Hindawi Publishing Corporation
Pain Research and Treatment
Volume 2012, Article ID 263972, 22 pages
doi:10.1155/2012/263972
Review Article
Review of the History and Current Status of Cell-Transplant
Approaches for the Management of Neuropathic Pain
Mary J. Eaton,1 Yerko Berrocal,2 Stacey Q. Wolfe,3 and Eva Widerström-Noga1, 4
1 Miami
VA Health System Center, D806C, 1201 NW 16th Street, Miami, FL 33125, USA
of Cellular Biology and Pharmacology, Herbert Wertheim College of Medicine, Florida International University,
Miami, FL 33199, USA
3 Department of Neurosurgery, Tripler Army Medical Center, 1 Jarrett White Road, Honolulu, HI 96859, USA
4 The Miami Project to Cure Paralysis, Miller School of Medicine at the University of Miami, Miami, FL 33136, USA
2 Department
Correspondence should be addressed to Mary J. Eaton, meatonscience@gmail.com
Received 8 March 2012; Accepted 9 April 2012
Academic Editor: Steve McGaraughty
Copyright © 2012 Mary J. Eaton et al. This is an open access article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Treatment of sensory neuropathies, whether inherited or caused by trauma, the progress of diabetes, or other disease states, are
among the most difficult problems in modern clinical practice. Cell therapy to release antinociceptive agents near the injured
spinal cord would be the logical next step in the development of treatment modalities. But few clinical trials, especially for chronic
pain, have tested the transplant of cells or a cell line to treat human disease. The history of the research and development of useful
cell-transplant-based approaches offers an understanding of the advantages and problems associated with these technologies, but
as an adjuvant or replacement for current pharmacological treatments, cell therapy is a likely near future clinical tool for improved
health care.
1. Introduction
The transplantation of cells into the CNS for therapeutic purposes can be envisioned with increasingly demanding goals
in mind: (1) local and sustained provision of therapeutic
molecules, such as pharmacologic agents and neurotrophic
factors; and (2) replacement of lost cellular populations and
reconstruction of local neuronal circuitry. To a large extent,
the demands of the particular therapeutic application will
be the key factor in determining the goals of the transplant
paradigm, and this guides both the selection of optimal cell
type(s) and parameters (graft dose, site, timing, immunosuppressive regimen, etc.) for transplantation. With this in
mind, the current review will explore the wide variety of
approaches in neural transplantation that have been explored
for the therapeutic management of pain. Since the goals of
pain management can be widely disparate, approaches have
evolved along distinctive paths during the progression of this
field. Thus, while the provision of a local cellular source
of biologic, rather than pharmacologic analgesic molecules
may be appropriate in the management of some etiologies of
new-developing neuropathic pain, cases of chronic, persistent neuropathic might require more heroic measures including replacement of lost neural populations and reestablishment of appropriate neurocircuitry. Nevertheless, some
overlap in the goals of these requirements can be envisioned,
for example, the provision of neurotrophic or neuroprotective molecules for the attenuation of hyperexcitability in
acute pain or replacement of lost inhibitory neurocircuitry in
chronic pain. Thus, this review will examine the history and
development of the various cell types and paradigms, which
run the gamut from primary tissue fragments to engineered
stem cell lines, that have been taken in various models of
chronic pain in order to identify breakthrough approaches
in the treatment of these debilitating conditions.
During the past three decades, cell therapy as an
approach to treat pain has progressed from a hypothesis for
a method for modulating pain processing to the development
of the first human cell sources that are being tested in clinical
pain treatment. The near future will likely provide new
�2
challenges for the implementation in a wider audience of
those who suffer chronic pain, considering problems common to all forms of cell transplantation, that is, immune
rejection versus long-term survival and efficacy in the
human host; dependable, well-characterized cell sources for
grafts; cells that can safely integrate into or near the CNS,
without danger of tumors or significant, deleterious effects;
the ability to control the antinociceptive output of cell grafts,
ideally increasing with the cyclic episodes of pain efficacy
in a wide variety of pain causalities. However, cell therapy
for pain offers much promise as a replacement or adjunct
to current clinical methodologies, once the mechanisms of
pain are well understood, so that such bioengineered cellular
tools can be used appropriately. Although it is likely that the
majority of the cell types grafted thus far are functioning
much like a cellular minipump, providing neuroprotective
and neurotrophic agents in the damaged CNS, more studies
to implement lost neuronal circuitry to modulate pain need
to be accomplished. Future studies will likely better define
the processes and mechanisms that will lead to improved
selection of cell types and trophic agents which can be utilized in combination to provide improved therapeutic outcomes following disease and injury to the nervous system
that leads to debilitating pain.
2. Problem of Chronic Neuropathic Pain in
Various Disease States and PNS/CNS Injuries
The treatment of neuropathic pain is perhaps one of the most
difficult problems in modern clinical practice. In addition to
affecting a large population, it is a staggeringly heterogenous
diagnosis with multiple etiologies which respond in varied
manners to a myriad of treatments. Current pharmacologic
treatments often prove ineffective, must be used at impractical dose levels, or have unacceptable side effects.
While the prevalence of neuropathic pain had previously
been conservatively estimated at 0.6% of the U.S. population
[1], better definition, understanding and recognition of this
diagnosis has led to a more realistic prevalence of 7-8%,
recently reported in Europe [2, 3]. A recent review by the
Neuropathic Pain Special Interest Group of the International Association for the Study of Pain (IASP) estimated
the overall prevalence of neuropathic pain at 3.3 to 8.2%
[4]. However, due to the large variation in reported prevalence and incidence, they also recommended further
research efforts regarding the development of standardized
methods for identification and assessment of neuropathic
pain. Neuropathic pain usually presents with allodynia, pain
felt in response to a normally innocuous stimulus, and
hyperalgesia, increased sensation of suprathreshold nociceptive stimuli [5]. It is often associated with uncomfortable
dysesthesias and may have continuous and paroxysmal components.
3. Etiologies
Neuropathic pain may result from disorders of the central
nervous system, the peripheral nervous system, or may be
Pain Research and Treatment
mixed. Nearly any traumatic event or disease leading to
neuronal damage, or neuropathy, has the potential to cause
neuropathic pain. Causes of neuropathy include trauma,
vascular and metabolic disorders, infections, neoplasms, toxins, autoimmune disease, as well as genetic and nutritional
deficiencies. As the individual causes of neuropathic pain
are seemingly innumerable, we will mention only the more
common etiologies.
Trauma, usually in the form of spinal cord injury and also
due to direct peripheral nerve damage, is one of the leading
causes of severe neuropathic pain [6]. Traumatic neuropathic
pain affects nearly 60% of individuals with spinal cord injury
[5]. Neuropathic pain is most common at or below the level
of injury and is often diffuse and poorly localized [7], making
this type of pain difficult to deal with for the individuals with
SCI [8]. Few treatments are effective and most individuals
have to continue to leave with persistent pain [9]. While there
are several pharmacologic agents that have shown success in
clinical trials [10], the side effects are often ill tolerated at the
dosages needed for relief.
One of the most common peripheral causes of neuropathic pain is diabetes. Diabetes mellitus is one of the
most prevalent diseases in the United States, affecting 25.8
million (8.3% of the population) [11]. Nearly 70 percent
of those with diabetes have diabetic peripheral neuropathy,
which can lead to severe neuropathic pain of the distal
extremities.
There are many infectious causes of peripheral neuropathy, including viral and bacterial etiologies. Viral infections
are more common and usually result in more severe neuropathic pain. They include herpes varicella-zoster (shingles),
Epstein-Barr virus, cytomegalovirus, and herpes simplex.
The human immunodeficiency virus (HIV) can cause several
different forms of neuropathy, including a rapidly progressive, painful polyneuropathy affecting the distal extremities
which is often the first clinically apparent sign of HIV infection [12]. Lyme disease, diphtheria, and leprosy are bacterial
diseases characterized by extensive peripheral nerve damage.
Neoplasms can create neuropathic pain due to direct nerve
compression and/or infiltration. While in a pure sensory
nerve, these may be surgically resected; cases involving motor
nerves or plexi are not amenable to surgical therapy and
must be managed by pharmacologic or neuromodulatory
treatments. Radiation, certain chemotherapeutic agents, and
paraneoplastic syndromes can also result in peripheral neuropathy.
Toxins can result in a heterogeneous group of peripheral
neuropathies. Those exposed to heavy metals, such as arsenic, lead, mercury, thallium, or industrial toxins, as well as
certain therapeutic drugs in the anticonvulsant, chemotherapeutic, antiviral, and antibiotic classes, can also cause
peripheral neuropathy and neuropathic pain. Nutritional
deficiencies, in particular thiamine deficiency due to its
prevalence amongst alcoholics, may also result in peripheral
neuropathy. Trigeminal neuralgia is an excruciating cause
of facial pain but is usually amenable to surgical vascular
decompression of the nerve. Central neuropathic pain can
be caused by multiple sclerosis and certain stroke syndromes
[13]. Genetic and autoimmune neuropathies are rarer but
�Pain Research and Treatment
add to the overall population of those with neuropathic
pain.
4. Treatment
Given the widely diversified causes of central and peripheral
neuropathy that can lead to neuropathic pain, it becomes
much clearer as to the difficulty in treating this diagnosis.
Clearly, the underlying condition is treated first, followed
by symptomatic treatment of the pain. Unfortunately, only
a dismal 40–60% of patients with neuropathic pain achieve
partial relief. A significant roadblock of the treatment
dilemma has been the difficulty with the most appropriate
animal model to use for basic research, as well as the disconnect between behavioral outcomes examined in animal
studies and those reported in the presentation of pain in a
clinical setting [14].
In an effort to clarify the existing therapeutic paradigm
for neuropathic pain, recent guidelines have been derived
for pharmacological therapy [15–18]. These have combined
evidence from randomized controlled trials with expert
opinion and currently offer the clearest treatment paradigm.
While certain drugs work best for specific indications, likely
due to the mechanism of that disease etiology, it is becoming
clearer that a combination of pharmacologics, adjuvant
treatment and neuromodulation are usually needed to attain
adequate pain relief [19–21].
Despite multiple therapeutic options, the treatment of
neuropathic pain remains difficult and inconsistent. While
combination therapy and an increasing number of adjunct
therapies assist in treating intractable pain, there still remains
no cure. Pain despite standard treatment due to poor efficacy, unacceptable side effects, and disease escalation demand continued investigation and development of new technologies to treat neuropathic pain.
5. Pain Classification
In the clinical setting, a broad classification of pain is made
in order to differentiate between nociceptive and neuropathic
pain types. This is a critical distinction because these pain
types are dependent on partly different underlying mechanisms, and therefore, they usually require different treatment
strategies. Arriving at an accurate neuropathic pain diagnosis
is not straight forward, and this problem has been recognized
both in pain research and in clinical pain management settings. To address this problem, the International Association
for the Study of Pain (IASP) has proposed a modification
of the present pain taxonomy. Neuropathic pain is currently
defined as “pain initiated or caused by a primary lesion or
dysfunction in the nervous system” [22]. However, Treede
and colleagues [23, 24] recently suggested eliminating “dysfunction” from the definition and instead redefine the neuropathic pain definition to “pain arising as a direct consequence
of a lesion or disease affecting the somatosensory system.”
In order to standardize the classification into neuropathic
and nonneuropathic pain, they recommended differentiating
pain into “definite,” “probable,” and “possible” neuropathic
pain. The following criteria were proposed to be required for
3
“definite” neuropathic pain: (1) pain distribution consistent
with injury to the peripheral nervous system (PNS) or the
central nervous system (CNS); (2) history of an injury or
disease affecting the PNS or CNS; (3) abnormal sensory signs
within the body area corresponding to the injured area of
the CNS or PNS; (4) a diagnostic test confirming a lesion or
disease in these structures.
These criteria are applicable to many neuropathic pain
conditions. However, in conditions with multiple concomitant pain types after CNS injuries, such as in SCI-related
pain, distinguishing between neuropathic and nociceptive
pain may be more difficult when pain is located in an area
below the lesion but with partial sensory preservation. For
such pain locations, abnormal sensory findings may not
indicate a neuropathic pain diagnosis, since these will be
present in the painful area regardless of whether pain is
nociceptive or neuropathic [25].
Basic research studies have identified multiple underlying
mechanisms of neuropathic pain and designed interventions
to target them. However, significant knowledge gaps exist
regarding the best methods to characterize pain subgroups
(phenotypes) and their relationship to the underlying pain
mechanisms in pain patients. A precise diagnosis is critical
to the development of more effective treatments that are
tailored to specific underlying mechanisms. Because neuropathic pain is dependent on multiple mechanisms [26], this
knowledge gap is a significant barrier to translation of basic
research finding into successful management of neuropathic
pain.
The determination of clinical pain phenotypes is a promising way to classify pain types. This process may include
statistical grouping of pain characteristics [27]. For example, a combination of the descriptive adjectives “burning,”
“tingling,” “pricking,” “shooting,” and “freezing” pain, and
evoked pain, differentiated between neuropathic and nonneuropathic pain in 618 patients with diabetic neuropathic
pain, idiopathic neuropathic pain, or post-herpetic neuralgia
or nociceptive osteoarthritis pain, or low back pain [28].
Another method used for defining clinical pain phenotypes
includes quantitative sensory testing (QST; [29, 30]). Measurement of detection thresholds for tactile stimuli determines large-fiber and dorsal column-mediated function, and
thermal detection and pain thresholds determine small-fiber
and spinothalamic tract-mediated function. Thus, QST may
facilitate the comparisons with basic research studies, since
these studies often assess behavioral, evoked nociceptive responses.
6. Potential Strategies for Cell-Based
Interventive Therapies: Rationale
6.1. Cellular Minipumps for Treatment of Pain. The earliest
studies using cell transplants for pain were originally developed from the concept of descending inhibitory neurotransmitter modulation of sensory information [31], and
that these same agents, such as catecholamines and opiates,
released by cell grafts [32–36] after injury, could provide
antinociception. Projections from midbrain, locus ceruleus, ventromedial, and ventrolateral medulla directly or
�4
indirectly terminate at spinal level to modulate incoming
nociceptive signals. In addition, dorsal horn interneurons
provide inhibitory influences at the same termini. A variety
of neurotransmitters, peptides, opioids, and lately neurotrophins, such as BDNF, have been implicated in spinal inhibition. These include the endogenous neurotransmitters serotonin (5HT), noradrenaline, and gamma-aminobutyric acid
(GABA); the endogenous opioids ß-endorphin, enkephalins,
cannabinoids; endogenous peptides such galanin, and neurotrophins such as BDNF. Many of the commonly used
pharmacologic therapies target these agents’ receptors and
reuptake mechanisms to increase or imitate their presence
in acute and chronic pain. But it was recognized as early
as 1980s [36] that these agents could be supplied by grafts
of autologous adrenal medullary tissue [37] or chromaffin
cells [38] which had been purified from adrenal tissue, and
transplanted in a chronic arthritic pain model [39], after
nerve transection [40], or peripheral nerve injury and painful
neuropathy [41, 42] to attenuate behavioral hypersensitivity.
Where a similar strategy using pharmacological agents
and mechanical intrathecal delivery might be considered,
intrathecal and/or intra administration cerebroventricular of
opioids is limited by cost, the need for specialized maintenance and mechanical malfunctions if implantable drug
delivery systems, or by the risk of bacterial contamination
and ambulatory constraints when repeated daily injections
via an intrathecal access port are used [43]. Intrathecal cell
therapy secreting these same antinociceptive agents can be
seen as an advantage. Since it was also noted that minimal
immunosuppression was all that was required for good graft
function and survival in the immune-protected nervous
system [44], such studies led to the early initiation of clinical trials for chronic cancer pain with this cell transplant
approach [42, 45, 46].
Pain Research and Treatment
7. Early Use of Cell Therapy
reduction in the c-fos induction by formalin in the presence
of chromaffin grafts [57], probably by stimulating some
persistent cellular process, such as increasing the descending
inhibitory controls that regulate the firing of subpopulations
of spinal cord nociresponsive neurons with release of opioids
from grafted chromaffin cells, inhibitory modulation that
may be an important determinant, but not the only one,
of their analgesic effect [58]. To be able to use chromaffin
cell therapy in humans, adrenal chromaffin cell grafts were
prepared from xenogenic bovine sources and tested for
antinociception after nerve injury [35, 59]. Such sources of
primary bovine chromaffin cells have been safely used in
initial trials with human patients with intractable cancer pain
[60, 61]. But such primary tissue sources for the purification
and use of chromaffin cells are not likely to be homogeneous,
since they are often obtained from multiple donors. The
ability to use and manipulate cell lines as a defined and stable
source would be an alternate for eventual use in cell therapy.
Adult human chromaffin tissue has also been transplanted in humans for cancer pain [62], but when the
immune response in the human host is examined after
human chromaffin grafts, one conclusion is that further purification and/or the immunoisolation of tissues grafted in
the CNS will be necessary when using these primary adult
human adrenal sources, particularly when the possibility of
long-term and repeated grafting is considered [63]. However,
there are recent reports [64] of successful human fetal
adrenal transplant to treat pain associated with rheumatoid
arthritis, and in a rat model of partial nerve injury [65],
certainly suggesting that fetal or precursor chromaffin tissue
could be used as an antinociceptive source [66, 67]. But using
such primary tissue sources for the further purification [68]
for successful cell therapy necessitates immunosuppression
of the human host, such that examination of encapsulation
technologies of grafted cells continued in many rat and
human studies (Figure 1).
7.1. Primary Adrenal Chromaffin Tissue and Cells. Some
of the earliest studies utilized primary chromaffin cells in
a rat model of neuropathic pain [41]. Chromaffin cells
contain a cocktail of antinociceptive agents, peptides, and
neurotrophins [47, 48]. These chromaffin cell grafts were
placed either in midbrain structures [38], or in the lumbar
subarachnoid space after partial chronic constriction injury
(CCI) to the sciatic nerve [42], or after injection of formalin
in the rat’s hindpaw [49] for the antinociceptive effect. Many
studies have sought to elucidate the agents released by these
chromaffin grafts that might serve an antinociceptive role.
These primary chromaffin cells grafts raise the levels of CSF
met-enkephalin [32], increase CSF levels of catecholamines
[50], and reduce morphine cross-tolerance [51] when
used with morphine for pain. Changes in the spinal cord
induced by nerve injury are attenuated by chromaffin grafts,
such the induction of spinal NADPH-diaphorase [52] and
cGMP [53], spinal c-fos induction [54], NMDA-induced
hypersensitivity [55], and the loss of endogenous inhibitory
GABA synthesis in the dorsal horn [56] that accompanies
nerve injury. It is likely that adrenal transplants also block
short-term spinal nociceptive facilitation, illustrated by the
7.2. Clinical Trials Utilizing Cell Therapy for Neuropathic
Pain. As mentioned above, cell therapy utilizing intrathecal
adrenal chromaffin grafts to treat cancer pain was initiated
in the early 1990s [41, 46, 61], which reported long-lasting
pain relief, in correlation with met-enkephalin release into
the CSF [43]. Typically not all late-stage cancer patients
respond well to systemic opioids for pain management,
with adverse effects and poor pain control [69], and hence
requiring intrathecal delivery. The efficacy of this cell therapy
technique depends on the ability of those cells to produce
analgesic opioids and on the immuno-privileged property
of the central nervous system, in which rejection risks are
limited [70]. Before inclusion in an open Phase II trial, all the
cancer patients to be grafted with human chromaffin cells
had their pain controlled by daily intrathecal (I-Th) morphine administration. Out of the 12 patients who profited
from enhanced analgesia with long-term followup (average
4.5 months), five no longer required the I-Th morphine
(with prolonged interruption of systemic opioids as well),
two durably decreased I-Th morphine intake, and five were
stabilized until the end of their followup. Durable decline and
�Pain Research and Treatment
5
are often obtained from multiple donors. The ability to use
and manipulate stable antinociceptive cell lines as a defined
source has provided a rich literature for their experimental
use in cell therapy (Table 1).
8. Strategies for the Creation of Immortalized
Cell Lines: Rationale/Studies
(a)
(c)
(b)
Figure 1: Model of lumbar subarachnoid injection of human
neurons near the human spinal cord. MRI image of the human
spinal cord (a) with a lumbar puncture of the subarachnoid
space adjacent to the cord (b), and injection of cells, such as the
GABAergic human neuronal hNT2.17 cells (c) for pain relief, as
delivered by syringe (d). A similar technique has been used in all
pre-clinical animal experiments and clinical studies with human
chromaffin cell injections for pain.
stabilization were interpreted as indicative of analgesic activity by comparison with the usual dose escalation observed
during disease progression, related to increased CSF metenkephalin levels associated with the grafts [71]. The grafts
were tolerated, and there is evidence of long-term survival
[72], despite the presence of CSF lymphocytes, where single
treatment failure and three of four cases of partial efficacy
occurred in grafts where CSF lymphocytes were present,
indicating that impairment of the local immunosuppressive
balance can lead to activation of host CSF CD4 T cells and
drive a rejection process when grafts are not encapsulated
[63]. It was concluded that graft immunoisolation, by using
cell encapsulation, seems to be unavoidable in spite of the
graft site [70]. Such ultimately failed clinical trials provided
a better understanding of the limits (at that time) for this
approach [43, 62, 72, 73]. Adult human chromaffin tissue has
also been transplanted in humans for cancer pain [62], but
when the immune response in the human host is examined
after human chromaffin grafts, one conclusion is that further
purification and/or the immunoisolation of tissues grafted
in the CNS will be necessary when using these primary adult
human adrenal sources, particularly when the possibility of
long-term and repeated grafting is considered [63]. However
there is a recent report [64] of successful human fetal adrenal
transplant to treat pain associated with rheumatoid arthritis,
certainly suggesting that fetal or precursor chromaffin
tissue could be used as an antinociceptive source [66]. But
such primary tissue sources for the purification and use of
chromaffin cells are not likely to be homogeneous, since they
8.1. Naturally Occurring (Tumor) Cell Lines. A cell line has
the ability to be expanded in vitro, is stable enough in its
phenotype to be characterized in vitro and after grafting; and
can be used for in vivo transplant. The archetypal adrenal
medullary cell line is the rat PC12 cell line, first established
from a transplantable rat adrenal pheochromocytoma
[74], which was shown to respond to NGF with reversible
loss of mitotic activity and differentiation to a neuronal
phenotype. This natural, oncogenic cell line has been used
as a model to bioengineer the addition of the gene [75] for
the analgesic [76] peptide histogranin (SHG) which acts as
an antagonist for the excitatory NMDA receptor, as SHG can
enhance the antinociceptive properties of grafted cells, such
as chromaffin transplants [77]. Although originally reported
to lack phenylethanolamine N-methyltransferase (PNMT)
and epinephrine synthetic capability [74], further characterization [78] suggests both PNMT activity and epinephrine
synthesis in PC12 cells. Although this cell line has often been
examined for its response to manipulation to agents, such as
morphine analogs important in pain modulation [79], it has
also been tested as a grafted catecholamine source to test cell
therapy for pain relief [80]. However, PC12 cells tend to form
tumors, rather than to integrate and release antinociceptive
agents. Grafts of the mouse B16 F1C29 melanoma cell line,
which also release catecholamines, was able to reduce pain
behaviors in the tail-flick model when accompanied by
morphine [81], but again, such grafts are tumorigenic, and
their transplant can itself induce pain behaviors [82]. The
monaminergic human NB69 neuroblastoma cell line was
able to reduce neuropathic pain in a nerve injury model
[83], presumably related to serotonin release from the grafts,
but the tumorigenic potential is a consideration with a nondifferentiated tumor line. Other studies with implantation
of tumor-derived cell lines, like AtT-20 or AtT20/hENK
[84], Neuro2A [85], Neuro2A/POMC [86], or P19 [87], that
overexpress opioid peptides have been attempted, but such
grafts would also carry the risk of tumor formation.
Although the ability of opioids to provide pain relief
with SCI remains controversial, the release of enkephalin-like
molecules from genetically modified cell grafts, such as AtT20/ENK cells, as therapeutic was an early strategy [84, 88].
One goal of such a opioid-based strategy would be to reduce
the side-effect of tolerance that develops with morphine and
its analogs [84] (Table 2).
8.2. Conditional Immortalization to Create Cell Lines. Retroviral infection of neural precursors, when cells are actively
proliferating, with an immortalizing gene sequence in vitro,
is a strategy applicable to a variety of cell types that
might be useful for transplantation [89], and especially the
neural phenotype with v-myc [90] or the wild-type SV40
�6
Pain Research and Treatment
Table 1: Primary tissue used for cell therapy.
Source
Pain model
Primary cells/tissue:
Adrenal-rat
[49, 57, 58, 219, 245–249]
Bovine
[35, 59, 247, 250–254]
Encapsulated bovine
[247, 255–258]
bovine scaffolds [259]
Porcine
[253, 254, 260–262]
Encapsulated porcine [262]
Human
[62, 67, 71, 263, 264]
Human encapsulated [67]
Acute [247]
Midbrain [38]
Formalin [54, 58, 247, 249,
253, 260, 261]
Nerve injury
[46, 57, 67, 256, 262]
Dorsal rhizotomy [246]
Excitotoxic SCI
[219, 255, 265]
Hemisection SCI [245]
Human Cancer
[64, 71, 266, 267]
Arthritis [56, 65, 268]
Results
(i) Reduced “excessive grooming” behaviors [219]
(ii) Reduction or stabilization in complementary opioid intake in human
cancer [71]
(iii) Reductions in both fore- and hindlimb mechanical and thermal allodynia
[245]
(iv) Failed antinociception after intraventricular transplant [256]
(v) Reduces edema, anterograde axoplasmic transport [249]
(vi) Restores spinal GABA-ir decreased spinal c-Fos [58, 253]
(vii) Failed antinociception [247, 247, 269–271]
(viii) Reduced cold or TA/TH behaviors [67, 219, 262]
(ix) Reduced tonic pain behaviors [261]
(x) Delayed, reduced self-directed pain behaviors [246]
(xi) Antinociceptive effects on A-delta and C-fiber-mediated responses [59]
(xiii) Long-term proenk and tyrosine hydroxlylase in grafts [248]
(xiv) Reduce forelimb/hindlimb allodynia [245]
Table 2: Naturally occurring (tumor) cell lines.
Source
Tumor Cell Lines:
Rat PC12 [74]
Encapsulated PC12 [272]
Mouse B16 [81]
Human NB69 [83]
AtT-20 [84, 273]
Encapsulated AtT-20 [85],
Neuro2A [85]
Encapsulated Neuro2A [1327]
P19 [87],
Bio-engineered—AtT-20/hENK [84, 273]
Encapsulated Neuro2A/POMC [86]
Autologous rat macrophages/proENK [274]
PC12/SHG peptide [75]
Pain model
Results
Tail-flick or chemical
induction
[81, 84, 85, 87, 88]
Acute [81, 84, 85, 88, 273]
Partial nerve injury (CCI)
[83, 272, 274]
Formalin [87]
(i) Analgesic [85, 88]
(ii) Reduced opioid tolerance [84]
(iii) Antinociceptive [81, 83, 84, 273, 274]
(iv) Reduced cold allodynia [83, 272]
Tail-flick or chemical
induction [84, 273]
Formalin [75]
(i) Increased ACTH release with TET-ON stimulation [86]
(ii) Reduced Phase II formalin-induced responses [75]
large T temperature-sensitive antigen (tsTag) oncogene [91].
Immortalization with tsTag can result in cell lines capable of
undergoing proliferation at permissive temperature (33◦ C)
and differentiation under appropriate temperature conditions (nonpermissive; 39◦ C) [92, 93]. Infection of precursors
with the temperature-sensitive allele of Tag (tsTag) in vitro
[94] and in vivo [95] has allowed cells to undergo growth
arrest and continue differentiation under nonpermissive
temperature (39◦ C) conditions. These differentiating temperatures are possible both in vitro, allowing transformed
cells to revert to a near-normal primary cell phenotype, as
well as in vivo, where CNS transplant temperatures are near
39◦ C [96], and tumors are not formed because the immortalizing gene is not expressed. Thus, conditional immortalization with the oncogenic tsTag construct incorporates the
advantages of cell lines, including the convenience of growing
large quantities that can be characterized and safety tested
and the ability to also genetically engineer-in the expression
of additional therapeutic molecules, while reducing the
disadvantages of tumor cell lines.
Though describing engineered-cell grafts as “biological
minipumps” for secretion of neurotrophic or antinociceptive agents has only been recently discussed [97, 98], the
practicality has been examined for at least the last 25 years
[99, 100]. But, the same strategy, using engineered cells that
might secrete potentially antinociceptive molecules when
placed in the lumbar subarachnoid space after PNS or CNS
injury, much like the primary adrenal chromaffin cells and
opioid cell lines described above, has seen few applications
for use in chronic pain [81, 84]. But the potential application
of such cell line grafts for the diverse problems with neuropathic pain in human therapy is significant [101], given the
paucity of homogeneous primary tissue. Unlike primary or
immortalized chromaffin cells, the engineered cells being
tested in a variety of models of acute and chronic pain
were initially neuronal epithelial precursor cell lines derived
from the rat medullary raphe. Two lines that have been
bioengineered, called RN46A, and RN33B were isolated
from embryonic day 12.5 (E12.5) rat brainstem after immortalization with the SV40 tsTag sequence [102, 103].
Although they were derived from the same primary cultured
neuronal precursors, there are significant differences in their
phenotypes: RN46A cells are an early serotonergic precursor
neuronal cell line, with the potential to switch developmental
phenotype [102], depending on the timing and exposure
to a variety of neurotrophic and other factors, including
�Pain Research and Treatment
BDNF [104], CNTF [105], GDNF [106], and ACTH [107].
This cell line was made to synthesize and secrete the neurotrophin BDNF, by the addition of the sequence for rat BDNF
to its genome, causing the cells to have improved survival
in vitro and in vivo, and develop a permanent serotonergic
(5HT) phenotype [108]. Since additional 5HT might be postulated to have a beneficial antinociceptive effect on neuropathic pain [109] differentiated cells were placed in a lumbar
subarachnoid location after sciatic nerve chronic constriction injury (CCI). Transplants of this serotonergic cell line
46A-B14, placed two weeks after CCI and the development
of severe hypersensitivity to thermal and tactile stimuli were
able to potently and permanently reverse the symptoms of
neuropathic pain [110], compared to grafts of the same cells
which did not receive the BDNF gene and did not synthesize 5HT in vitro or in vivo. Transplants of other cell
lines genetically engineered to synthesize and secrete potentially antinociceptive molecules such the inhibitory peptide
galanin [111], the neurotrophin BDNF [112], and the inhibitory neurotransmitter GABA [113] have all been tested
after CCI and the induction of neuropathic pain, and each
has reversed the thermal and tactile allodynia and hyperalgesia that develop after CCI. Each engineered cell line is
characterized for its particular gene expression under permissive and nonpermissive temperature conditions, since the
cell lines are usually transplanted immediately after proliferation at 33◦ C. Following placement of the differentiating
cells in the subarachnoid space, especially in models of
pain, both cell graft survival and continued expression of
the antinociceptive phenotype were examined in vivo. An
example of such an engineered rat neuronal cell line, the
RN33-GAD67, which synthesizes and secretes GABA after
differentiation in vitro and transplant in vivo [113] in the CCI
pain model, where GABA is synthesized after differentiation
in these cells. But such an effect for neuropathic pain seems
to require an early transplant time, since grafts of these rat
neuronal GABA cells are less effective when placed late after
nerve injury [114]. With both types of behavioral hypersensitivity, thermal and tactile hyperalgesia, rat GAD67 grafts
cause immediate reversal of hypersensitivity when the behaviors are measured one week later. Such potent reversal is
common to each of the engineered cell lines used for therapy
after partial nerve injury models, and more recently with
SCI models [115–118], especially thermal hyperalgesia. But
using the CCI model of neuropathic pain and near-identical
transplant numbers and experimental conditions for all these
studies has identified the rat GABA- and 5HT-cell lines as
especially efficacious, since attenuation of hypersensitivity
is more potent and permanent in the presence of these
graft phenotypes, although early transplant time seems to be
favored in the CCI model [119]. But other antinociceptive
cell types have also been conditionally-immortalized to test
their usefulness in eventual clinical applications.
Mitotic cells found in embryonic medullary adrenal
tissue can also be conditionally immortalized with the tsTag
oncogene so that the differentiated cell type keeps many
of the phenotypic features of primary chromaffin cells.
Conferring immortalization with the SV40 large T antigen
expression has a variety of effects on cells when the wild-type
7
large T protein is present, including binding of large T and
inactivation of the growth suppressors pRB, p53, and SEN6
[120, 121], a decrease in G1 and increase in G2 and M cell
cycle phase duration [122], and the ability of large T antigen
to block the differentiation process [123]. However, after
immortalization with the temperature-sensitive allele tsTag
[94, 124], immortalized cells resume the stage of life span
and function of an uninfected cell when they are shifted to
nonpermissive temperature conditions [125]. These cells at
the nonpermissive temperature have lost the ability to drive
cell proliferation, since the large T antigen is labile at the
higher temperature conditions [126] and the T antigen is not
able to drive mitosis in cells immortalized with the construct,
and differentiation is favored [94, 124]. In general, SV40 large
T antigen-immortalized cell lines retain the phenotype of the
differentiated lineage of the parent. Cell lines generated with
the SV40 large T antigen retain contact inhibition in vitro
[127, 128] and do not produce tumors or induce immune
rejection even when injected into nude mice [129] or rats
[130–137].
Rat and bovine chromaffin cells immortalized with tsTag
in vitro [138] express many of the markers found in primary
chromaffin cells and when differentiated in vitro, as the oncogenic Tag protein is degraded and mitosis ceases, these markers remain and are able to be regulated by continued differentiation, by agents such as dexamethasone and by stimulation
of the cAMP pathway with forskolin, mechanisms seen in
primary chromaffin cells [138]. Such immortalized chromaffin cells are stable and appear homogeneous, suggesting that
they could be useful for further genetic manipulation and as
a source for transplant studies in vivo [139].
The cell biology and developmental responsiveness during differentiation of chromaffin cells [140] reveals clues to
the differentiation program of conditionally immortalized
chromaffin cell lines in vitro. The enzyme tyrosine hydroxylase (TH; EC1.14.3.x) catalyzes the rate-limiting step [141]
in the biosynthesis of catecholamines in chromaffin cells
in the adrenal medulla [142, 143] and has been used as
one of the antigenic markers for the mature chromaffin
phenotype of primary rat and bovine chromaffin cells in
vitro [144], as well as DβH and PNMT. Both the rat RAD5.2
and bovine BADA.20 chromaffin cell lines express these catecholamine enzyme immunoreactivities at both permissive
(low levels) and nonpermissive temperatures, when the cells
are proliferating or differentiating, respectively, though levels
of the DβH enzyme appears to change with differentiation
at nonpermissive temperature (39◦ C). Tyrosine hydroxylase
(TH) expression is not upregulated in the rat chromaffin
cell line but seems to be a feature of immortalized bovine
chromaffin cell in vitro [138]. But further increased catecholamine enzyme expression in the chromaffin cell lines
requires treatment with forskolin and/or dexamethasone
during differentiation, since differentiation at 39◦ C is in
serum-free medium [138]. Differentiated primary chromaffin cells from rat [145, 146] and bovine [34] sources have
often been used to study the synthesis and release of the
catecholamine neurotransmitters norepinephrine and epinephrine in vitro. However, even with upregulation of enzyme
expression, these conditionally immortalized chromaffin rat
�8
and bovine cells do not synthesize catecholamines under
in vitro conditions [138]. Since chromaffin cell lines probably require an adequate substrate interaction for a completely normalized chromaffin phenotype, the absence of
detectible catecholamine synthesis in differentiated RAD5.2
and BADA.20 cells may be due to removal from their fibroblast environment. Another possible, and more likely, explanation for the absence of catecholamine synthesis is a continued low level of Tag expression, even though it is greatly
reduced after three weeks of differentiation at 39◦ C. It is
possible that even a low level of Tag suppresses some normal
cellular functions, such as neurotransmitter synthesis.
This attempt at conditional immortalization of chromaffin cells using the tsTag oncogene and retroviral infection
in vitro, demonstrating continual cell lines retaining many
features of the mature chromaffin cell phenotype. The
availability of conditionally immortalized chromaffin cell
lines for a variety of studies, including their use as transplants in various models of neuropathic [139], reflects the
growing interest in the development of molecular biological
techniques of cellular therapy for treating neuropathic pain,
but further attempts to develop the immortalization technologies were needed.
8.3. Reversible Immortalization to Create Cell Lines. The ability to reverse immortalization in a tightly controlled manner
was the logical next step in the creation of cell lines from
rare phenotypes [147]. But such reversible-immortalized
cell lines that might be used for antinociception have been
little studied [148]. The generation of chromaffin cell lines,
utilizing the temperaturesensitive allele of SV40 large T
antigen (tsTag) are able to reverse neuropathic pain after
transplant in the spinal subarachnoid space after CCI of the
sciatic nerve [139]. Even with near 100% disappearance of
Tag in the grafts within a few weeks after transplant [139],
oncogene expression in vivo remains a potential possibility
and such cells would not be an appropriate strategy for safe
clinical use in humans.
Studies exploiting sitespecific DNA recombination and
Cre/lox excision have suggested that cells can be targeted in
vitro [149] and in vivo [150] for removal of deleterious genes,
including the Tag sequence [151]. Reversible immortalization with Tag and Cre/lox technology was first reported with
human fibroblasts by Westerman and Leboulch [152] and
more recently with human myogenic cells and hepatocytes
[153] and hepatic progenitors [154]. In these latter studies,
Cre was introduced by transfection or infection, inefficient
methods that may lead to a lack of disimmortalization and
the loss, through the subsequent selection of disimmortalized cells, of a significant part of the population. Moreover,
in vivo excision is not possible. Use of a vector that allows a
silent, but inducible, form of Cre is preferred for the timed
excision of the oncogene.
A number of chimeric Cre-containing fusion proteins,
especially fusions with the ligand-binding domains of steroid
receptors, have been created to utilize the binding by synthetic ligands to activate Cre [155]. CrePR1 is a fusion protein [156], consisting of the fusion of Cre and the ligand
binding domain of a mutant human progesterone receptor
Pain Research and Treatment
(hPRB891). Cre activity in the cells is activated by the binding of the steroid RU486, which in turn induces the translocation of CrePR1 to the nucleus where the Cre is active
to excise the floxed sequences. The requirement for RU486
and the use of a mutated steroid receptor for disimmortalization would assure that if nondisimmortalized cells
were transplanted, Cre would not be activated by circulating endogenous progesterone, a strategy used for inducible
recombination with in vivo CNS studies [157].
It has been demonstrated [158] that embryonic rat
adrenal chromaffin cells could be immortalized with a oncogenic tsTag construct, utilizing retroviral infection of these
early chromaffin precursors, where the tsTag construct (tsATN) was flanked by loxP sequences. Following isolation of
immortalized cells using positive neomycin selection, the
cells were further infected with a retrovirus expressing the
CrePR1 gene, which encodes a fusion protein which combines Cre activity plus the mutant human steroid receptor,
hPRB891. Cultures of embryonic rat adrenal cells were
immortalized with the tsA-TN retroviral vector encoding
the loxP-flanked temperature-sensitive allele of SV40 large
T antigen (tsA-TN), which included a positive/negative
neo/HSV-TK sequence for selection with either G418 or gancyclovir, respectively.
A number of chimeric Cre-containing fusion proteins,
especially fusions with the ligand-binding domains of steroid
receptors, have been created to utilize the binding by synthetic ligands to activate Cre [155]. CrePR1 is a fusion
protein [156], consisting of the fusion of Cre and the ligand
binding domain of a mutant human progesterone receptor
(hPRB891).
When immortalized chromaffin cells are disimmortalized with cre-lox technology to disimmortalize the chromaffin cells in vitro, complete removal of the Tag sequence
before differentiation seems to allow neurotransmitter synthesis and a more normal phenotype [158]. Compared to
downregulation of the tsTag protein in conditionally immortalized rat chromaffin cells, disimmortalization in vitro
in these disimmortalizable rat chromaffin cells, called the
loxtsTag/CrePR1/RAD chromaffin cell line, the Tag protein
was completely and efficiently removed by 10 days of treatment with RU486, followed by incubation with the antibiotic
gancyclovir [158]. Cells which were not disimmortalized,
were removed by their continued expression of the thymidine
kinase (TK), which is toxic in the presence of gancyclovir
[159].
Irreversible removal of a potentially subverting oncogene
by its excision using the Cre/Lox system might thus be a clinically useful strategy, especially since the core temperature
of humans is lower than that of rodents, and the expression
of a temperature-sensitive antigen might not be completely
blocked in a clinical context [152, 160–164]. Note that in this
respect, use of moduletable Cre activity that can be activated
by the synthetic steroid RU486 [156, 157] has added a means
to select the timing of disimmortalization and render the
overall procedure more flexible and efficient. Interestingly,
the disimmortalized rat chromaffin cells had very increased
expression of tyrosine hydroxylase (TH), the rate limiting
enzyme for catecholamine synthesis, in vitro. This was
�Pain Research and Treatment
9
Table 3: Strategies for creating cell lines.
Source
Model
Conditionally immortalized Cell lines:
Embryonic rat Raphe/SV40tsTag
[102, 103, 275–277]
Embryonic rat DRG neuron, 50B11
[90]
partial nerve injury
Human DRG neuron, HD10.6,
(CCI) [139]
v-myc [278]
Embryonic rat and bovine
Chromaffin [138, 139]
Human embryonic Chromaffin
cells/tsTag [279]
Bioengineered rat Raphe/tsTag/
BDNF [110, 211]
Rat raphe/tsTag/galanin [111]
Rat raphe/tsTag/GAD67 [113]
Rat chromaffin/tsTag/Met-ENK
[165, 170]
Results
(i) Expressed capsaicin receptor transient
receptor potential vanilloid family-1
(TRPV-1) and responded to capsaicin in
vitro [90]
(i) enkephalin? [279, 280]
(ii) Expressed sensory neuron-associated
transcription factors and exhibited capsaicin
sensitivity [278]
(iii) Antinociceptive [139]
(i) Antinociceptive
[84, 110, 113, 116, 119, 158, 211]
(ii) Restores dorsal horn GAD/GABA system
Partial nerve injury
in CCI [229]
(CCI) [84, 110, 113, 158, (iii) Only intrathecal, not intraspinal, grafts
211, 229]
of 5HT cells are antinociceptive [115]
Formalin/c-fos
(iv) Attenuates bilateral DH hypersensitivity
induction [170]
[117]
Hemisection SCI
(v) Restores spinal serotonin, downregulates
[115–118]
the serotonin transporter, and increases
BDNF tissue content [118]
(vi) Reduce formalin-evoked c-fos
expression [170]
Reversibly immortalized Cell Lines:
Tetracycline-regulated of SV40 large
T-antigen (Tag) in human embryonic Partial nerve injury
stem (ES) cells and mice [147]
(CCI) [158]
Cre/lox-regulated Disimmortalizable
Embryonic rat chromaffin cells [158]
Antinocicptive Molecule
Released
(i) Antinociceptive [158]
accompanied by 5-fold increase in norepinephrine synthesis
in vitro [158]. But these disimmortalizable rat chromaffin
cells not only synthesize epinephrine after Tag excision, but
they also apparently make increased catecholamine enzymes
besides TH, judged by qualitative immunohistochemistry
for the enzymes compared to both nonexcised and those
immortalized with only tsTag [138]. Also of importance,
transplant of disimmortalized rat chromaffin cells was able
nearly eliminate neuropathic pain in the CCI model of partial
nerve injury, when compared to the injury alone or transplant of immortalized chromaffin cells. Rather than suggesting that antinociception is the result of catecholamine
synthesis, release or secretion from grafted chromaffin cells,
the existence of an equivalent functional effect by nondisimmortalized cells suggests that another agent or mechanism is
responsible for reduction of neuropathic pain by these genetically manipulated chromaffin cells, at least in this model of
pain. Even if chromaffin grafts do not make significant levels
of catecholamines in vivo, the antinociception the grafts
provide might be a result of other antinociceptive molecules
synthesized and released by the cells, such as GABA or
met-enkephalin. Presumably the increased norepinephrine
phenotype recovered following excision of the oncogene by
disimmortalized cells would function to advantage in cell
(i) 5HT
[110, 116–118, 211, 229]
(ii) BDNF [110, 118, 211]
(iii) GABA [110, 113]
(iv) galanin [111]
(v) Met-enkephalin [170]
(i) enkephalin? [158]
(ii) release norepinephrine
[158]
therapy, but with disimmortalized rat chromaffin cell grafts
no such advantageous effect could be demonstrated. Rather,
the value of disimmortalization before transplantation is to
provide a measure of safety, with the complete absence of the
oncogene and prevention of even a remote possibility of viral
transfer of the large T antigen in the host, after grafting such
cells (Table 3).
8.4. Transgenic Opioid Expression in Immortalized Cell Lines.
A further advance to model genetically modified, disimmortalizable chromaffin cell lines, is the work by Duplan
and colleagues [165], who infected the disimmortalizable
loxtsTag/CrePR1/RAD chromaffin cell line with constructs
for the synthesis and secretion of the opioid met-enkephalin
(met-Enk). These transgenic rat chromaffin cell lines expressed easily detectible met-ENK in vitro cells, which contained
the met-ENK construct contained high levels of this opioid.
The transgene also contained a neurotrophin growth factor
(NGF) sequence for secretion of synthesized nascent protein,
and chromaffin cells which contained the met-ENK transgene were able to secrete the highest levels of the met-ENK
opioid from the cells. The value of opioids from chromaffin
grafts in cellular therapy, especially for pain [166], has seen
precedents in both animal [32, 62, 167], and more recently,
�10
human clinical work [43, 71, 165] when primary chromaffin
tissue was used as a graft source. When these disimmortalizable loxtsTag/CrePR1/RAD chromaffin cells were grafted,
by Duplan and colleagues, two weeks before injection of
formalin into the hindpaw in a model of tonic pain [168,
169], those rats which had been given grafts of cells which
secreted met-ENK did not develop the long-term response
to formalin injection, compared to rats which had no
grafted cells or those that had only received cells which were
transgenic for the vector only [170]. Although it is not yet
known how disimmortalization may influence the expression of transgene, such as the opioid met-ENK gene used
here, irreversible removal of a potentially subverting oncogene by its excision using the cre/lox system might be a clinically useful strategy. Of course, immortalization of human
chromaffin tissue with an oncogene, such as SV40Tag,
is not likely with any potential for deleterious expression of SV40 proteins [171], but disimmortalization utilizing
cre/lox site-directed removal of oncogenes in a growing
technology to create useful graft sources for cell therapy for
a variety of conditions [160, 161, 172]. There are a variety
of possible oncogenic sequences that could be used for the
reversible immortalization of human chromaffin cell lines,
including v-myc [173]. However, the creation of reversibly
immortalizable human chromaffin cell lines, perhaps from
precursors [174], is still somewhat in the near future [175].
But such a homogeneous source will also allow for the
manipulation of the chromaffin cell’s genome to investigate
the mechanisms of action responsible for cell grafts to repair
the injured CNS environment. Similar immortalization of
human chromaffin precursors and creation of human chromaffin lines [65, 67, 73] presage the advent of cellular therapy
as a therapeutic strategy that includes further development
of human stem cell and progenitor/precursor cell lines
[176].
9. Current Strategies for Immortalized
Cell Lines: Rationale/Studies
9.1. Stem Cells. An increasing number of articles describing
regenerative methods to improve function after injury and in
certain disease states have appeared in the last few years. Most
are related to transplants with stem cells [98], progenitors
[176, 177], and bone marrow and nontransplants. Stem
cell transplants can be ranked in the following descending
order of preference; bone marrow-derived cells, neural stem
cells, human umbilical cord blood cells, embryonic stem
cells, and myoblasts. Bone-marrow-derived cells and human
umbilical cord blood cell have been used for study in various
disease fields. The nonstem cell transplantation group is
made up primarily of islet cells, followed by biomaterials,
and other cells or tissues from a variety of sources [178].
With their more limited multipotency, the use and potential
of progenitor cells for improving function has still made
significant progress recently [179–181], especially in the
potential for renal and cardiac regeneration and reduction
of ischemia [181–183]. But another critical potential to be
fulfilled is in the area of the management of chronic, and
especially neuropathic, pain.
Pain Research and Treatment
9.2. Stem/Progenitor/Precursors (Animal Studies). In a recent
report [184] utilizing the partial nerve injury with CCI to
induce neuropathic pain, rat spinal embryonic progenitor
cells (SPC) that used basic fibroblast growth factorB2
(FGF-2) for proliferation of the SPC in vitro were able
to reduce thermal hyperalgesia after intrathecal transplant.
Presumably, grafted cells had been induced to a GABAergic
phenotype by FGF-2 in vitro and survived in its absence
after transplant, maintaining their phenotype to modulate
the neuropathic pain. The authors suggest that the grafts
also increased the glycine content in the CSF of grafted
animals, suggesting that if precursors could be induced
to a phenotype that provides nociceptive inhibition, they
would function much like cell minipumps, surviving in
the intrathecal space. Also in the CCI model of peripheral
pain, freshly isolated syngeneic marrow mononuclear cells
were injected i.v. following the unilateral nerve injury and
tactile allodynia and thermal hyperalgesia evaluated weekly.
Marrow transplantation did not prevent pain, and 5 days
after CCI all animals were equivalently lesioned. However, 10
days after CCI, rats that received marrow transplants demonstrated paw withdrawal response and paw withdrawal latency
patterns indicating recovery from pain, whereas untreated
rats continued to have significant pain behavior patterns.
The mechanisms underlying this improvement following
bone marrow injection are unknown. The authors speculate
that the marrow cells functioned as anti-inflammatory,
neuroprotective, and proangiogenic, modulating ischemic,
inflammatory, and cytotoxic events in the pain that follows
nerve constriction in this model. However, marrow transplants are also known to exacerbate diabetic neuropathy in a
different model of pain [185]. In this case, marrow cells fused
with peripheral neurons, stimulating apoptosis.
One cause of severe neuropathic pain is traumatic injury
that involves SCI is spinal root avulsion, and replacement
of DRG neurons could reduce that pain. A recent study
investigated whether human neural stem/progenitor cells
(hNSPCs) transplanted to the DRG cavity can serve as
a source for repairing lost peripheral sensory connections
[186]. The hNSPCs robustly differentiate to neurons, which
survive long-term transplantation. The neuronal population
in the transplants was tightly surrounded by astrocytes,
suggesting their active role in neuron survival. Furthermore,
3 months after grafting, hNSPCs were found in the dorsal
root transitional zone (DRTZ) and within the spinal cord.
The level of differentiation of transplanted cells was high
in the core of the transplants whereas cells that migrated
to the DRTZ and spinal cord were undifferentiated, nestinexpressing precursors. However, hNSPCs are not sufficient
to restore normal sensory function; additional factors are
required to guide their differentiation to the desired type of
neurons.
9.3. Neuroprogenitor Cell Lines for Pain (The NT2 Cell
Line). More than two decades ago, it was discovered that,
when treated with retinoic acid (RA), a human embryonal
carcinoma cell line, NTera2cl.D/l (NT2, hNT2), differentiates
irreversibly into several morphologically and phenotypically
distinct cell types, which include terminally differentiated
�Pain Research and Treatment
postmitotic CNS neurons [187, 188]. Successive replating of
RA-treated NT2 cells, in the presence of growth inhibitors,
results in the isolation of purified human neurons [189],
which have been extensively characterized and tested in vivo
in a number of animal models of traumatic injury and
neurodegenerative disease [188, 190–194]. This NT2 human
neural cell line has been used for a variety of studies that
reveal not only the regulation of an oncogenic phenotype by
agents such as retinoic acid [189, 195, 196], but it has been
well characterized for the expression of a variety of neural
phenotypic properties [197] and proteins [198, 199] with
differentiation of the cells in vitro and in vivo [200]. The
potential application of NT2 neurons in cell transplantation
therapy for CNS disorders, and their use as vehicles for delivering exogenous proteins into the human brain for gene therapy, has been envisioned [201]. Such NT2 neurons have been
used in Phase I-II clinical trials for the treatment of stroke
[202–204], and this cell line or its derivatives can likely be
utilized for further reparative transplant strategies [205]. The
rate-limiting enzyme GAD, for GABA synthesis is present in
differentiating NT2 neurons in vitro [206, 207], and GABA
is a phenotype for NT2 cells differentiated and transplanted
in vivo [208]. But the NT2 cell line has a great variety of
phenotypes expressed in differentiated cells [193, 207], making it less-than-ideal for a specific antinociceptive phenotype
expression that might be required for application in pain
management, as has been modeled in rat cell lines described
above. While induction of a GABAergic phenotype in neural
stem cells is possible with a somewhat complicated method
of sequential exposure to epigenetic signals in vitro [209], the
host graft environment does not always allow for induction
of desirable phenotypes in vivo [210]. A naturally occurring,
stable antinociceptive phenotype in a clinically useful human
progenitor cell line, such as that derived from the NT2 cell
line, is more desirable, and these are described below.
9.4. NT2-Derived Cell Lines for Pain. Since the NT2 cell line
contains a mixed phenotype population of cells, many of
which would likely be antinociceptive based on multiple
studies with rat cell lines by this author and others using
central and peripheral models of neuropathic pain [110, 111,
113, 115–119, 170, 211], it was considered likely that individual cell lines could be subcloned from the NT2 parental
cell lines, using ordinary subcloning techniques involving
isolation of individual cells plated sparsely, allowing them
to grow into colonies, surrounding these with cloning rings,
and removing these colonies to establish individual cell
lines. This rather laborious process resulted in a number of
well-growing, morphologically and immunohistochemically
distinct NT2 subclonal cell lines, numbered consecutively as
they were isolated. Two of the cell lines were chosen for their
potential to function as sources of neurotransmitters which
might prove useful in further testing in animal models of
pain, the hNT2.17 [212] and hNT2.19 [213] cell lines. Since
they are derived from the neuroprogenitor parent cell line
NT2, these are considered to be human neuroprogenitor cell
lines as well, resulting in a neuronal-limited phenotype, and
will be described below. These human progenitor cell lines
are being developed for clinical use. Their characterization
11
and use in animal models reflect what will be required of any
similar regenerative cell therapy for FDA approval [98, 214].
9.5. The Human Neuronal GABA hNT2.17 Cell Line. Centrally induced excitotoxic SCI has been developed as a model
of neuropathic pain [215, 216]. Intraspinal injection of
quisqualic acid (QUIS), a mixed AMPA/metabotropic receptor agonist, produces injury with pathological characteristics
similar to those associated with ischemic and traumatic
SCI [217]. In addition, the pathological changes that this
SCI induces, significant mechanical allodynia, and thermal
hyperalgesia have been shown to be important behavioral
components, without the additional motor dysfunction seen
in other SCI models [218]. Each of these sensory behaviors is
indicative of altered sensory function and/or pain, similar to
that reported after SCI. After spinal transplantation of primary adrenal tissue grafts following QUIS injections, painrelated behaviors, including the hypersensitivity to mechanical stimuli and “excessive grooming” were significantly
reduced [219]. Given the related loss of GABA inhibition that
seems to accompany SCI and the induction of neuropathic
pain [220–222], the excitotoxic SCI model was used to examine the hNT2-derived GABAergic hNT2.17 cell transplant
into the lumbar subarachnoid space following injury and the
ability of those grafts to reverse behavioral hypersensitivity
[212]. These cells cease to express tumor genes, express an
exclusively neuronal, GABAergic and glycinergic phenotype,
and synthesize, secrete and release GABA and glycine into
the extracellular environment with differentiation [212].
Their morphology is similar to the GABA/glycine spinal
interneurons found in the dorsal horn sensory laminae [223]
and such characteristics are stable in more than 10 years of
use in transplant studies. These inhibitory human neurons
additionally co-localize GABA and glycine and the vesicular
inhibitory amino acid transporter (VIATT, VGAT), especially
along the neurite outgrowths in vitro, suggesting that this
molecular machinery allows co-release in hNT2.17 cells
[224], without the need for a separate glycine transporter.
When differentiated hNT2.17 cells are placed two weeks after
the QUIS SCI, mechanical allodynia and thermal hyperalgesia are potently and permanently attenuated, with no greater
effect when twice the normal transplant dose (1 million
cells/i.t. injection) is used [225, 226], or grafts are placed
in the cervical subdural space [226]. Besides transplant dose
and graft placement, the immunosuppression regimen and
transplant time after SCI were also optimized [226]. The
same optimal transplant dose was only moderately effective
when placed in chronic SCI, six weeks after SCI, compared to
100% effectiveness when placed in an acute SCI, 2 weeks after
injury. Additionally, maximal graft effectiveness required two
weeks of immunosuppression with cyclosporine A (CsA;
10 mg/Kg), immediately following transplant. No immunosuppression or less lengthy exposure to CsA provided
minimal or no attenuation [226]. The “excessive grooming”
behaviors associated with this model were also examined.
When excessively grooming rats that had been transplanted
with either viable or nonviable hNT2.17 cells and exposed
to different immunosuppression regimens were examined
for development, resolution, worsening, or no change of
�12
Pain Research and Treatment
excessive grooming, a trend toward improvement was associated with viable grafts and at least 1 week of accompanying
CsA immunosuppression. When transplant was delayed to 6
weeks, no improvement in excessive grooming was seen. This
last finding duplicates what was seen in the QUIS SCI model
and graft of antinociceptive adrenal medullary tissue [219],
suggesting potent reversal of behavioral hypersensitivity
may have a neuroprotective effect on the progression of
spinal excitotoxicity associated spinal lesions. We [227], and
others [228], have recently reported on the use of hNT2.17
cell therapy in various other models of peripheral and
central nervous system damage, including: CCI of the sciatic
nerve, streptozotocin-induced diabetic peripheral neuropathy (DPN) pain, and severe contusive SCI. Much as we [229]
and others [56] have seen in the CCI peripheral nerve injury
model and antinociceptive cell grafts Vaysse and colleagues
[228], reported that the decrease in GABA expression in the
spinal dorsal horn of CCI injured animals is concomitant
with a decline of its synthetic enzyme GAD67 immunoreactivity (ir) and mRNA but not GAD65. In hNT2.17 transplanted animals a strong induction of GAD67 mRNA one
week after graft was seen, which was followed by a recovery
of GAD67 and GABA ir. This effect paralleled a reduction of
hindpaw hypersensitivity and thermal hyperalgesia induced
by CCI. These results suggest not only that hNT2.17 GABA
cells can modulate neuropathic pain after CCI by minimizing
the imbalance and restoring the cellular GABAergic pathway,
but that such a mechanism may be associated with any potent
antinociceptive cell graft, at least in the CCI model. The
same, or a similar mechanism may explain the antinociceptive effects of hNT2.17 grafts in contusive SCI and DPN pain
[227]. DPN pain studies have suggested aberrant spinal or
supraspinal modulation of sensory processing [230, 231],
including a central mechanism [232] with the ventral posterolateral thalamus becoming hyperexcitable in the presence
of spinal and supraspinal disinhibition. Disinhibition and
loss of spinal GABA modulation are also well reported in
SCI pain [222]. But evidence for a GABAergic mechanism
associated with hNT2.17 transplant and antinociception in
these other models of pain awaits further studies.
therapy with a rat 5HT cell line that is able to permanently
reverse neuropathic pain that develops after partial nerve
injury [110] and hemisection SCI [115, 241]. The human
neuronal 5HT hNT2.19 cells used for cell therapy after severe
contusive SCI reverses behavioral hypersensitivity [241],
without affecting motor dysfunction when grafts are placed
intrathecally. These same cell grafts modestly recover motor
function when placed intraspinally [213] in the same severe
contusion SCI model of chronic pain and motor dysfunction.
Additionally, grafts of hNT2.19 cells attenuate tactile allodynia and thermal hyperalgesia in the excitotoxic SCI QUIS
model [227], much like grafts of hNT2.17 cells. In fact, lumbar intrathecal 5HT hNT2.19 and GABA hNT2.19 grafts are
equally nociceptive no matter which SCI pain model is used,
excitotoxic or contusive [227], suggesting that these cells
may affect the same or similar mechanism-of-action that is
common to both models that initiates behavioral hypersensitivity. We have already shown a GABAergic mechanismof-action for grafts of hNT2.17 cells [228] and suggested it
may be common in SCI pain. Although grafts of a 5HT rat
neuronal cell line which is antinociceptive after hemisection
SCI [116], depending on graft location [115], much like
grafts of hNT2.19 cells, it does so by attenuating bilateral
hyperexcitability of dorsal horn neurons [117], restores
spinal serotonin, downregulates the serotonin transporter,
and increases BDNF tissue content in the spinal cord [118],
these same 5HT rat cell line grafts also induce a GABAergic
mechanism of action in the CCI model of nerve injury
and neuropathic pain [229]. Obviously, it will be important
in future studies to understand how each separate human
neuronal cell line provides antinociception in each PNS or
CNS pain model, but the same or similar mechanisms are
not out of the question. Since the 5HT hNT2.19 cells, like
the hNT2.17 cell line, are exclusively neuronal, although
with a different neurotransmitter phenotype, and equally
nontumorogenic before and after transplant [227, 241], this
human progenitor cell line is equally appropriate to develop
as a clinical tool, not only to treat neuropathic pain, but also
motor dysfunction, especially after SCI [241–243] (Table 4).
9.6. The Human Neuronal 5HT hNT2.19 Cell Line. Current
understanding of central and supraspinal [233] mechanisms
for the induction and maintenance of chronic pain after SCI
suggests a major role for the hypofunction of serotonergic
(5HT) inhibitory systems [234–236]. This same SCI leads to
the loss of descending serotonergic excitatory inputs caudal
to the lesion site and altered neurotransmitter status within
the ventral horn a-motoneurons, which also contributes to
motor dysfunction after SCI [116, 237]. A variety of animal
studies have used a 5HT rat cell line [110, 116–118] or
5HT raphe transplants [238, 239] as a means to ameliorate
some of these problems. Supplemental cell therapy can also
work to create a spinal environment to ameliorate local
damage and simultaneously promote a regenerative response
in multiple axonal populations, including descending spinal
serotonin fibers [240], or reverse chronic pain after SCI by
reversing the hyperexcitability in the dorsal horn pain processing centers [117]. We have described the use of 5HT cell
10. Summary of Advantages and
Disadvantages and Future Directions of
Cell-Therapy Approaches
To summarize the conclusions from 30 years of cell therapy
studies, the advantages and disadvantages of a cell-based
approach to the treatment of neuropathic pain would include
the following (1) It is likely that only human cells will be useful as a source, whether primary tissue or cell lines given that
such sources are the least likely to be rejected, would function
appropriately, and respond to environmental cues in the
human host. Encapsulation technologies could be helpful
here, if these technologies could keep the grafts both viable
and functional. However, (2) it is likely that there are limits
to the achievable levels of a given biologic agent that can be
delivered by the cells and multiple intrathecal injections over
time, with return of pain, may be necessary. (3) It is possible
that delivery of a multitude of substances, in addition to
�Pain Research and Treatment
13
Table 4: Stem/Precursor cell lines.
Source
Stem/Progenitors:
Rat spinal (embryonic) progenitor cells
[184]
Adrenal progenitors—human [281]
Human neuronal/progenitors:
Human NT2 cell line [205, 282, 283]
Model
Results
Partial nerve injury (CCI) [184]
(i) Reduced thermal hyperalgesia [184]
Excitotoxic SCI pain [283]
(i) Release cannabinoids [282]
(ii) Antinociceptive [283]
Human NT2.17 GABA cell line
[212, 225, 226, 228, 283, 284]
Excitotoxic SCI (QUIS)
[212, 225, 226, 283–285]
Streptozotocin-induced diabetic
peripheral neuropathy (DPN) [283]
Partial nerve injury (CCI) [228, 283]
(i) Antinociceptive [212, 226, 228, 283]
(ii) Restores spinal GABA DH inhibition [228]
(iii) Colocalize/release GABA and glycine [212]
Human NT2.19 5HT cell line
[213, 241, 283]
(i) Contusive SCI [213, 241]
(ii) Excitotoxic SCI [283]
(i) Intraspinal grafts attenuate motor
dysfunction [213]
(ii) Intrathecal grafts provide antinociception
[241, 283]
those of therapeutic interest, many of which cannot be
completely defined before hand, will be associated with cellbased therapy. Different subgroups of pain patients may
respond to such agents in either positive or negative ways
dependent on each person’s primary cause of pain. Valid and
reliable phenotypic classification of pain based on individual
signs and symptoms, and various biomarkers, may be helpful
in defining such subgroups and their responses to a specific
substance related to cell transplant. Such responses are
unknown until very large populations are treated with any
given cell source. (4) It seems that more acute neuropathic
pain is treatable with cell therapy; chronic pain may require
multiple i.t. injections as needed. Even still, pain relief may
not be equally effective in all cases, and additional pharmacologic and cognitive/adjuvant therapies will be needed. (5)
There is a dependence on the survival of implanted cells,
which may be limited by immunologic factors, nutrient and
oxygen supply, and so forth. However, such survival and
efficacy can be tested preclinically, in nonhuman studies. (6)
It is likely, at least for now, that only the simplest approaches
to creating cell sources will be quickly approved for clinical
trials, that is, not overly-manipulated (in cell culture) or
bio-engineered cells (containing viral vectors). (7) Some
course of immunosuppression will likely be required, even
for autologous sources, but such regimens could be tested
rigorously in preclinical experiments, that is, nonhuman
primates. (8) An intrathecal graft site would likely be the
best for cell injections for the treatment of neuropathic pain.
Any other transplant type would need to be placed as near
to its “site-of-action” as is reasonable, especially if grafted cells are known to not migrate, such as with NT2 cells. (9)
If cells are used for antinociception, and placed intrathecally,
those that passively secrete inhibitory (or drive inhibitory
systems) neurotransmitters would likely work the best, rather
than cells that secrete any number of known and unknown
agents. (10) Transplant sources need to be tested in as
many preclinical peripheral and central models of motor
and sensory injury as possible, to avoid later “off-label”
use/side-effects in humans. (11) A pragmatic, rather than
a purely mechanistic, approach can be used for preclinical
work. It is more useful that cell therapy approaches are tested,
without necessarily understanding how they work, as long
as such technologies are proven as safe as possible. (12) All
efforts should be taken to keep patients/provider costs as
low as possible, so that cell therapy can be applied almost
as readily as pharmacologic treatments. Cell-based research
and development will likely be an expensive and complicated
solution to treat pain, compared to a purely pharmacologic
or mixed-use mechanical-pump/spinal-stimulator delivery
approach. (13) The rapid establishment of a Research Ethics
Consortium should be established, to be tasked to assemble an interdisciplinary panel of experts who will apply
ethical principles to analyze the social merit relative to the
economic incentives of this emerging technology [244]. This
consortium will evaluate how these novel ethical issues in
emerging technologies are addressed under current oversight
and regulatory structures and where there may be gaps and
need for revised or new public policy approaches.
References
[1] G. J. Bennett, “Neuropathic pain: new insights, new interventions,” Hospital Practice, vol. 33, no. 10, pp. 95–114, 1998.
[2] N. Torrance, B. H. Smith, M. I. Bennett, and A. J. Lee, “The
epidemiology of chronic pain of predominantly neuropathic
origin. Results from a general population survey,” Journal of
Pain, vol. 7, no. 4, pp. 281–289, 2006.
[3] D. Bouhassira, M. Lanteri-Minet, N. Attal, B. Laurent, and
C. Touboul, “Prevalence of chronic pain with neuropathic
characteristics in the general population,” Pain, vol. 136, no.
3, pp. 380–387, 2008.
[4] M. Haanpää, N. Attal, M. Backonja et al., “NeuPSIG guidelines on neuropathic pain assessment,” Pain, vol. 152, no. 1,
pp. 14–27, 2011.
[5] E. R. Felix, Y. Cruz-Almeida, and E. G. Widerstrom-Noga,
“Chronic pain after spinal cord injury: what characteristics
make some pains more disturbing than others?” Journal of
Rehabilitation Research and Development, vol. 44, no. 5, pp.
703–716, 2007.
[6] P. J. Siddall, J. M. McClelland, S. B. Rutkowski, and M.
J. Cousins, “A longitudinal study of the prevalence and
�14
[7]
[8]
[9]
[10]
[11]
[12]
[13]
[14]
[15]
[16]
[17]
[18]
[19]
[20]
[21]
[22]
[23]
[24]
Pain Research and Treatment
characteristics of pain in the first 5 years following spinal cord
injury,” Pain, vol. 103, no. 3, pp. 249–257, 2003.
F. Biering-Sorensen, N. B. Finnerup, D. D. Cardenas et al.,
“International spinal cord injury pain classification: part I.
Background and description,” Spinal Cord. In press.
E. G. Widerstrom-Noga, E. Felipe-Cuervo, J. G. Broton, R. C.
Duncan, and R. P. Yezierski, “Perceived difficulty in dealing
with consequences of spinal cord injury,” Archives of Physical
Medicine and Rehabilitation, vol. 80, no. 5, pp. 580–586, 1999.
Y. Cruz-Almeida, A. Martinez-Arizala, and E. G. Widerstrom-Noga, “Chronicity of pain associated with spinal cord
injury: a longitudinal analysis,” Journal of Rehabilitation
Research and Development, vol. 42, no. 5, pp. 585–594, 2005.
P. J. Siddall, M. J. Cousins, A. Otte, T. Griesing, R. Chambers,
and T. K. Murphy, “Pregabalin in central neuropathic pain
associated with spinal cord injury: a placebo-controlled trial,”
Neurology, vol. 67, no. 10, pp. 1792–1800, 2006.
“2011 National Diabetes Fact Sheet,” 2011, http://www.cdc
.gov/diabetes/pubs/pdf/ndfs 2011.pdf.
J. R. Mendell and Z. Sahenk, “Painful sensory neuropathy,”
The New England Journal of Medicine, vol. 348, no. 13, pp.
1243–1255, 2003.
H. Klit, N. B. Finnerup, and T. S. Jensen, “Central poststroke pain: clinical characteristics, pathophysiology, and
management,” The Lancet Neurology, vol. 8, no. 9, pp. 857–
868, 2009.
C. J. Vierck, P. T. Hansson, and R. P. Yezierski, “Clinical
and pre-clinical pain assessment: are we measuring the same
thing?” Pain, vol. 135, no. 1-2, pp. 7–10, 2008.
R. H. Dworkin, A. B. O’Connor, M. Backonja et al., “Pharmacologic management of neuropathic pain: evidence-based
recommendations,” Pain, vol. 132, no. 3, pp. 237–251, 2007.
N. Attal, G. Cruccu, M. Haanpää et al., “EFNS guidelines on
pharmacological treatment of neuropathic pain,” European
Journal of Neurology, vol. 13, no. 11, pp. 1153–1169, 2006.
D. E. Moulin, A. J. Clark, I. Gilron et al., “Pharmacological
management of chronic neuropathic pain—consensus statement and guidelines from the canadian pain society,” Pain
Research and Management, vol. 12, no. 1, pp. 13–21, 2007.
R. H. Dworkin, A. B. O’Connor, J. Audette et al., “Recommendations for the pharmacological management of neuropathic pain: an overview and literature update,” Mayo Clinic
Proceedings, vol. 85, no. 3, supplement, pp. S3–S14, 2010.
T. P. Nash, “Treatment options in painful diabetic neuropathy,” Acta Neurologica Scandinavica, Supplement, vol. 100, no.
173, pp. 36–42, 1999.
G. Cruccu, T. Z. Aziz, L. Garcia-Larrea et al., “EFNS guidelines on neurostimulation therapy for neuropathic pain,”
European Journal of Neurology, vol. 14, no. 9, pp. 952–970,
2007.
C. Norrbrink Budh and T. Lundeberg, “Non-pharmacological pain-relieving therapies in individuals with spinal cord
injury: a patient perspective,” Complementary Therapies in
Medicine, vol. 12, no. 4, pp. 189–197, 2004.
H. Merskey and N. Bogduk, Classification of Chronic Pain:
Descriptions of Chronic Syndromes and Definitions of Pain
Terms, IASP Press, Seattle, Wash, USA, 2nd edition, 1994.
R. D. Treede, T. S. Jensen, J. N. Campbell et al., “Neuropathic
pain: redefinition and a grading system for clinical and
research purposes,” Neurology, vol. 70, no. 18, pp. 1630–1635,
2008.
T. S. Jensen, R. Baron, M. Haanpää et al., “A new definition
of neuropathic pain,” Pain, vol. 152, no. 10, pp. 2204–2205,
2011.
[25] N. B. Finnerup, L. Sorensen, F. Biering-Sorensen, I. L. Johannesen, and T. S. Jensen, “Segmental hypersensitivity and spinothalamic function in spinal cord injury pain,” Experimental Neurology, vol. 207, no. 1, pp. 139–149, 2007.
[26] C. J. Woolf and M. B. Max, “Mechanism-based pain diagnosis: issues for analgesic drug development,” Anesthesiology,
vol. 95, no. 1, pp. 241–249, 2001.
[27] T. W. Victor, M. P. Jensen, A. R. Gammaitoni, E. M. Gould,
R. E. White, and B. S. Galer, “The dimensions of pain quality:
factor analysis of the pain quality assessment scale,” Clinical
Journal of Pain, vol. 24, no. 6, pp. 550–555, 2008.
[28] R. H. Dworkin, M. P. Jensen, A. R. Gammaitoni, D. O.
Olaleye, and B. S. Galer, “Symptom profiles differ in patients
with neuropathic versus non-neuropathic pain,” Journal of
Pain, vol. 8, no. 2, pp. 118–126, 2007.
[29] R. Rolke, W. Magerl, K. A. Campbell et al., “Quantitative
sensory testing: a comprehensive protocol for clinical trials,”
European Journal of Pain, vol. 10, no. 1, pp. 77–88, 2006.
[30] C. Maier, R. Baron, T. R. Tolle et al., “Quantitative sensory
testing in the German research network on neuropathic pain
(DFNS): somatosensory abnormalities in 1236 patients with
different neuropathic pain syndromes,” Pain, vol. 150, no. 3,
pp. 439–450, 2010.
[31] P. J. Siddall and M. J. Cousins, “Spine update: spinal pain
mechanisms,” Spine, vol. 22, no. 1, pp. 98–104, 1997.
[32] J. Sagen and J. E. Kemmler, “Increased levels of met-enkephalin-like immunoreactivity in the spinal cord CSF of rats
with adrenal medullary transplants,” Brain Research, vol. 502,
no. 1, pp. 1–10, 1989.
[33] B. G. Livett, D. M. Dean, L. G. Whelan et al., “Co-release
of enkephalin and catecholamines from cultured adrenal
chromaffin cells,” Nature, vol. 289, no. 5795, pp. 317–319,
1981.
[34] B. G. Livett, P. Boksa, D. M. Dean et al., “Use of isolated chromaffin cells to study basic release mechanisms,” Journal of the
Autonomic Nervous System, vol. 7, no. 1, pp. 59–86, 1983.
[35] J. Sagen, G. D. Pappas, and H. B. Pollard, “Analgesia induced
by isolated bovine chromaffin cells implanted in rat spinal
cord,” Proceedings of the National Academy of Sciences of the
United States of America, vol. 83, no. 19, pp. 7522–7526, 1986.
[36] J. Sagen, G. D. Pappas, and M. J. Perlow, “Adrenal medullary
tissue transplants in the rat spinal cord reduce pain sensitivity,” Brain Research, vol. 384, no. 1, pp. 189–194, 1986.
[37] J. I. Ruz-Franzi and J. M. González-Darder, “Study of the
analgesic effects of the implant of adrenal medullary into
the subarachnoid space in rats,” Acta Neurochirurgica, Supplement, vol. 52, pp. 39–41, 1991.
[38] J. Sagen, G. D. Pappas, and M. J. Perlow, “Alterations in
nociception following adrenal medullary transplants into the
rat periaqueductal gray,” Experimental Brain Research, vol.
67, no. 2, pp. 373–379, 1987.
[39] J. Sagen, H. Wang, and G. D. Pappas, “Adrenal medullary
implants in the rat spinal cord reduce nociception in a
chronic pain model,” Pain, vol. 42, no. 1, pp. 69–79, 1990.
[40] R. Ginzburg and Z. Seltzer, “Subarachnoid spinal cord transplantation of adrenal medulla suppresses chronic neuropathic pain behavior in rats,” Brain Research, vol. 523, no. 1,
pp. 147–150, 1990.
[41] J. Sagen, “Chromaffin cell transplants for alleviation of chronic pain,” ASAIO Journal, vol. 38, no. 1, pp. 24–28, 1992.
[42] A. T. Hama and J. Sagen, “Reduced pain-related behavior
by adrenal medullary transplants in rats with experimental
painful peripheral neuropathy,” Pain, vol. 52, no. 2, pp. 223–
231, 1993.
�Pain Research and Treatment
[43] Y. Lazorthes, B. Sallerin, J. C. Verdie et al., “Management
of intractable cancer pain: from intrathecal morphine to
chromaffin cell allograft,” Neurochirurgie, vol. 46, no. 5, pp.
454–465, 2000.
[44] J. D. Ortega, J. Sagen, and G. D. Pappas, “Short-term
immunosuppression enhances long-term survival of bovine
chromaffin cell xenografts in rat CNS,” Cell Transplantation,
vol. 1, no. 1, pp. 33–41, 1992.
[45] J. Sagen, G. D. Pappas, and A. P. Winnie, “Alleviation of pain
in cancer patients by adrenal medullary transplants in the
spinal subarachnoid space,” Cell Transplantation, vol. 2, no.
3, pp. 259–266, 1993.
[46] A. P. Winnie, G. D. Pappas, T. K. D. Gupta, H. Wang, J.
D. Ortega, and J. Sagen, “Subarachnoid adrenal medullary
transplants for terminal cancer pain: a report of preliminary
studies,” Anesthesiology, vol. 79, no. 4, pp. 644–653, 1993.
[47] S. P. Wilson, K. J. Chang, and O. H. Viveros, “Opioid peptide
synthesis in bovine and human adrenal chromaffin cells,”
Peptides, vol. 2, supplement 1, pp. 83–88, 1981.
[48] K. Unsicker, “The trophic cocktail made by adrenal chromaffin cells,” Experimental Neurology, vol. 123, no. 2, pp. 167–
173, 1993.
[49] J. B. Siegan and J. Sagen, “Attenuation of formalin pain
responses in the rat by adrenal medullary transplants in the
spinal subarachnoid space,” Pain, vol. 70, no. 2-3, pp. 279–
285, 1997.
[50] J. Sagen, J. E. Kemmler, and H. Wang, “Adrenal medullary
transplants increase spinal cord cerebrospinal fluid catecholamine levels and reduce pain sensitivity,” Journal of Neurochemistry, vol. 56, no. 2, pp. 623–627, 1991.
[51] H. Wang and J. Sagen, “Absence of appreciable tolerance
and morphine cross-tolerance in rats with adrenal medullary
transplants in the spinal cord,” Neuropharmacology, vol. 33,
no. 5, pp. 681–692, 1994.
[52] A. T. Hama and J. Sagen, “Induction of spinal NADPHdiaphorase by nerve injury is attenuated by adrenal medullary transplants,” Brain Research, vol. 640, no. 1-2, pp. 345–
351, 1994.
[53] J. B. Siegan, A. T. Hama, and J. Sagen, “Alterations in rat
spinal cord cGMP by peripheral nerve injury and adrenal
medullary transplantation,” Neuroscience Letters, vol. 215, no.
1, pp. 49–52, 1996.
[54] J. Sagen and H. Wang, “Adrenal medullary grafts suppress cfos induction in spinal neurons of arthritic rats,” Neuroscience
Letters, vol. 192, no. 3, pp. 181–184, 1995.
[55] J. B. Siegan and J. Sagen, “Attenuation of NMDA-induced
spinal hypersensitivity by adrenal medullary transplants,”
Brain Research, vol. 680, no. 1-2, pp. 88–98, 1995.
[56] T. Ibuki, A. T. Hama, X. T. Wang, G. D. Pappas, and J. Sagen,
“Loss of GABA-immunoreactivity in the spinal dorsal horn
of rats with peripheral nerve injury and promotion of recovery by adrenal medullary grafts,” Neuroscience, vol. 76, no. 3,
pp. 845–858, 1996.
[57] J. B. Siegan, U. Herzberg, B. R. Frydel, and J. Sagen,
“Adrenal medullary transplants reduce formalin-evoked cfos expression in the rat spinal cord,” Brain Research, vol. 944,
no. 1-2, pp. 174–183, 2002.
[58] I. D. Hentall, B. R. Noga, and J. Sagen, “Spinal allografts of
adrenal medulla block nociceptive facilitation in the dorsal
horn,” Journal of Neurophysiology, vol. 85, no. 4, pp. 1788–
1792, 2001.
[59] J. Sagen, H. Wang, P. A. Tresco, and P. Aebischer, “Transplants
of immunologically isolated xenogeneic chromaffin cells
provide a long-term source of pain-reducing neuroactive
15
[60]
[61]
[62]
[63]
[64]
[65]
[66]
[67]
[68]
[69]
[70]
[71]
[72]
[73]
[74]
substances,” Journal of Neuroscience, vol. 13, no. 6, pp. 2415–
2423, 1993.
E. Buchser, M. Goddard, B. Heyd et al., “Immunoisolated
xenogeneic chromaffin cell therapy for chronic pain: initial
clinical experience,” Anesthesiology, vol. 85, pp. 1005–1012,
1996.
J. Sagen, “Chromaffin cell transplants in the CNS: basic and
clinical update,” in Yearbook of Cell and Tissue Transplantation, R. P. Lanza and W. L. Chick, Eds., pp. 71–89, Kluwer
Academic, Dodrecht, The Netherlands, 1996.
G. D. Pappas, Y. Lazorthes, J. C. Bes, M. Tafani, and A. P.
Winnie, “Relief of intractable cancer pain by human chromaffin cell transplants: experience at two medical centers,”
Neurological Research, vol. 19, no. 1, pp. 71–77, 1997.
J. Tkaczuk, J. C. Bes, H. Duplan et al., “Intrathecal grafting
of unencapsulated adrenal medullary tissue can bring CD4 T
lymphocytes into CSF: a potentially deleterious event for the
graft,” Cell Transplantation, vol. 9, no. 1, pp. 79–91, 2000.
N. Bhattacharya, M. K. Chhetri, K. L. Mukherjee et al.,
“Human fetal adrenal transplant: a possible role in relieving
intractable pain in advanced rheumatoid arthiritis,” Clinical
and Experimental Obstetrics and Gynecology, vol. 29, no. 3,
pp. 197–206, 2002.
Y. Jeon, W. Y. Baek, S. H. Chung, N. Shin, H. R. Kim, and S.
A. Lee, “Cultured human chromaffin cells grafted in spinal
subarachnoid space relieves allodynia in a pain rat model,”
Korean Journal of Anesthesiology, vol. 60, no. 5, pp. 357–361,
2011.
J. C. Bes, B. R. Frydel, E. D. Potter et al., “Human embryonic
and fetal adrenal glands as sources of neural precursors
for possible transplantation strategies,” American Society for
Neural Transplantation and Repair, vol. 8, article 61, 2001.
S. Jozan, J. Aziza, S. Châtelin et al., “Human fetal chromaffin
cells: a potential tool for cell pain therapy,” Experimental Neurology, vol. 205, no. 2, pp. 525–535, 2007.
P. Michalewicz, C. E. Laurito, G. D. Pappas, Y. Lu, and D. C.
Yeomans, “Purification of adrenal chromaffin cells increases
antinociceptive efficacy of xenotransplants without immunosuppression,” Cell Transplantation, vol. 8, no. 1, pp. 103–109,
1999.
S. Mercadante, G. Intravaia, P. Villari et al., “Intrathecal
treatment in cancer patients unresponsive to multiple trials
of systemic opioids,” Clinical Journal of Pain, vol. 23, no. 9,
pp. 793–798, 2007.
J. C. Bes, Y. Lazorthes, J. C. Sol, J. Tkaczuk, and B. Sallerin,
“Clinical perspectives of xenografts: encapsuled chromaffin
cells and pain,” Pathologie Biologie, vol. 48, no. 4, pp. 365–
367, 2000.
Y. Lazorthes, J. Sagen, B. Sallerin et al., “Human chromaffin
cell graft into the CSF for cancer pain management: a prospective phase II clinical study,” Pain, vol. 87, no. 1, pp. 19–
32, 2000.
J. C. Bes, J. Tkaczuk, K. A. Czech et al., “One-year chromaffin
cell allograft survival in cancer patients with chronic pain:
morphological and functional evidence,” Cell Transplantation, vol. 7, no. 3, pp. 227–238, 1998.
Y. Lazorthes, J. C. Bes, J. Sagen et al., “Transplantation of
human chromaffin cells for control of intractable cancer
pain,” Acta Neurochirurgica, Supplement, vol. 64, pp. 97–100,
1995.
L. A. Greene and A. S. Tischler, “Establishment of a noradrenergic clonal line of rat adrenal pheochromocytoma cells
which respond to nerve growth factor,” Proceedings of the
National Academy of Sciences of the United States of America,
vol. 73, no. 7, pp. 2424–2428, 1976.
�16
[75] S. Gajavelli, D. A. Castellanos, O. Furmanski, P. C. Schiller,
and J. Sagen, “Sustained analgesic peptide secretion and cell
labeling using a novel genetic modification,” Cell Transplantation, vol. 17, no. 4, pp. 445–455, 2008.
[76] J. B. Siegan and J. Sagen, “A natural peptide with NMDA inhibitory activity reduces tonic pain in the formalin model,”
NeuroReport, vol. 8, no. 6, pp. 1379–1381, 1997.
[77] F. NasiriNezhad and J. Sagen, “NMDA antagonist peptide supplementation enhances pain alleviation by adrenal
medullary transplants,” Cell Transplantation, vol. 14, no. 4,
pp. 203–211, 2005.
[78] J. C. Byrd, M. Hadjiconstantinou, and D. Cavalla, “Epinephrine synthesis in the PC12 pheochromocytoma cell line,”
European Journal of Pharmacology, vol. 127, no. 1-2, pp. 139–
142, 1986.
[79] M. Yoshikawa, H. Nakayama, S. Ueno, M. Hirano, H.
Hatanaka, and H. Furuya, “Chronic fentanyl treatments
induce the up-regulation of µ opioid receptor mRNA in rat
pheochromocytoma cells,” Brain Research, vol. 859, no. 2, pp.
217–223, 2000.
[80] T. L. Stockley and P. L. Chang, “Non-autologous transplantation with immuno-isolation in large animals—a review,”
Annals of the New York Academy of Sciences, vol. 831, pp. 408–
426, 1997.
[81] H. H. Wu, B. R. Lester, Z. Sun, and G. L. Wilcox, “Antinociception following implantation of mouse B16 melanoma
cells in mouse and rat spinal cord,” Pain, vol. 56, no. 2, pp.
203–210, 1994.
[82] V. Curto-Reyes, L. Juárez, E. Garcı́a-Pérez et al., “Local loperamide inhibits thermal hyperalgesia but not mechanical
allodynia induced by intratibial inoculation of melanoma
cells in mice,” Cellular and Molecular Neurobiology, vol. 28,
no. 7, pp. 981–990, 2008.
[83] J. L. de la Calle, M. A. Mena, J. R. Gonzaez-Escalada, and C.
L. Paı́no, “Intrathecal transplantation of neuroblastoma cells
decreases heat hyperalgesia and cold allodynia in a rat model
of neuropathic pain,” Brain Research Bulletin, vol. 59, no. 3,
pp. 205–211, 2002.
[84] H. H. Wu, G. L. Wilcox, and S. C. McLoon, “Implantation of
AtT-20 or genetically modified AtT-20/hENK cells in mouse
spinal cord induced antinociception and opioid tolerance,”
Journal of Neuroscience, vol. 14, no. 8, pp. 4806–4814, 1994.
[85] Y. Saitoh, T. Taki, N. Arita, T. Ohnishi, and T. Hayakawa,
“Analgesia induced by transplantation of encapsulated tumor
cells secreting β-endorphin,” Journal of Neurosurgery, vol. 82,
no. 4, pp. 630–634, 1995.
[86] Y. Saitoh, Y. Eguchi, Y. Hagihara et al., “Dose-dependent
doxycycline-mediated adrenocorticotropic hormone secretion from encapsulated Tet-on proopiomelanocortin
Neuro2A cells in the subarachnoid space,” Human Gene
Therapy, vol. 9, no. 7, pp. 997–1002, 1998.
[87] K. Ishii, M. Isono, R. Inoue, and S. Hori, “Attempted gene
therapy for intractable pain: dexamethasone-mediated exogenous control of β-endorphin secretion in genetically modified cells and intrathecal transplantation,” Experimental Neurology, vol. 166, no. 1, pp. 90–98, 2000.
[88] Y. Saitoh, T. Taki, N. Arita, T. Ohnishi, and T. Hayakawa,
“Cell therapy with encapsulated xenogeneic tumor cells
secreting β-endorphin for treatment of peripheral pain,” Cell
Transplantation, vol. 4, supplement 1, pp. S13–S17, 1995.
[89] H. Hodges, K. Pollock, P. Stroemer et al., “Making stem cell
lines suitable for transplantation,” Cell Transplantation, vol.
16, no. 2, pp. 101–115, 2007.
[90] W. Chen, R. Mi, N. Haughey, M. Oz, and A. Hoke, “Immortalization and characterization of a nociceptive dorsal root
Pain Research and Treatment
[91]
[92]
[93]
[94]
[95]
[96]
[97]
[98]
[99]
[100]
[101]
[102]
[103]
[104]
[105]
[106]
ganglion sensory neuronal line,” Journal of the Peripheral Nervous System, vol. 12, no. 2, pp. 121–130, 2007.
Q. Gökhan, Q. Song, and M. F. Mehler, “Generation and
regulation of developing immortalized neural cell lines,”
Methods, vol. 16, no. 3, pp. 345–358, 1998.
U. Lendahl and R. D. G. McKay, “The use of cell lines in
neurobiology,” Trends in Neurosciences, vol. 13, no. 4, pp.
132–137, 1990.
C. L. Cepko, “Immortalization of neural cells via retrovirusmediated oncogene transduction,” Annual Review of Neuroscience, vol. 12, pp. 47–65, 1989.
P. S. Jat and P. A. Sharp, “Cell lines established by a temperature-sensitive simian virus 40 large-T-antigen gene are
growth restricted at the nonpermissive temperature,” Molecular and Cellular Biology, vol. 9, no. 4, pp. 1672–1681, 1989.
P. S. Jat, M. D. Noble, P. Ataliotis et al., “Direct derivation
of conditionally immortal cell lines from an H-2Kb -tsA58
transgenic mouse,” Proceedings of the National Academy of
Sciences of the United States of America, vol. 88, no. 12, pp.
5096–5100, 1991.
J. Y. Jiang, B. G. Lyeth, G. L. Clifton, L. W. Jenkins, R. J.
Hamm, and R. L. Hayes, “Relationship between body and
brain temperature in traumatically brain-injured rodents,”
Journal of Neurosurgery, vol. 74, no. 3, pp. 492–496, 1991.
T. M. S. Chang and S. Prakash, “Therapeutic uses of microencapsulated genetically engineered cells,” Molecular Medicine Today, vol. 4, no. 5, pp. 221–227, 1998.
H. Isaac Chen, A. Bakshi, N. C. Royo, S. N. Magge, and D. J.
Watson, “Neural stem cells as biological minipumps: a faster
route to cell therapy for the CNS?” Current Stem Cell Research
and Therapy, vol. 2, no. 1, pp. 13–22, 2007.
F. H. Gage, J. A. Wolff, M. B. Rosenberg et al., “Grafting
genetically modified cells to the brain: possibilities for the
future,” Neuroscience, vol. 23, no. 3, pp. 795–807, 1987.
A. D. Zurn, J. Tseng, and P. Aebischer, “Treatment of
Parkinson’s disease. Symptomatic cell therapies: cells as biological minipumps,” European neurology, vol. 36, no. 6, pp.
405–408, 1996.
J. Sagen and M. J. Eaton, “Cellular implantation for the
treatment of chronic pain,” in Pain: Current Understanding,
Emerging Therapies, and Novel Approaches to Drug Discovery,
W. K. Schmidt, Ed., pp. 815–833, Marcel Dekker, New York,
NY, USA, 2003.
L. A. White, M. J. Eaton, M. C. Castro et al., “Distinct regulatory pathways control neurofilament expression and neurotransmitter synthesis in immortalized serotonergic neurons,”
Journal of Neuroscience, vol. 14, no. 11 I, pp. 6744–6753, 1994.
S. R. Whittemore and L. A. White, “Target regulation of
neuronal differentiation in a temperature-sensitive cell line
derived from medullary raphe,” Brain Research, vol. 615, no.
1, pp. 27–40, 1993.
M. J. Eaton, J. K. Staley, M. Y. Y. Globus, and S. R. Whittemore, “Developmental regulation of early serotonergic
neuronal differentiation: the role of brain-derived neurotrophic factor and membrane depolarization,” Developmental Biology, vol. 170, no. 1, pp. 169–182, 1995.
J. S. Rudge, M. J. Eaton, P. Mather, R. M. Lindsay, and S.
R. Whittemore, “CNTF induces raphe neuronal precursors
to switch from a serotonergic to a cholinergic phenotype in
vitro,” Molecular and Cellular Neurosciences, vol. 7, no. 3, pp.
204–221, 1996.
M. J. Eaton, H. A. Dancausse, and S. R. Whittemore, “GDNF
and neurturin affect the survival and 5HT synthesis in
immortalized raphe neuronal precursors,” in Proceedings of
the Summer Neuropeptide Conference, 1997.
�Pain Research and Treatment
[107] M. J. Eaton and S. R. Whittemore, “Adrenocorticotropic hormone activation of adenylate cyclase in raphe neurons: multiple regulatory pathways control serotonergic neuronal differentiation,” Journal of Neurobiology, vol. 28, no. 4, pp. 465–
481, 1995.
[108] M. J. Eaton and S. R. Whittemore, “Autocrine BDNF secretion enhances the survival and serotonergic differentiation
of raphe neuronal precursor cells grafted into the adult rat
CNS,” Experimental Neurology, vol. 140, no. 2, pp. 105–114,
1996.
[109] A. E. Farakash and R. K. Portney, “The pharmacological
management of chronic pain in the paraplegic patient,” The
Journal of the American Paraplegia Society, vol. 9, pp. 41–50,
1986.
[110] M. J. Eaton, H. A. Dancausse, D. I. Santiago, and S. R. Whittemore, “Lumbar transplants of immortalized serotonergic
neurons alleviate chronic neuropathic pain,” Pain, vol. 72, no.
1-2, pp. 59–69, 1997.
[111] M. J. Eaton, S. Karmally, M. A. Martinez, J. A. Plunkett,
T. Lopez, and P. J. Cejas, “Lumbar transplant of neurons
genetically modified to secrete galanin reverse pain-like
behaviors after partial sciatic nerve injury,” Journal of the
Peripheral Nervous System, vol. 4, no. 3-4, pp. 245–257, 1999.
[112] P. Cejas, J. A. Plunkett, M. A. Martinez et al., “A BDNFsynthesizing cell line ameliorates chronic neuropathic pain,”
Society for Neuroscience, vol. 25, article 1945, 1999.
[113] M. J. Eaton, J. A. Plunkett, M. A. Martinez et al., “Transplants
of neuronal cells bioengineered to synthesize GABA alleviate
chronic neuropathic pain,” Cell Transplantation, vol. 8, no. 1,
pp. 87–101, 1999.
[114] M. J. Eaton, “SCI pain is a GABA-sensitive phenomenon
amendable to GABA cell therapy,” in Proceedings of the 7th
International Conference on the Mechanisms and Treatment of
Neuropathic Pain, 2004.
[115] B. C. Hains, J. A. Yucra, M. J. Eaton, and C. E. Hulsebosch, “Intralesion transplantation of serotonergic precursors enhances locomotor recovery but has no effect on
development of chronic central pain following hemisection
injury in rats,” Neuroscience Letters, vol. 324, no. 3, pp. 222–
226, 2002.
[116] B. C. Hains, K. M. Johnson, D. J. McAdoo, M. J. Eaton, and
C. E. Hulsebosch, “Engraftment of serotonergic precursors
enhances locomotor function and attenuates chronic central
pain behavior following spinal hemisection injury in the rat,”
Experimental Neurology, vol. 171, no. 2, pp. 361–378, 2001.
[117] B. C. Hains, K. M. Johnson, M. J. Eaton, W. D. Willis, and
C. E. Hulsebosch, “Serotonergic neural precursor cell grafts
attenuate bilateral hyperexcitability of dorsal horn neurons
after spinal hemisection in rat,” Neuroscience, vol. 116, no. 4,
pp. 1097–1110, 2003.
[118] B. C. Hains, S. D. Fullwood, M. J. Eaton, and C. E. Hulsebosch, “Subdural engraftment of serotonergic neurons following spinal hemisection restores spinal serotonin, downregulates serotonin transporter, and increases BDNF tissue
content in rat,” Brain Research, vol. 913, no. 1, pp. 35–46,
2001.
[119] L. A. Stubley, M. A. Martinez, S. Karmally, T. Lopez, P.
Cejas, and M. J. Eaton, “Only early intervention with gammaaminobutyric acid cell therapy is able to reverse neuropathic
pain after partial nerve injury,” Journal of Neurotrauma, vol.
18, no. 4, pp. 471–477, 2001.
[120] K. K. Jha, S. Banga, V. Palejwala, and H. L. Ozer, “SV40mediated immortalization,” Experimental Cell Research, vol.
245, no. 1, pp. 1–7, 1998.
17
[121] K. H. Scheidtmann, “SV40 large T antigen induces a protein
kinase responsible for phosphorylation of the cellular protein
p53,” Current Topics in Microbiology and Immunology, vol.
144, pp. 85–88, 1989.
[122] T. L. Sladek and J. W. Jacobberger, “Simian virus 40 large Tantigen expression decreases the G1 and increases the G2+
M cell cycle phase durations in exponentially growing cells,”
Journal of Virology, vol. 66, no. 2, pp. 1059–1065, 1992.
[123] V. Cherington, M. Brown, E. Paucha, J. St Louis, B. M.
Spiegelman, and T. M. Roberts, “Separation of simian
virus 40 large-T-antigen-transforming and origin-binding
functions from the ability to block differentiation,” Molecular
and Cellular Biology, vol. 8, no. 3, pp. 1380–1384, 1988.
[124] K. Frederiksen, P. S. Jat, N. Valtz, D. Levy, and R. McKay,
“Immortalization of precursor cells from the mammalian
CNS,” Neuron, vol. 1, no. 6, pp. 439–448, 1988.
[125] Z. Ikram, T. Norton, and P. S. Jat, “The biological clock that
measures the mitotic life-span of mouse embryo fibroblasts
continues to function in the presence of simian virus 40
large tumor antigen,” Proceedings of the National Academy of
Sciences of the United States of America, vol. 91, no. 14, pp.
6448–6452, 1994.
[126] I. Reynisdottir, D. R. O’Reilly, L. K. Miller, and C. Prives,
“Thermally inactivated simian virus 40 tsA58 mutant T
antigen cannot initiate viral DNA replication in vitro,”
Journal of Virology, vol. 64, no. 12, pp. 6234–6245, 1990.
[127] P. S. Frisa, M. N. Goodman, G. M. Smith, J. Silver, and J.
W. Jacobberger, “Immortalization of immature and mature
mouse astrocytes with SV40 T antigen,” Journal of Neuroscience Research, vol. 39, no. 1, pp. 47–56, 1994.
[128] M. N. Goodman, J. Silver, and J. W. Jacobberger, “Establishment and neurite outgrowth properties of neonatal and adult
rat olfactory bulb glial cell lines,” Brain Research, vol. 619, no.
1-2, pp. 199–213, 1993.
[129] P. S. Jat and P. A. Sharp, “Large T antigens of simian virus 40
and polyomavirus efficiently establish primary fibroblasts,”
Journal of Virology, vol. 59, no. 3, pp. 746–750, 1986.
[130] K. N. Prasad, E. D. Clarkson, F. G. La Rosa, J. EdwardsPrasad, and C. R. Freed, “Efficacy of grafted immortalized
dopamine neurons in an animal model of parkinsonism: a
review,” Molecular Genetics and Metabolism, vol. 65, no. 1, pp.
1–9, 1998.
[131] D. E. Bredesen, K. Hisanaga, and F. R. Sharp, “Neural transplantation using temperature-sensitive immortalized neural
cells: a preliminary report,” Annals of Neurology, vol. 27, no.
2, pp. 205–207, 1990.
[132] P. J. Renfranz, M. G. Cunningham, and R. D. G. McKay,
“Region-specific differentiation of the hippocampal stem cell
line HiB5 upon implantation into the developing mammalian brain,” Cell, vol. 66, no. 4, pp. 713–729, 1991.
[133] S. R. Whittemore, V. R. Holets, R. W. Keane, D. J. Levy, and
R. D. G. McKay, “Transplantation of a temperature-sensitive,
nerve growth factor-secreting, neuroblastoma cell line into
adult rats with fimbria-fornix lesions rescues cholinergic
septal neurons,” Journal of Neuroscience Research, vol. 28, no.
2, pp. 156–170, 1991.
[134] S. M. Onifer, S. R. Whittemore, and V. R. Holets, “Variable
morphological differentiation of a raphe-derived neuronal
cell line following transplantation into the adult rat CNS,”
Experimental Neurology, vol. 122, no. 1, pp. 130–142, 1993.
[135] L. S. Shihabuddin, J. A. Hertz, V. R. Holets, and S. R.
Whittemore, “The adult CNS retains the potential to direct
region-specific differentiation of a transplanted neuronal
precursor cell line,” Journal of Neuroscience, vol. 15, no. 10,
pp. 6666–6678, 1995.
�18
[136] L. S. Shihabuddin, J. P. Brunschwig, V. R. Holets, M.
B. Bunge, and S. R. Whittemore, “Induction of mature
neuronal properties in immortalized neuronal precursor
cells following grafting into the neonatal CNS,” Journal of
Neurocytology, vol. 25, no. 2, pp. 101–111, 1996.
[137] L. S. Shihabuddin, V. R. Holets, and S. R. Whittemore, “Selective hippocampal lesions differentially affect the phenotypic
fate of transplanted neuronal precursor cells,” Experimental
Neurology, vol. 139, no. 1, pp. 61–72, 1996.
[138] M. J. Eaton, B. Frydel, T. Lopez et al., “Generation and initial
characterization of conditionally immortalized chromaffin
cells,” Journal of Cellular Biochemistry, vol. 79, pp. 38–57,
2000.
[139] M. J. Eaton, M. Martinez, S. Karmally, T. Lopez, and J. Sagen,
“Initial characterization of the transplant of immortalized
chromaffin cells for the attenuation of chronic neuropathic
pain,” Cell Transplantation, vol. 9, no. 5, pp. 637–656, 2000.
[140] K. Unsicker, “The chromaffin cell: paradigm in cell, developmental and growth factor biology,” Journal of Anatomy, vol.
183, no. 2, pp. 207–221, 1993.
[141] M. Livett, S. Spector, A. Sjoerdsma et al., “Elucidation of
the rate-limiting step in norepinephrine biosynthesis in the
perfused guinea-pig heart,” Journal of Pharmacology and
Experimental Therapeutics, vol. 148, pp. 1–8, 1965.
[142] V. M. Pickel, T. Hyub Joh, P. M. Field et al., “Cellular localization of tyrosine hydroxylase by immunohistochemistry,”
Journal of Histochemistry and Cytochemistry, vol. 23, no. 1,
pp. 1–12, 1975.
[143] I. Totzauer, W. Amselgruber, F. Sinowatz, and M. Gratzl,
“Early expression of chromogranin A and tyrosine hydroxylase during prenatal development of the bovine adrenal
gland,” Anatomy and Embryology, vol. 191, no. 2, pp. 139–
143, 1995.
[144] K. A. Czech, R. Pollak, G. D. Pappas, and J. Sagen,
“Bovine chromaffin cells for CNS transplantation do not
elicit xenogeneic T cell proliferative responses in vitro,” Cell
Transplantation, vol. 5, no. 2, pp. 257–267, 1996.
[145] A. A. J. Verhofstad, “Kinetics of adrenal medullary cells,”
Journal of Anatomy, vol. 183, no. 2, pp. 315–326, 1993.
[146] B. G. Livett, “Adrenal medullary chromaffin cells in vitro,”
Physiological Reviews, vol. 64, no. 4, pp. 1103–1161, 1984.
[147] K. Anastassiadis, M. Rostovskaya, S. Lubitz, S. Weidlich,
and A. F. Stewart, “Precise conditional immortalization
of mouse cells using tetracycline-regulated SV40 large Tantigen,” Genesis, vol. 48, no. 4, pp. 220–232, 2010.
[148] M. J. Eaton and H. Duplan, “Useful cell lines derived from
the adrenal medulla,” Molecular and Cellular Endocrinology,
vol. 228, no. 1-2, pp. 39–52, 2004.
[149] B. Sauer and N. Henderson, “Site-specific DNA recombination in mammalian cells by the Cre recombinase of
bacteriophage P1,” Proceedings of the National Academy of
Sciences of the United States of America, vol. 85, no. 14, pp.
5166–5170, 1988.
[150] B. Sauer, “Inducible gene targeting in mice using the Cre/lox
system,” Methods, vol. 14, no. 4, pp. 381–392, 1998.
[151] F. Paillard, “Reversible cell immortalization with the Cre-lox
system,” Human Gene Therapy, vol. 10, no. 10, pp. 1597–
1598, 1999.
[152] K. A. Westerman and P. Leboulch, “Reversible immortalization of mammalian cells mediated by retroviral transfer
and site-specific recombination,” Proceedings of the National
Academy of Sciences of the United States of America, vol. 93,
no. 17, pp. 8971–8976, 1996.
[153] N. Kobayashi, M. Miyazaki, K. Fukaya et al., “Treatment of
surgically induced acute liver failure with transplantation of
Pain Research and Treatment
[154]
[155]
[156]
[157]
[158]
[159]
[160]
[161]
[162]
[163]
[164]
[165]
[166]
[167]
[168]
[169]
[170]
highly differentiated immortalized human hepatocytes,” Cell
Transplantation, vol. 9, no. 5, pp. 733–735, 2000.
A. Weber, “Immortalization of hepatic progenitor cells,”
Pathologie Biologie, vol. 52, no. 2, pp. 93–96, 2004.
D. Metzger and R. Feil, “Engineering the mouse genome by
site-specific recombination,” Current Opinion in Biotechnology, vol. 10, no. 5, pp. 470–476, 1999.
C. Kellendonk, F. Tronche, A. P. Monaghan, P. O. Angrand,
F. Stewart, and G. Schütz, “Regulation of Cre recombinase
activity by the synthetic steroid RU 486,” Nucleic Acids
Research, vol. 24, no. 8, pp. 1404–1411, 1996.
C. Kellendonk, F. Tronche, E. Casanova, K. Anlag, C. Opherk,
and G. Schütz, “Inducible site-specific recombination in the
brain,” Journal of Molecular Biology, vol. 285, no. 1, pp. 175–
182, 1999.
M. J. Eaton, J. P. Herman, N. Jullien, T. L. Lopez, M. Martinez, and J. Huang, “Immortalized chromaffin cells disimmortalized with Cre/lox site-directed recombination for use
in cell therapy for pain after partial nerve injury,” Experimental Neurology, vol. 175, no. 1, pp. 49–60, 2002.
Y. X. Jiang, Y. Lu, T. J. Liu, J. Yang, Y. Chen, and Y. W.
Fang, “Using HSV-TK/GCV suicide gene therapy to inhibit
lens epithelial cell proliferation for treatment of posterior
capsular opacification,” Molecular Vision, vol. 17, pp. 291–
299, 2011.
J. Cai, M. Ito, K. A. Westerman, N. Kobayashi, P. Leboulch,
and I. J. Fox, “Construction of a non-tumorigenic rat hepatocyte cell line for transplantation: reversal of hepatocyte
immortalization by site-specific excision of the SV40 T
antigen,” Journal of Hepatology, vol. 33, no. 5, pp. 701–708,
2000.
N. Kobayashi, T. Fujiwara, K. A. Westerman et al., “Prevention of acute liver failure in rats with reversibly immortalized
human hepatocytes,” Science, vol. 287, no. 5456, pp. 1258–
1262, 2000.
J. P. Herman, H. Becq, and A. Enjalbert, “A reversible immortalization procedure to obtain neural cell lines,” Society for
Neuroscience, vol. 23, article 319, 1997.
L. Berghella, L. De Angelis, M. Coletta et al., “Reversible
immortalization of human myogenic cells by site-specific
excision of a retrovitally transferred oncogene,” Human Gene
Therapy, vol. 10, no. 10, pp. 1607–1617, 1999.
N. Kobayashi, H. Noguchi, K. A. Westerman et al., “Efficient
Cre/loxP site-specific recombination in a HepG2 human liver
cell line,” Cell Transplantation, vol. 9, no. 5, pp. 737–742,
2000.
H. Duplan, J. C. Bes, M. Tafani et al., “Adrenal medullary
explants as an efficient tool for pain control: adhesive biomolecular components are involved in graft function ex vivo,”
Experimental Neurology, vol. 163, no. 2, pp. 331–347, 2000.
H. Wang and J. Sagen, “Optimization of adrenal medullary
allograft conditions for pain alleviation,” Journal of Neural
Transplantation and Plasticity, vol. 5, no. 1, pp. 49–64, 1994.
J. D. Ortega and J. Sagen, “Pharmacologic characterization
of opioid peptide release from chromaffin cell transplants
using a brain slice superfusion method,” Experimental Brain
Research, vol. 95, no. 3, pp. 381–387, 1993.
A. Tjolsen, O. G. Berge, S. Hunskaar, J. H. Rosland, and K.
Hole, “The formalin test: an evaluation of the method,” Pain,
vol. 51, no. 1, pp. 5–17, 1992.
K. McCormack, P. Prather, and C. Chapleo, “Some new
insights into the effects of opioids in phasic and tonic
nociceptive tests,” Pain, vol. 78, no. 2, pp. 79–98, 1998.
H. Duplan, R. Y. Li, C. Vue et al., “Grafts of immortalized
chromaffin cells bio-engineered to improve met-enkephalin
�Pain Research and Treatment
[171]
[172]
[173]
[174]
[175]
[176]
[177]
[178]
[179]
[180]
[181]
[182]
[183]
[184]
[185]
[186]
release also reduce formalin-evoked c-fos expression in rat
spinal cord,” Neuroscience Letters, vol. 370, no. 1, pp. 1–6,
2004.
D. Ferber, “Public health: creeping consensus on SV40 and
polio vaccine,” Science, vol. 298, no. 5594, pp. 725–727, 2002.
J. Liu, J. Pan, S. Naik et al., “Characterization and evaluation
of detoxification functions of a nontumorigenic immortalized porcine hepatocyte cell line (HepLiu),” Cell Transplantation, vol. 8, no. 3, pp. 219–232, 1999.
A. Villa, E. Y. Snyder, A. Vescovi, and A. Martı́nez-Serrano,
“Establishment and properties of a growth factor-dependent,
perpetual neural stem cell line from the human CNS,”
Experimental Neurology, vol. 161, no. 1, pp. 67–84, 2000.
F. Deimling, S. Finotto, K. Lindner et al., “Characterization
of adrenal chromaffin progenitor cells in mice,” Advances in
Pharmacology, vol. 42, pp. 932–935, 1998.
A. Schober, K. Krieglstein, and K. Unsicker, “Molecular
cues for the development of adrenal chromaffin cells and
their preganglionic innervation,” European Journal of Clinical
Investigation, Supplement, vol. 30, supplement 3, pp. 87–90,
2000.
M. J. Eaton, S. Q. Wolfe, and E. Widerstrom-Noga, “Use of
progenitor cells in pain management,” in Stem Cell & Regenerative Medicine, H. Cheung, Ed., pp. 94–128, Bentham
Science, Oak Park, Ill, USA, 2010.
M. B. Newman, I. Misiuta, A. E. Willing et al., “Tumorigenicity issues of embryonic carcinoma-derived stem cells:
relevance to surgical trials using NT2 and hNT neural cells,”
Stem Cells and Development, vol. 14, no. 1, pp. 29–43, 2005.
D. H. Park, C. V. Borlongan, D. J. Eve, and P. R. Sanberg, “The
emerging field of cell and tissue engineering,” Medical Science
Monitor, vol. 14, no. 11, pp. RA206–RA220, 2008.
E. N. Kozlova, “Strategies to repair lost sensory connections
to the spinal cord,” Molekuliarnaia Biologiia, vol. 42, no. 5,
pp. 820–829, 2008.
A. N. Raval, “Therapeutic potential of adult progenitor cells
in the management of chronic myocardial ischemia,” American Journal of Cardiovascular Drugs, vol. 8, no. 5, pp. 315–
326, 2008.
M. S. Goligorsky, M. C. Kuo, D. Patschan, and M. C. Verhaar,
“Review article: endothelial progenitor cells in renal disease,”
Nephrology, vol. 14, no. 3, pp. 291–297, 2009.
C. Stamm, Y. H. Choi, B. Nasseri, and R. Hetzer, “A heart full
of stem cells: the spectrum of myocardial progenitor cells in
the postnatal heart,” Therapeutic Advances in Cardiovascular
Disease, vol. 3, no. 3, pp. 215–229, 2009.
M. Jevon, A. Dorling, and P. I. Hornick, “Progenitor cells and
vascular disease,” Cell Proliferation, vol. 41, supplement 1, pp.
146–164, 2008.
C. R. Lin, P. C. Wu, H. C. Shih et al., “Intrathecal spinal
progenitor cell transplantation for the treatment of neuropathic pain,” Cell Transplantation, vol. 11, no. 1, pp. 17–24,
2002.
T. Terashima, H. Kojima, M. Fujimaya et al., “The fusion of
bone-marrow-derived proinsulin-expressing with nerve cells
underlies diabetic neuropathy,” Proceedings of the National
Academy of Sciences of the United States of America, vol. 102,
no. 35, pp. 12525–12530, 2005.
E. Akesson, M. Sandelin, N. Kanaykina, H. Aldskogius,
and E. N. Kozlova, “Long-term survival, robust neuronal
differentiation, and extensive migration of human forebrain
stem/progenitor cells transplanted to the adult rat dorsal root
ganglion cavity,” Cell Transplantation, vol. 17, no. 10-11, pp.
1115–1123, 2008.
19
[187] P. W. Andrews, I. Damjanov, D. Simon et al., “Pluripotent
embryonal carcinoma clones derived from the human teratocarcinoma cell line Tera-2. Differentiation in vivo and in
vitro,” Laboratory Investigation, vol. 50, no. 2, pp. 147–162,
1984.
[188] S. J. Pleasure and V. M. Y. Lee, “NTera 2 cells: a human
cell line which displays characteristics expected of a human
committed neuronal progenitor cell,” Journal of Neuroscience
Research, vol. 35, no. 6, pp. 585–602, 1993.
[189] P. W. Andrews, “Retinoic acid induces neuronal differentiation of a cloned human embryonal carcinoma cell line in
vitro,” Developmental Biology, vol. 103, no. 2, pp. 285–293,
1984.
[190] C. V. Borlongan, Y. Tajima, J. Q. Trojanowski, V. M. Y.
Lee, and P. R. Sanberg, “Transplantation of cryopreserved
human embryonal carcinoma-derived neurons (NT2N cells)
promotes functional recovery in ischemic rats,” Experimental
Neurology, vol. 149, no. 2, pp. 310–321, 1998.
[191] W. M. W. Cheung, A. H. Chu, M. F. Leung, and N. Y. Ip,
“Induction of trk receptors by retinoic acid in a human
embryonal carcinoma cell line,” NeuroReport, vol. 7, no. 6,
pp. 1204–1208, 1996.
[192] A. Ferrari, E. Ehler, R. M. Nitsch, and J. Gotz, “Immature
human NT2 cells grafted into mouse brain differentiate into
neuronal and glial cell types,” The FEBS Letters, vol. 486, no.
2, pp. 121–125, 2000.
[193] I. Guillemain, G. Alonoso, G. Patey et al., “Human NT2 neurons express a large variety of neurotransmission phenotypes
in vitro,” The Journal of Comparative Neurology, vol. 422, pp.
380–395, 2000.
[194] J. I. Satoh and Y. Kuroda, “Differential gene expression
between human neurons and neuronal progenitor cells in
culture: an analysis of arrayed cDNA clones in NTera2 human
embryonal carcinoma cell line as a model system,” Journal of
Neuroscience Methods, vol. 94, no. 2, pp. 155–164, 2000.
[195] I. Guillemain, G. Fontes, A. Privat, and I. Chaudieu, “Early
programmed cell death in human NT2 cell cultures during
differentiation induced by all-trans-retinoic retinoic acid,”
Journal of Neuroscience Research, vol. 71, no. 1, pp. 38–45,
2003.
[196] E. Dmitrovsky, D. Moy, W. H. Miller, A. Li, and H. Masui,
“Retinoic acid causes a decline in TGF-α expression, cloning
efficiency, and tumorigenicity in a human embryonal cancer
cell line,” Oncogene Research, vol. 5, no. 3, pp. 233–239, 1990.
[197] P. Gortz, W. Fleischer, C. Rosenbaum, F. Otto, and M. Siebler,
“Neuronal network properties of human teratocarcinoma
cell line-derived neurons,” Brain Research, vol. 1018, no. 1,
pp. 18–25, 2004.
[198] F. Megiorni, B. Mora, P. Indovina, and M. C. Mazzilli,
“Expression of neuronal markers during NTera2/cloneD1
differentiation by cell aggregation method,” Neuroscience
Letters, vol. 373, no. 2, pp. 105–109, 2005.
[199] V. M. Y. Lee and P. W. Andrews, “Differentiation of NTERA2 clonal human embryonal carcinoma cells into neurons
involves the induction of all three neurofilament proteins,”
Journal of Neuroscience, vol. 6, no. 2, pp. 514–521, 1986.
[200] M. M. Daadi, S. Saporta, A. E. Willing, T. Zigova, M. P.
McGrogan, and P. R. Sanberg, “In vitro induction and in
vivo expression of bcl-2 in the hNT neurons,” Brain Research
Bulletin, vol. 56, no. 2, pp. 147–152, 2001.
[201] J. Q. Trojanowski, S. R. Kleppner, R. S. Hartley et al., “Transfectable and transplantable postmitotic human neurons: a
potential ’platform’ for gene therapy of nervous system
diseases,” Experimental Neurology, vol. 144, no. 1, pp. 92–97,
1997.
�20
[202] D. Kondziolka, L. Wechsler, S. Goldstein et al., “Transplantation of cultured human neuronal cells for patients with
stroke,” Neurology, vol. 55, no. 4, pp. 565–569, 2000.
[203] P. T. Nelson, D. Kondziolka, L. Wechsler et al., “Clonal
human (hNT) neuron grafts for stroke therapy: neuropathology in a patient 27 months after implantation,” American
Journal of Pathology, vol. 160, no. 4, pp. 1201–1206, 2002.
[204] C. C. Meltzer, D. Kondziolka, V. L. Villemagne et al.,
“Serial[18F] fluorodeoxyglucose positron emission tomography after human neuronal implantation for stroke,” Neurosurgery, vol. 49, no. 3, pp. 586–592, 2001.
[205] D. Usvald, P. Vodicka, J. Hlucilova et al., “Analysis of
dosing regimen and reproducibility of intraspinal grafting
of human spinal stem cells in immunosuppressed minipigs,”
Cell Transplantation, vol. 19, no. 9, pp. 1103–1122, 2010.
[206] A. Yoshioka, M. Yudkoff, and D. Pleasure, “Expression
of glutamic acid decarboxylase during human neuronal
differentiation: studies using the NTera-2 culture system,”
Brain Research, vol. 767, no. 2, pp. 333–339, 1997.
[207] G. Podrygajlo, M. A. Tegenge, A. Gierse et al., “Cellular phenotypes of human model neurons (NT2) after differentiation
in aggregate culture,” Cell and Tissue Research, vol. 336, no. 3,
pp. 439–452, 2009.
[208] S. Saporta, A. E. Willing, L. O. Colina et al., “In vitro and
in vivo characterization of hNT neuron neurotransmitter
phenotypes,” Brain Research Bulletin, vol. 53, no. 3, pp. 263–
268, 2000.
[209] M. Bosch, J. R. Pineda, C. Sunol et al., “Induction of GABAergic phenotype in a neural stem cell line for transplantation in
an excitotoxic model of Huntington’s disease,” Experimental
Neurology, vol. 190, no. 1, pp. 42–58, 2004.
[210] Q. L. Cao, R. M. Howard, J. B. Dennison, and S. R. Whittemore, “Differentiation of engrafted neuronal-restricted
precursor cells is inhibited in the traumatically injured spinal
cord,” Experimental Neurology, vol. 177, no. 2, pp. 349–359,
2002.
[211] P. J. Cejas, M. Martinez, S. Karmally et al., “Lumbar
transplant of neurons genetically modified to secrete brainderived neurotrophic factor attenuates allodynia and hyperalgesia after sciatic nerve constriction,” Pain, vol. 86, no. 1-2,
pp. 195–210, 2000.
[212] M. J. Eaton, S. Q. Wolfe, M. Martinez et al., “Subarachnoid
transplant of a human neuronal cell line attenuates chronic
allodynia and hyperalgesia after excitotoxic SCI in the rat,”
Journal of Pain, vol. 8, no. 1, pp. 33–50, 2007.
[213] M. J. Eaton, D. D. Pearse, J. S. McBroom, and Y. A.
Berrocal, “The combination of human neuronal serotonergic
cell implants and environmental enrichment after contusive
SCI improves motor recovery over each individual strategy,”
Behavioural Brain Research, vol. 194, no. 2, pp. 236–241,
2008.
[214] J. Sagen, “Cellular therapies for spinal cord injury: what will
the FDA need to approve moving from the laboratory to the
human?” Journal of Rehabilitation Research and Development,
vol. 40, no. 4, supplement 1, pp. 71–79, 2003.
[215] R. P. Yezierski, S. Liu, G. L. Ruenes, K. J. Kajander, and K.
L. Brewer, “Excitotoxic spinal cord injury: behavioral and
morphological characteristics of a central pain model,” Pain,
vol. 75, no. 1, pp. 141–155, 1998.
[216] R. P. Yezierski and S. H. Park, “The mechanosensitivity of
spinal sensory neurons following intraspinal injections of
quisqualic acid in the rat,” Neuroscience Letters, vol. 157, no.
1, pp. 115–119, 1993.
Pain Research and Treatment
[217] S. Liu, G. L. Ruenes, and R. P. Yezierski, “NMDA and
non-NMDA receptor antagonists protect against excitotoxic
injury in the rat spinal cord,” Brain Research, vol. 756, no. 1-2,
pp. 160–167, 1997.
[218] V. Dietz and A. Curt, “Neurological aspects of spinal-cord
repair: promises and challenges,” The Lancet Neurology, vol.
5, no. 8, pp. 688–694, 2006.
[219] K. L. Brewer and R. P. Yezierski, “Effects of adrenal medullary
transplants on pain-related behaviors following excitotoxic
spinal cord injury,” Brain Research, vol. 798, no. 1-2, pp. 83–
92, 1998.
[220] C. O. Stiller, J. G. Cui, W. T. O’Connor et al., “GABA-ergic
mechanisms may be involved in the spinal cord stimulation induced reversion of allodynia: animal studies with
microdialysis,” American Pain Society Abstracts, vol. 95,
article 801, 1995.
[221] C. Qin, J. Q. Du, J. S. Tang, and R. D. Foreman, “Bradykinin
is involved in the mediation of cardiac nociception during
ischemia through upper thoracic spinal neurons,” Current
Neurovascular Research, vol. 6, no. 2, pp. 89–94, 2009.
[222] J. G. Meisner, A. D. Marsh, and D. R. Marsh, “Loss of
GABAergic interneurons in laminae I–III of the spinal
cord dorsal horn contributes to reduced GABAergic tone
and neuropathic pain after spinal cord injury,” Journal of
Neurotrauma, vol. 27, no. 4, pp. 729–737, 2010.
[223] F. I. Sutherland, B. Anne Bannatyne, R. Kerr, J. S. Riddell,
and D. J. Maxwell, “Inhibitory amino acid transmitters
associated with axons in presynaptic apposition to cutaneous
primary afferent axons in the cat spinal cord,” The Journal of
Comparative Neurology, vol. 452, no. 2, pp. 154–162, 2002.
[224] S. M. Wojcik, S. Katsurabayashi, I. Guillemin et al., “A
shared vesicular carrier allows synaptic corelease of GABA
and glycine,” Neuron, vol. 50, no. 4, pp. 575–587, 2006.
[225] S. Q. Wolfe, M. Garg, N. M. A. Cumberbatch et al.,
“Optimizing the transplant dose of a human neuronal cell
line graft to treat SCI pain in the rat,” Neuroscience Letters,
vol. 414, no. 2, pp. 121–125, 2007.
[226] M. J. Eaton and S. Q. Wolfe, “Clinical feasibility for cell
therapy using human neuronal cell line to treat neuropathic
behavioral hypersensitivity following spinal cord injury in
rats,” Journal of Rehabilitation Research and Development, vol.
46, no. 1, pp. 145–166, 2009.
[227] M. J. Eaton and Y. Berrocal, “Potential for cell-transplant
therapy with human neuronal precursors to treat neuropathic pain in models of PNS and CNS injury: comparison
of hNT2.17 and hNT2.19 cell lines,” Pain Research Treatment.
In press.
[228] L. Vaysse, J. C. Sol, Y. Lazorthes, M. Courtade-Saidi, M. J.
Eaton, and S. Jozan, “GABAergic pathway in a rat model
of chronic neuropathic pain: modulation after intrathecal
transplantation of a human neuronal cell line,” Neuroscience
Research, vol. 69, no. 2, pp. 111–120, 2011.
[229] M. J. Eaton, J. A. Plunkett, M. A. Martinez, S. Karmally, and
K. Montanez, “Changes in GAD and GABA immunoreactivity in the spinal dorsal horn after peripheral nerve injury and
promotion of recovery by lumbar transplant of immortalized
serotonergic precursors,” Journal of Chemical Neuroanatomy,
vol. 16, no. 1, pp. 57–72, 1998.
[230] N. A. Calcutt, “Potential mechanisms of neuropathic pain in
diabetes,” International Review of Neurobiology, vol. 50, pp.
205–228, 2002.
[231] T. Z. Fischer, A. M. Tan, and S. G. Waxman, “Thalamic
neuron hyperexcitability and enlarged receptive fields in the
�Pain Research and Treatment
[232]
[233]
[234]
[235]
[236]
[237]
[238]
[239]
[240]
[241]
[242]
[243]
[244]
[245]
STZ model of diabetic pain,” Brain Research, vol. 1268, no. C,
pp. 154–161, 2009.
T. Z. Fischer and S. G. Waxman, “Neuropathic pain in
diabetes—evidence for a central mechanism,” Nature Reviews
Neurology, vol. 6, no. 8, pp. 462–466, 2010.
S. Shapiro, “Neurotransmission by neurons that use serotonin, noradrenaline, glutamate, glycine, and γ-aminobutyric acid in the normal and injured spinal cord,” Neurosurgery, vol. 40, no. 1, pp. 168–177, 1997.
B. C. Hains, A. W. Everhart, S. D. Fullwood, and C. E. Hulsebosch, “Changes in serotonin, serotonin transporter expression and serotonin denervation supersensitivity: involvement
in chronic central pain after spinal hemisection in the rat,”
Experimental Neurology, vol. 175, no. 2, pp. 347–362, 2002.
B. Zhang, M. E. Goldberger, and M. Murray, “Proliferation
of SP- and 5HT-containing terminals in lamina II of rat
spinal cord following dorsal rhizotomy: quantitative EMimmunocytochemial studies,” Experimental Neurology, vol.
123, no. 1, pp. 51–63, 1993.
B. C. Hains, W. D. Willis, and C. E. Hulsebosch, “Serotonin
receptors 5-HT1A and 5-HT3 reduce hyperexcitability of
dorsal horn neurons after chronic spinal cord hemisection
injury in rat,” Experimental Brain Research, vol. 149, no. 2,
pp. 174–186, 2003.
Y. Saruhashi, W. Young, and R. Perkins, “The recovery of 5HT immunoreactivity in lumbosacral spinal cord and locomotor function after thoracic hemisection,” Experimental
Neurology, vol. 139, no. 2, pp. 203–213, 1996.
M. G. Ribotta, J. Provencher, D. Feraboli-Lohnherr, S.
Rossignol, A. Privát, and D. Orsal, “Activation of locomotion
in adult chronic spinal rats is achieved by transplantation of
embryonic raphe cells reinnervating a precise lumbar level,”
Journal of Neuroscience, vol. 20, no. 13, pp. 5144–5152, 2000.
D. Feraboli-Lohnherr, D. Orsal, A. Yakovleff, M. G. Ribotta,
and A. Privat, “Recovery of locomotor activity in the
adult chronic spinal rat after sublesional transplantation of
embryonic nervous cells: specific role of serotonergic neurons,” Experimental Brain Research, vol. 113, no. 3, pp. 443–
454, 1997.
L. M. Ramer, E. Au, M. W. Richter, J. Liu, W. Tetzlaff, and A. J.
Roskams, “Peripheral olfactory ensheathing cells reduce scar
and cavity formation and promote regeneration after spinal
cord injury,” The Journal of Comparative Neurology, vol. 473,
no. 1, pp. 1–15, 2004.
M. J. Eaton, E. Widerström-Noga, and S. Q. Wolfe, “Subarachnoid transplant of a human neuronal serotonergic cell
line attenuates chronic allodynia and hyperalgesia without
affecting motor dysfunction after severe contusive spinal cord
injury,” Neurology Research International, vol. 2011, Article
ID 891605, 24 pages, 2011.
P. A. Walker, M. T. Harting, S. K. Shah et al., “Progenitor cell
therapy for the treatment of central nervous system injury: a
review of the state of current clinical trials,” Stem Cells International, vol. 2010, Article ID 369578, 8 pages, 2010.
J. Hernándeza, A. Torres-Espı́na, and X. Navarro, “Adult stem
cell transplants for spinal cord injury repair: current state in
preclinical research,” Current Stem Cell Research and Therapy,
vol. 6, no. 3, pp. 273–287, 2011.
C. V. Borlongan, C. McWhirter, C. Fultz-Carver et al., “The
case for an ethics research consortium for emerging technologies: public perception of stem cell research and development,” Technology and Innovation, vol. 12, pp. 21–28, 2010.
B. C. Hains, K. M. Chastain, A. W. Everhart, D. J. McAdoo,
and C. E. Hulsebosch, “Transplants of adrenal medullary
chromaffin cells reduce forelimb and hindlimb allodynia in
21
[246]
[247]
[248]
[249]
[250]
[251]
[252]
[253]
[254]
[255]
[256]
[257]
[258]
[259]
a rodent model of chronic central pain after spinal cord
hemisection injury,” Experimental Neurology, vol. 164, no. 2,
pp. 426–437, 2000.
M. Guenot, J. W. Lee, F. Nasirinezhad, and J. Sagen, “Deafferentation pain resulting from cervical posterior rhizotomy
is alleviated by chromaffin cell transplants into the rat spinal
subarachnoid space,” Neurosurgery, vol. 60, no. 5, pp. 919–
925, 2007.
M. D. Lindner, J. M. Francis, P. E. McDermott et al.,
“Numerous adrenal chromaffin cell preparations fail to
produce analgesic effects in the formalin test or in tests of
acute pain even with nicotine stimulation,” Pain, vol. 88, no.
2, pp. 177–188, 2000.
X. T. Wang, J. R. Unnerstall, T. Ibuki, H. Wang, and G. D.
Pappas, “Comparison of tyrosine hydroxylase and preproenkephalin expression in rat adrenal medullary explants in
vitro and transplanted into subarachnoid space,” Experimental Neurology, vol. 161, no. 1, pp. 346–360, 2000.
U. Herzberg, A. Hama, and J. Sagen, “Spinal subarachnoid
adrenal medullary transplants reduce hind paw swelling and
peripheral nerve transport following formalin injection in
rats,” Brain Research, vol. 1198, pp. 85–92, 2008.
J. D. Ortega, J. Sagen, and G. D. Pappas, “Survival and integration of bovine chromaffin cells transplanted into rat
central nervous system without exogenous trophic factors,”
The Journal of Comparative Neurology, vol. 323, no. 1, pp. 13–
24, 1992.
K. A. Czech, J. W. Ryan, J. Sagen, and G. D. Pappas, “The
influence of xenotransplant immunogenicity and immunosuppression on host MHC expression in the rat CNS,”
Experimental Neurology, vol. 147, no. 1, pp. 66–83, 1997.
I. Decosterd, E. Buchser, N. Gilliard, J. Saydoff, A. D. Zurn,
and P. Aebischer, “Intrathecal implants of bovine chromaffin cells alleviate mechanical allodynia in a rat model of
neuropathic pain,” Pain, vol. 76, no. 1-2, pp. 159–166, 1998.
J. C. Sol, R. Y. Li, B. Sallerin et al., “Intrathecal grafting
of porcine chromaffin cells reduces formalin-evoked c-Fos
expression in the rat spinal cord,” Cell Transplantation, vol.
14, no. 6, pp. 353–365, 2005.
Y. Lu, R. Jing, D. C. Yeomans, and G. D. Pappas, “Porcine
chromaffin cells, culture, and transplant for antinociceptive
effects in rodents and primates,” Neurological Research, vol.
26, no. 7, pp. 707–712, 2004.
W. Yu, J. X. Haoa, X. J. Xu et al., “Immunoisolating encapsulation of intrathecally implanted bovine chromaffin cells
prolongs their survival and produces anti-allodynic effect in
spinally injured rats,” European Journal of Pain, vol. 2, no. 2,
pp. 143–151, 1998.
M. D. Lindner, J. M. Francis, M. A. Plone et al., “The analgesic
potential of intraventricular polymer-encapsulated adrenal
chromaffin cells in a rodent model of chronic neuropathic
pain,” Experimental and Clinical Psychopharmacology, vol. 8,
no. 4, pp. 524–538, 2000.
T. Moustafa, S. Girod, F. Tortosa et al., “Viability and functionality of bovine chromaffin cells encapsulated into alginate-PLL microcapsules with a liquefied inner core,” Cell
Transplantation, vol. 15, no. 2, pp. 121–133, 2006.
S. R. Winn and D. F. Emerich, “Managing chronic pain
with encapsulated cell implants releasing catecholamines and
endogenous opiods,” Frontiers in Bioscience, vol. 10, no. 1, pp.
367–378, 2005.
Y. M. Elcin, A. E. Elcin, and G. D. Pappas, “Functional and
morphological characteristics of bovine adrenal chromaffin cells on macroporous poly(D,L-lactide-co-glycolide) scaffolds,” Tissue Engineering, vol. 9, no. 5, pp. 1047–1056, 2003.
�22
[260] J. C. Sol, S. Larrue, R. Y. Li et al., “Intrathecal grafting of
porcine chromaffin cells in the rat reduce nociception in a
tonic pain model,” Experimental Neurology, vol. 175, article
433, 2002.
[261] J. C. Sol, B. Sallerin, S. Larrue et al., “Intrathecal xenogeneic
chromaffin cell grafts reduce nociceptive behavior in a rodent
tonic pain model,” Experimental Neurology, vol. 186, no. 2,
pp. 198–211, 2004.
[262] Y. M. Kim, K. H. Kwak, J. O. Lim, and W. Y. Baek, “Reduction
of allodynia by intrathecal transplantation of microencapsulated porcine chromaffin cells,” Artificial Organs, vol. 33, no.
3, pp. 240–249, 2009.
[263] J. T. Hansen, M. F. D. Notter, S. H. Okawara, and D. M. Gash,
“Organization, fine structure, and viability of the human
adrenal medulla: considerations for neural transplantation,”
Annals of Neurology, vol. 24, no. 5, pp. 599–609, 1988.
[264] H. Zhou, J. Aziza, J. C. Sol et al., “Cell therapy of pain: characterization of human fetal chromaffin cells at early adrenal
medulla development,” Experimental Neurology, vol. 198, no.
2, pp. 370–381, 2006.
[265] W. Yu, J. X. Hao, X. J. Xu et al., “Long-term alleviation
of allodynia-like behaviors by intrathecal implantation of
bovine chromaffin cells in rats with spinal cord injury,” Pain,
vol. 74, no. 2-3, pp. 115–122, 1998.
[266] J. Tkaczuk, J. C. Bes, H. de Bouet du Portal et al., “Intrathecal
allograft of chromaffin cells for intractable pain treatment:
a model for understanding CNS tolerance mechanisms in
humans,” Transplantation Proceedings, vol. 29, no. 5, pp.
2356–2357, 1997.
[267] J. M. Joseph, M. B. Goddard, J. Mills et al., “Transplantation
of encapsulated bovine chromaffin cells in the sheep subarachnoid space: a preclinical study for the treatment of
cancer pain,” Cell Transplantation, vol. 3, no. 5, pp. 355–364,
1994.
[268] H. Wang and J. Sagen, “Attenuation of pain-related hyperventilation in adjuvant arthritic rats with adrenal medullary
transplants in the spinal subarachnoid space,” Pain, vol. 63,
no. 3, pp. 313–320, 1995.
[269] M. D. Lindner, B. R. Frydel, J. M. Francis, and C. K. Cain,
“Analgesic effects of adrenal chromaffin allografts: contingent
on special procedures or due to experimenter bias?” Journal
of Pain, vol. 4, no. 2, pp. 64–73, 2003.
[270] M. D. Lindner, “Clinical attrition due to biased preclinical
assessments of potential efficacy,” Pharmacology and Therapeutics, vol. 115, no. 1, pp. 148–175, 2007.
[271] M. D. Lindner, J. M. Francis, and J. A. Saydoff, “Erratum:
intrathecal polymer-encapsulated bovine adrenal chromaffin
cells fail to produce analgesic effects in the hotplate and
formalin test (Experimental Neurology (2000) 165:2 (370383)),” Experimental Neurology, vol. 170, no. 1, p. 225, 2001.
[272] S. Wu, C. Ma, G. Li, M. Mai, and Y. Wu, “Intrathecal implantation of microencapsulated PC12 cells reduces cold allodynia in a rat model of neuropathic pain,” Artificial Organs, vol.
35, no. 3, pp. 294–300, 2011.
[273] H. H. Wu, S. C. McLoon, and G. L. Wilcox, “Antinociception
following implantation of AtT-20 and genetically modified
AtT-20/hENK cells in rat spinal cord,” Journal of Neural
Transplantation and Plasticity, vol. 4, no. 1, pp. 15–26, 1993.
[274] M. Hino, T. Ogata, T. Morino, H. Horiuchi, and H.
Yamamoto, “Intrathecal transplantation of autologous macrophages genetically modified to secrete proenkephalin
ameliorated hyperalgesia and allodynia following peripheral
nerve injury in rats,” Neuroscience Research, vol. 64, no. 1, pp.
56–62, 2009.
Pain Research and Treatment
[275] L. A. White and S. R. Whittemore, “Immortalization of raphe
neurons: an approach to neuronal function in vitro and in
vivo,” Journal of Chemical Neuroanatomy, vol. 5, no. 4, pp.
327–330, 1992.
[276] L. A. White, R. W. Keane, and S. R. Whittemore, “Differentiation of an immortalized CNS neuronal cell line decreases
their susceptibility to cytotoxic T cell lysis in vitro,” Journal of
Neuroimmunology, vol. 49, no. 1-2, pp. 135–143, 1994.
[277] S. R. Whittemore, L. A. White, L. S. Shihabuddin, and M.
J. Eaton, “Phenotypic diversity in neuronal cell lines derived
from raphe nucleus by retroviral transduction,” Methods, vol.
7, no. 3, pp. 285–296, 1995.
[278] H. K. Raymon, S. Thode, J. Zhou et al., “Immortalized
human dorsal root ganglion cells differentiate into neurons
with nociceptive properties,” Journal of Neuroscience, vol. 19,
no. 13, pp. 5420–5428, 1999.
[279] M. J. Eaton, L. Vaysse, J. P. Herman et al., “Creation of
immortalized chromaffin cell lines for clinical applications,”
IRPCA Advances and Research Updates, vol. 9, no. 1, pp. 13–
26, 2007.
[280] W. R. Galpern, L. H. Burns, T. W. Deacon, J. Dinsmore,
and O. Isacson, “Xenotransplantation of porcine fetal ventral
mesencephalon in a rat model of Parkinson’s disease: functional recovery and graft morphology,” Experimental Neurology, vol. 140, no. 1, pp. 1–13, 1996.
[281] J. C. Bes and J. Sagen, “Dissociated human embryonic and
fetal adrenal glands in neural stem cell culture system: open
fate for neuronal, nonneuronal, and chromaffin lineages?”
Annals of the New York Academy of Sciences, vol. 971, pp. 563–
572, 2002.
[282] C. E. Goodfellow, S. E. Graham, M. Dragunow, and M. Glass,
“Characterization of NTera2/D1 cells as a model system for
the investigation of cannabinoid function in human neurons
and astrocytes,” Journal of Neuroscience Research, vol. 89, no.
10, pp. 1685–1697, 2011.
[283] J. Eaton and Y. Berrocal, “Potential for cell-transplant therapy
with human neuronal precursors to treat neuropathic pain in
models of PNS and CNS injury: comparison of hNT2.17 and
hNT2.19 cell lines,” Pain Research Treatment. In press.
[284] S. C. Quintero Wolfe, N. Cumberbatch, I. Menendez, M.
Martinez, and M. Eaton, “Intrathecal transplantation of a
human neuronal cell line for the treatment of neuropathic
pain in a spinal cord injury model,” Clinical Neurosurgery,
vol. 54, pp. 220–225, 2007.
[285] M. J. Eaton, “Development of human cell therapy for functional recovery following SCI,” The Journal of Spinal Cord
Medicine, vol. 27, article 155, 2004.
�
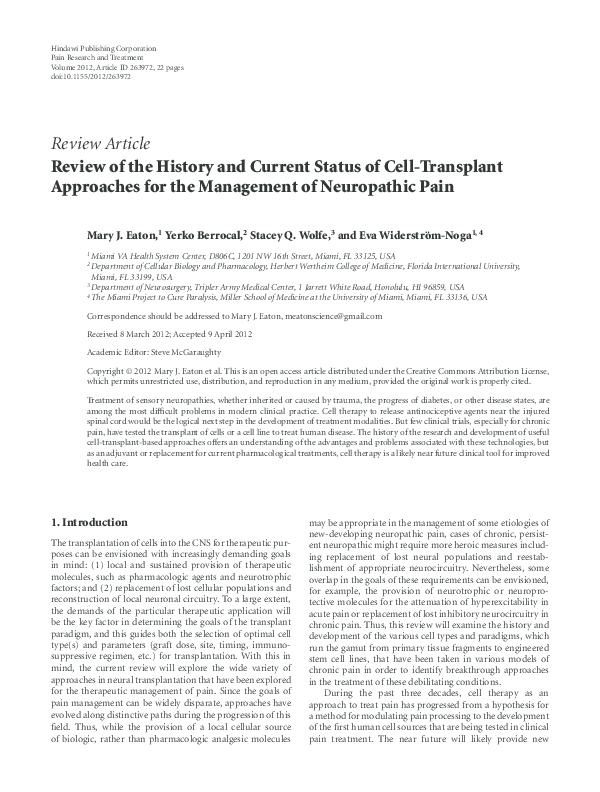
 Stacey Wolfe
Stacey Wolfe