where other techniques
have failed, including cervical injuries.
The physicians in our study reported the efficiency of
QCGs in the above-mentioned situations but also
described two more original uses that are likely to be
interesting.
(1) The possibility of stopping scalp bleeding, leaving
time for the physician to perform other urgent
procedures (e.g. rescue, perfusion, and intubation)
before achieving the final hemostasis suturing.
(2) The opportunity to remove a tourniquet after the
effective application of a hemostatic dressing. This
point confirms the results observed in swine with the
possibility to reduce tourniquet time through the use
of this type of dressing [10].
No side-effects have been described in our series, either
at the time of hemostatic dressing application in a prehospital setting or during removal in the hospital. This
result confirms the fact that QCGs in their current form
(rolled gauze impregnated with kaolin) produce no exothermic reaction and do not have any side-effects.
Conversely, injury by heating and the risk of granule
dispersion into the tissue were described with first generations of QuikClot devices that were composed of
zeolite granules [3].
It was not possible to introduce hemostatic dressing into
the wound in two cases and effectiveness in these cases
was affected. Indeed, for the dressing to be effective, it
must be in contact with the vascular breach and then
associated with manual compression for at least 3–5 min
[3]. This has not been completely possible for these two
patients as the wounds were deep and punctiform.
Finally, it may seem surprising that QCG has been used
only 30 times during the study period. This low usage is
related to the procedure of our department that planned,
during the study period, to use hemostatic dressing only
in case of failure or an inability to perform other
hemostasis gestures. The results of our study have since
led us to expand the use of these devices.
Limitations of the study
The self-evaluation of a hemostatic dressing’s efficiency
by the user has multiple biases [3]. The observation of
decreased bleeding remains subjective and is difficult to
quantify. The absence of a control group makes it
Copyright r 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
�4 European Journal of Emergency Medicine 2015, Vol 00 No 00
impossible to measure the efficiency of QCG, in terms of
immediate or late prognosis, and a comparison with other
devices such as standard gauze or elastic bandages.
However, carrying out a randomized clinical study to
assess the effectiveness of these dressings in the context
of human uncontrolled bleeding would be difficult and
has not been achieved by other teams. Despite these
limitations, certain benefits could be observed more
objectively, such as the removal of tourniquets after
hemostatic dressing application.
Conclusion
In civil practice, standard gauze field dressings, direct
pressure, and tourniquets appear occasionally inadequate
for the control of a hemorrhage. The provision of
hemostatic dressings in resuscitation ambulances helps
physicians and nurses to face these situations by providing them with an additional tool to limit bleeding
while rapidly transporting the injured individual to a
surgical facility.
The absence of major side-effects and the level of
interest noted among physicians who used QCGs for
3 years in our department confirmed our intention to
equip our Basic Life Support teams with hemostatic
dressings.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
1
Evans JA, van Wessem KJ, McDougall D, Lee KA, Lyons T, Balogh ZJ.
Epidemiology of traumatic deaths: comprehensive population-based
assessment. World J Surg 2010; 34:158–163.
2 Bennett BL, Littlejohn L. Review of new topical hemostatic dressings for
combat casualty care. Mil Med 2014; 179:497–514.
3 Rhee P, Brown C, Martin M, Salim A, Plurad D, Green D, et al. QuikClot use
in trauma for hemorrhage control: case series of 103 documented uses.
J Trauma 2008; 64:1093–1099.
4 Bulger EM, Snyder D, Schoelles K, Gotschall C, Dawson D, Lang E, et al. An
evidence-based prehospital guideline for external hemorrhage control:
American College of Surgeons Committee on Trauma. Prehosp Emerg Care
2014; 18:163–173.
5 Granville-Chapman J, Jacobs N, Midwinter MJ. Pre-hospital haemostatic
dressings: a systematic review. Injury 2011; 42:447–459.
6 Kheirabadi BS, Scherer MR, Estep JS, Dubick MA, Holcomb JB.
Determination of efficacy of new hemostatic dressings in a model of extremity
arterial hemorrhage in swine. J Trauma 2009; 67:450–459.
7 Ran Y, Hadad E, Daher S, Ganor O, Kohn J, Yegorov Y, et al. QuikClot
Combat Gauze use for hemorrhage control in military trauma: January 2009
Israel Defense Force experience in the Gaza Strip – a preliminary report of
14 cases. Prehosp Disaster Med 2010; 25:584–588.
8 Smith AH, Laird C, Porter K, Bloch M. Haemostatic dressings in
prehospital care. Emerg Med J 2013; 30:784–789.
9 Travers S, Dubourg O, Ribeiro Parenti L, Lefort H, Albarello S, Domanski L.
Prehospital use of haemostatic dressing QuikClot ACS + ™ for hemorrhage
control of a perineal trauma. Ann Fr Anesth Reanim 2012; 31:969–971.
10 MacIntyre AD, Quick JA, Barnes SL. Hemostatic dressings reduce tourniquet
time while maintaining hemorrhage control. Am Surg 2011; 77:162–165.
Copyright r 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
�
 Hugues Lefort
Hugues Lefort