DEPRESSION
AND
ANXIETY 25:27–37 (2008)
Research Article
USE OF HEALTH SERVICES FOR MAJOR DEPRESSIVE
AND ANXIETY DISORDERS IN FINLAND
J. Hämäläinen, M.D., M.A.,1,2� E. Isometsä, M.D., Ph.D.,1,3 S. Sihvo, Ph.D.,4 S. Pirkola, M.D., Ph.D.,4
and O. Kiviruusu, B.Soc.Sc1
Factors associated with people suffering from major depressive disorder (MDD)
or anxiety disorders seeking or receiving treatment are not well known. In the
Health 2000 Study, a representative sample (n 5 6005) of Finland’s general
adult (Z30 years) population was interviewed with the M-CIDI for mental
disorders and health service use for mental problems during the last 12 months.
Predictors for service use among those with DSM-IV MDD (n 5 298) or anxiety
disorders (n 5 242) were assessed. Of subjects with MDD, anxiety disorders, or
both, 34%, 36%, and 59% used health services, respectively. Greater severity
and perceived disability, psychiatric comorbidity, and living alone predicted
health care use for MDD subjects, and greater perceived disability, psychiatric
comorbidity, younger age, and parent’s psychiatric problems for anxiety disorder
subjects. The use of specialist-level mental health services was predicted by
psychiatric comorbidity, but not characteristics of the disorders per se. Perceived
disability and comorbidity are factors influencing the use of mental health
services by both anxiety disorder and MDD subjects. However, still only
approximately one-half of those suffering from even severe and comorbid
disorders use health services for them. Depression and Anxiety 25:27–37, 2008.
& 2007 Wiley-Liss, Inc.
Key words: health care utilization; major depressive disorder; anxiety
disorders; general population
INTRODUCTION
Depressive and anxiety disorders are common and
have a substantial impact on functioning and quality
of life [Lopez and Murray, 1998]. The efficacy and
effectiveness of pharmacological and psychotherapeutic
treatments for these disorders have been established
and numerous evidence-based practice guidelines for
treatment exist [Hyler, 2002; NHS, Depression 2004;
NHS, Anxiety, 2004]. However, it is similarly well
established by epidemiological studies worldwide that
about half of the subjects suffering from severe forms
of these disorders and more than half of those with
moderate or mild disorders do not seek or receive
treatment from health services [Kessler, 2005].
Previous studies [Leaf et al., 1988; Bassett et al.,
1998; Lefebvre et al., 1998; Ten Have et al., 2002]
have suggested that severity of the psychiatric symptoms, psychiatric comorbidity, available resources, and
different health behavior patterns influence seeking
r 2007 Wiley-Liss, Inc.
1
National Public Health Institute, Department of Mental Health
and Alcohol Research, Helsinki, Finland
2
Helsinki City Health Department, Eastern Health Centre,
Department of Psychiatry, Helsinki, Finland
3
Department of Psychiatry, University of Helsinki, Helsinki,
Finland
4
STAKES, National Research and Development Centre for
Welfare and Health, Helsinki, Finland
Contract grant sponsor: Helsinki City Health Department.
�Correspondence to: Juha Hämäläinen, National Public Health
Institute, Department of Mental Health and Alcohol Research,
Mannerheimintie 166, 00300 Helsinki, Finland.
E-mail: Juha.Hamalainen@ktl.fi
Received for publication 14 February 2006; Revised 5 July 2006;
Accepted 18 July 2006
DOI 10.1002/da.20256
Published online 19 January 2007 in Wiley InterScience (www.
interscience.wiley.com).
�28
Hämäläinen et al.
treatment. Also, different sociodemographic factors
may have an influence on help-seeking [Olfson and
Klerman, 1992; Crow et al., 1994; Lin and Parikh,
1999]. Although several recommendations and consensus statements have been produced in order to
define the role of general and specialist psychiatric
health care services [Alonso et al., 2004], little is known
about the factors affecting the actual flow of patients in
the health care system.
The availability of pharmaco- and psychotherapies
for depressive and anxiety disorders have improved
over the last few years. Epidemiological information on
treatment therefore will rapidly become outdated.
Treatment-seeking behavior is affected by changes in
both treatment provision practices and public awareness of acceptability, accessibility, and usefulness of
treatments. As these factors vary from one setting
to another and over time, information from different
countries with differing health care systems is useful
for a comprehensive epidemiological view. For purposes
of public health evaluation, only relatively recent
information on service provision is valuable.
Previous Finnish studies have reported that in 1996
the proportion of subjects in the general population
with a major depressive episode who used any health
services for their depression during the past 12 months
was only 28% [Laukkala et al., 2001; Hämäläinen et al.,
2004]. Whether this finding remains true is unknown.
Furthermore, studies focusing on individual disorders
may not provide the whole picture, as comorbidity is
common and may influence help-seeking behavior.
Knowledge about possible urban/rural residence and
other sociodemographic differences in the use of health
care services for mental disorders is important for
developing these services. To date, however, only a few
nationwide studies on health service use for comorbid
depressive and anxiety disorders have been carried out
[Regier et al., 1993; Bebbington et al., 2000; Alonso
et al., 2004; Wang et al., 2005].
Our aim was to investigate patterns of use of health
care services for major depressive disorder (MDD) and
anxiety disorders, and possible differences between
those two groups, in Finland using a nationally
representative survey from 2000/2001. Our particular
interest was in investigating the impact of disorder
severity, mental disorder comorbidity, concurrent
somatic illnesses, sociodemographic factors, and
patterns of health behavior on health service use
for mental health problems. We also investigated
factors influencing the distribution of patients between
primary and specialized care.
MATERIALS AND METHODS
This study is based on a multidisciplinary epidemiological study, the Health 2000 Study, conducted in
2000–2001 in Finland. The two-stage stratified clustersampling frame comprised 8028 adults age 30 years and
over living in mainland Finland. This frame was
Depression and Anxiety DOI 10.1002/da
regionally stratified according to the five university
hospital regions, each serving approximately one
million inhabitants. The data collection phase started
in August 2000 and was completed in March 2001, with
a total of 7415 subjects attending one or another phase
of the study. Data were collected by home interviews
and examinations, telephone interviews, and health
questionnaires, followed by a clinical health examination including a structured mental health interview.
Details and the methodology of the project have been
published elsewhere [Aromaa and Koskinen, 2003;
Pirkola et al., 2005].
CIDI INTERVIEW
A Finnish-translation of the German computerized
version of the CIDI (Composite International Diagnostic Interview) (M-CIDI) [Wittchen et al., 1998] was
performed on 6038 subjects (95% of those attending
the comprehensive health examination phase), 33 of
whom were subsequently excluded for interviewee
unreliability (e.g., mental retardation, self-expressed
intention to lie). The total number of included interviews was thus 6005, which is 75% of the original
sample. The mental health interview was carried out
at the end of the comprehensive health examination.
Interviews were conducted to determine the 12-month
prevalences of major depressive episodes and disorder,
dysthymia, general anxiety disorder, panic disorder
with or without agoraphobia, agoraphobia, social
phobia, alcohol abuse, and alcohol dependence. For a
detailed description of the CIDI procedure, see Pirkola
et al. [2005].
MENTAL DISORDERS AND THEIR
COMORBIDITY
The available DSM-IV diagnoses were grouped into
the two categories of MDD and anxiety disorders
(including generalized anxiety disorder, agoraphobia,
panic disorder with or without agoraphobia, and social
phobia) [Pirkola et al., 2005]. Information about MDD
included its severity, duration, recurrence, and resulting subjective disability. For anxiety disorders, information included severity and subjective disability. In
addition to MDD and four different anxiety disorders,
we collected data on dysthymia, alcohol disorders, and
smoking status. We studied comorbidity of MDD and
an anxiety disorder within the last 12 months. The
severity of MDD was assessed on the basis of the
number (5–9) of depressive symptoms described by the
subject and divided into three categories: mild (5),
moderate (6, 7), and severe (8, 9). As we had no
information about the duration of the current major
depressive episode, we used the duration of the most
severe lifetime episode (in weeks) and the duration of
depressive symptoms (in years) as proxy variables. The
severity of anxiety disorders was classified on the basis
of both the number of pertinent anxiety symptoms
and the presence of avoidance into three grades (mild,
�Research Article: Health Service Use for Depression and Anxiety
few symptoms and small avoidance; moderate, many
symptoms or great avoidance; and severe, many
symptoms and great avoidance). Further, information
was collected on the respondent’s subjective disability
related to MDD or anxiety disorders (four categories:
major, moderate, slight, and none).
SOCIODEMOGRAPHIC AND HEALTH
BEHAVIOR FACTORS
Information on basic sociodemographic variables was
collected in the interview. These variables included age,
sex, marital status, current employment status, education, whether respondents reside in a rural or urban
location, presence and number of chronic somatic
disorders, and whether the subjects parents had
psychiatric problems (e.g., schizophrenia, other
psychosis, or depression) in his/her childhood. Level
of education and employment status were classified
into three categories and professional status into four.
Subjects with alcohol use disorders fulfilled the
diagnostic criteria of alcohol dependence or alcohol
abuse during the last 12 months. Subjects were
considered smokers if they reported current daily
smoking of cigarettes, cigars, or a pipe and having
smoked at least 100 times during their lifetime. The
variables used to assess different diagnoses, sociodemographic factors, health behaviors, and somatic
health (self-informed presence and number of somatic
long-term illnesses) have been described in detail
previously [Pirkola et al., 2005].
USE OF MENTAL HEALTH SERVICES
Questions about health service use for mental
problems during the past year (yes/no) covered use of
specialist-level mental health services (including municipal services of psychiatric outpatient clinics, mental
health centers, psychiatric hospitals, and private
psychiatrists) and primary health care services (including among others, municipal health centers and
occupational health services). Persons who had used
both psychiatric and primary health services were
classified under special mental health services. Information was also collected on the use of primary health
care services for any reason during the past year.
STATISTICAL METHODS
In the statistical analyses, correlates for use of health
services were first analyzed by basic bivariate analyses,
including the chi-square test. To control for confounding factors, binomial logistic regression analyses were
performed. Values of Po.05 were considered statistically significant. A weighting adjustment was used in
the analyses to take into account the sampling design
and nonparticipation [Aromaa and Koskinen, 2003;
Pirkola et al., 2005]. The STATA statistical package
(College Station, TX, v. 8.0) was used in analyses.
29
Logistic regression analyses with manual backward
elimination procedures was used to choose variables
that would best associate with any health service use for
MDD and anxiety disorders. The use of general versus
special mental health services was analyzed in a similar
manner. Independent variables in the initial models
included sociodemographic factors, severity of MDD
and anxiety disorders, related disability, and all possible
psychiatric comorbidities.
RESULTS
The sample of subjects with MDD (n 5 298)
comprised 93 men (31%) and 205 women (69%). Of
these subjects, 91 (31%) suffered from mild, 155 (52%)
from moderate, and 52 (17%) from severe MDD, and
the median duration of the most severe lifetime episode
was 3, 3, and 12 weeks, respectively. The sample of
subjects suffering from any anxiety disorder (n 5 242)
comprised 95 men (39%) and 147 women (61%). The
number of sufferers of different disorders were: panic
disorder 114 (40%), generalized anxiety disorder 75
(27%), social anxiety disorder 60 (21%), and agoraphobia 33 (12%). Of persons suffering from any
anxiety disorder, 71 (29%) suffered from mild, 106
(44%) from moderate, and 65 (27%) from severe
disorder. Sixty-six individuals (22% of persons with
MDD, 27% of persons with any anxiety disorder)
had both MDD and any of the anxiety disorders.
Of the comorbid group, 15 (23%) suffered from mild,
31 (47%) from moderate, and 20 (30%) from severe
MDD. For anxiety disorders, the respective figures
were 17 (26%), 29 (44%), and 20 (30%).
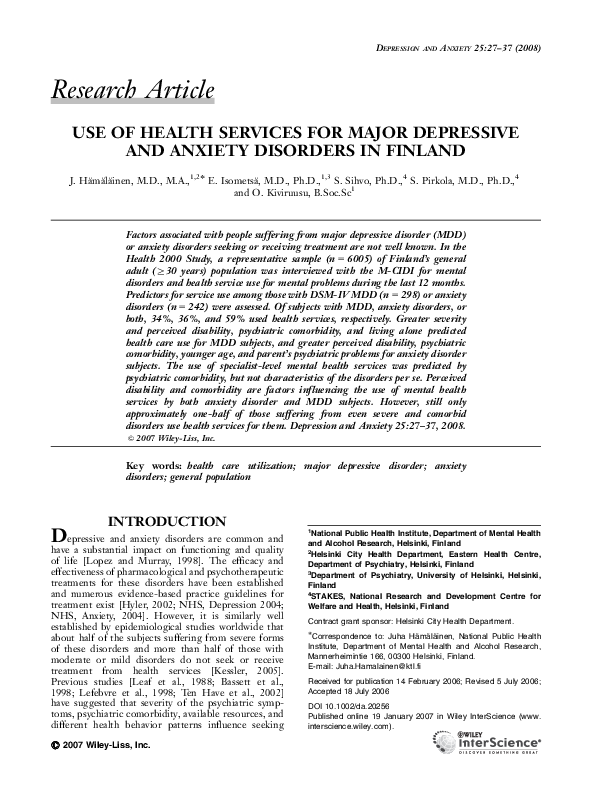
USE OF HEALTH SERVICES
The proportion of subjects classified as having MDD
who used any health services for mental problems
during the past 12 months was 30% for men and 36%
for women. The corresponding proportions for anxiety
disorder were 38% and 35%. For persons having both
MDD and an anxiety disorder the proportion was 58%
(Fig. 1). The relation between use of health services
and sociodemographic factors differed for MDD and
anxiety disorders (Table 1). For MDD and anxiety
disorders, the reported use was higher (32–41%) in the
younger age groups, but somewhat lower (11–21%) in
the older (Z60 years) age group. The difference was
statistically significant both for anxiety disorders (chisquare, P 5.031) and for MDD (chi-square, P 5.000).
The median duration of MDD among all subjects
was 4 weeks, 8 weeks in those using health services, and
3 weeks in nonusers (significant difference, Mann–Whitney U test, P 5.028). The median severity of
the MDD was moderate in both users and nonusers.
The median subjective disability related to depression
was moderate in those using health services and mild in
nonusers. The median severity of anxiety disorders was
Depression and Anxiety DOI 10.1002/da
�30
Hämäläinen et al.
Cases with MDD and/or
Anxiety DO
MDD only
MDD and Anxiety DO
Anxiety DO only
No use of health services
for mental problems
n
231
66
175
%
100
100
100
MDD only
MDD and Anxiety DO
Anxiety DO only
n
167
28
126
%
72
42
72
Use of health services
for mental problems
MDD only
MDD and Anxiety DO
Anxiety DO only
MDD only
MDD and Anxiety DO
Anxiety DO only
n
64
38
49
%
28
58
28
General only
Both general
and specialist
Specialist only
n %
n %
n %
n
29 13
8 12
17 10
14 6
12 18
18 10
21 9
18 27
14 8
35 15
30 45
32 18
Total specialist
%
Figure 1. Use of health services for mental problems with pure major depressive disorder (MDD), persons with MDD and an anxiety
disorder (Anxiety DO) and persons with a pure anxiety disorder during the past 12 months.
moderate in both users and nonusers. The median
subjective disability related to anxiety disorders was
moderate in those using health services and mild in
nonusers. For specific anxiety disorders, the use of
services differed slightly; for panic disorder, the use was
33% (38/114), for social phobia 51% (30/59), for
agoraphobia 39% (13/33), and for generalized anxiety
disorder 43% (32/75). In the final logistic regression
models explaining the use of health services for mental
health reasons (Tables 2, 3), subjective disability and
comorbidity remained significant for both MDD and
anxiety disorders.
ROLE OF SPECIFIC SYMPTOMS
For MDD, specific symptoms of depression were
significantly associated with the use of health care
services. In the preliminary model, an association was
found between use of services and increased appetite,
increased weight, increased sleep, feelings of guilt,
feelings of inferiority, decreased self-confidence,
poor memory, difficulty in making decisions,
thoughts of death, wishing to die, thoughts of suicide,
and plans for suicide. In a logistic regression model
explaining contact with health care services, after
adjusting for severity of MDD, feelings of inferiority
(odds ratio (OR) 2.01, 95% confidence interval (CI):
Depression and Anxiety DOI 10.1002/da
1.24–3.46) and plans for suicide (OR 17.26, 95% CI:
2.10–141.67) remained significant. Due to the small
number of cases, we could not include suicide attempts
in the analysis.
USE OF SPECIALIST-LEVEL SERVICES
Specialist-level mental health services accounted
for 64% (71% for men and 61% for women) of
all health service use associated with MDD and 71%
(72% for men and 71% for women) of use associated
with anxiety disorders. For both groups the age
distribution of use was almost identical, with specialist-level services being used least by the oldest (Z60
years) age group. In a logistic regression model for use
of specialist-level mental health services, (vs. use
of general health services only), the only significant
factor in the final model for MDD was comorbidity
with an anxiety disorder (OR 3.08, 95% CI: 1.21–7.45).
For anxiety disorders comorbidity with MDD was
not significant (OR 1.99, 95% CI: 0.75–5.29). While
specialists tended to see cases that were more severe,
of longer duration, caused more subjective disability,
and generally had more psychiatric comorbidity, the
results were not significant after adjusting for other
factors.
�Research Article: Health Service Use for Depression and Anxiety
31
TABLE 1. Relation of sociodemographic, disorder-specific, and comorbid psychiatric disorder factors and use of
different levels of psychiatric health services for major depressive disorder (MDD) and anxiety disorders during the
past 12 months
No use
Characteristic
%
MDD
Sex
Male
70
Female
64
Age, years
30–39
68
40–49
62
50–59
61
60–
79
Marital status
Unmarried
58
Married
71
Cohabiting
65
Divorced
49
Widowed
84
Employment
Employed
68
Unemployed
55
Retired
68
Student, etc.
62
Education
Low
64
Medium
64
High
70
Living environment
Urban
63
Semi-urban
66
Rural
70
Chronic somatic disorders
No
69
1–2
58
3–
63
Smoking
Yes
59
No
68
Severity of MDD
Mild
76
Moderate
67
Severe
44
Duration of MDD, weeks
0–4
76
5–16
58
17–32
55
33–
54
Subjective disability
Mild
78
Moderate
61
Severe
46
Recurrence of MDD
Single
64
Recurrent
68
Alcohol disorder
Yes
63
No
67
Dysthymia
Yes
49
No
69
General level
Specialist level
Total
n
%
n
%
n
%
n
P�
65
130
9
14
8
29
22
22
20
45
100
100
93
204
0.369
55
64
42
34
11
12
16
12
9
12
11
5
21
27
23
9
17
28
16
4
100
100
100
100
81
104
69
43
0.318
19
110
17
27
21
12
9
19
20
12
4
14
5
11
3
30
21
15
31
4
10
32
4
17
1
100
100
100
100
100
33
156
26
55
25
0.031
124
22
40
08
14
18
7
13
25
7
4
1
19
28
25
31
34
11
15
4
100
100
100
100
183
40
59
13
0.426
74
61
60
10
16
12
12
15
10
26
20
19
30
19
16
100
100
100
116
95
86
0.551
75
78
40
11
14
14
13
16
8
26
20
16
31
24
9
100
100
100
119
118
57
0.592
135
38
22
10
15
20
20
10
7
21
27
17
41
18
6
100
100
100
196
66
35
0.276
43
151
16
11
12
25
25
21
18
46
100
100
73
222
0.323
69
103
23
6
14
19
5
22
10
19
19
37
17
29
19
100
100
100
91
154
52
0.002
107
28
16
26
8
13
14
19
11
6
4
9
16
29
31
27
22
14
9
13
100
100
100
100
140
48
29
48
0.035
107
62
26
9
14
20
12
14
11
14
26
34
19
26
19
100
100
100
138
102
56
0.001
105
90
15
10
24
13
22
22
36
29
100
100
165
132
0.465
38
157
7
14
4
33
30
20
18
46
100
100
60
236
0.087
26
169
13
12
7
30
38
18
20
45
100
100
53
244
0.006
Depression and Anxiety DOI 10.1002/da
�32
Hämäläinen et al.
TABLE 1. Continued
No use
Characteristic
%
Panic disorder
Yes
46
No
67
Social phobia
Yes
29
No
69
Agoraphobia
Yes
38
No
67
GAD
Yes
44
No
68
Any anxiety disorder
Yes
42
No
72
Parental psychiatric problems
Yes
51
No
69
Anxiety disorders
Sex
Male
65
Female
62
Age, years
30–39
61
40–49
58
50–59
59
60–
89
Marital status
Unmarried
60
Married
70
Cohabiting
46
Divorced
52
Widowed
92
Employment
Employed
67
Unemployed
46
Retired
68
Student, etc.
69
Education
Low
58
Medium
57
High
73
Living environment
Urban
62
Semi-urban
60
Rural
77
Chronic somatic disorders
No
66
1–2
63
3–
59
Smoking
Yes
60
No
66
Severity
Mild
70
Moderate
65
Severe
55
General level
Specialist level
Total
n
%
n
%
n
%
n
P�
14
184
8
13
2
35
46
20
11
54
100
100
24
273
0.013
6
187
5
13
1
34
67
19
14
50
100
100
21
271
0.000
3
191
0
13
0
36
63
21
5
60
100
100
8
297
0.027
12
172
19
12
5
29
37
21
10
52
100
100
27
253
0.158
28
167
12
13
8
29
46
15
30
35
100
100
66
231
0.000
21
171
12
13
5
32
37
18
15
45
100
100
41
248
0.024
96
58
10
11
15
10
25
28
36
26
100
100
147
94
0.839
37
49
35
33
15
10
9
8
9
8
5
3
25
32
32
3
15
27
19
1
100
100
100
100
61
84
59
37
0.018
25
85
11
22
11
12
9
21
10
0
5
11
5
4
0
29
21
33
38
8
12
25
8
16
1
100
100
100
100
100
42
121
24
42
12
0.074
80
18
45
11
12
15
8
0
14
6
5
0
22
39
24
31
26
15
16
5
100
100
100
100
120
39
66
16
0.169
42
43
69
11
13
7
8
10
7
31
29
19
22
22
18
100
100
100
72
75
94
0.182
58
64
30
10
12
8
9
13
3
28
28
15
26
30
6
100
100
100
93
107
39
0.408
86
45
23
10
9
15
13
6
6
24
28
26
32
20
10
100
100
100
131
71
39
0.793
52
102
10
10
9
16
30
23
26
36
100
100
87
154
0.528
49
69
36
11
11
8
8
12
5
19
24
37
13
25
24
100
100
100
70
106
65
0.163
Depression and Anxiety DOI 10.1002/da
�Research Article: Health Service Use for Depression and Anxiety
33
TABLE 1. Continued
No use
Characteristic
General level
Total
n
%
n
%
n
%
n
P�
12
138
10
10
3
21
48
21
14
43
100
100
29
202
0.027
19
134
9
11
5
20
56
17
30
32
100
100
54
186
0.000
9
141
21
9
6
19
46
23
13
47
100
100
28
207
0.001
%
Alcohol disorder
Yes
41
No
69
Dysthymia
Yes
35
No
72
Parental psychiatric problems
Yes
32
No
68
Specialist level
GAD, generalized anxiety disorder.
�Pearson chi-square test.
TABLE 2. Logistic regression model of use of health
services for mental problems among respondents
with major depressive disorder (MDD) during the past
12 months
TABLE 3. Logistic regression model of use of health
services for mental problems among respondents with
anxiety disorder during the past 12 months
Variable
Variable
OR
Sex
Female (reference)
1.00
Male
0.62
Age, years
0.98
(continuous)
Living alone
No (reference)
1.00
Yes
1.82
Severity of major depressive episode
Mild (reference)
1.00
Moderate
1.44
Severe
2.44
Subjective disability
Mild (reference)
1.00
Moderate
1.80
Severe
2.81
Comorbid anxiety disorder
No (reference)
1.00
Yes
3.29
95% CI
0.35–1.12
0.96–1.01
1.00–3.29
0.76–2.74
1.10–5.44
0.98–3.28
1.37–5.77
1.81–5.96
OR
Sex
Female (reference)
1.00
Male
1.17
Age, years
0.97
(continuous)
Living alone
No (reference)
1.00
Yes
2.02
Subjective disability
1.00
Mild or moderate
(reference)
Severe
2.36
Comorbid major depressive disorder
No (reference)
1.00
Yes
3.03
Parental psychiatric problems
No (reference)
1.00
Yes
4.18
95% CI
0.62–2.20
0.94–1.00
1.05–3.92
1.26–4.42
1.57–5.85
1.59–11.00
OR, odds ratio; CI, confidence interval.
OR, odds ratio; CI, confidence interval.
DISCUSSION
We found that among individuals suffering from
MDD or an anxiety disorder in Finland, those with
subjectively more disabling and comorbid disorders
used health services more frequently. Use of services
did not, however, differ according to sociodemographic
factors. Of individuals suffering from one disorder, a
considerable proportion (about 2/3) did not receive
treatment, and even for the most severe comorbid cases
only 60% of individuals received treatment. These
poor treatment rates are disappointing in view of the
majority of persons with anxiety and depression having
contacted primary health services for other reasons.
The continuing low rate of treatment-seeking for
mental health problems is also dismaying given that
effective treatments do exist and their availability has
increased. In Finland the personnel resources of health
care system have increased in recent years (e.g., the
number of psychotherapists) and also the variety of
different pharmacotherapies.
In earlier studies, wide variation has emerged in
the rates of treatment-seeking. For depression, the
proportion of treated individuals has ranged from
17.0–77.8% [Bristow and Patten, 2002]. In the most
recent European studies included in the multinational
ESEMeD project [Alonso et al., 2004], use for mood
Depression and Anxiety DOI 10.1002/da
�34
Hämäläinen et al.
disorder subjects was 36.5% and for anxiety disorder
subjects 26.1%. In the Dutch NEMESIS study,
by contrast, 63.8% of persons with mood disorders
received some form of help, with the corresponding
proportion of anxiety disorder subjects being 40.5%
[Bijl and Ravelli, 2000]. Thus, for persons with an
anxiety disorder the proportion seeking treatment may
be lower overall, although considerable variation may
be present among different disorders. In an earlier
Finnish study [Laukkala et al., 2001; Hämäläinen et al.,
2004] the proportion of subjects in the general
population with a major depressive episode who used
any health services for their depression during the past
12 months was slightly smaller, 28%. Due to lack of
information about comorbidity and some methodological differences, these estimates are not fully comparable. Earlier reports have indicated that for panic
disorder and generalized anxiety disorder the use of
medical services is higher than for social and specific
phobias [Bijl and Ravelli, 2000; Olfson et al., 2000].
In our study, medical service usage by our social phobia
subjects was relatively high. This may be related to low
prevalence estimates and possibly more severe social
phobia in our subjects [Pirkola et al., 2005].
IMPACT OF SEVERITY AND COMORBIDITY
Relationships between use of health services and
characteristics of depressive episodes have been investigated in a few previous studies, which have revealed
that more severe and disabling depression is more
likely to be treated [Leaf et al., 1988; Bassett et al.,
1998; Lefebvre et al., 1998; Ten Have et al., 2002].
Consistent with these studies, we found that the level
of functional impairment had an independent effect
on the use of health services. Also for anxiety disorder
subjects, the more severe and disabling the disorder,
the more frequent the use of the services.
Comorbid psychiatric disorders may also affect
the likelihood of treatment for other disorders. The
influence may increase [Goodwin and Andersen, 2002],
as in comorbid affective and anxiety disorders, or
decrease the likelihood of treatment [Roy-Byrne et al.,
2000; Goodwin and Andersen, 2002; Koenen et al.,
2003]. In our data, comorbidity of MDD and anxiety
disorder significantly increased the use of services from
about 20% to 50%. Internationally, comparable results
have been reported. In the Netherlands [Bijl and
Ravelli, 2000], use of any form of services by subjects
with one disorder in the past 12 months was 23.3%,
and by subjects with two or more disorders 55.5%. In
Canada [Kessler et al., 1997] the corresponding figures
were 17.8% and 39.4%, and in the US [Kessler et al.,
1999] 18.8% and 33.9%. Interestingly, the impact of an
alcoholic disorder increased the likelihood of treatment
if the person also had an anxiety disorder, but not
MDD. Earlier, there have been similar findings of
perceived need for help [Mojtabai et al., 2002]. Only a
few studies [Bucholz and Robins, 1987; Dew et al.,
Depression and Anxiety DOI 10.1002/da
1991; Du Fort et al., 1999] have examined whether the
presence of certain specific symptoms of depression is
related to help-seeking; these findings are somewhat
inconsistent. Du Fort et al. [1999] found that suicidal
ideation and psychomotor retardation were associated
with seeking treatment. Our finding of suicidal
planning being significant, even after adjusting for
the severity of MDD, suggests the importance of at
least severe suicidal symptoms in the use of health
services.
SOCIODEMOGRAPHIC FACTORS
The likelihood of depression and anxiety disorders
being treated has been linked to a variety of factors,
including being female, older, separated, divorced or
widowed, unemployed, and better educated [Olfson
and Klerman, 1992; Crow et al., 1994; Lin and Parikh,
1999]. In our subjects, help-seeking for mental
problems was constant up to the age of 60 years, after
which a distinct decrease was observed, consistent with
earlier findings [Roness et al., 2005]. Probable reasons
for the lack of help-seeking later in life include lack
of identification of mental problems, a tendency to
somatize problems, more negative attitudes toward
psychiatry, and lack of specialized mental health
resources in the geriatric health care system. In our
final analysis of health care usage by MDD or anxiety
disorder subjects, no other sociodemographic factor
other than living alone remained statistically significant. At least three previous studies [Lin et al., 1996;
Lefebvre et al., 1998; Bijl and Ravelli, 2000] report
higher service usage among single householders and
unmarried people. Other studies have found either
no such association [Sherbourne, 1988; Golding et al.,
1990; Phillips and Murrell, 1994] or an increasing use
of mental health services but not primary health
services [Ten Have et al., 2002]. It has also been
suggested that both the amount of and the satisfaction
with the social support received may have a protective
effect against service use [Pescosolido et al., 1998; Ten
Have et al., 2002]. The low impact of sociodemographic factors (income, education, etc.) compared
with some previous studies [Kessler et al., 2001] may
reflect the low financial threshold and relatively broad
coverage of mental health services in Finland.
To our knowledge, only a few earlier findings have
been made about an adult subject’s childhood family
environment on subsequent use of services for psychiatric symptoms. Higher rates of perceived need
of treatment have been reported for participants with
a maternal history of mental illness [Mojtabai et al.,
2002]. For MDD, the probability of treatment-seeking
in the proband was observed to be significantly
increased only if the affected relative had themselves
sought treatment for their depression [Kendler, 1995].
We also found a clear connection between one or
both parents having had a psychiatric disorder and the
use of services by anxiety disorder. For MDD, a weaker
�Research Article: Health Service Use for Depression and Anxiety
nonsignificant association was present in the final
model. Theoretically, psychiatric disorders in persons
in the childhood environment may give subjects a
model of how to get treatment for mental suffering
(‘‘social learning’’ model [Bandura, 1986]). In further
analyses, the episodes of depression in this subgroup
of MDD persons proved to be more severe and started
at an earlier age. No such differences were observed in
anxiety disorder persons.
SPECIALIST-LEVEL MENTAL
HEALTH SERVICES
Few studies have compared the characteristics of
people using general or special mental health services
for MDD or anxiety disorders, and the results have
been mixed. These studies have reported 25–40% use
of special mental health services [Kessler et al., 1994;
Wang et al., 2002]. The specialist-level mental health
system has been speculated to treat people with more
severe and complex disorders. The findings, however,
are contradictory. In our study the use of special mental
health services was quite high (2/3 for both MDD and
anxiety disorders), although comparable with the
results of the ESEMeD project [Alonso et al., 2004].
Only psychiatric comorbidity, not disorder severity or
subjective disability, increased the use of special mental
health services markedly (for MDD from 1/7 to 1/2), a
finding consistent with earlier reports. Generally, one
might conclude that the mental health care sector may
be overmeeting needs, i.e., dealing with too many mild
cases that could better be treated in primary care [Bijl
and Ravelli, 2000]. In fact, there is no clear uniform
definition of ‘‘need for services’’ in the population.
Particularly in cases with nonchronic psychiatric
disturbance, people can sometimes successfully cope
with their symptoms and functional disabilities with
support from their nonprofessional social network.
STUDY STRENGTHS AND LIMITATIONS
We used CIDI diagnoses in a relatively large
nationwide subject pool investigating several different
depressive and anxiety disorders, which allowed us
to estimate the effect of comorbidity on the use of
services. The study, however, did have some limitations. As in many other epidemiological studies, we
used self-reports of use of mental health services. For a
number of reasons (including recall bias), self-reported
estimates of use may be lower than the corresponding
data from administrative records [Golding et al., 1988;
Rhodes et al., 2002]. Moreover, we collected only
general information on the ‘‘use of health services for
mental problems.’’ We had no direct information about
the duration of the major depressive episode in the
last year, only about the duration of the most severe
lifetime episode. Nevertheless, the length of different
depressive episodes over the lifetime appears consistent
[Solomon et al., 1997; Spijker et al., 2002]. Due to the
small number of cases, we could not perform analyses
35
on different anxiety disorders to detect possible
intergroup variability. Further, we had no specific
information on the ‘‘attitude’’ factors likely to influence
an individual’s decision to seek professional help for
psychiatric problems (willingness to disclose problems,
fear of stigma, negative stereotypes of treatments,
and other cultural factors) [Christiana et al., 2000;
Collins et al., 2004], or on the delay between symptom
onset and first consultation with a professional (often
6–14 years across anxiety and mood disorders) [Kessler
et al., 1998; Christiana et al., 2000]. We also did not
have information on persons under 30 years. In young
adults the prevalence of disorders and the use of
services may differ from the older age groups studied.
Finally, we did not have information on detection of
mental disorders by general practitioners, although
they are the gatekeepers to mental health services
[Ormel et al., 1991]. The vast majority of individuals
with anxiety and depression contacted primary care at
least once in the past year [Ohayon et al., 2000]. Of our
subject pool, 84% visited a doctor at least once in the
last year, providing an opportunity to detect and
diagnose MDD or anxiety disorder.
REFERENCES
Alonso J, Angermeyer MC, Bernert S, Bruffaert R, Brugha TS,
Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I,
Haro JM, Katz SJ, Kessler RC, Kovess V, Lepine JP, Ormel J,
Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez
S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M,
Domingo-Salvany A, Ferrer M, Joo SS, Martinez-Alonso M,
Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacin C,
Romera B, Taub N, Volleberg WA; ESEMeD/MHEDEA 2000
Investigators, European Study of the Epidemiology of Mental
Disorders (ESEMeD) Project. 2004. Psychotropic drug utilization
in Europe: results from the European Study of the Epidemiology
of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand
Suppl 420:55–64.
Aromaa A, Koskinen S (eds.). 2003. Health and functional capacity in
Finland. Baseline results of the Health 2000. Health Examination
Survey. Helsinki: Publications of the National Public Health
Institute.
Bandura A. 1986. Social foundation of thought and action: a social
cognitive theory. Englewood Cliffs, NJ: Prentice-Hall.
Bassett SS, Chase GA, Folstein MF, Regier DA. 1998. Disability and
psychiatric disorders in an urban community: measurement,
prevalence and outcomes. Psychol Med 28:509–517.
Bebbington PE, Brugha TS, Meltzer H, Jenkins R, Ceresa C, Farrell
M, Lewis G. 2000. Neurotic disorders and the receipt of
psychiatric treatment. Psychol Med 30:1369–1376.
Bijl RV, Ravelli A. 2000. Psychiatric morbidity, service use, and need
for care in the general population: results of the Netherlands
Mental Health and Incidence Study. Am J Public Health 90:
602–607.
Bristow K, Patten S. 2002. Treatment-seeking rates and associated mediating factors among individuals with depression. Can
J Psychiatry 47:660–665.
Bucholz KK, Robins LN. 1987. Who talks to a doctor about existing
depressive illness? J Affect Disord 12:241–250.
Christiana JM, Gilman SE, Guardino M, Mickelson K, Morselli PL,
Olfson M, Kessler RC. 2000. Duration between onset and time of
Depression and Anxiety DOI 10.1002/da
�36
Hämäläinen et al.
obtaining initial treatment among people with anxiety and mood
disorders: an international survey of members of mental health
patient advocate groups. Psychol Med 30:693–703.
Collins KA, Westra HA, Dozois DJ, Burns DD. 2004. Gaps in
accessing treatment for anxiety and depression: challenges for the
delivery of care. Clinl Psychol Rev 24:583–616.
Crow MR, Smith HL, McNamee AH, Piland NF. 1994. Considerations in predicting mental health care use: implications for
managed care plans. J Mental Health Admin 21:5–23.
Dew MA, Bromet EJ, Schulberg HC, Parkinson DK, Curtis EC.
1991. Factors affecting service utilization for depression in a white
collar population. Soc Psychiatry Psychiatr Epidemiol 26:230–237.
Du Fort GG, Newman SC, Boothroyd LJ, Bland RC. 1999.
Treatment seeking for depression: role of depressive symptoms
and comorbid psychiatric diagnoses. J Affect Disord 52:31–40.
Golding JM, Gongla P, Brownell A. 1988. Feasibility of validating
survey self-reports of mental health service use. Am J Community
Psychol 16:39–51.
Golding JM, Karno M, Rutter CM. 1990. Symptoms of major
depression among Mexican-Americans and non-Hispanic whites.
Am J Psychiatry 147:861–866.
Goodwin R, Andersen RM. 2002. Use of the behavioral model of
health care use to identify correlates of use of treatment for panic
attacks in the community. Soc Psychiatry Psychiatr Epidemiol 37:
212–219.
Hyler SE. 2002. APA online CME practice guideline for the treatment opatients with major depressive disorder. J Psychiatr Pract 8:
315–319.
Hämäläinen J, Isometsä E, Laukkala T, Kaprio J, Poikolainen K,
Heikkinen M, Lindeman S, Aro H. 2004. Use of health services
for major depressive episode in Finland. J Affect Disord 79:
105–112.
Kendler KS. 1995. Is seeking treatment for depression predicted by a
history of depression in relatives? Implications for family studies of
affective disorders. Psychol Med 25:807–814.
Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M,
Eshleman S, Wittchen HU, Kendler KS. 1994. Lifetime and
12-month prevalence of DSM-III-R psychiatric disorders in the
United States. Results from the National Comorbidity Survey.
Arch Gen Psychiatry 51:8–19.
Kessler RC, Frank RG, Edlund M, Katz SJ, Lin E, Leaf P. 1997.
Differences in the use of psychiatric outpatient services between
the United States and Ontario. N Engl J Med 336:551–557.
Kessler RC, Olfson M, Berglund PA. 1998. Patterns and predictors
of treatment contact after first onset of psychiatric disorders.
Am J Psychiatry 155:62–69.
Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf
P. 1999. Past-year use of outpatient services for psychiatric
problems in the National Comorbidity Survey. Am J Psychiatry
156:115–123.
Kessler RC, Berglund PA, Bruce ML. 2001. The prevalence and
correlates of untreated serious mental illness. Health Serv Res 36:
987–1007.
Kessler RC, Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I,
Kovess V, Lepine JP, Angermeyer MC, Bernert C, de Girolamo G,
Morosini P, Polidori G, Kikkawa T, Kawakami N, Ono Y,
Takeshima T, Uda H, Karam EG, Fayyad JA, Karam AN,
Mneimneh ZN, Medina-Mora ME, Borges G, Lara C, de Graaf
R, Ormel J, Gureje O, Shen Y, Huang Y, Zhang M, Alonso J, Haro
JM, Vilagut G, Bromet EJ, Gluzman S, Webb C, Kessler RC,
Merikangas KR, Anthony JC, Von Korff MR, Wang PS, Brugha
TS, Aguilar-Gaxiola S, Lee S, Heeringa S, Pennell BE, Zaslavsky
AM, Ustun TB, Chatterji S; WHO World Mental Health Survey
Consortium 2004. Prevalence, severity and unmet need for
Depression and Anxiety DOI 10.1002/da
treatment of mental disorders in the World Health Organization
World Mental Health Surveys. JAMA 291:2581–2590.
Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters
EE, Wang P, Wells KB, Zaslavsky AM. 2005. Prevalence and
treatment of mental disorders 1990 to 2003. N Engl J Med 352:
2515–2523.
Koenen KC, Goodwin R, Struening E, Hellman F, Guardino M.
2003. Posttraumatic stress disorder and treatment seeking in a
national screening sample. J Trauma Stress 16:5–16.
Laukkala T, Isometsä E, Hämäläinen J, Heikkinen M, Lindeman S,
Aro H. 2001. Antidepressant treatment of depression in the
Finnish general population. Am J Psychiatry 158:2077–2079.
Leaf PJ, Bruce ML, Tischler GL, Freeman DH, Weissman MM,
Myers JK. 1988. Factors affecting the utilization of specialty and
general medical mental health services. Med Care 26:9–26.
Lefebvre J, Lesage A, Cyr M, Toupin J, Fournier L. 1998. Factors
related to utilization of services for mental health reasons in
Montreal, Canada. Soc Psychiatry Psychiatr Epidemiol 33:291–298.
Lin E, Parikh SV. 1999. Sociodemographic, clinical, and attitudinal
characteristics of the untreated depression in Ontario. J Affect
Disord 53:153–162.
Lin E, Goering P, Offord DR, Campbell D, Boyle MH. 1996. The
use of mental health services in Ontario: epidemiological findings.
Can J Psychiatry 41:572–577.
Lopez AD, Murray C. 1998. The global burden of disease, 19902020. Nat Med 4:1241–1243.
Mojtabai R, Olfson M, Mechanic D. 2002. Perceived need and helpseeking in adults with mood, anxiety or substance use disorders.
Arch Gen Psychiatry 59:77–84.
NHS, Depression. Management of depression in primary and
secondary care. Clinical Guideline 23, December 2004 (www.nice.
org.uk/CG022NICEguideline). [Accessed 15 December 2004.]
NHS, Anxiety. Management of anxiety (panic disorder, with or
without agoraphobia, and generalized anxiety disorder) in adults in
primary, secondary and community care. Clinical Guideline 22,
December 2004 (www.nice.org.uk/CG022NICEguideline). [Accessed 22 December 2004.]
Ohayon MM, Shapiro CM, Kennedy SH. 2000. Differentiating
DSM-IV anxiety and depressive disorders in the general population: comorbidity and treatment consequences. Can J Psychiatry 45:
166–172.
Olfson M, Klerman GL. 1992. Depressive symptoms and mental
health service utilization in a community sample. Soc Psychiatry
Psychiatr Epidemiol 27:161–167.
Olfson M, Guardino M, Struening E, Schneier FR, Hellman F,
Klein DF. 2000. Barriers to the treatment of social anxiety. Am J
Psychiatry 157:521–527.
Ormel J, Koeter MW, Van Den Brink W, Van De Willige G. 1991.
Recognition, management, and course of anxiety and depression in
the general practice. Arch Gen Psychiatry 48:700–706.
Pescosolido BA, Wright ER, Alegria M, Vera M. 1998. Social
networks and patterns of use among the poor with mental health
problems in Puerto Rico. Med Care 36:1057–1072.
Phillips MA, Murrell SA. 1994. Impact of psychological and physical
health, stressful events and social support on subsequent mental
health help seeking among older adults. J Consult Clin Psychol 62:
270–275.
Pirkola SP, Isometsä E, Suvisaari J, Joukamaa M, Poikolainen K,
Koskinen S, Aromaa A, Lonnqvist JK. 2005. DSM-IV moodanxiety- and alcohol use disorders and their comorbidity in the
Finnish general population. Soc Psychiatry Psychiatr Epidemiol
40:1–10.
Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ,
Goodwin FK. 1993. The de facto US Mental and Addictive
�Research Article: Health Service Use for Depression and Anxiety
Disorders Service System: Epidemiologic Catchment Area prospective 1-year prevalence rates of disorders and services. Arch Gen
Psychiatry 50:85–94.
Rhodes AE, Lin E, Mustard CA. 2002. Self-reported use of mental
health services versus administrative records: should we care?
Int J Met Psych Res 11:125–133.
Roness A, Mykletun A, Dahl AA. 2005. Help-seeking behaviour in
patients with anxiety disorders and depression. Acta Psychiatr
Scand 111:51–58.
Roy-Byrne P, Stang P, Wittchen H, Ustun B, Walters EE, Kessler
RC. 2000. Lifetime panic-depression comorbidity in the National
Comorbidity Survey. Br J Psychiatry 176:229–235.
Sherbourne CD. 1988. The role of social support and life stress
events in use of mental health services. Soc Sci Med 27:1393–1400.
Solomon DA, Keller MB, Leon AC Mueller TI, Shea MT, Warshaw
M, Maser JD, Coryell W, Endicott J. 1997. Recovery from major
depression. A 10-year prospective follow-up across multiple
episodes. Arch Gen Psychiatry 54:989–991.
Spijker J, De Graaf R, Bijl RV, Beekman AT, Ormel J, Nolen WA.
2002. Duration of major depressive episodes in the general
37
population: results from the Netherlands Mental Health
Survey and Incidence Study (NEMESIS). Br J Psychiatry 181:
208–213.
Ten Have M, Wollebergh W, Bijl R, Ormel J. 2002. Combined effect
of mental disorders and low social support on care service use for
mental health problems in the Dutch general population. Psychol
Med 32:311–323.
Wang PS, Demier O, Kessler RC. 2002. Adequacy of treatment for
serious mental illness in the United States. Am J Public Health
92:92–98.
Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC.
2005. Twelve-month use of mental health services in the United
States. Arch Gen Psychiatry 62:629–640.
Wittchen HU, Lachner G, Wunderlich U. 1998. Test-retest
reliability of the computerized DSM-IV version of the MunichComposite International Diagnostic Interview (M-CIDI). Soc
Psychiatry Psychiatr Epidemiol 33:568–578.
Young AS, Klap R, Sherbourne CD, Wells KB. 2001. The quality of
care for depressive and anxiety disorders in the United States.
Arch Gen Psychiatry 58:55–61.
Depression and Anxiety DOI 10.1002/da
View publication stats
�
 Sami Pirkola
Sami Pirkola