Ultrasound Assessment of Abnormal Fetal
Growth
David A. Nyberg, Alfred Abuhamad, and Yves Ville
A
ccurate pregnancy dating is the most important initial step in modern obstetric
management. Precise knowledge of gestational
age is essential for the management of pregnancies and in particular fetal growth abnormalities.
Unfortunately, dating by menstrual history is often unreliable. Up to 40% of women are not
certain of their dates and even when they are,
their wide distribution tends to over-estimate
gestational age (GA) when compared with ultrasound.1 Dating based on ultrasound is often
more predictive than even certain menstrual
dates, when ultrasound in performed in the first
half of the pregnancy.2-5
Overestimation of gestational age is common
when based on menstrual dates. This has the
effect of underestimating the rate of preterm
delivery6 and overestimating the number of postdate pregnancies. In a routinely scan-dated population, Gardosi et al7 found that 72% of inductions performed for post-term pregnancy (⬎ 294
days) according to menstrual dates were not
actually post-term according to ultrasound dating. Early ultrasound dating can therefore substantially reduce the number of pregnancies
considered postdates, and decrease the need for
term inductions.
Ultrasound Dating
First Trimester
In general, the earlier the ultrasound, the more
accurate the assessment of dates. This is logical
because all fetuses begin at the same size yet may
vary dramatically in size by term. Because of the
high degree of accuracy, dating by ultrasound in
the first half of pregnancy has become a routine
part of antenatal care in many institutions
around the world.
Before 6 weeks, dating can be done by measurement and observation of the gestational
sac.8 The gestational sac is visible as early as 4
weeks, and should always be visible by 5 weeks
(Fig 1). The size of the gestational sac can be
correlated with gestational age.9 Because the
mean sac diameter (MSD) grows at a rate of 1
mm per day, gestational age can be estimated by
the formula:
Gestational age (days) ⫽ 30 ⫹ MSD (mm).10
Among all measurements, maximum embryo’s length at 6 to 10 weeks (Fig 2) and crown
rump length (CRL) measurement up to 14
weeks are the most accurate at determining GA
(Table 1). The random error is in the range of 4
to 8 days SD (standard deviation) at the 95th
percentile.11-16 The largest study that uses a strict
methodology is that of Wisser et al.16 They highlight potential pitfalls of previous studies and
show a predictivity interval of 4.7 days SD on 160
in vitro fertilization (IVF) patients, including 21
multiple pregnancies.
Second and Third Trimesters
When the CRL is above 60 mm, other biometric
parameters are more useful for dating the pregnancy.17 Standardized measurements include
the biparietal diameter, head circumference, femur length, humerus length, and abdominal
circumference. These grow in a predictable way
and so can be correlated with GA (Table 2).
Virtually any other bone or organ can be measured and compared with GA. The head circumference is the most predictive parameter of gestational age between 14 and 22 weeks’ gestation
as it predicts GA by 3.4 days.5 Other parameters,
such as the biparietal diameter (BPD), abdominal circumference (AC), and femur length (FL)
also have good accuracy during the second trimester. Combining various biometric parameters improves the prediction of GA slightly over
the head circumference (HC) alone.18 In the
third trimester, the best single measurement of
Address reprint requests to David A. Nyberg, MD, 10401 E. McDowell Mtn Ranch Rd, #2-372, Scottsdale, AZ 85255.
© 2004 Elsevier Inc. All rights reserved.
0146-0005/04/2801-0002$30.00/0
doi:10.1053/j.semperi.2003.10.010
Seminars in Perinatology, Vol 28, No 1 (February), 2004: pp 3-22
3
�4
Abnormal Fetal Growth
Figure 1. Gestational sac at 5 weeks of gestation. A
yolk sac is faintly visualized.
GA based on standard biometry is the femur
length.
The BPD and HC reflect head size, which
in turn reflects brain growth. Although head
measurements primarily reflect the calcified calvarium, they are subject to variation based on
compression of the calvarium. BPD and HC can
be reliably measured from 13 weeks of gestation
when ossification of the parietal bones of the
skull has occurred. It should be noted that head
measurements are slightly larger in male fetuses
compared to female fetuses,19 and this difference can produce systematic errors in dating in
the range of 1.5 to 2.5 days.20,21
The occipito-frontal diameter (OFD) is measured in the same plane as the BPD with the
calipers placed on the outer skull table (Fig 3).
The HC can be either directly measured or can
be calculated from the BPD and OFD [HC ⫽
(BPD ⫹ OFD) ⫻ 1.57]. The direct method is less
than 2% bigger than the calculated measurement. Fetal head shape variations (dolichocephaly, brachycephaly) and fetal position can affect
head measurements, particularly the BPD in
which case the HC is preferable.
Femur length is the most commonly obtained
long bone measurement and is reproducibly
measured from 13 weeks onwards (Fig 4). Humerus length is also frequently obtained, especially during the second trimester. The femur
grows 3 mm per week from 14 to 27 weeks and 1
mm per week in the third trimester. Reported
accuracy for pregnancy dating ranges from 1
week in the second trimester to 3 to 4 weeks at
term.22Femur length after 18 to 19 weeks correlates with maternal height,23 and also correlates
with neonatal length. Long bone measurements
also vary with ethnicity with longer measurements in Black populations.24-26
The AC is a measure of fetal girth. It includes
soft tissues of the abdominal wall as well as a
measure of internal organs, primarily the liver.
Unlike other commonly used fetal measurements, it is not influenced by bone. The importance of AC is reflected by the fact that, at term,
95% of newborns are found to be within 20% of
expected length of 20 cm, whereas the weight
may vary by 100% or more. Therefore, differences in weight must be explained primarily by
variations in girth. Not surprisingly, then, the AC
is among the least predictive measures of fetal
age but the most predictive of fetal growth.27-29
The AC is measured on an axial plane at the
level of the stomach and the bifurcation of the
main portal vein into the right and left branches
taking care of having a section as round as possible, not deformed by the pressure of the probe
(Fig 5). The most accurate should approximate
a perpendicular plane to the spine at the level of
the hepatic vein. Ribs should show a symmetric
covering of the lateral contours. The AC shows
linear growth with a mean of 11 to 12 mm per
week throughout gestation. Mean AC and percentiles for abdominal circumference are shown
in Table 3.
Assessment of Fetal Size
Estimation of Fetal Weight
The best overall measure of fetal size is obtained
by estimating fetal weight. Numerous formulae
for estimating fetal weight have been described
and used (Table 4).30-34 With standard biometry,
some formulas use head measurements and AC,
others use long bone measurements and AC,
and others use all 4 measurements. The AC is
included in all commonly used formulas of estimated fetal weight, and AC also strongly influences fetal weight estimates.35 Weight estimates
based on AC alone have also been reported.36,37
Virtually any fetal bone or organ can be mea-
�Nyberg, Abuhamad, and Ville
5
Figure 2. Growth during the
first trimester. (A) Embryonic
length at 7 weeks of gestation. The crown rump length
is indicated. The yolk sac and
amnion are also visualized although discrete embryonic
landmarks are not seen. (B)
Scan at 12 weeks shows remarkable growth of the fetus.
Crown rump length measurement is indicated by red
arrow. Fetal detail is now
appreciated.
sured and be shown to grow in a predictable
pattern. In an attempt to improve the accuracy
of estimating fetal weight, it is tempting to add
many more measurements to standard biometry.
However, it is probably more worthwhile to ensure an accurate measurement of the AC rather
than adding other measurements of biometry.
Complicated formulas of fetal weight have not
been found to be more predictive than those
relying on standard biometry. Fetal weight estimates that are based on an artificial neural network model have also been proposed.38 Regard-
less of the method, estimation of fetal weight is
limited by the imprecision of fetal measurements, especially during the third trimester.
In experienced hands, nearly 80% of estimated
weights are within 10% of the actual birth weight
and most of the remaining are within 20% of
birth weight. However, sonographic accuracy decreases with less experienced sonographers.39
Also a number of studies have documented that
prediction of fetal weight by ultrasound may
be limited. For example, one study by Baum et
al39 found that sonographic estimation of fetal
�6
Abnormal Fetal Growth
Table 1. Predicted Menstrual Age From Crown
Rump Length (CRL) Measurements
Crown Rump Length (mm)
Menstrual Age (weeks)
0.2
0.3
0.4
0.4
0.5
0.6
0.7
0.8
0.9
1.0
1.0
1.1
1.2
1.3
1.4
1.5
1.6
1.7
1.8
1.9
2.0
2.1
2.2
2.3
2.4
2.5
2.6
2.8
2.9
3.0
3.1
3.2
3.4
3.5
3.7
3.8
4.0
4.1
4.2
4.4
4.6
4.8
5.0
5.2
5.4
5.5
5.6
5.7
5.8
5.9
6.0
6.1
6.2
6.3
6.4
6.5
6.6
5.7
5.9
6.0
6.1
6.3
6.4
6.6
6.7
6.9
7.0
7.1
7.3
7.4
7.6
7.7
7.9
8.0
8.1
8.3
8.4
8.6
8.7
8.9
9.0
9.1
9.3
9.4
9.6
9.7
9.9
10.0
10.1
10.3
10.4
10.6
10.7
10.9
11.0
11.1
11.3
11.4
11.6
11.7
11.9
12.0
12.1
12.2
12.3
12.3
12.4
12.5
12.6
12.6
12.7
12.8
12.8
12.9
Table 1. (Cont’d)
Crown Rump Length (mm)
Menstrual Age (weeks)
6.7
6.8
6.9
7.0
7.1
7.2
7.3
7.4
7.5
7.6
7.7
7.8
7.9
8.0
8.1
8.2
8.3
8.4
13.0
13.1
13.1
13.2
13.3
13.4
13.4
13.5
13.6
13.7
13.8
13.8
13.9
14.0
14.1
14.2
14.2
14.3
Data from Hadlock FP, Shah YP, Kanon DJ, et al: Fetal
crown-rump length: Reevaluation of relation to menstrual
age (5-18 weeks) with high-resolution real-time US. Radiology 182:501-505, 1992.
weight was no better than clinical or patient
estimates at term.
Weight formulas that include BPD, HC, AC,
and FL results in a mean absolute error of
around 10%.40,41 Some formulas for estimating
fetal weight are volume based and they would be
expected to be more accurate in predicting fetal
weight.31,32 However, these volume-based equations have not been shown to be more accurate
in other studies and result in large systematic
errors.42 Some formulae have been specifically
designed for premature babies43,44 However,
specific formulas for premature or very low birth
weight fetuses have not been found to be more
accurate in estimation of fetal weights than standard formulas by others.45
Three dimensional ultrasound has been used
to estimate fetal weight46,47 and theoretically this
method should result in improved estimation of
fetal weight compared to estimations based on
standard biometry (Fig 6). However, one limitation is that the most commonly used three-dimensional ultrasound systems have a limited
field of view that does not include the entire
fetus. As an alternative, 3-D ultrasound can evaluate specific fetal structures rather than the entire fetus. For example, Song et al48 measured
thigh volume with three-dimensional ultrasound
and reported that this method was more accu-
�Nyberg, Abuhamad, and Ville
7
Table 2. Predicted Fetal Measurements at Specific
Gestational Age in Centimeters
GA (Weeks)
BPD
HC
FL
AC
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
1.7
2.1
2.5
2.9
3.2
3.6
3.9
4.3
4.6
5.0
5.3
5.6
5.9
6.2
6.5
6.8
7.1
7.3
7.6
7.8
8.0
8.3
8.5
8.7
8.8
9.0
9.2
9.3
9.4
6.8
8.2
9.7
11.1
12.4
13.8
15.1
16.4
17.7
18.9
20.1
21.3
22.4
23.5
24.6
25.6
26.6
27.5
28.4
29.3
30.1
30.8
31.5
32.2
32.8
33.3
33.8
34.2
34.6
0.7
1.1
1.4
1.7
2.1
2.4
2.7
3.0
3.3
3.6
3.8
4.1
4.4
4.6
4.9
5.1
5.4
5.6
5.8
6.1
6.3
6.5
6.7
6.9
7.1
7.2
7.4
7.6
7.7
4.6
6.0
7.3
8.6
9.9
11.2
12.5
13.7
15.0
16.2
17.4
18.5
19.7
20.8
21.9
23.0
24.0
25.1
26.1
27.1
28.1
29.1
30.0
30.9
31.8
32.7
33.6
34.4
35.3
Abbreviations: BPD, biparietal diameter; HC, head circumference; FL, femur length; AC, abdominal circumference.
BPD ⫽ ⫺3.08 ⫹ 0.41*GA ⫺ 0.000061*GA2 (SD 3 mm)
HC ⫽ ⫺11.48 ⫹ 1.56*GA ⫺ 0.0002548* GA2 (SD 1 cm)
AC ⫽ ⫺13.3 ⫹ 1.61*GA ⫺ 0.00998*G GA2 (SD 1.34 cm)
FL ⫽ ⫺3.91 ⫹ 0.427*GA ⫺ 0.0034* GA2 (SD 3 mm)
Data from Hadlock FP, Deter RL, Harrist RB, et al: Estimating fetal age: Computer assisted analysis of multiple fetal
growth parameters. Radiology 152:497-501, 1984.
Figure 3. Transverse view of the fetal head obtained
at the level of the thalami at 22 weeks of gestation.
Note the BPD diameter and OFD.
day. Fetal length continues in a predictable way,
growing approximately one half centimeter per
week throughout pregnancy. By the end of the
first half of pregnancy, the fetus is about half its
eventual length, but only about one seventh of
its ultimate weight. The fetus adds much of its
weight during the third trimester. When growth
is expressed as a change proportional to current
weight, a constant deceleration is observed after
14 weeks.50
Estimated Fetal Weight Percentiles
An appropriate method of assessing fetal growth
is to determine the estimated weight percentile.
rate than two-dimensional ultrasound for predicting fetal weight during the third trimester of
pregnancy. Similarly, Schild et al47 combined
three-dimensional volume estimates of the thigh,
upper arm, and abdomen and found it to be
superior to two-dimensional biometry for estimating fetal weights. Also, Lee et al49 describe a
model for estimation of fetal weight based on
fractional thigh volume and AC.
Assessment of Fetal Growth
The gestational period is characterized by extraordinary fetal growth. During the first trimester, the embryo grows approximately 1 mm per
Figure 4. Longitudinal view of the femur obtained at
18 weeks of gestation. Note that femural measurement is obtained as the distance from the outer edges
of each metaphysic.
�8
Abnormal Fetal Growth
Figure 5. Transverse view of the fetal abdomen obtained at 28 weeks of gestation at the level of the
abdominal circumference. Note the stomach (S),
spone (sp), and intraabdominal portion of the umbilical vein (UV).
GA.54 More accurate neonatal charts have been
derived from neonates with accurate ultrasound
dating (Fig 7).55,56
A number of individual variables affect fetal
growth including maternal height, maternal
and paternal weight, parity, ethnicity, maternal
smoking, as well as the gender of the fetus.57,58
Paternal height also plays a minor role.59 Among
other variables, smaller fetal size tends to reflect
both maternal and paternal birth weights. Magnus et al58 found the mean maternal birth
weight was significantly less among those who
had experienced 2 small for GA (SGA) births
compared to those with no SGA births (3,127 ⫾
54 g v 3,424 ⫾ 22 g). Interestingly, the mean
paternal birth weight was also lower (3,497 ⫾
88 g v 3,665 ⫾ 24 g) from affected pregnancies
with 2 previous SGA births.
Table 3. Reference Values for Abdominal
Circumference (cm)
Abdominal Circumference (cm)
This requires comparison of estimated fetal
weight with expected weight for age. A commonly used weight percentile chart is presented
in Table 5 and Figure 7. Once the fetal weight
has been estimated and compared with expected
weight for age, it is a simple matter to determine
the estimated weight percentile. Normal values
are generally accepted as between the 10th and
90th percentiles, although these cutoffs are arbitrary and the 5th and 95th percentiles are
more predictive.
Expected weight standards have been generated either by weighing babies at birth, or by
using sonographic estimates of fetal weight.17
Variable results have been published.51 Some of
these differences may reflect the wide heterogeneity in ethnic composition, physical characteristics and socioeconomic status of the populations studied. Limitations of such standards
should be recognized and have been reviewed by
Altmann and Chitty.52
Weight charts based on clinical dates showed
a false flattening of birth weight curves at term
secondary to overestimation of GA based on
the menstrual history.53 In contrast, ultrasoundderived growth charts do not show a flattening
near term (Fig 7). One problem with birth
weight charts based on birth weights is that premature births or stillbirths tend to be small for
Percentiles
Menstrual Age (weeks) 3rd
14.0
15.0
16.0
17.0
18.0
19.0
20.0
21.0
22.0
23.0
24.0
25.0
26.0
27.0
28.0
29.0
30.0
31.0
32.0
33.0
34.0
35.0
36.0
37.0
38.0
39.0
40.0
6.4
7.5
8.6
9.7
10.9
11.9
13.1
14.1
15.1
16.1
17.1
18.1
19.1
20.0
20.9
21.8
22.7
23.6
24.5
25.3
26.1
26.9
27.7
28.5
29.2
29.9
30.7
10th
50th
90th
97th
6.7
7.9
9.1
10.3
11.5
12.6
13.8
14.9
16.0
17.0
18.1
19.1
20.1
21.1
22.0
23.0
23.9
24.9
25.8
26.7
27.5
28.3
29.2
30.0
30.8
31.6
32.4
7.3
8.6
9.9
11.2
12.5
13.7
15.0
16.2
17.4
18.5
19.7
20.8
21.9
23.0
24.0
25.1
26.1
27.1
28.1
29.1
30.0
30.9
31.8
32.7
33.6
34.4
35.3
7.9
9.3
10.7
12.1
13.5
14.8
16.3
17.6
18.8
20.0
21.3
22.5
23.7
24.9
26.0
27.2
28.3
29.4
30.4
31.5
32.5
33.5
34.4
35.4
36.4
37.3
38.2
8.3
9.7
11.2
12.7
14.1
15.5
17.0
18.3
19.7
20.9
22.3
23.5
24.8
26.0
27.1
28.4
29.5
30.6
31.8
32.9
33.9
34.9
35.9
37.0
38.0
38.9
39.9
From Callen et al. Data from Hadlock FP, Deter RL, Harrist
RB, Park SK. Estimating fetal age: Computer-assisted analysis
of multiple fetal growth parameters. Radiology 152:497-501,
1984.
�Nyberg, Abuhamad, and Ville
9
Table 4. Various Formulas used to Estimate Fetal Weight (in grams unless specified)
Warsof 1977
BPD, AC
Shepard 1982
BPD, AC
Roberts 1985
BPD, HC, AC, FL
Combs
HC, AC, FL
Hadlock 1984
FL, AC
Hadlock 1984
BPD, HC, FL, AC
Hadlock 1985
BPD, HC, FL, AC
Hadlock 1985
FL, AC
Log10 (Wt in kg) ⫽ ⫺1.599 ⫹ (0.144 ⫻ BPD) ⫹ (0 ⫻ AC) ⫺ (0.000111 ⫻ AC ⫻ BPD2)
Log10 (Wt in kg) ⫽ ⫺1.7492 ⫹ (0.166 ⫻ BPD) ⫹ (0.046 ⫻ AC) ⫺ (0.002646 ⫻ AC ⫻
BPD)
Log10 (Wt) ⫽ 1.6758 ⫹ (0.01707 ⫻ AC) ⫹ (0.042478 ⫻ BPD) ⫹ (0.05216 ⫻ FL) ⫹
(0.01604 ⫻ HC)
Wt ⫽ 0.23718 ⫻ AC2 ⫻ FL ⫹ (0.03312 ⫻ HC3)
Log10 (Wt) ⫽ 1.3598 ⫹ (0.051 * AC) ⫹ (0.1844 * F (.0037 *AC *FL))
Log10 (Wt) ⫽ 1.5115 ⫹ (0.0436 * AC) ⫹ (0.1517 FL) ⫺ (0.00321 * FL * AC) ⫹
(0.0006923 * BP HC)
Log (Wt) ⫽ 1.3596 ⫺ 0.00386*FL*AC ⫹ 0.0064 *HC ⫹ 0.00061*BPD*AC ⫹ 0.0424 *AC
⫹ 0.174 *FL
Log10 (Wt) ⫽ 1.304 ⫹ .05281*AC ⫹ 0.1938*FL ⫺ 0.004 *AC*FL
Abbreviations: Wt, weight; BPD, biparietal diameter; HC, head circumference; FL, femur length; AC, abdominal circumference.
Shepard MJ, Richards VA, Berkowitz RL, et al. An evaluation of two equations for predicting fetal weight by ultrasound Am J
Obstet Gynecol 1982;142:47.
Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK. Estimation of fetal weight with the use of head, body and femur
measurements: a prospective study. Am J Obstet Gynecol 1985;152:333-7.
Hadlock FP, Harrist RB, Carpenter RJ, et al. Sonographic estimation of fetal weight. Radiology 1984;150:535-40.
Roberts AB, Lee AJ, James AG. Ultrasonic estimation of fetal weight: a new predictive model incorporating femur length for
the low-birth-weight fetus. J Clin Ultrasound 1986;13:555-559.
Warsof SL, Gohari P, Berkowitz RL, et al. The estimation of fetal weight by computer-assisted analysis. Am J Obstet Gynecol
1977;128:881.
Compared with population-based birth weight
charts, some authors have found that individual
birth weight standards better correlate with fetal
outcome.60 For example, Clausson et al61 found
that individual growth standards better detected
fetuses at risk of stillbirth, neonatal death, and
low Apgar scores. Sciscione et al62 also conclude
that adjusting birth weight standards for maternal and infant characteristics may improve prediction of adverse outcomes. An example of individualized growth standards may be found on
the internet.63
Multiple gestations have similar growth curves
to singletons until the third trimester. Ong et
al64 found that the growth pattern of the AC for
twins is nearly identical to singletons until 32
weeks and then begins to gradually fall from
singleton curves, whereas the femur length was
more similar to singletons.
Serial Ultrasound
In clinical practice when abnormal growth is
suspected, serial ultrasound examinations are
more helpful than a single point on the growth
curve. Different methods of quantifying and ex-
Figure 6. Three-dimensional ultrasound. This could
give an accurate volume estimate to determine fetal
weight. However, it is difficult to capture the entire
fetus in a limited field of view available for most
three-dimensional ultrasound systems.
�10
Abnormal Fetal Growth
Table 5. Fetal Weight Percentiles, in grams, by
Gestational Age (GA)
GA (Weeks)
3rd
10th
50th
90th
97th
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
26
34
43
54
69
87
109
135
166
204
247
298
357
424
500
586
681
787
903
1029
1163
1306
1457
1613
1773
1936
2098
2259
2414
2563
2700
2825
2935
29
37
48
61
77
97
121
150
185
227
275
331
397
472
556
652
758
876
1005
1145
1294
1454
1621
1795
1973
2154
2335
2514
2687
2852
3004
3144
3266
35
45
58
73
93
117
146
181
223
273
331
399
478
568
670
785
913
1055
1210
1379
1559
1751
1953
2162
2377
2595
2813
3028
3236
3435
3619
3787
3934
41
53
68
85
109
137
171
212
261
319
387
467
559
664
784
918
1068
1234
1415
1613
1824
2048
2285
2529
2781
3036
3291
3542
3785
4018
4234
4430
4602
44
56
73
92
117
147
183
227
280
342
415
500
599
712
840
984
1145
1323
1517
1729
1955
2196
2449
2711
2981
3254
3528
3797
4058
4307
4538
4749
4933
NOTE. Ln (wt) ⫽ 0.578 ⫹ 0.332 MA ⫺ 0.00354 * MA2)
SD ⫽ 12.7% of predicted weight.
Data from ref 55.
evaluated include cheek-to-cheek diameter, soft
tissue thickness of the thigh or arm, and measurement of subcutaneous fat. Fetal abdominal
subcutaneous fat measurement correlates with
other measurements of fetal nutrition. For example, Donoghue et al67 found that fetuses with
an abdominal subcutaneous fat measurement of
5 mm or less were more likely to have an AFI
(amniotic fluid index) ⬍ 8 cm, an AC ⬍ 10th
percentile, and show lower postnatal parameters
of growth including a lower mean ponderal index and a decreased skinfold thickness at birth.
Matsumoto et al68 developed a “fetal nutrition
score” by qualitative assessment of the amount of
subcutaneous tissue present at 3 locations (face,
ribs, and buttocks) on prenatal three-dimensional ultrasound. The fetal nutrition score
strongly correlated with birth weight and neonatal nutritional score, and also correlated with
Apgar score, but not with umbilical cord arterial
blood pH.
Abnormal Growth
Deviations of normal fetal growth can be seen by
at least 20 weeks of gestation69 and probably as
early as the first trimester in some cases (see
Smith, this issue). Abnormal growth may represent subnormal growth (growth restriction), or
abnormally accelerated growth. Of the two,
growth restriction is more strongly related to
fetal abnormalities and adverse outcome.
pressing serial changes in fetal size have been
described, including the use of conditional percentiles.65,66 Standards based on serial measurements would seem a more appropriate technique for quantifying fetal growth as they
account for fetal size earlier in gestation, which
is an important determinant of subsequent fetal
growth and correct for the mathematical phenomenon of “regression towards the mean.”66
Use of first trimester ultrasound as a baseline has
also permitted more accurate growth curves.55,56
Other Measures of Fetal Growth
Other measures of fetal growth may not attempt
to estimate fetal weight or size, but rather look at
more specific areas. Soft tissues that have been
Figure 7. Fetal weight percentiles. Expected weight
(middle line) and weight percentiles. (Data from ref
55).
�Nyberg, Abuhamad, and Ville
Identification of fetuses with growth disturbances depends to a large extent on sonographic assessment. Growth disturbances may
also be suspected based on clinical findings of
decreased fundal height measurement and poor
maternal weight gain, in addition to identification of maternal risk factors, such as diabetes or
hypertension. Various metabolic analytes in the
maternal serum have been associated with normal and abnormal fetal growth. Of these, the
association between fetal leptin concentrations
and fetal weight appear the strongest.70 However, to date, evaluation of maternal analytes has
not been incorporated into clinical practice.
Intrauterine Growth Restriction
Identification of affected fetuses with intrauterine growth restriction (IUGR) is important because of a higher risk of fetal mobidity and
mortality compared to appropriately grown fetuses matched for gestational age.71 Long-term
follow-up studies have shown an increased incidence of physical handicap and neurodevelopmental delay in growth restricted fetuses.72,73
The presence of chronic metabolic acidemia in
utero, rather than actual birth weight appears to
be the best predictor of long-term neurodevelopmental delay.74 In pregnancies with growth
restricted fetuses, timing of the delivery is the
most critical step in clinical management. Balancing the risk of prematurity with the risk of
long-term neurodevelopmental delay is a serious
challenge facing physicians involved in the care
of these pregnancies.
The term “small for gestational age” (SGA) is
commonly used to describe all fetuses who are
small and, by this definition, represent a heterogeneous group of both normal and “growthrestricted” fetuses. We reserve the term “IUGR”
to fetuses who are SGA and who show other
evidence of chronic hypoxia or malnutrition.
Nevertheless, the terms SGA and IUGR are frequently used interchangeably.
The most common definition of SGA is a
fetus whose weight is below the 10th percentile
for gestational age. However, this definition is
not universally accepted. Some authors may define it has fetal weight below the 5th or 3rd
percentile, AC below the 10th, 5th, or 3rd percentile, or lack of normal growth of the abdominal
circumference on serial examinations. Other may
11
categorize growth disturbance based on absolute
weight at birth such as ⬍2,500 or ⬍1,500 g.
However, this obscures the distinction between
smallness caused by prematurity and that caused
by growth restriction.
Risk Factors
Causes and associations for IUGR are shown in
Table 6 The most common associations are with
maternal hypertension, and/or a history of
IUGR in previous pregnancies. Conversely, a his-
Table 6. Causes and Associations With IUGR
Maternal
Pregnancy induced hypertension/pre-eclampsia
Severe chronic hypertension
Severe maternal diabetes mellitus
Collagen vascular disease
Heart disease
Smoking159
Poor Nutrition
Renal disease
Lung disease/hypoxia
Environmental agents
Endocrine disorders
Previous history of IUGR
Uterine-placental
Uterine-placental dysfunction
Placental infarct
Chronic abruption
Multiple gestation/twin transfusion syndrome
Confined placental mosaicism
Fetal
Chromosome abnormalities
Confined placental mosaicism
Anomalies
Skeletal dysplasias
Multiple anomaly syndromes
aarskog
Ataxia-Telangiectasia Syndrome
Bloom
Brachmann-de Lange
Charge
Coffin-Siris
Dubowitz
Fanconi
Johansen-Blizzard
Neu-Laxova syndrome
Noonan
Pena-Shokier
Roberts
Russel-Silver
Seckel
Smith-Lemli-Opitz syndrome
Williams (Catch 22)
Infection
Teratogens
�12
Abnormal Fetal Growth
tory of SGA fetuses is a risk factor for preeclampsia.75 Table 7 presents risk factors for development of IUGR.
Underlying uterine-placental dysfunction is a
commonly evoked cause for otherwise unexplained fetal IUGR. Uterine-placental dysfunction has been correlated with a range of pathological findings including smaller placentas,
increase in the thickness of tertiary-stem villi
vessel wall, and decrease in lumen circumference. Uterine-placental dysfunction produces fetal hypoxia, which results in subnormal growth,
oligohydramnios, and alterations in blood flow.76
IUGR may be the primary, or in some cases
the only sonographic evidence of underlying fetal
anomalies. Early onset IUGR is a common manifestation of major chromosome abnormalities,
particularly trisomies 18 and 13, and triploidy.77,78
Other chromosomal anomalies or genetic
syndromes may exhibit growth delay as a
dominant feature. Chromosome abnormalities
confined to the placenta (confined placental
mosaicism) may also present with IUGR and
affected pregnancies are also at higher risk for
fetal death.79 Abnormal growth and development has also been associated with disturbed
genomic imprinting (expression of genes depending on whether they are located on the
maternal or on the paternal chromosome). This
has lead to the suggestion that the genomic
imprinting has evolved as a mechanism to regulate embryonic and fetal growth.80
Diagnosis
The primary sonographic means for detecting
SGA fetuses is demonstration of estimated fetal
weight to be less than a discriminatory level,
commonly set as the 10th percentile. Because
estimated fetal weight is strongly influenced by
AC, it is important to obtain accurate and consistent measurement of the AC whenever growth
disturbances are suspected. Small AC percentiles
have been found to be a sensitive marker for
IUGR. The small AC measurement may reflect a
reduction in size of the liver or other intraabdominal organs, reduced amounts of fat, or
possibly an elevated diaphragm because of poor
lung growth.81
Symmetric Versus Asymmetric IUGR
“Symmetric” IUGR has been used to describe a
growth pattern when all biometric measurements appear affected to the same degree,
whereas “asymmetric” IUGR has been used to
characterize a smaller abdominal circumference
compared to other growth parameters. Asymmetric IUGR would then show abnormal ratios
such as the HC/AC ratio or FL/AC ratio.82
When first introduced, the term symmetric
IUGR was suggested as more likely to reflect
underlying fetal condition including aneuploidy,
whereas asymmetric IUGR supposedly reflected
underlying uterine-placental dysfunction. However, these assumptions have proved to be
largely false. Asymmetric IUGR was more likely
to be associated with a major fetal anomaly in
one study,83 may be seen with aneuploidy (for
example, triploidy), and present as early as symmetric IUGR.84 Fetuses with symmetric and
asymmetric IUGR also show a similar degree of
acid-base impairment.85 The FL/AC ratio has
Table 7. Risk Factors for the Development of IUGR. Percent Difference in Estimated Fetal Weight and Birth
Weight Associated With Various Maternal and Fetal Characteristics by Gestational Age
Mean Gestational Age
Characteristics
18 wk
25 wk
31 wk
36 wk
40 wk (birth)
Black v white
Female v male
Cigarettes, ⬎20 vs none
Previous low birth weight vs none
Height, ⬍157 cm v ⬎167 cm
Body mass index, ⬍19.5 v ⬎26
Weight gain, ⬍8 kg v ⬎16 kg
Hypertension v none
NS
⫺9.2°
NS
NS
NS
NS
NS
NS
NS
⫺2.6°
NS
NS
NS
⫺3.6°
⫺3.6°
NS
NS
⫺1.4°
NS
NS
⫺3.3°
⫺3.8°
⫺3.8°
NS
⫺4.3*
⫺3.2*
⫺5.1*
⫺2.8°
⫺4.4*
⫺6.7*
⫺5.0*
NS
⫺4.9*
⫺4.6*
⫺6.2*
⫺3.6*
⫺5.9*
⫺8.8*
⫺7.5*
⫺4.3°
Data from Goldenberg RL, Davis RV, Clizer SN, et al: Maternal risk factors and their influence on fetal anthropometric
measurements. Am J Obstet Gynecol 168:1197-1205, 1993.
�Nyberg, Abuhamad, and Ville
also been found to be useful for prediction of
IUGR.86
Despite these arguments, it is worthwhile to
compare the pattern of fetal biometry. Low
weight to length ratio is correlated with perinatal morbidity, even in infants not small for gestational age.87 This may reflect fetuses who are
compromised but whose weight does not fall
below the 10th percentile. Dashe et al83 also
found that fetuses with asymmetric SGA are at
increased risk for intrapartum and neonatal
complications. Fetuses with asymmetric IUGR
were more likely to have pregnancy-induced hypertension at or before 32 weeks (7% v 1%), and
cesarean delivery for nonreassuring fetal heart
(15% v 3%, P ⬍ .001) compared to symmetric
IUGR. They were also more likely to have adverse neonatal outcome (14% v 5%, P ⫽ .001)
including respiratory distress, intraventricular
hemorrhage, sepsis, or neonatal death compared to appropriate for gestational age (AGA)
fetuses. In contrast, symmetric SGA infants were
not at increased risk.
Disproportionately small HC is also important
to identify and, when severe, may indicate microcephaly. Microcephaly is typically diagnosed
when the HC is 3 SDs below the mean for gestational age.88 The causes of microcephaly are
diverse. Among these, cocaine exposure has
been associated with microcephaly. Newborns
exposed to a high levels of cocaine exhibit asymmetric growth restriction in which the HC is
disproportionately smaller than would be predicted from the birth weight (head wasting).
The deficit in head size associated with cocaine
exposure may reflect the effects of a specific
central nervous system insult that interferes with
prenatal brain growth.89
Serial Ultrasound Examinations
Dynamic evaluation of fetal growth with serial
ultrasound is more important than a single examination when fetal measurements are below
the 10th percentile. This is true irrespective of
the methods used including cross-sectional or
longitudinal growth charts, customized growth
charts or predicted fetal growth. The optimal
measurement interval in small fetuses to combine an acceptable technical error and useful
clinical data seems to be around 10 days to overcome intra- and inter-observer variabilities.90
13
However, longer time intervals will more accurately reflect fetal growth in low-risk patients.91
Using 2 or more ultrasounds during the third
trimester, Smith-Bindman et al92 found that subnormal fetal growth was associated with a 3.9
times the risk of a birth weight less than 2,500 g,
17.7 times the risk of a birth weight less than the
3rd percentile, 2.3 times the risk of preterm
birth, 2.6 times the risk of a prolonged hospitalization for the newborn, and 3.6 times the risk of
admission to the neonatal intensive care unit.
For each outcome, inadequate growth on serial
examinations identified more fetuses with poor
birth outcomes than low estimated fetal weight
from a single examination. These authors conclude that serial ultrasounds can detect inadequate growth and fetuses at risk of poor outcomes, even when GA is unknown. On the other
hand, Williams and Nwebube93 found that a single measurement of the fetal AC made within 1
week prior to delivery was better than assessment
of serial examinations in the third trimester for
detecting patients who require cesarean delivery
for fetal distress.
Other Ultrasound Measures of IUGR
A number of other abnormal morphologic measurements or ratios may be used in an attempt to
identify fetuses affected with IUGR. The most
interesting measurements are those of internal
organs such as the brain, kidneys, and liver. The
kidneys are affected in fetuses with IUGR and
this probably explains oligohydramnios in these
patients. Silver et al94 found that IUGR fetuses
had significantly smaller renal volumes than
control fetuses, but no difference in renal artery
Doppler measurements. Smaller renal volumes
may correlate with oligonephropathy and this
may help to explain the association between
IUGR and an increased risk of developing hypertension and related cardiovascular diseases
among adults.94
Boito et al95 used three-dimensional ultrasound to evaluate liver size in growth disturbances. Among normally grown fetuses, they
found that the mean liver volume was 9.7 mL
(SD 4.4) at 20 weeks and 96.4 mL (SD 8.2) at 36
weeks of gestation. In a small group of fetuses
affected with growth restriction, the the liver
volume was 45% of expected whereas the AC was
82% of expected. Although this difference was
�14
Abnormal Fetal Growth
not statistically significant, it suggests that measurement of hepatic volume may be more sensitive than measurement of AC for evaluating fetuses with growth restriction. In a subsequent
study, Boito et al95 found that fetuses found to
be SGA had a higher brain to liver volume ratio
than control fetuses (5.9 v 3.4, P ⬍ .001). Furthermore, the brain/liver volume ratio was inversely related umbilical venous blood flow.
Other Parameters of Assessing Fetal Well
Being
Measurements of fetal biometry can help identify fetuses who are SGA, but cannot necessarily
distinguish healthy from compromised fetuses.
Therefore, in the setting of a SGA fetus, it is
important to correlate fetal size with other correlates of fetal health. Available methods for
evaluating fetal well being include cardiotography (CTG), amniotic fluid assessment with or
without other components of the biophysical
profile, and Doppler studies.97-99 These methods
provide a wealth of information regarding fetal
well being that can help to identify compromised fetuses. Although these tests are usually
interpreted separately, integration of these tests
could provide a better overall assessment of fetal
health. Scoring systems that incorporate sonographic estimates of fetal weight, amniotic fluid
assessment, and clinical parameters have been
devised.99,100
Cardiotocography, also known as the nonstress test, is one of the more established methods of fetal surveillance. During cardiotocography, the physician looks for heart rate variability
as a sign of fetal well-being. Heart rate variability
is the final result of the rhythmic, integrated
activity of autonomic neurons generated by organized cardiorespiratory reflexes.101 In growth
restricted fetuses, higher baseline rates, decreased long- and short-term variability, and delayed maturation of reactivity is seen in heart
rate tracings.102,103 Some studies suggest that replacing standard CTG with computer analysis
further improves the prediction of fetal distress
and mortality in IUGR fetuses.104 Unaided visual
analyses of fetal heart rate records have been
shown to have limited reliability and reproducibility.105,106 Furthermore, the presence of
overtly abnormal patterns of fetal heart rate tracings represents late signs of fetal deteriora-
tion.107,108 Relying on unaided visual analysis of
cardiotocography as the only test of fetal surveillance in growth restricted fetuses have come
under criticism as it represents late signs of fetal
deterioration and thus its sole use may not optimize long-term outcome of these pregnancies.
The biophysical profile (BPP) has been correlated with fetal pH, perinatal morbidity and
fetal mortality in cases of IUGR.109 Lower BPP
scores have associated with low arterial pH, low
Apgar scores and increased rate of cesarean sections in growth restricted fetus.110 The biophysical profile has also been shown to better correlate with fetal well being than fetal heart rate
tracing among patients in labor.111 In nearly all
cases of severe IUGR, abnormal BPP scores occur after or simultaneously with deterioration of
arterial and venous flow patterns on Doppler
studies. Therefore, addition of Doppler studies
should improve the performance of the biophysical score in the detection of fetal distress.112
The classic BPP evaluates five characteristics:
fetal movement, tone, breathing, heart reactivity, and amniotic fluid volume estimation. The
basis of the BPP is that components of the
BPP follow a predictable pattern secondary to
hypoxia. Loss of fetal breathing movements is
the most sensitive, but also the least specific, of
the parameters. Further hypoxia may reduce fetal movements and, in the most severe cases,
affect fetal tone.
Low amniotic fluid volume reflects chronic
hypoxia whereas the other parameters reflect
more acute changes. Low amniotic fluid is usually defined as an amniotic fluid index of 5 or
less, although various criteria have been used.113
A number of modifications to the standard
BPP have been proposed. The most common
modification is to omit heart reactivity and to
evaluate that separately as the nonstress test.114
The rapid BPP has been defined as amniotic fluid assessment and sound-provoked fetal
movement. It has been found to be an effective
predictor of intrapartum fetal distress in highrisk pregnancies and appears to be more effective than nonstress tests.115
Doppler ultrasound can provide important
physiologic information of altered flow states,
either in the fetal-placental or the uterine-placental circulations. The umbilical artery is the
most common site of sampling with duplex
Doppler. It reflects the umbilical-placental cir-
�Nyberg, Abuhamad, and Ville
culation from the fetal side. Abnormal waveforms patterns may be seen with IUGR and placental dysfunction.
Doppler may also be used to interrogate a
variety of other sites of the fetal circulation,
including the middle cerebral artery, aorta, and
splenic artery, among others.116 A comparison of
arterial resistance of the umbilical and cerebral
circulations has been referred to as the cerebroplacental Doppler ratio. Although this ratio varies somewhat during pregnancy, reflecting the
quadratic relationship of resistance observed
of the middle cerebral artery with gestational
age,117 it almost always exceeds 1 throughout
pregnancy. Reversal of this normal relationship
may be seen with the “brain sparing” effect.
A number of cross-sectional and longitudinal
studies have highlighted the fetal cardiovascular
adaptation to hypoxemia and the progressive
stages of such adaptation.118-123 Findings from
these studies suggest that arterial Doppler is the
first Doppler abnormality to be seen. Venous
Doppler abnormalities, which reflect fetal cardiac dyfunction, are late signs of fetal adaptation
and are commonly associated with the presence
fetal acidemia. Overt abnormalities of fetal heart
tracing and loss of biophysical parameters appear to follow venous Doppler changes in most
growth restricted fetuses.
Use of Doppler ultrasound has been shown to
improve outcome in high-risk pregnancies.124
Clinical management based on information obtained from umbilical artery Doppler velocimetry
prior to 32 weeks may result in decreased perinatal mortality and lower rates of obstetric interventions.125 Although morphometric measurements are, not surprisingly, more accurate than
Doppler studies for identification of SGA fetuses,126 Doppler studies have found to be useful
in prediction of adverse outcome among SGA
fetuses.127
Uterine artery Doppler reflects the uterineplacenta circulation from the maternal side. Abnormal placentation and trophoblastic invasion
may result in abnormal waveform patterns of the
uterine arteries, and predict future development
of pre-eclampsia and IUGR. Uterine artery
Doppler has the potential to identify patients in
the “pre-disease” condition who are at risk for
fetal growth delay and adverse outcome.128 Uterine artery Doppler has been shown to be particularly effective in patients at risk of developing
15
hypertension when used during the second trimester. Abnormal uterine artery Doppler waveforms near term have also been associated with
an increased risk of adverse outcome among
growth restricted fetuses.129
Macrosomia
Large-for-gestational age (LGA) is defined by an
estimated fetal weight greater than the 90th percentile. Neonatal macrosomia is defined in absolute terms as birth weight greater than 4,500 g;
old charts used 4,000 g but physiological birth
weights have increased over the years. As expected, the prevalence of macrosomia varies
widely between countries.
Because of a higher risk of fetal mortality and
morbidity, accurate prediction of macrosomia is
a public health problem which answer partly
relies on fetal ultrasound examination. However, there are 3 problems in screening for
macrosomia: the sonographic diagnosis of
macrosomia is not reliable, 90% of macrosomic
babies will not suffer any complication, and finally prevention of perinatal morbidity and mortality would imply a 10% increase in the cesarean
section rate and its maternal morbidity.
Risk Factors
Risk factors are well established with a good
sensitivity but are not specific since most women
at risk will deliver babies of normal weight. The
main risk factors are grouped under the acronym “DOPE,” standing for diabetes, obesity,
postdates, excessive fetal weight or maternal
weight gain sequence.
Genetically driven excessive growth can be
seen in a number of conditions (Table 8). An
excessive prenatal growth rate is usually maintained throughout the pregnancy. Precise diagnosis is often difficult to ascertain and relies on
subtle differences; the prognosis is also extremely difficult to ascertain antenatally and in
the neonatal period.130
Diagnosis
There are numerous mathematical formulae
and indices developed to predict fetal macrosomia.131-137 Simple formulae for estimating fetal
weight may do just as well as complex ones.138,139
Nearly all formulas include the AC because it
accurately reflects fetal girth.
�16
Abnormal Fetal Growth
Table 8. Associations With Excessive Fetal Growth (Macrosomia)
Pertinent features in early
Overgrowth syndromes
Excessive growth
of prenatal Onset
Accelerated osseous
maturation
Developmental delay
Mental retardation
Poor co-ordination
Learning difficulties
Hoarse, abnormal cry
Dysarthric speech
Dilated ventricles and
cavum septiPellucidi
Craniofacial features
Macrocephaly
Hypertelorism
Large ears
Down-slanting palpebral
fissures
Relative micrognathia
Limbs
Campto(clino)-dactyly
Prominent finger pads
Flared metaphases
Increased risk for
malignancy
Gene locus
Weaver
Sotos
Marshall-Smith
Beckwith-Widemann
Simpson-Golabi-Behmel
⫹⫹⫹
⫹⫹
⫹
⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹⫹
⫹
⫹⫹
⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹⫹
⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹
⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹
⫹
⫹
⫹
⫹⫹
⫹⫹
⫹⫹
⫹
⫹
⫹
No Speech
⫹⫹⫹
⫹⫹
⫹
⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹⫹
⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹⫹
⫹⫹⫹
⫹
⫹
?
⫹⫹
?
?
⫹
⫹
⫹⫹
⫹⫹
⫹
⫹
⫹⫹
⫹⫹
11p15.5
⫹
Xp26
⫹
Data from Ville Y, Nyberg DA, in Nyberg DA, McGahan JC, Pretorius DH, et al: Growth, Doppler, and Fetal Assessment,
Diagnostic Imaging of Fetal Anomalies, Lippincott and Williams, 2003.
Most studies now define macrosomia as
estimated weight greater than 4,500 g. However, some studies have used 4,500 g among
nondiabetics but 4,000 g among diabetic women
since they are at greater risk of fetal macrosomia.140
The mean sonographic error in estimating
fetal weight is higher with macrosomic fetuses,
reaching 15% at term compared to less than
10% for normal size fetuses. Field et al135 found
that regardless of maternal size, almost half of
the weight predictions were within 5% of the
actual birth weight Approximately 50% to 70%
of estimated weights fall within than 10% of the
actual birth weight encompassing the cut-off of
4,000 g in 95% of the cases when the estimated
birth weight is equal or superior to 4,000 g.133-137
On the other hand, maternal diabetes probably
does not change the accuracy of the measurements, although some authors suggest that prediction of fetal weight is worse in diabetic pregnancies.141 In nondiabetic patients, the addition
of a glucose challenge test at 24 to 28 weeks
showed limited ability to improve sonographic
prediction of fetal macrosomia.142 Measurement
of AC alone may identify macrosomic fetuses.
Gilby et al143 found that if the AC was ⬍35 cm,
the risk of infant birth weights ⬎4,500 g was
⬍1%. On the other hand, if the AC is ⬎ or ⫽ 38
cm, the risk was 37% (37/99), and ⬎50% of
these infants were identified (37/69 or 53.6%).
Holcomb et al144 suggest that the abdominal
circumference percentile is useful and should be
reported, in addition to estimated weight percentile, in fetuses who are large for GA.
Other measurements may be obtained to
help detect macrosomia and complications of
macrosomia, including soft tissue measurements. However, measurements of soft tissue do
not appear to be superior to clinical or sonographic predictions in identifying fetuses with
weights of at least 4,000 g.145
Ultrasound is not considered to be specific
enough to predict shoulder dystocia. A few studies using ultrasound or even magnetic resonance
imaging have been encouraging.146-148 However,
�Nyberg, Abuhamad, and Ville
the sensitivity and specificity of are unlikely to be
over 40% and 75% respectively, which would
mean to perform a cesarean section in 25% of
the patients to avoid only 40% of all shoulder
dystocias.149
A number of studies have concluded that clinical examination works just as well as ultrasound
to predict birth weight at term, especially when it
is above 4,500 g.150-154 A two-step clinical and
sonographic approach does not perform better
since the sensitivity is 17% and the positive predictive value is only 36% for estimated birth
weight of ⬎4,000 g.150
The predictive value of a LGA fetus is further
increased when polyhydramnios is also present.
Sohaey et al155 reported that 28% of fetus with
polyhydramnios had birth weights at the 90th
percentile or greater. Conversely, the combination of oligohydramnios and a fetal weight estimate below the 90th percentile virtually excludes the possibility of LGA.156
The origin for polyhydramnios among largefor-gestational age fetuses remains unclear. Maternal diabetes is not independently associated
with polyhydramnios, after accounting for
macrosomia.157 Some have suggested polyhydramnios may reflect increased renal vascular
flow, whereas others suggest it is secondary to
bulk flow of water across the surface of the fetus,
umbilical cord, placenta and membranes. Larger
fetuses with larger lung volumes and placental
surface areas would be expected to produce
greater amounts of amniotic fluid. Although
one might also expect a relationship between
the severity of polyhydramnios and birth weight,
no direct correlation has been found.157,158
Conclusions
A primary role of obstetric ultrasound is determining GA and assessing fetal growth. Although
a large number of fetal measurements can be
obtained, standard assessment relies on only
measurements of the head, abdomen, and one
or more long bones. From these measurements,
the fetal weight can be estimated and compared
with the expected weight to calculate the weight
percentile. Three-dimensional ultrasound may
have a future role in estimation of fetal weight.
Assessment of fetal growth should not be
viewed in isolation. Other methods for assessing
fetal health include fetal cardiotrography, assess-
17
ment of amniotic fluid, the biophysical profile,
and Doppler studies. The clinical history and
risk factors should also be considered. Finally,
serial ultrasound assessment is more predictive
than a single ultrasound exam for assessing fetal
growth and health.
References
1. Campbell S, Warsof SL, Little D, et al: Routine ultrasound screening for the prediction of gestational age.
Obstet Gynecol 65:613-620, 1985
2. Waldenstrom U, Axelsson O, Nilsson S: A comparison
of the ability of a sonographically measured biparietal
diameter and the last menstrual period to predict the
spontaneous onset of labor. Obstet Gynecol 76:336-338,
1990
3. Wilcox M, Gardosi J, Mongelli M, et al: Birth weight
from pregnancies dated by ultrasound in a multicultural British population. Br Med J 307:588-591, 1993
4. Gardosi J, Mongelli M: Risk assessment adjusted for
gestational age in maternal serum screening for Down’s
syndrome. Br Med J 306:1509, 1993
5. Chervenak FA, Skupski DW, Romero R, et al: How
accurate is fetal biometry in the assessment of fetal age?
Am J Obstet Gynecol 178:228-237, 1998
6. Goldenberg RL, Davis RO, Cutter GR, et al: Prematurity, postdates, and growth retardation: The influence
of use of ultrasonography on reported gestational age.
Am J Obstet Gynecol 160:462-470, 1989
7. Gardosi J, Vanner T, Francis A: Gestational age and
induction of labour for prolonged preganncy. Br J
Obstet Gynaecol 104:792-797, 1997
8. Warren WB, Peisner DB, Raju S, et al: Dating the early
pregnancy by sequential appearance of embtyonic
structures. Am J Obstet Gynecol 161:747, 1989
9. Daya S: Accuracy of gestational age estimation by
means of fetal crown-rump length measurement. Am J
Obstet Gynecol 168:903-908, 1987
10. Nyberg DA, Mack LA, Laing FC, et al: Distinguishing
normal from abnormal gestational sac growth in early
pregnancy. J Ultrasound Med 6:23-27, 1987
11. Robinson HP, Fleming JE: A critical evaluation of sonar “crown-rump length” measurement. Br J Obstet
Gynaecol 82:702-710, 1975
12. Drumm JE, Clinch J, McKenzie G: The ultrasonic measurement of fetal crown rump length as a method of
assessing gestational age. Br J Obstet Gynaecol 83:417421, 1976
13. Daya S, Woods S, Ward S, et al: Early pregnancy assessment with transvaginal ultrasound scanning. Can Med
Assoc J 144:441-446, 1996
14. Lasser DM, Peisner DB, Wollenbergh J, et al: First
trimester fetal biometry using transvaginal sonography.
Ultrasound Obstet Gynecol 3:104-108, 1993
15. McGregor SN, Tamura RK, Sabbagha RE, et al: Underestimation of gestational age by conventional crown
rump length dating curves. Am J Obstet Gynecol 70:
344-348, 1987
16. Wisser J, Dirscheld P: Estimation of gestational age by
�18
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
Abnormal Fetal Growth
transvaginal sonographic measurement of greatest embryonic length in dated human embryos. Ultrasound
Obstet Gynecol 4:457-462, 1994
Hadlock FP: Sonographic estimation of fetal age and
weight. Radiol Clin North Am 28:39-50, 1990
Hadlock FP, Harrist RB, Shah YP, et al: Estimating fetal
age using multiple parameters: A prospective evaluation in a racially mixed population. Am J Obstet Gynecol 156:955-957, 1987
Bromley B, Frigoletto FD Jr, Harlow BL, et al: Biometric
measurements in fetuses of different race and gender.
Ultrasound Obstet Gynecol 3:395-402, 1993
Tunon K, Eik-Nes SH, Grottum P: Fetal outcome in
pregnancies defined as post-term according to the last
menstrual period estimate, but not according to the
ultrasound estimate. Ultrasound Obstet Gynecol 14:1216, 1999
Kallen K: Mid-trimester ultrasound prediction of gestational age: Advantages and systematic errors. Ultrasound Obstet Gynecol 2002 20:558-63, 2002
Stebbins B, Jaffe R: Fetal biometry and gestational age
estimation, in Jaffe R, Bui TH (eds): Textbook of Fetal
Ultrasound. London, Parthenon Publishing, 1999, pp
47-57
Pierce BT, Hancock EG, Kovac CM, et al: Influence of
gestational age and maternal height on fetal femur
length calculations. Obstet Gynecol 975 Pt 1:742-746,
2001
Bromley B, Frigoletto FD Jr, Harlow BL, et al: Biometric
measurements in fetuses of different race and gender.
Ultrasound Obstet Gynecol 3:395-402, 1993
Shipp TD, Bromley B, Mascola M, et al: Variation in
fetal femur length with respect to maternal race. J
Ultrasound Med 20:141-144, 2001
Davis RO, Cutter GR, Goldenberg RL, et al: Fetal
biparietal diameter, head circumference, abdominal
circumference and femur length. A comparison by race
and sex. J Reprod Med 38:201-206, 1993
Kurjak A, Kirkinen P, Latin V: Biometric and dynamic
ultrasound assessment of small-for-dates infants: Report
of 260 cases. Obstet Gynecol 56:281-284, 1980
Landon MB, Mintz MC, Gabbe SG: Sonographic evaluation of fetal abdominal growth: Predictor of the large
for gestational age infant in pregnancies complicated
by diabetes mellitus. Am J Obstet Gynecol 160:115-121,
1989
Basel D, Lederer R, Diamant YZ: Longitudinal ultrasonic biometry of various parameters in fetuses with
abnormal growth rate. Acta Obstet Gynecol Scand 66:
143-149, 1987
Hadlock FP: Ultrasound evaluation of fetal growth, in
Callen PW (ed): Ultrasonography in Obstetrics and
Gynecology. Philadelphia, PA, Saunders, 1994, pp 129143
Dudley NJ: Selection of appropriate ultrasound methods for estimation of fetal weight. Br J Radiol 68:385388, 1995
Coombs CA, Jaekle RK, Rosenn B, et al: Sonographic
estimation of fetal weight based on a model of fetal
volume. Obstet Gynecol 82:365-370, 1993
Rose BI, McCallum WD: A simplified method for esti-
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
mating fetal weight using ultrasound measurements.
Obstet Gynecol 69:671-675, 1987
Medchill MT, Peterson CM, Garbaciak J: Prediction of
estimated fetal weight in extremely low birth weight
neonates (500-1000 g). Obstet Gynecol 78:286-290,
1991
Hadlock FP, Harrist RB, Carpenter RJ, et al: Sonographic estimation of fetal weight. Radiology 150:535540, 1984
Smith GCS, Smith MFS, McNay MB, et al: The relation
between fetal abdominal circumference and birthweight: Findings in 3512 pregnancies. Br J Obstet
Gynaecol 104:186-190, 1997
Gore D, Williams M, O’Brien W, et al: Fetal abdominal
circumference for prediction of intrauterine growth
restriction. Obstet Gynecol 95:S78-S79, 2000 (4 suppl 1)
Chuang L, Hwang JY, Chang CH, et al: Ultrasound
estimation of fetal weight with the use of computerized
artificial neural network model. Ultrasound Med Biol
28:991-996, 2002
Baum JD, Gussman D, Wirth JC 3rd: Clinical and patient estimation of fetal weight vs. ultrasound estimation. J Reprod Med 47:194-198, 2002
Robson SC, Gallivan S, Walkinshaw SA, et al: Ultrasonic
estimation of fetal weight: Use of targeted formulas in
small for gestational age fetuses. Obstet Gynecol 82:
359-64, 1993
Sabbagha RE, Minogue J, Tamura RK, et al: Estimation
of birth weight by use of ultrasonographic formulas
targeted to large-, appropriate-, and small-for-gestational-age fetuses. Am J Obstet Gynecol 160:854-862, 1989
Edwards A, Goff J, Baker L: Accuracy and modifying
factors of the sonographic estimation of fetal weight 26.
Aust N Z J Obstet Gynaecol 41:187-190, 2001
Scott F, Beeby P, Abbott J, et al: New formula for
estimating fetal weight below 1000 g: Comparison with
existing formulas. J Ultrasound Med 15:669-672, 1996
Weiner CP, Sabbagha RE, Vaisrub N, et al: Ultrasonographic fetal weight prediction: Role of head circumference and femur length. Obstet Gynecol 65:812-817,
1985
Jouannic JM, Grange G, Goffinet F, et al: Validity of
sonographic formulas for estimating fetal weight below
1,250 g: A series of 119 cases. Fetal Diagn Ther 16:254258, 2001
Zelop CM: Prediction of fetal weight with the use of
three-dimensional ultrasonography. Clin Obstet Gynecol 43:321-325, 2000
Schild RL, Fimmers R, Hansmann M: Fetal weight estimation by three-dimensional ultrasound. Ultrasound
Obstet Gynecol 16:445-452, 2000
Song TB, Moore TR, Lee JI, et al: Fetal weight prediction by thigh volume measurement with three-dimensional ultrasonography. Obstet Gynecol 96:157-161,
2000
Lee W, Deter RL, Ebersole JD, et al: Birth weight prediction by three-dimensional ultrasonography: Fractional limb volume. J Ultrasound Med 20:1283-1292,
2001
Hooper PM, Mayes DC, Demianczuk NN: A model for
foetal growth and diagnosis of intrauterine growth restriction. Stat Med 21:95-112, 2002
�Nyberg, Abuhamad, and Ville
51. Goldenberg RL, Cutter GR, Hoffman HJ, et al: Intrauterine growth retardation: Standards for diagnosis.
Am J Obstet Gynecol 161:271-277, 1989
52. Altman DG, Chitty LS: Charts of fetal size. Methodology. Br J Obstet Gynaecol 101:29-34, 1994
53. Marsal K, Persson PH, Larsen T, et al: Intrauterine
growth curves based on ultrasonographically estimated
fetal weights. Acta Paediatr Scand 85:843-848, 1996
54. Singer DB, Sung CJ, Wigglesworth JS: Fetal growth and
maturation with standards for body and organ development, in Wigglesworth JS, Singer DB (eds): Textbook
of Fetal and Perinatal Pathology. Boston, MA, Blackwell
Science, 1991, pp 11-47
55. Hadlock FP, Harrist RB, Martinez-Poyer J: In utero
analysis of fetal growth: A sonographic weight standard.
Radiology 181:129-133, 1991
56. Doubilet PM, Benson CB, Nadel AS, et al: Improved
birth weight table for neonates developed from gestations dated by early ultrasonography. J Ultrasound Med
16:241-249, 1997
57. Hindmarsh PC, Geary MP, Rodeck CH, et al: Intrauterine growth and its relationship to size and shape at
birth. Pediatr Res 52:263-268, 2002
58. Magnus P, Bakketeig LS, Hoffman H: Birth weight of
relatives by maternal tendency to repeat small-for-gestational-age (SGA) births in successive pregnancies.
Acta Obstet Gynecol Scand 165:35-38, 1997 (suppl)
59. Wilcox MA, Newton CS, Johnson IR: Paternal influences on birthweight. Acta Obstet Gynecol Scand 74:
15-18, 1995
60. Gardosi J, Chang A, Kalyan B, et al: Customised antenatal growth charts. Lancet 339:283-287, 1992
61. Clausson B, Gardosi J, Francis A, et al: Perinatal outcome in SGA births defined by customised versus population-based birthweight standards. Br J Obstet Gynecol 108:830-834, 2001
62. Sciscione AC, Gorman R, Callan N: Adjustment of birth
weight standards for maternal and infant characteristics improves the prediction of outcome in the smallfor-gestational-age infant. Am J Obstet Gynecol 175:
544-547, 1996
63. Gestation Network http://www.gestation.net/birthweight
_centiles/centile_online.htm administered by the West
Midlands Perinatal Institute
64. Ong S, Lim MN, Fitzmaurice A, et al: The creation of
twin centile curves for size. Br J Obstet Gynecol 109:
753-758, 2002
65. Chang TC, Robson SC, Spencer JAD, et al: Identification of fetal growth retardation: Comparison of Doppler waveform indices and serial ultrasound measurements of abdominal circumference and fetal weight.
Obstet Gynecol 82:230-236, 1993
66. Owen P, Ogston S: Conditional centiles for the quantification of fetal growth. Ultrasound Obstet Gynecol
11:110-117, 1998
67. Skinner Keelin O’Donoghue F, Gardeil R, Greene MJ,
et al: Is fetal abdominal subcutaneous fat comparable
with established indices of growth restriction? J Obstet
Gynaecol 21:439-442, 2001
68. Matsumoto M, Yanagihara T, Hata T: Three-dimensional qualitative sonographic evaluation of fetal soft
tissue. Hum Reprod 15:2438-2442, 2000
19
69. Yoshida SH, Unno N, Kagawa H, Shinozuka N, et al:
Sonographic determination of fetal size from 20 weeks
of gestation onward correlates with birth weight. J Obstet Gynaecol Res 27:205-211, 2001
70. Cetin I, Morpurgo PS, Radaelli T, et al: Fetal plasma
leptin concentrations: Relationship with different intrauterine growth patterns from 19 weeks to term. Pediatr
Res 48:646-651, 2000
71. Bernstein IM, Horbar JD, Badger GJ, et al: Morbidity
and mortality among very-low-birth weight neonates
with intrauterine growth restriction. Am J Obstet Gynecol 182:198-202, 2000
72. Kok JH, den Ouden AL, Verloove-Vanhorick SP, et al:
Outcome of very preterm small for gestational age
infants: The first nine years of life. Br J Obstet Gynecol
105:162-168, 1998
73. Fattal-Valevski A, Leitner Y, Kutai M, et al: Neurodevelopmental outcome in children with intrauterine
growth retardation: A 3-year follow-up. J Child Neurol
14:724-727, 1999 (abstr)
74. Soothill PW, Ajayi RA, Campbell S, et al: Relationship
between fetal academia at cordocentesis and subsequent neurodevelopment. Ultrasound Obstet Gynecol
2:80-83, 1992
75. Rasmussen S, Irgens LM, Albrechtsen S, et al: Predicting preeclampsia in the second pregnancy from low
birth weight in the first pregnancy. Obstet Gynecol 965
Pt 1:696-700, 2000
76. Mitra SC, Seshan SV, Riachi LE: Placental vessel morphometry in growth retardation and increased resistance of the umbilical artery Doppler flow. J Matern
Fetal Med 9:282-286, 2000
77. Snijders RJ, Sherrod C, Gosden CM, et al: Fetal growth
retardation: Associated malformations and chromosomal abnormalities. Am J Obstet Gynecol 168:547-555,
1993
78. Dicke JM, Crane JP: Sonographic recognition of major
malformations and aberrant fetal growth in trisomic
fetuses. J Ultrasound Med 10:433-438, 1991
79. Stipoljev F, Latin V, Kos M, et al: Correlation of confined placental mosaicism with fetal intrauterine
growth retardation. A case control study of placentas at
delivery. Fetal Diagn Ther 16:4-9, 2001
80. Devriendt K: Genetic control of intra-uterine growth.
Eur J Obstet Gynecol Reprod Biol 92:29-34, 2000
81. Roberts AB, Mitchell JM, McCowan LM, et al: Ultrasonographic measurement of liver length in the smallfor-gestational-age fetus. Am J Obstet Gynecol 1803 Pt
1:634-638, 1999
82. David C, Gabrielli S, Pilu G, et al: The head-to-abdomen circumference ratio: A reappraisal. Ultrasound
Obstet Gynecol 5:256-259, 1995
83. Dashe JS, McIntire DD, Lucas MJ, et al: Effects of
symmetric and asymmetric fetal growth on pregnancy
outcomes. Obstet Gynecol 96:321-327, 2000
84. Vik T, Vatten L, Jacobsen G, et al: Prenatal growth in
symmetric and asymmetric small-for-gestational-age infants. Early Hum Dev 48:167-176, 1997
85. Blackwell SC, Moldenhauer J, Redman M, et al: Relationship between the sonographic pattern of intrauterine growth restriction and acid-base status at the time of
�20
86.
87.
88.
89.
90.
91.
92.
93.
94.
95.
96.
97.
98.
99.
100.
101.
102.
103.
Abnormal Fetal Growth
cordocentensis. Arch Gynecol Obstet 264:191-193,
2001
Benson CB, Doubilet PM, Saltzman DH, et al: FL/AC
ratio: Poor predictor of intrauterine growth retardation. Invest Radiol 20:727-730, 1985
Williams MC, O’Brien WF: A comparison of birth
weight and weight/length ratio for gestation as correlates of perinatal morbidity. J Perinatol 17:346-350,
1997
Brandon MWG, Kirman BH, Williams CE: Microcephaly. J Ment Sci 105:721, 1959
Bateman DA, Chiriboga CA: Dose-response effect of
cocaine on newborn head circumference. Pediatrics
106:E33, 2000
Divon M, Chamberlain P, Sipos L, et al: Identification
of the small for gestational age independent indices of
fetal growth. Am J Obstet Gynecol 155:1197-2003, 1986
Owen P, Maharaj S, Khan KS, et al: Interval between
fetal measurements in predicting growth restriction.
Obstet Gynecol 97:499-504, 2001
Smith-Bindman R, Chu PW, Ecker JL, et al: US evaluation of fetal growth: Prediction of neonatal outcomes.
Radiology 223:153-161, 2002
Williams KP, Nwebube N: Abdominal circumference: A
single measurement versus growth rate in the prediction of intrapartum Cesarean section for fetal distress.
Ultrasound Obstet Gynecol 17:493-495, 2001
Silver LE, Decamps PJ, Korst LM, et al: Intrauterine
growth restriction is accompanied by decreased renal
volume in the human fetus. Am J Obstet Gynecol 188:
1320-1325, 2003
Boito SM, Laudy JA, Struijk PC, et al: Three-dimensional US assessment of hepatic volume, head circumference, and abdominal circumference in healthy and
growth-restricted fetuses. Radiology 223:661-665, 2002
Boito S, Struijk PC, Ursem NT, et al: Fetal brain/liver
volume ratio and umbilical volume flow parameters
relative to normal and abnormal human development.
Ultrasound Obstet Gynecol 21:256-261, 2003
Ott WJ: Diagnosis of intrauterine growth restriction:
Comparison of ultrasound parameters. Am J Perinatol
19:133-137, 2002
Resnik R: Intrauterine growth restriction. Obstet Gynecol 99:490-496, 2002
Benson CB, Belville JS, Lentini JF, et al: Intrauterine
growth retardation: Diagnosis based on multiple parameters—A prospective study. Radiology 177:499-502,
1990
Benson CB, Boswell SB, et al: Improved prediction of
intrauterine growth retardation with use of multiple
parameters. Radiology 168:7-12, 1988
Hanna BD, Nelson MN, White-Traut RC, et al: Heart
rate variability in preterm brain-injured and very-lowbirth-weight infants. Biol Neonate 77:147-155, 2000
Nijhuis IJ, ten Hof J, Mulder EJ, et al: Fetal heart rate
in relation to its variation in normal and growth retarded fetuses. Eur J Obstet Gynecol Rep Biol 89:27-33,
2000
Vindla S, James D, Sahota D: Computerised analysis of
unstimulated and stimulated behaviour in fetuses with
intrauterine growth restriction. Eur J Obstet Gynecol
Rep Biol 83:37-45, 1999
104. Weiner Z, Farmakides G, Schulman H, et al: Surveillance of growth-retarded fetuses with computerized fetal heart rate monitoring combined with Doppler velocimetry of the umbilical and uterine arteries. J
Reprod Med 41:112-118, 1996
105. Devoe L, Golde S, Kilman Y, et al: A comparison of
visual analyses of intrapartum fetal heart rate tracings
according to the new National Institute of Child Health
and Human Development guidelines with computer
analyses by an automated fetal heart rate monitoring
system. Am J Obstet Gynecol 183:361-366, 2000
106. Bracero LA, Roshanfekr D, Byrne DW: Analysis of antepartum fetal heart rate tracing by physician and computer. J Matern Fetal Med 9:181-185, 2000
107. Hecher K, HackelÖer B: Cardiotocogram compared
to Doppler investigation of the fetal circulation in
the premature growth-retarded fetus: Longitudinal
observations. Ultrasound Obstet Gynecol 9:152-160,
1997
108. Ribbert LS, Visser GH, Mulder EJ, et al: Changes with
time in fetal heart rate variation, movement incidences
and haemodynamics in intrauterine growth retarded
fetuses: A longitudinal approach to the assessment of
fetal well being. Early Hum Dev 31:195-208, 1993
109. Manning FA, Snijders R, Harman CR, et al: Fetal biophysical profile score. VI. Correlation with antepartum
umbilical venous fetal pH. Am J Obstet Gynecol 169:
755-763, 1993
110. Habek D, Hodek B, Herman R, et al: Fetal biophysical
profile and cerebro-umbilical ratio in assessment of
perinatal outcome in growth-restricted fetuses. Fetal
Diagn Ther 18:12-16, 2003
111. Kim SY, Khandelwal M, Gaughan JP, et al: Is the intrapartum biophysical profile useful? Obstet Gynecol 102:
471-476, 2003
112. Baschat AA, Gembruch U, Harman CR: The sequence
of changes in Doppler and biophysical parameters as
severe fetalgrowth restriction worsens. Ultrasound Obstet Gynecol 18:571-577, 2001
113. Magann EF, Isler CM, Chauhan SP, et al: Amniotic
fluid volume estimation and the biophysical profile:
A confusion of criteria. Obstet Gynecol 96:640-642,
2000
114. Petrovic O, Skunca E, Matejcic N: A simplified
fetal biophysical profile. Int J Gynaecol Obstet 61:9-14,
1998
115. Tongsong T, Piyamongkol W, Anantachote A, et al:
The rapid biophysical profile for assessment of fetal
well-being. J Obstet Gynaecol Res 25:431-436, 1999
116. Oz U, Kovanci E, Jeffress A, et al: Splenic artery
Doppler in the prediction of the small-for-gestational
age infant. Ultrasound Obstet Gynecol 20:346-350,
2002
117. Baschat AA, Gembruch U: The cerebroplacental Doppler ratio revisited. Ultrasound Obstet Gynecol 21:124127, 2003
118. Bahado-Singh RO, Kovanci E, Jeffres A, et al: The
Doppler cerebroplacental ratio and perinatal outcome
in intrauterine growth restriction. Am J Obstet Gynecol
180:750-756, 1999
119. Rizzo G, Capponi A, Talone PE, et al: Doppler indices
from inferior vena cava and ductus venosus in predict-
�Nyberg, Abuhamad, and Ville
120.
121.
122.
123.
124.
125.
126.
127.
128.
129.
130.
131.
132.
133.
134.
135.
ing pH and oxygen tension in umbilical blood at cordocentesis in growth-retardated fetuses. Ultrasound
Obstet Gynecol 7:401-410, 1996
Baschat AA, Gembruch U, Reiss I, et al: Relationship
between arterial and venous Doppler and perinatal
outcome in fetal growth restriction. Ultrasound Obstet
Gynecol 16:407-413, 2000
Baschat AA, Gembruch U, Harman CR: The sequence
of changes in Doppler and biophysical parameters as
severe fetal growth restriction worsens. Ultrasound Obstet Gynecol 18:571-577, 2001
Hecher K, Bilardo CM, Stigter RH, et al: Monitoring of
fetuses with intrauterine growth restriction: A longitudinal study. Ultrasound Obstet Gynecol 18:564-570,
2001
Ferrazzi E, Bozzo M, Rigano S, et al: Temporal sequence of abnormal Doppler changes in the peripheral
and central circulatory systems of the severely growthrestricted fetus. Ultrasound Obstet Gynecol 19:140-146,
2002
Zarko A, Neilson JP: Doppler ultrasonography in highrisk pregnancies: Systematic review with meta-analysis.
Am J Obstet Gynecol 172:1379-1387, 1995
Marsal K: Intrauterine growth restriction. Curr Opin
Obstet Gynecol 14:127-135, 2002
Chang TC, Robson SC, Boys RJ, et al: Prediction of
the small for gestational age infant: Which ultrasonic
measurement is best? Obstet Gynecol 80:1030-1038,
1992
Chang TC, Robson SC, Spencer JA, et al: Prediction of
perinatal morbidity at term in small fetuses: Comparison of fetal growth and Doppler ultrasound. Br J Obstet
Gynaecol 101:422-427, 1994
Baschat AA: Integrated fetal testing in growth restriction: combining multivessel Doppler and biophysical parameters. Ultrasound Obstet Gynecol 21:1-8,
2003
Vergani P, Roncaglia N, Andreotti C, et al: Prognostic
value of uterine artery Doppler velocimetry in growthrestricted fetuses delivered near term. Am J Obstet
Gynecol 187:932-936, 2002
Schwartzler P, Homfray T, Campbell S, et al: Prenatal
findings on ultrasound and X-ray in a case of overgrowth syndrome associated with increased nuchal
translucency. Prenat Diagn 21:341-345, 2001
Hirata GI, Medearis AL, Horenstein J, et al: Ultrasonographic estimation of fetal weight in the clinically
macrosomic fetus. Am J Obstet Gynecol 162:238-242,
1990
Elliott JP, Garite TJ, Freeman RK, et al: Ultrasound
prediction of fetal macrosomia in diabetic patients.
Obstet Gynecol 60:159-162, 1982
Alsulyman OM, Ouzounian JG, Kjos SL: The accuracy
of intrapartum ultrasonographic fetal weight estimation n diabetic pregnancies. Am J Obstet Gynecol 177:
503-506, 1997
Benacerraf BR, Gelman R, Frigoletto FD: Sonographically estimated fetal weights: Accurracy and limitations.
Am J Obstet Gynecol 159:1118-1121, 1988
Field NT, Piper JM, Langer O: The effect of maternal
obesity on the accuracy of fetal weight estimation. Obstet Gynecol 86:102-107, 1995
21
136. Hedriana HL, Moore TR: A comparison of single versus
multiple growth ultrasonographic examinations in predicting birth weight. Am J Obstet Gynecol 170:16001604, 1994; discussion 1604-1606
137. Platek DN, Divon MY, Anyeagbunam A, et al: Intrapartum ultrasonographic estimates of fetal weight by the
house staff. Am J obstet Gynecol 165:842-845, 1991
138. Shepard MJ, Richards VA, Berkowitz RL: An evaluation
of 2 equations for predicting fetal weight by ultrasound. Am J Obstet Gynecol 142:47-51, 1982
139. Coombs CA, Rosenn B, Miodovnik M, et al: Sonographic EFW and macrosomia: Is there an optimum
formula to predict diabetic fetal macrosomia? J Matern
Fetal Med 9:55-61, 2000
140. Sokol RJ, Chik L, Dombrowski MP, et al: Correctly
identifying the macrosomic fetus: Improving ultrasonography-based prediction. Am J Obstet Gynecol
182:1489-1495, 2000
141. Wong SF, Chan FY, Cincotta RB, et al: Sonographic
estimation of fetal weight in macrosomic fetuses: Diabetic versus non-diabetic pregnancies. Aust N Z J Obstet Gynaecol 41:429-432, 2000
142. Sylvestre G, Divon MY, Onyeije C, et al: Diagnosis
of macrosomia in the postdates population: combining sonographic estimates of fetal weight with glucose challenge testing. J Matern Fetal Med 9:287-290,
2000
143. Gilby JR, Williams MC, Spellacy WN: Fetal abdominal
circumference measurements of 35 and 38 cm as predictors of macrosomia. A risk factor for shoulder dystocia. J Reprod Med 45:936-938, 2000
144. Holcomb WL Jr, Mostello DJ, Gray DL: Abdominal
circumference vs. estimated weight to predict large for
gestational age birth weight in diabetic pregnancy. Clin
Imaging 24:1-7, 2000
145. Chauhan SP, West DJ, Scardo JA, et al: Spartanburg
Antepartum detection of macrosomic fetus: Clinical
versus sonographic, including soft-tissue measurements. Obstet Gynecol 95:639-642, 2000
146. Winn HN, Holcomb W, Shumway JB, et al: The neonatal bisacromial diameter: A prenatal sonographic evaluation. J Perinat Med 25:484-487, 1997
147. Riska A, Laine H, Voutilainen P, et al: Estimation of
fetal shoulder width by measurement of humerospinous distance by ultrasound. Ultrasound Obstet Gynecol 7:272-274, 1996
148. Kastler B, Gangi A, Mathelin C, et al: fetal shoulder
measurements with MRI. J Comput Assist Tomogr 17:
777-780, 1993
149. Verspyck E, Goffinet F, Hellot M, et al: Newborn
shoulder width: A prospective study of 2222 consecutive measurements. Br J Obstet Gynaecol 106:589-593,
1999
150. Gonen R, Spiegel D, Abend M: Is macrosomia predictable and are shoulder dystocia and birth trauma preventable? Obstet Gynecol 88:526-529, 1996
151. Watson WJ, Soisson AP, Harlass FE: Estimated weight of
the term fetus. Accurracy of ultrasound vs. clinical examination. J Reprod Med 33:369-371, 1988
152. Raman S, Urquhart R, Yusof M: Clinical versus ultrasound estimation of fetal weight. Aust N Z J Obstet
Gynaecol 32:196-199, 1992
�22
Abnormal Fetal Growth
153. Chauhan SP, Lutton PM, Bailey KJ, et al: Intrapartum
clinical, sonographic and parous patient’s estimation
of newborn birth weight. Obstet Gynecol 79:956-958,
1992
154. Chauhan SP, Hendrix NW, Magann EF, et al: Limitations of clinical and sonographic estimates of birth
weight: Experience with 1034 parturients. Obstet Gynecol 91:72-77, 1998
155. Sohaey R, Nyberg DA, Sickler GK, et al: Idiopathic
polyhydramnios: Association with fetal macrosomia.
Radiology 190:393-396, 1994
156. Benson CB, Coughlin BF, Doubilet PM: Amniotic fluid
volume in large-for-gestational age fetuses of nondiabetic mothers. J Ultrasound Med 10:149-151, 1991
157. Lazebnik N, Hill LM, Guzick D, et al: Severity of polyhydramnios does not affect the prevalence of large-forgestational-age newborn infants. J Ultrasound Med 15:
385-388, 1996
158. Owen P, Osman I, Farrell T: Is there a relationship
between fetal weight and amniotic fluid index? Ultrasound Obstet Gynecol 20:61-63, 2002
159. Andres RL, Day MC: Perinatal complications associated
with maternal tobacco use. Semin Neonatol 5:231-241,
2000
�
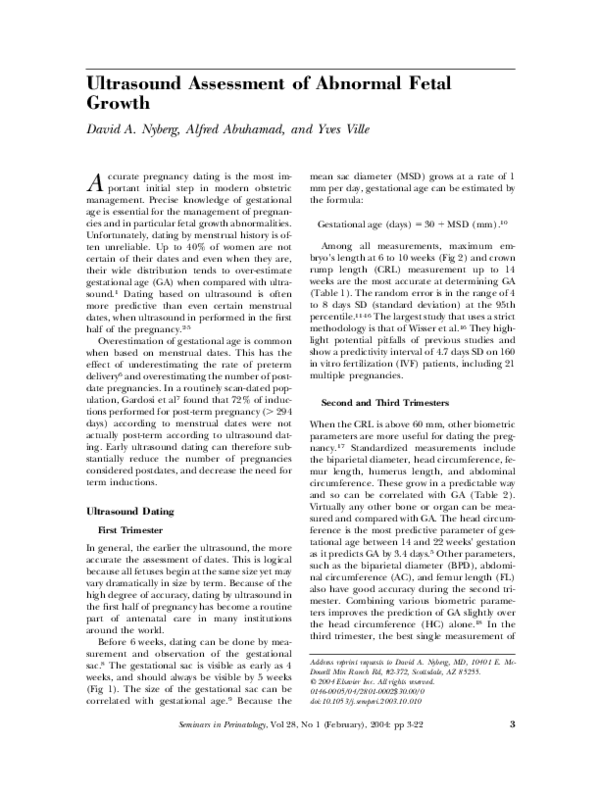
 Alfred Abuhamad
Alfred Abuhamad