symposium article
Annals of Oncology 19 (Supplement 7): vii289–vii293, 2008
doi:10.1093/annonc/mdn452
Management of weight loss and anorexia
J. B. Hopkinson, D. N. M. Wright & C. Foster
Macmillan Research Unit, University of Southampton, Southampton, UK
what is cancer cachexia syndrome?
There is no agreed definition of CCS (see Table 1 for examples
of defining characteristics [4, 5]). However, it is agreed that
cancer cachexia differs from starvation. It cannot be reversed by
food intake alone and causes loss of lean muscle mass in
addition to fat, whereas in starvation fat is lost in preference to
muscle.
the prevalence of cancer cachexia
syndrome
The prevalence of cancer cachexia differs across cancer site
and stage of disease. Symptoms can be present at diagnosis and
are most commonly seen in those with gastrointestinal and
lung malignancies [6]. More than three-quarters of people
with advanced cancer live with the symptoms [7,8]. Weight
loss and anorexia are important because they have been
associated with survival, treatment tolerance and quality of life
[1–3,9,10].
what causes cancer cachexia
syndrome?
secondary cachexia
Secondary cachexia is caused by factors that compromise
dietary intake leading to malnutrition; the obstacle course to
eating. The obstacles include nausea and vomiting; localized
pain, such as mouth ulcers; taste and smell abnormalities, such
as those induced by chemotherapy; diarrhoea or constipation;
fatigue; and mechanical obstruction, such as a tumour
occluding the oesophagus.
what can we do to manage cancer
cachexia syndrome?
Effective treatment of primary cachexia requires antineoplastic
therapy. Secondary cachexia is dependent on multiple physical,
psychological and social factors that may be amenable to both
pharmacological and non-pharmacological intervention.
management of primary cachexia
The solution to metabolic abnormalities is seen to lie in the
development of pharmacological agents that can prevent or
block the metabolic changes induced by cancer. Yavuzsen et al.
[13] conducted a systematic review of randomized controlled
trials from 1966 to autumn 2004 and found three groups of
pharmacological agent beneficial for people with the anorexia
and weight loss of cancer cachexia. The review found the
following.
(i)
The cause of cancer cachexia is multifaceted and not completely
understood. A useful model for understanding the pathways of
causation categorizes contributory factors into two groups:
primary and secondary cachexia [11,12].
The progestin, megestrol acetate, had been used in
23 studies involving 3436 patients. A dose of 480–800 mg/
day can bring about short-term weight gain that is
thought to be due to fat and fluid retention, as opposed
to lean muscle mass. Side effects include increased risk of
embolism, whilst improvements in quality of life are
uncertain.
ª The Author 2008. Published by Oxford University Press on behalf of the European Society for Medical Oncology.
All rights reserved. For permissions, please email: journals.permissions@oxfordjournals.org
Downloaded from annonc.oxfordjournals.org by guest on May 11, 2011
Involuntary weight loss and anorexia are symptoms of cancer
cachexia syndrome (CCS). The syndrome causes at least 20%
of deaths in people with cancer [1]. Furthermore, weight loss
and malnutrition are associated with poorer treatment
tolerance and outcomes [2], and poorer quality of life [3].
The challenge for clinicians is to know how best to manage
the symptoms of weight loss and anorexia for optimal patient
outcomes.
The aim of this article is to examine critically the
management of weight loss and anorexia in people with
CCS. It will draw on evidence collated from the Macmillan
Weight and Eating Studies, to justify a new approach that
complements current pharmacological and nutritional
management. Implications for clinical practice are discussed.
primary cachexia
Primary cachexia is brought about by tumour-induced
metabolic change. The cancer itself generates tumour products
that disturb normal tissue repair. Catabolism is accelerated,
whilst anabolism slows, leading to tissue loss. In addition, the
cancer triggers a systemic inflammatory response. This
inflammatory response includes an elevated metabolic rate and
release of biochemical products that suppress appetite and
cause early satiety. The consequence of metabolic abnormalities
is anorexia and loss of fat plus muscle mass.
symposium
article
introduction
�symposium article
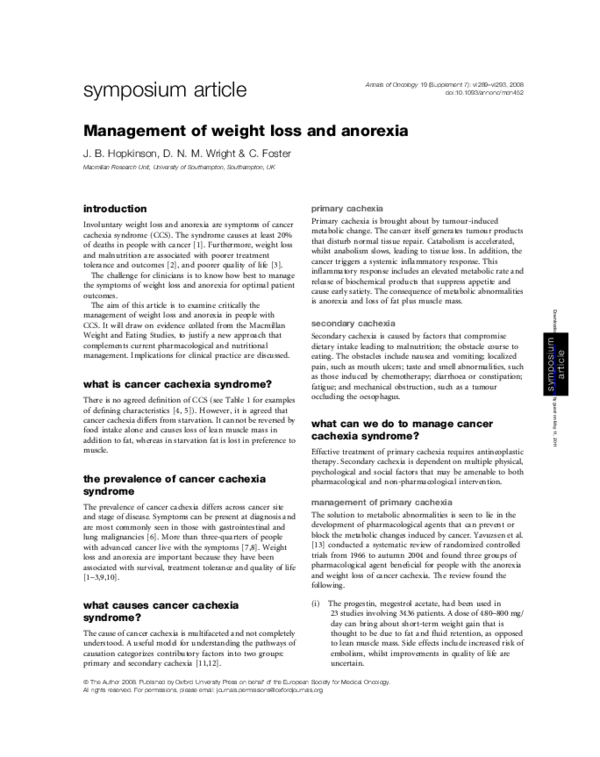
Table 1. Comparison of defining characteristics of cancer cachexia
syndrome adopted by two authors
Weight loss (>5%)
Anorexia
Muscle wasting
Aesthesia
Anaemia
Oedema
(Macdonald et al. 2003 [4])
Weight loss (>10% pre-illness)
Food intake (<1500 kcal/day)
Systemic inflammation (C-reactive
protein >10 mg/l)
(Fearon et al. 2006 [5])
(ii) Corticosteroids have been trialled in six studies involving
647 patients. They improve appetite and quality of life
over a limited time of a few weeks.
(iii) The prokinetic, metoclopramide, has been tested for
effect on weight and appetite in two studies involving
55 patients. The drug hastens stomach emptying, so can
help with early satiety, but does not improve appetite.
management of secondary cachexia
The solution to malnutrition induced by secondary cachexia is
seen to lie in improving nutritional intake. Skipworth and
Fearon [15] set out the scientific rationale for optimizing
nutritional intake in all people with cancer. Indeed, there is
evidence that nutritional intake can be enhanced, achieving
weight stabilization or weight gain in people receiving active
treatment for gastrointestinal and head and neck tumours.
Approaches that have been demonstrated to be effective are the
enrichment of foods [16]; enteral feeding [17]; and nutritional
counselling provided by a specialist dietician [16,18].
Nutritional supplements have been found to improve weight in
people with unresectable pancreatic cancer [19].
In the future, it is likely that there will be nutraceuticals
available to help people manage the anorexia and weight loss
that can accompany cancer. Neutraceuticals are nutritional
supplements to which a pharmacological agent has been added.
An example is ProSureÒ, which has been found to lead to weight
stability in a small group of seven people with pancreatic cancer
when taken in a quantity of three 240 ml cartons daily [20]. To
date there is no scientific evidence that special diets (e.g. nondairy) can contribute to controlling the progression of cancer.
an emerging approach: management of
psychosocial factors that lead to
suboptimal nutritional intake
Causes of and solutions for primary and secondary cachexia lie
with the individual who has cancer. Solutions are sought that
vii290 | Hopkinson et al.
change the biochemical processes within the body or change the
nutrients available for bodily function. This conceptualization
contributes to our understanding of cancer cachexia by
considering the person independently of the social context in
which they live. However, social context may contribute to the
development of weight loss and anorexia. There is growing
recognition that psychosocial intervention may be important to
the management of CCS [21–26].
what is the evidence that psychosocial factors lead
to suboptimal dietary intake?
The Macmillan Weight and Eating Studies, since 2000, have
sought to understand peoples’ experience of weight loss and
anorexia when they have advanced cancer [8,27,28] and to
develop interventions that help people live with the
symptoms [29]. This work supports the argument that social
context contributes to the problems of weight loss and
anorexia.
The studies include a mixed methods case study of people
under the care of two specialist community palliative care
teams working in the South of England. A method of
data collection was a brief questionnaire sent to 232 people
with advanced cancer. This sample represented 67% of the
total caseload of the two community palliative care teams
over a 2-week period. Patients were invited to self-report
weight loss, loss of appetite and concern about the
symptoms.
Of the 199 people (response rate 85%) who returned
a completed questionnaire, 79% reported weight loss, 76%
reported eating less as compared with before they knew they
were unwell, and 52% reported concern about one or both of
the symptoms [8]. To establish why people experienced
concern, a purposive sample of 30 patients was selected for
interview from those who completed the questionnaire. The
interview sample was of 14 men and 16 women, aged 43–85
years (median age 70), 16 of whom reported concern about
their weight or loss of appetite on the questionnaire.
The findings demonstrate that healthy eating messages and
conflict over food within families make a difference to what is
eaten by people with advanced cancer. These are examples of
socially constructed factors that influence dietary intake.
healthy eating messages make a difference to what
is eaten
For people who have lost weight and have a small appetite,
an energy- and protein-dense diet is appropriate [30].
Optimizing calorie and protein intake with a small appetite
usually requires a change in the type of foods eaten. Full-fat
products and calorie-dense foods can enable an adequate
nutritional intake. Thus, previously discouraged foods, such
as chocolate, cakes and puddings, become important foods to
prevent or limit malnutrition.
People taking part in the Macmillan Weight and Eating
Study were keen to take a healthy diet. They were exposed to
many messages about diet and food via the media, books, and
family and friends. They believed that a healthy diet, high in
fibre, fruit and vegetables, and low in fat, would contribute to
their health and well-being.
Volume 19 | Supplement 7 | September 2008
Downloaded from annonc.oxfordjournals.org by guest on May 11, 2011
Trials of other pharmacological agents are in progress. For
example, thalidomide is being trialled for its ability to arrest
systemic inflammation and in turn impact on appetite and
weight (see Cancer Research UK clinical trials database [14]).
Current debate around the management of cachexia also
includes the question of whether pharmacology could be used
prophylactically.
Annals of Oncology
�Annals of Oncology
‘‘I try not to eat fatty things so much now’’ (Doris)
When they were unable to eat healthy foods this could cause
guilt and self-blame.
‘‘I’m not eating vegetables. I’m not eating fruit. It scares me’’
(Stella)
Healthy eating messages informed what people with
advanced cancer thought that they should eat and led them to
persist with trying to eat foods they found unpleasant or
difficult to eat.
‘‘I force myself to eat (grilled lamb) because I know it has nutrients’’
(Paul)
Yet we all eat more of the things that we enjoy. Ideology
around healthy eating can lead to a less than optimum dietary
intake. There is potential for shifting ideas about what is an
appropriate diet for someone with cancer cachexia.
‘‘If I’m forced to eat, I don’t eat it’’ (Jimmy)
For some, although conflict had arisen, it had not persisted.
They had found a way of managing the situation, leading to
resolution of the disagreement. Steven had adopted a strategy
of education in order to resolve a disagreement between himself
and his mother who believed he should be eating a healthy diet.
‘‘You’ve got to make the people around you understand what your
limitations are . so that they can understand what you are going
through’’.
Interviewer: ‘‘How have you done that?’’
‘‘I had to sit down with (my mother) and explain’’ (Steven)
Since some patients found ways of resolving disagreements
for themselves, it seems likely that healthcare professionals
could support people in managing conflict. They could draw on
their own experience of families who have found effective ways
of managing conflict over food. Sharing this experiential
knowledge (without identifying the actors) could both
demonstrate that disagreements over food can be temporary
and present ideas that enable families to see new ways of
managing their problems.
revisiting what we can do to manage
cancer cachexia syndrome
The finding that psychosocial factors influence the dietary
intake of people living with advanced cancer is important. If
Volume 19 | Supplement 7 | September 2008
social context makes a difference to what people eat, then
there is the potential for psychosocial intervention to change
dietary intake, and hence play a role in the management of
CCS.
The exploratory study described above was of mainly
white British people with advanced cancer living in the
South of England. It is possible that the findings do not
translate to other geographical locations or to people with
potentially curable cancer. However, the participants’
accounts provided evidence of healthy eating messages and
conflict over food influencing their dietary intake prior to
learning that they had advanced disease. Furthermore,
psychosocial factors, including conflict over food, have
been recognized as contributing to problems for people
with cancer in other countries: Canada [31]; Sweden
[C. Tishelman, personal communication]; Ireland [32]; and
Switzerland [26].
tertiary cachexia?
The finding that psychosocial factors influence the
dietary intake of people with advanced cancer augments
the conceptualization of CCS. The syndrome might
usefully be understood as a constellation of problems
with primary (metabolic), secondary (physical obstacles to
eating) and tertiary (psychosocial) contributory causative
factors.
Tertiary cachexia has not previously been differentiated from
other causes. When it is conceptualized as distinct from
primary and secondary, new possibilities for the management
of CCS emerge: psychosocial interventions for the management
of weight loss and anorexia.
psychosocial interventions for cancer
cachexia syndrome
The Macmillan Weight and Eating Studies have established that
for people living with CCS there are no existing psychosocial
interventions that have been tested for effectiveness
(unpublished literature review—contact first author for
details). The studies are based on the assumption that the
management of eating-related problems may need to
differentiate between potentially curable and advanced cancers.
This perspective is informed by evidence that nutritional
counselling can arrest weight loss and improve quality of life
in people receiving treatment for potentially curable
gastrointestinal cancers [16,19]. Yet, in contrast, there is
currently no evidence that people with advanced cancer can
improve their survival or quality of life [8,21] by changing
what they eat. Therefore, the goal of psychosocial
intervention may need to change from optimizing nutritional
intake to mitigating weight- and eating-related distress when
the focus of treatment and care shifts from achieving cure to
optimizing quality of life. However, for many patients,
mitigation of distress is likely to be achieved by supporting
them in optimizing their nutritional intake within the
confines of their small appetite and other obstacles to
eating.
doi:10.1093/annonc/mdn452 | vii291
Downloaded from annonc.oxfordjournals.org by guest on May 11, 2011
conflict over food makes a difference to what is
eaten
Partners and family members are committed to helping
patients living with advanced cancer. However, they can
unintentionally contribute to the patient’s eating difficulties.
Whilst carers considered their role to include encouraging food
intake, this can be perceived by the patient as being nagged or
forced to eat. Contrary to carers’ intention, their approach to
the eating problem can become a barrier to food intake.
symposium article
�symposium article
implications for practice: management
of tertiary cachexia
intervention
The multidisciplinary team has an important role to play in
supporting people with CCS who have weight loss and
difficulty eating. Whilst dieticians are the professional group
with expertise in nutritional support, doctors and nurses have
contact with all patients, so are in a prime position to offer
first-line assessment and intervention or referral to specialist
dietetic services.
There is little evidence to guide intervention for the socially
constructed obstacles to eating well with CCS. However,
psychosocial interventions have been demonstrated to be
effective in bringing about dietary behavioural change in other
contexts, such as eating disorders [39] and heart disease [40,
41]. Work is currently in progress testing the effect of
a complex psychosocial intervention on outcomes for patients
with advanced cancer living with CCS [29].
Clinical assessment that reveals psychosocial obstacles to
eating, such as suboptimal food intake due to the influence
of healthy eating messages and conflict over food can, in part,
be addressed through the provision of information, such
as: (i) a healthy diet (i.e. low fat, high fibre, five portions of
fruit and vegetables daily) has no proven benefit for someone
with advanced cancer; (ii) people eat more of the things
they enjoy/find easiest to eat; (iii) people with a small
appetite typically find nutritious fluids and soft foods easiest;
(iv) cold foods, soft foods and fluids can be as nutritious as
cooked meals; (v) cancer causes metabolic change that
suppresses appetite, making it difficult to eat—difficulty
eating is not an indication of not trying to eat, emotional
weakness or giving up; and (vi) disagreements over food are
common in families managing CCS and it can be helpful for
each family member to explain to the others what is troubling
them.
vii292 | Hopkinson et al.
resources to support clinical practice
There is limited information available on eating well with CCS.
One source of information, based on evidence from the
Macmillan Weight and Eating Studies, is a set of eight
information leaflets to help patients with advanced cancer and
their carers live with weight loss and eating-related problems
(published by Macmillan Cancer Support, London, 2007 and
available from www.be.macmillan.org.uk/Order).
conclusions
Understandings of CCS have been informed by the biomedical
model of disease, leading to interventions that change the
balance of biochemicals and/or nutrients within the body with
the purpose of managing symptoms. This conceptualization
can be augmented by considering psychosocial factors that
contribute to the development of the syndrome. Psychosocial
support may improve outcomes for people living with cancer,
anorexia and weight loss.
disclosures
No significant relationships.
references
1. Tisdale MJ. Molecular pathways leading to cancer cachexia. Physiology 2005;
20: 340–348.
2. Andreyev HJN, Norma AR, Oates J, Cunningham D. Why do patients with weight
loss have a worse outcome when undergoing chemotherapy for gastrointestinal
malignancies? Eur J Cancer 1998; 34: 503–509.
3. O’Gorman P, McMillan DC, McArdle CS. Impact of weight loss, appetite, and the
inflammatory response on quality of life in gastrointestinal cancer patients. Nutr
Cancer 1998; 32: 76–80.
4. MacDonald N. Nutrition as an integral component of supportive care. Oncology
2003; 17: 8–10.
5. Fearon K, Voss AC, Hustead DS. Definition of cancer cachexia: effect of weight
loss, reduced food intake, and systemic inflammation on functional status and
prognosis. Am J Clin Nutr 2006; 83: 1345–1350.
6. DeWys WD, Begg C, Lavin PT et al. Prognostic effect of weight loss prior to
chemotherapy in cancer patients. Am J Med 1980; 69: 491–497.
7. Poole K, Froggatt K. Loss of weight and loss of appetite in advanced cancer:
a problem for the patient, the carer, or the health professional? Palliat Med
2002; 16: 499–506.
8. Hopkinson JB, MacDonald J, Wright DNM, Corner JL. The prevalence of concern
about weight loss and change in eating habits in people with advanced cancer.
J Pain Symptom Manag 2006; 32: 322–331.
9. Bosaeus I, Daneryd P, Lundholm K. Dietary intake, resting energy expenditure,
weight loss and survival in cancer patients. J Nutr 2002; 132: 3465S–3466S.
10. Hutton JL, Baracos VE, Wismer WV. Chemosensory dysfunction is a primary
factor in the evolution of declining nutritional status and quality of life in patients
with advanced cancer. J Pain Symptom Manag 2007; 33: 156–165.
11. Guenter P, Ferguson M, Thrush K, Coble Voss A. Understanding tumor-induced
weight loss. Medsurg Nurs 2002; 11: 215–227.
12. Strasser F, Bruera E. Update on anorexia and cachexia. Hematol Oncol Clin North
Am 2002; 16: 589–617.
13. Yavuzsen T, Davis MP, Walsh D et al. Systematic review of the treatment of
cancer-associated anorexia and weight loss. J Clin Oncol 2005; 23:
8500–8511.
14. Cancer Research UK. http://www.cancerhelp.org.uk/trials/trials/trial.asp?trialno=
7572. Accessed 13 Feb 2008. This e-mail address is being protected from spam
bots, you need JavaScript enabled to view it.
Volume 19 | Supplement 7 | September 2008
Downloaded from annonc.oxfordjournals.org by guest on May 11, 2011
clinical assessment
To date, responsibility for dietary management has rested
largely with patients and their families. People affected by
cancer have low expectations of help with weight loss and
anorexia from healthcare professionals [27]. However, there is
growing recognition that information might help people
optimize their nutritional intake from the point of diagnosis
[33–35]. In the UK, the National Institute for Health and
Clinical Excellence [36] has issued guidance recommending
that everyone receiving primary or secondary services has
a nutritional assessment.
Nutritional screening tools validated in cancer populations
assess nutritional status or risk of malnutrition. An example is
the Patient-Generated Subjective Global Assessment (PG-SGA)
[37,38]. Such screening tools enable the identification of
patients who have lost weight and are experiencing physical
problems that act as obstacles to eating loss. However, none of
these tools covers the range of psychosocial factors that can
contribute to the malnutrition component of CCS. To identify
these factors it is necessary to ask questions about the
experience of food intake.
Annals of Oncology
�Annals of Oncology
Volume 19 | Supplement 7 | September 2008
28. Hopkinson JB, Wright DNM, Corner JL. The experience of weight loss in people
with advanced cancer. J Adv Nurs 2006; 54: 304–312.
29. Hopkinson JB. A study of the effectiveness of the Macmillan Approach to Weight
loss and Eating difficulties (MAWE) in helping people live with advanced cancer.
2005 Unpublished study proposal.
30. British Dietetic Association. Nutritional Advisory Group for the Elderly (NAGE).
Have You Got a Small Appetite? Your Guide to Eating Well. Birmingham: NAGE
2002.
31. McClement SE. Cancer anorexia–cachexia syndrome: psychological effect on the
patient and family. J Wound, Ostomy Continence Nurses Soc 2005; 32: 264–268.
32. Reed J. Living with cancer cachexia: exploring the perspectives of patients and
their significant others. 4th Cachexia Conference, Tampa, USA, December 2007.
33. Langer CJ, Hoffman JP, Ottery FD. Clinical significance of weight loss in cancer
patients: rationale for the use of anabolic agents in the treatment of cancerrelated cachexia. Nutrition 2001; 17: S1–S20.
34. Ottery FD. Supportive nutrition to prevent cachexia and improve quality of life.
Semin Oncol 1995; 22 (2 Suppl 3): 98–111.
35. Whitman MM. The starving patient: supportive care for people with cancer. Clin J
Oncol Nurs 2000; 4(May–Jun): 121–125.
36. National Institute for Health and Clinical Excellence. Nutritional Support in Adults.
Clinical Guideline 32. London: NICE 2006.
37. Bauer J Capra S, Ferguson M. Use of the scored Patient-Generated Subjective
Global Assessment (PG-SGA) as a nutritional assessment tool in patients with
cancer. Eur J Clin Nutr 2002; 56: 779–785.
38. Thoresen L, Fjeldstad I, Krogstad K et al. Nutritional status of patients with
advanced cancer: the value of using the subjective global assessement of
nutritional status as a screening tool. Palliat Med 2002; 16: 33–42.
39. National Institute for Health and Clinical Excellence. Eating Disorders: Core
Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia
Nervosa and Related Eating Disorders. London: NICE 2004.
40. Clark NM, Dodge JA. Exploring self-efficacy as a predictor of disease
management. Health Educ Behav 1999; 26: 72–89.
41. Jacobssson A, Pihl-Lindgren E, Frilund B. Malnutrition in patients suffering from
chronic heart failure; the nurse’s care. Eur J Heart Fail 2001; 3: 449–456.
doi:10.1093/annonc/mdn452 | vii293
Downloaded from annonc.oxfordjournals.org by guest on May 11, 2011
15. Skipworth RJE, Fearon KCH. The scientific rationale for optimizing nutritional
support in cancer. Eur J Gastroenterol Hepatol 2007; 19: 371–377.
16. Ravasco P, Grillo IM, Vidal PM, Camilo M. Dietary counselling improves patient
outcomes: a prospective, randomized, controlled trial in colorectal cancer
patients undergoing radiotherapy. J Clin Oncol 2005; 23: 1431–1438.
17. Arends J, Bodoky G, Bozzetti F et al. ESPEN guidelines on enteral nutrition: nonsurgical oncology. Clin Nutr 2006; 25: 245–259.
18. Ravasco P, Grillo IM, Camilo M. Cancer wasting and quality of life react to early
individualised nutritional counselling!. Clin Nutr 2007; 26: 7–15.
19. Bauer J, Capra S, Battistutta D et al. Compliance with nutrition prescription
improves outcomes in patients with unresectable pancreatic cancer. Clin Nutr
2005; 24: 998–1004.
20. Barber MD, Fearon KCH, Tisdale MJ et al. Effect of a fish oil-enriched nutritional
supplement on metabolic mediators in patients with pancreatic cancer cachexia.
Nutr Cancer 2001; 40: 118–124.
21. Brown JK. A systematic review of the evidence on symptom management of
cancer related anorexia. Oncol Nurs Forum 2002; 29: 517–532.
22. Mantovani G. An update on the most recent clinical and experimental issues of
cancer-related anorexia/cachexia syndrome. Support Palliat Cancer Care 2006;
2: 87–93.
23. Levy MH, Back A, Bazargan S et al. The National Comprehensive Cancer
Network (NCCN) palliative care clinical practice guidelines in oncology. J Natl
Compr Cancer Network 2006; 4(8).
24. Shragge JE, Wismer WV, Olson KL, Baracos VE. The management of anorexia by
patients with advanced cancer: a critical review of the literature. Palliat Med
2006; 20: 623–629.
25. Uomo G, Gallucci F, Rabitti G. Anorexia–cachexia syndrome in pancreatic cancer:
recent development in research and management 2006; 7: 157–162.
26. Strasser F, Binswanger J, Cerny T, Kesserlring A. Fighting a losing battle: eating
related distress of men with advanced cancer and their female partners. A mixed
methods study. Palliat Med 2007; 21: 129–137.
27. Hopkinson JB, Corner JL. Helping patients with advanced cancer live with
concerns about eating: a challenge for palliative care professionals. J Pain Sympt
Manag 2006; 31: 293–305.
symposium article
�
 Jane Hopkinson
Jane Hopkinson