EC8073- Medical Electronics
V Semester ECE
UNIT I
ELECTRO-PHYSIOLOGY AND BIO-POTENTIAL RECORDING
1. Define – Conduction Velocity
[A/M – 08], [N/D – 08], [M/J – 07]
Conduction velocity is defined as the rate at which an action potential moves down a fiber or is
propagated from cell to cell. It is also called as Nerve conduction rate.
2. Write down the Nernst equation of action potential.
An equation relating the potential across the membrane and the two concentrations of
the ion is called Nernst equation.
RT
C1 f1
E
ln
nF
C2 f 2
where,
R – Gas constant (8.315 x 107 ergs/mole/degree Kelvin)
T – Absolute Temperature, degrees Kelvin
n – Valence of the ion (the number of electrons added or removed to ionize the atom)
F – Faraday constant (96,500 coulombs)
C1, C2 – Two concentrations of the ion on the two sides of the membrane
f1, f2 – Respective activity coefficients of the ion on the two sides of the membrane
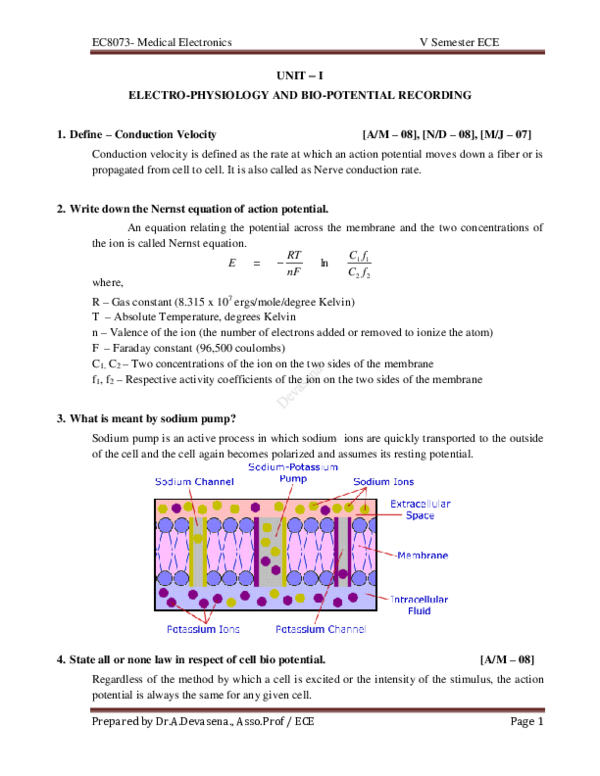
3. What is meant by sodium pump?
Sodium pump is an active process in which sodium ions are quickly transported to the outside
of the cell and the cell again becomes polarized and assumes its resting potential.
4. State all or none law in respect of cell bio potential.
[A/M – 08]
Regardless of the method by which a cell is excited or the intensity of the stimulus, the action
potential is always the same for any given cell.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 1
�EC8073- Medical Electronics
V Semester ECE
5. List the types of bioelectric potentials.
The types of bio electric potentials are
Heart – ElectroCardioGram (ECG)
Brain – ElectroEncephaloGram (EEG)
Muscle – ElectroMyoGram (EMG)
Eye (Retina) – ElectroRetinoGram (ERG)
Eye (Cornea - Retina) – ElectroOculoGram (EOG)
6. Define Electrode and List its types
The devices that convert ionic potential into electronic potential are called as electrode.
The types of electrode are
a) Micro electrode
b) Depth and needle electrode
c) Surface electrode
7. What are perfectly polarized and perfectly non polarized electrodes?
Electrodes in which no net transfer of charge occurs across the metal electrolyte interface is
called perfectly polarized electrode.
Electrodes in which unhindered exchange of charge occurs across the metal electrolyte
interface is called perfectly non polarized electrode.
8. What are the types of electrodes used in bipolar measurement?
[M/J – 12]
The types of electrodes used in bipolar measurement are
i) Limb electrodes
ii) Floating Electrodes
iii) Skin electrodes
9. Name the electrodes used for recording EMG and ECG.
Electrodes used for recording EMG are
i) Needle electrodes
ii) Surface electrodes
Electrodes used for recording ECG are
i) Limb electrodes
ii) Floating Electrodes
iii) Pregelled disposable electrodes
iv) Pasteless electrodes
[N/D – 12]
10. List out the electrodes used for EEG.
Electrodes used for recording EEG are
[M/J – 14]
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 2
�EC8073- Medical Electronics
i)
ii)
iii)
V Semester ECE
Needle electrodes
Surface electrodes
Needle electrode
11. State the importance of biological amplifiers.
[A/M – 10]
Bio signals such as ECG, EMG, EEG, and EOG have low amplitude and low frequency. So,
amplifier is used to boost the amplitude level of bio signals.
12. What are the requirements for bio-amplifiers?
The requirements for bio-amplifiers are
i) High input impedance
ii) Isolation and protection circuit
iii) High voltage gain
iv) Constant gain throughout required bandwidth
v) Low output impedance
vi) High CMRR
13. What are the basic components of biomedical systems?
The basic components of biomedical systems are
i) Patient
ii) Transducer
iii) Signal processing equipment
iv) Display
v) Control unit
vi) Stimulus
14. List the lead systems used in ECG recording.
The lead systems used in ECG recording are
i) Bipolar Limb leads or Standard leads
ii) Augmented unipolar limb leads
iii) Chest leads or precordial leads
[A/M – 10]
15. What is evoked potential?
The external stimuli are detected by the sense organs which cause changes in the electrical activity
of the brain. Due to this, potential is developed in the brain as the response to external stimului
like light, sound etc. It is called as evoked potential.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 3
�EC8073- Medical Electronics
V Semester ECE
[M/J – 12], [N/D – 12]
16. What is PCG?
A Phonocardiogram or PCG is a graphic display of the sounds generated by the heart and
picked up by a microphone at the surface of the body. Frequency response required is 5 to
2000 Hz. It is measured by special transducer or microphone.
17. Compare the signal characteristics of ECG and PCG.
ECG wave occurrence
QRS Complex
End of T wave
Beginning of P wave
[N/D – 11]
PCG wave occurrence
1 heart sound
2nd heart sound
3rd heart sound
st
18. State the importance of PCG signals.
[M/J – 09]
The importance of PCG signals are
i) Different types of heart sounds are measured.
ii) Additional sounds are heard between normal heart sound due to vibration setup in the
blood inside the heart by sudden closure of valves.
iii) The presence of higher frequencies (mumurs) in the phonocardiogram indicates a
possible hear disorder such as Aortic stenosis, Mitral regurgitation, mitral stenosis etc.
19. Define Latency as related to EMG
[N/D – 08]
Latency is defined as the elapsed time between the stimulating impulse and the muscle action
potential. In other words it is the time delay between stimulus and response
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 4
�EC8073- Medical Electronics
V Semester ECE
[N/D – 09], [M/J – 07]
20. Draw typical ECG waveform.
Wave
P
Amplitude (mV)
0.25
Duration (sec)
0.12 – 0.22 (P – R interval)
R
T
QRS Complex
1.06
0.1 – 0.5
-
0.07 – 0.1
0.05 – 0.15 (S – T segment)
0.09
21. What are the important bands of frequencies in EEG and state their importance.
[N/D – 04]
The important bands of frequencies in EEG are
Waves
Frequency (Hz)
Delta(δ)
0.5 – 4
These waves occur in deep sleep in premature babies and
in very serious organic brain disease.
Theta(θ)
4–8
These waves occurs during emotional stress in some adults
particularly during disappointment and frustration
Alpha(α)
8 – 13
They found in the normal persons when they are awake in
a quiet, resting state. During sleep they disappear.
Beta(β)
13- 22
It is observed when the person is alert active, busy, or
anxious thinking, active concentration
Observation
22. What are Intracellular fluid and Extracellular fluid?
The fluid outside the cell membrane is called as Extracellular fluid or External cell fluid (ECF).
The fluid inside the cell membrane is called as intracellular fluid or internal cell fluid (ICF).
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 5
�EC8073- Medical Electronics
V Semester ECE
23. What are the peak amplitude and frequency response for ECG, EEG and EMG?
The peak amplitude and frequency response for ECG, EEG, EMG are
Bioelectric potential
Peak
amplitude
Frequency
response
Records electrical
activity of heart
0.1 to 4mV
0.05 to
120 Hz
ElectroEncephaloGram Records electrical
(EEG)
activity of brain
2 to 200μV
0.1 to 100
Hz
50μV to
1mV
5 to 2000
Hz
ElectroCardioGram
(ECG)
ElectroMyoGram
(EMG)
Function
Records
potential
muscle
Observation
Used to measure
heart rate, arrhythmia
and abnormalities
Used to analysis
evoked
potential,
certain
patterns,
frequency response
Used as indicator of
muscle action for
measuring fatigue
24. The contraction of skeletal muscle is termed as what? Give its specifications.
[M/J – 14]
The contraction of skeletal muscle is termed as Electromyogram.
Specification:
Signal ranges – 0.1 to 0.5 mV
Frequency component – 20 Hz to 10 kHz
The surface electrode picks up many overlapping spikes and produces an average voltage from
various muscles and motor units.
25. Give the chemical composition of ECF and ICF.
The chemical composition of ECF and ICF are, ICF is rich in K+, Mg++, phosphates and ECF is
rich in Na+, Cl−.
26. Discuss about the origin of heart sounds.
With each heart beat the normal heart produces two distinct sounds described as “Lub-Dub”. The
lub is caused by the closure of the atrioventricular valves, which permits flow of blood from the
atria into the ventricles .this is called the first heart sound, it occurs approximately at the time of
the QRS complex of the electrocardiogram. The dub part of the heart sounds is called the second
heart sound and is caused by the closing of the semilunar valves, occurs about the time of the end
of the T wave of the cardiogram. A third heart sound is heard especially in young adults. Atrial
heart sound is not audible and it occurs when the atria do not contract.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 6
�EC8073- Medical Electronics
V Semester ECE
27. What is auscultation?
The technique of listening to sounds produced by organs and vessels of the body is called
auscultation.
28. What is myocardial infarct and angina pectoris?
An obstruction of part of the coronary arteries that supply blood for the heart muscle is called
myocardial infarct or heart attack, whereas merely a reduced flow in the coronary vessels can
cause a severe chest pain called angina pectoris.
29. Give the principle of transduction of heart sounds.
The sounds and murmurs which originate from the heart can be picked up from the chest using
stethoscope or by transduction of heart sounds in to electrical signal.
30. What are tachycardia and bradycardia?
The human hear rate varies normally over a range of 60 to 110 BPM. Rate faster than 110 BPM is
called tachycardia. Heart rate slower than 60 BPM is called bradycardia.
UNIT II
BIO-CHEMICAL AND NON ELECTRICAL PARAMETER MEASUREMENTS
Part A
1. What are the typical values of blood pressure and pulse rate of an adult?
[N/D – 12]
Systolic (maximum) blood pressure in the normal adult is in the range of 95 to145 mm Hg, with 120
mm Hg being average. Diastolic (lowest pressure between beats) blood pressure ranges from 60 to
90 mm Hg, 80 mm Hg being average.
2. What are systolic and diastolic pressures?
[N/D – 16]
The heart’s pumping cycle is divided into two major parts systole and diastole. Systole is defined as
the period of contraction of the heart muscles specifically the ventricular muscle at which time
blood is pumped into the pulmonary artery and the aorta. Systolic pressure is 120 mm Hg(average
value). Diastole is the period of dilation of the heart cavities as they fill with blood. Diastolic
pressure is 80 mm Hg (average value).
3. What is the reason for decrease of cardiac output?
The reason for decrease of cardiac output may be due to low blood pressure, reduced tissue
oxygenation, poor renal function, shock and acidosis.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 7
�EC8073- Medical Electronics
V Semester ECE
4. Define – Cardiac Output
Cardiac output is defined as the amount of blood delivered by the heart to the aorta per minute. In
case of adults during each beat, the amount of blood pumped ranges from 70 to 100 ml. for normal
adults the cardiac output is about 4- 6 liters/ minute.
5. State the principle behind the indicator dilution method.
The indicator dilution method is based on the principle that a known amount of dye or radio isotope
as an indicator is introduced with respect to time at the measurement site, so the volume flow of
blood can be estimated.
6. What is residual volume?
[M/J – 07]
Residual volume is the volume of gas remaining in the lungs at the end of maximum expiration.
7. Define – Tidal Volume
Tidal volume is also called as normal depth volume of breathing or is the volume of gas inspired or
expired during each normal quiet respiration cycle.
8. What is total lung capacity?
[N/D – 17]
The total lung capacity is the amount of gas contained in the lungs at the end of maximal
inspiration.
9. Define – Vital Capacity
The vital capacity (VC) is the maximum volume of gas that can be expelled from the lungs after a
maximal inspiration.
10. What is electrophoresis?
[M/J – 10]
Electrophoresis is a method for separating and analyzing macromolecular substances such as
plasma proteins. The method is based on the fact that, the molecules carry electric charges and
therefore migrate in an electric field.
11. How cardiac output is used?
[N/D – 16]
Using implanted electromagnetic fine probe on the aorta, find the cardiac output per minute
directly can be found by multiplying the stroke volume with the heart beat rate per minute.
12. What are the uses of gas analyzers?
Gas analyzers are used to determine the quantitative composition of inspired and expired gas to
assess the lung function.
13. What are the uses of blood flow meters?
Blood flow meters are used to monitor the blood flow in various blood vessels and to measure
cardiac output.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 8
�EC8073- Medical Electronics
V Semester ECE
14. What are the applications of flame photometer?
[N/D – 16]
The applications of flame photometer are, to analyze urine or blood in order to determine the
concentration of potassium (K), sodium (Na), calcium (Ca) and lithium (Li).
15. What are blood cells?
The blood cells have important functions in our body. The red blood cell is used for the transport of
oxygen and carbon dioxide. The white blood cells are part of the body’s defense against infections
and foreign substances. The platelet is involved in the clotting of blood.
16. What is the purpose PO2 electrode is used?
PO2 electrode is used to determine the oxygen tension in the blood. It is a piece of platinum wire
embedded in an insulating glass holder with the end of wire exposed to the electrolyte into which
the oxygen from the solution under measurement is allowed to diffuse through the membrane.
17. How is auto analyzer useful in medical field?
[A/M – 10], [M/J – 10]
Auto analyzer is used to measure blood chemistry and display that on a graphic recorder.
18. What are korotkoff sounds?
[N/D – 16]
In the Blood pressure (BP) measurement, when the systolic pressure exceeds the cuff pressure, then
the doctor can hear some crashing, snapping sounds through the stethoscope. These sounds are
called as korotkoff sounds.
19. What is cardiac output? What are the methods of measurement of cardiac output?
[N/D – 16]
Cardiac output is the amount of blood delivered by the heart to the aorta per minute. For normal
adult, the cardiac output is 4- 6 litres/min. The cardiac output is measured by using three.
20. What is BRONCHOSPIROMETER?
[M/J – 06]
A bronchospirometer is a dual Spirometer that measures the volumes and capacities of each lung
individually. The air-input device is a double luman tube that divides for entry into the airway to each
lung, and thus provides isolation for differential measurement. The main function of the
bronchospirometer is preoperative evaluation of oxygen consumption of each lung.
21. Define Electrophoresis
[A/M – 10]
Electrophoresis is a method for separating and analyzing macromolecular substances such as
plasma proteins. The method is based on the fact that, the molecules carry electric charges and
therefore migrate in a electric field.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 9
�EC8073- Medical Electronics
V Semester ECE
22. Give the changes in the hemoglobin content of red blood cells.
When the body produces too many red blood cells, the amount of hemoglobin in the blood
increases, and a chronic disease called polycythemia or dehydration is produced. When the
hemoglobin in the blood decreases, anemia is produced.
23. In what way the composition of blood sample is determined?
The composition of blood serum is determined by specialized chemical techniques. The different
components of biological substances can e determined by measuring how they either absorb or
emit visible light.
24. What is flame photometer?
By measuring optical density or absorbance A, the concentration of given substance in the sample
can be determined. Colorimeters can be in the filter photometer or spectrophotometer. When an
interference filter is used to select a given wavelength, it is called filter photometer.
25. Name three methods to obtain the direct measurement of blood pressure.
The three methods to obtain the direct measurement of blood pressure are
i) Percutaneous insertion
ii) Catheterization
iii) Implantation of a transducer.
26. Name the four physical principles based on which blood flow meters are constructed.
[N/D – 07]
The blood flow meter is constructed based on the following principles:
i) Electromagnetic induction.
ii) Ultrasonic principle (Transmit type, Doppler type)
iii) Thermal convection
iv) Radiograpic principle
v) Indicated dilution principle.
27. Define − Pneumotachograph
Pneumotachograph is an instrument to measure the patient’s air flow rate during respiration and
vital air capacity of the lung.
28. Why glass electrode is very much preferred as active electrode in a pH meter?
The glass electrode provides a membrane interface for H+ ions. So that, it is preferred as an
active electrode in pH measurement. The pH meter with hydroscopic glass observes the water
readily and provides best pH value.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 10
�EC8073- Medical Electronics
V Semester ECE
UNIT – III
ASSIST DEVICES AND BIO –TELEMETRY
Part A
1. Give two important factors that demand internal pace maker’s usage.
The two important factors that demand internal pace maker’s usage are
(i). Type and nature of the electrode used
(ii). Nature of the cardiac problems.
(iii). Mode of operation of the pacemaker system.
[A/M – 05]
2. Distinguish between Internal and External pacemakers.
[M/J – 07]
The differences between internal and external pacemakers are
Sl.No
Internal Pacemaker
External Pacemaker
1
The pacemaker is surgically implanted The pacemaker is placed outside the body. It may
beneath the skin near the chest
be in the form of wrist watch or in packet from one
wire go in to heart through the vein.
2
The electrode are called myocardiac The electrode are called endocardiac electrode and
electrode and are in contact with heart are applied to heart
muscle.
3
The battery can be replaced only by minor The battery can be easily replaced any defect or
surgery. Further any defect or adjustment adjustment in the circuit can be easily attended
in the circuit cannot be easily attended. without getting any help from a medical doctor
Doctors help is necessary to rectify the
defect in the circuit.
3. Classify Pacing modes
[N/D – 07]
Based on the modes of operation of the pacemakers, they can be classified into five types. They are:
i) Ventricular asynchronous pacemaker(fixed rate pacemaker)
ii) Ventricular synchronous pacemaker.
iii) Ventri defibrillator inhibited pacemaker (demand pacemaker)
iv) Atrial synchronous pacemaker.
v) Atrial sequential ventricular inhibited pacemaker.
4. What are the batteries used for implantable pacemaker?
The batteries used for implantable pacemakers are
i)Mercury cell,
ii)Lithium cells,
iii)Nuclear cell
Prepared by Dr.A.Devasena., Asso.Prof / ECE
[N/D – 12]
Page 11
�EC8073- Medical Electronics
V Semester ECE
5. What types of electrodes are used in a defibrillator?
The electrodes used in a defibrillator are
i) Internal electrodes - Spoon shaped
ii) External electrodes –Paddle shaped
[A/M – 05]
6. What are the three types of exchangers used in HEMODIALYSIS system?
The three types of exchangers used in HEMODIALYSIS systems are
i)Parallel Flow dialyzer,
ii)Coil Hemodialyser,
iii)Hollow Fiber Hemodialyser
[M/J – 05]
7. What is meant by fibrillation?
[M/J –09], [A/M – 10]
The condition at which this necessary synchronism is lost is known as fibrillation. During fibrillation the
normal rhythmic contractions of either atria or the ventricles are replaced by rapid irregular twitching of
the muscular wall.
8. Calculate the energy stored in 16μF capacitor of a DC defibrillator that is charged to a potential of
5000 Vdc.
Given Data:
C = 16μF
V = 5000
E = (1/2) CV2
= (1/2) 16 10-6 25 106
= 200 Joules
9. When do you need heart lung machine?
[M/J – 6]
Heart- Lung machine is a device that maintains the circulation of the blood and the oxygen content of
the body when connected with the arteriovenous system. It is also called pump generator. The machine
is used in open-heart surgery when it is necessary to effect bypass of the circulatory system of the heart
and lungs.
10. What is dialyzate? Mention its composition.
The dialyzate is an electrolyte, through the cellophane sheets urea, creatinine, uric acid and
phosphates are diffused from the blood to dialysate. The blood is taken out from the body and waste
products diffuse through a semi permeable membrane which is continuously rinsed by a dialyzing
solution or dialyzate.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 12
�EC8073- Medical Electronics
V Semester ECE
11. Compare Haemodialysis and peritoneal dialysis.
Sl.No.
1
2
3
4
Haemodialysis
Peritonial Dialysis
More effective for separating the Less effective
waste products
Dialyzing time is about 3 to 6 hours.
Dialysing time is about 9 to 12 hours
Complex and risk, because blood is
taken out from the body.
Blood is purified by an artificial
kidney machine in which blood is
taken out from the body and waste
products diffuse through a semi
permeable membrane which is
continuously rinsed by a dialyzing
solution.
Simple and risk free.
The peritoneal cavity in our body is used
as semipereable membrane and by
passing the dialysate into it, waste
products are removed from the blood by
diffusion.
12. What is the principle of dialysis in the artificial kidney?
Dialysis is a process by which waste products in the blood are removed and restoration of normal
pH value of the blood is obtained.
13. Define Nuclear Magnetic Resonance signal
A patient in an external magnetic field causes the magnetization of protons of hydrogen atoms in
his body. Due to magnetization, these protons align and process about the external magnetic field,
now a radiofrequency pulse at resonance frequency is transmitted into the patient under controlled
condition. The resonance condition proton responds by emitting radiofrequency signal. This is
called nuclear magnetic resonance signal.
14. What is ventilator?
Ventilator is a device used in intensive care unit to provide oxygen enriched, medicated air to a
patient at a controlled temperature. Ventilators can operate in different modes: Controlled mode
and assist mode.
15. What is the cardiac pacemaker and why is it used?
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 13
�EC8073- Medical Electronics
V Semester ECE
It is an electrical stimulator that produces periodic electric pulses that are conducted to electrodes
located on the surface of the heart (Epicardium), within the muscle (myocardium) or within the
cavity or the lining of the heart (Endocardium).
1. What is cardiac fibrillation?
It is a condition wherein the individual myocardial cells contract asynchronously with only very
local patterns relating the contraction of one cell and that of the next. It causes irreversible brain
damage.
17. What is NSR?
NSR- Normal Sinus Rhythm, Any change in the NSR results in a condition called Arrhythmia. It
can also cause Bradycardia. A condition of slow heart where the heart rate reduces to 30-50 beats
per minute (BPM) resulting in insufficient blood supply to the human body. It causes dizziness and
loss of consciousness.
18. What is the need for ventilator?
It is used to provide artificial respiration. Artificial respiration should be applied to the patient,
whenever respiration is suspended due to reasons like gas poisoning, electric shock etc.
19. What is IPP?
IPP means Intermittent Positive Pressure. Positive pressure ventilators are used to inflate the
lungs with IPP.
20. What are the various electrodes used for defibrillation?
Internal (spoon shaped) electrodes and external (paddle shaped) electrodes are used for
defibrillation.
21. For what purpose external stimulation and internal stimulation are employed?
External stimulation is employed to restart the normal rhythm of the heart in the case of cardiac
standstill. Internal stimulation is employed in cases requiring long term pacing because of
permanent damage that prevents normal self triggering of the heart.
22. How the heart muscle can be stimulated?
Like all the muscle tissues, the heart muscle can be stimulated with an electric shock. The
minimum energy required to excite the heart muscle is about 10 joules.
23. For what purpose pacemaker is used?
Pacemaker is an electrical pulse generator for starting and for maintaining the normal heart
beat.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 14
�EC8073- Medical Electronics
V Semester ECE
24. When does heart block occurs?
Heart block occurs when the internal electro conduction system of heart is interrupted.
25. What is counter shock?
The phenomenon of application of an electrical shock to resynchronize the heart is known as
counter shock.
26. What is meant by defibrillation?
Ventricular fibrillation can be converted into a more efficient rhythm by applying a high energy
shock to the heart. This sudden surge across the heart causes all muscle fibers to contract
simultaneously. The fibres may then respond to normal physicological pace making pulses. The
instrument administering the shock is known as defibrillator. This process is known as defibrillation.
Unit IV
PHYSICAL MEDICINE AND BIOTELEMETRY
Part A
1. What is meant by diathermy?
Diathermy is the treatment process by which, cutting coagulation of tissues are obtained.
[A/M – 10]
2. List the types of diathermy.
The types of diathermy are
i)Short wave diathermy
ii)Microwave diathermy
iii)Ultrasonic diathermy
iv)Surgical diathermy
3. What are the two methods of shortwave diathermy?
The two methods of shortwave diathermy are
i) Capacitive method
ii) Inductive method
4. What is condenser method of shortwave diathermy?
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 15
�EC8073- Medical Electronics
V Semester ECE
In the Condenser method, the output of the diathermy machine is connected to metal electrodes
called PADS. They are placed on the body so that the portion of the body sandwiched between them
acts as dielectric of the capacitor.
5. What is the different electro surgery techniques used in diathermy unit?
Fulguration - The term “fulguration” refers to a superficial tissue discoloration without affecting
deep-seated tissues.
Desiccation - The needle point electrodes are struck into the tissue and kept steady while passing
electric current. This creates a high local increase in heat and drying of tissues takes place. This is
called „desiccation‟ which produces dehydration of tissues.
Electrotomy - When the electrode is kept above the skin, an electrical arc is sent. The heat
developed produces a wedge shaped narrow cutting of the tissue on the surface.
Coagulation - When the electrode is kept near the skin, high frequency current is sent through the
tissue in the form of bursts and heating it locally so that it coagulates from inside
6. What is the modulation techniques used for biotelemetry? Mention the reason for adopting that
modulation scheme.
[N/D – 04]
The two different modulation techniques used for biotelemetry are
i)Double Modulation
ii)Pulse Width Modulation
The purpose behind this double modulation, it gives better interference free performance in
transmission, and this enables the reception of low frequency biological signals. The sub
modulators can be a FM (frequency modulation) system.
7. What are the advantages of biotelemetry system?
[M/J – 07, 09]
The advantages of biotelemetry systems are
i) It is used to record the bio-signals over long periods and while the
ii) Patient is engaged in his normal activities.
iii) The medical attendant or computer can easily diagnose the nature of Disease by seeing the
telemeter bio-signals without attending patient Room.
iv) Patient is not disturbed during recording.
v) For recording on animals, particularly for research, the biotelemetry is greatly used.
8. Specify the frequencies used for biotelemetry.[N/D - 12]
Wireless telemetry system uses modulating systems for transmitting biomedical signals. Two
modulators are used here. A lower frequency sub-carrier is employed in addition to very- high frequency
(VHF). This transmits the signal from the transmitter.
9. What is microwave diathermy?
Microwave diathermy involves the process of irradiating tissues of the patient‟s body with very
short wireless waves having frequency in the microwave region. Typically, the frequency used is
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 16
�EC8073- Medical Electronics
V Semester ECE
2450 MHz corresponding to a wavelength of 12.25 cm. Heating effect is produced by the absorption
of the microwaves in the region of the body under treatment.
10. What is the principle of ultrasonic diathermy?
In this method, the heating effect is produced because of the ultrasonic energy absorption property
of the tissues. The amount of energy absorbed by the tissues is depending upon the frequency of
ultrasonic waves from a conventional crystal oscillator.
11. What are the advantages diathermies?
The advantages of diathermies are
i) The subject’s body becomes a part of the electrical circuit and heat is produced within the
body and not transferred through the skin.
ii) The treatment can be controlled precisely.
iii) Careful placement of the electrodes permits localization of the heat to the region to be
treated.
12. What are the different types of current that are used for medical applications?
The different types of current are Threshold current, pain current, let-go current,
current, fibrillation and defibrillation current.
paralysis
13. What are the applications of Bio-Telemetry?
[M/J – 13]
The most common usage for biotelemetry is in dedicated cardiac care telemetry units or step-down
units in hospitals. Although virtually any physiological signal could be transmitted, application is
typically limited to cardiac monitoring.
14. What are the choices of radio carrier frequency for medical telemetry purpose?
[N/D – 16]
The bio-signals are amplified to radio frequency range of few hundred KHz to about 300 KHz and
then they are transmitted by transmitter antenna's.
15. Draw the block diagram of biotelemetry system.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
[ N/D – 08]
Page 17
�EC8073- Medical Electronics
V Semester ECE
16. Give the design of biotelemetry system.
Design of a Bio-telemetry system are
i) The telemetry system should be selected to transmit the bioelectric signals with maximum
fidelity and simplicity.
ii) There would not be any constraint for living system and any interference with the living system.
iii) The size and weight of the telemetry system should be small.
iv) It should have more stability and reliability.
v) The power consumption should be very small.
vi) For wire transmission shielding of cable is a must to reduce noise level.
17. List the uses of Bio-telemetry.
Uses of bio-telemetry are
i) Biotelemetry helps us to record the biosignals over long periods and while the patient is
engaged in his normal activities.
ii) The medical attendants can easily diagnose the nature of disease by seeing the
iii) telemetered signals without attending the patient’s room.
iv) Patient is in his room without any mechanical disturbance during recording by means of
biotelemetry.
v) To study the treatment effect biotelemetry is the essential one.
vi) For recording on animals, particularly for research the biotelemetry is greatly used.
vii) For monitoring the persons who are in action the biotelemetry is an ideal one.
18. List the methods of classification of telemetry system.
The Methods of classification of telemetry system:
i) On the basis of the characteristics of electric signal such as voltage current position frequency
and pulse
ii) Based on form of data transmitted –analog and digital
iii) Based on transmission of distance –short distance type or long distance type
iv) Based on whether user has control over transmission channel or not.
19. List the types of modulations used in bio-telemetry systems.
Three types of modulations are used in bio-telemetry systems. They are
Amplitude modulation:
In this type of modulation the amplitude of the carrier is varied in accordance with the signal to be
transmitted.
Frequency modulation:
In this type of modulation the instantaneous frequency of the carrier is varied in accordance with
the amplitude of the modulating signal.
Phase modulation:
Here phase angle is varied in accordance to be transmitted signal.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 18
�EC8073- Medical Electronics
V Semester ECE
Unit V
RECENT TRENDS IN MEDICAL INSTRUMENTATION
Part A
1. What is a radio-pill?
[N/D − 09][A/M − 10][M/J − 12]
The radio pill is capable of measuring various parameters that are available in the tract. With the
help of radio pill type devices, it is possible for us to measure or sense temperature, pH, enzyme
activity, and oxygen tension values. These measurements can be made in associated with
transducers. Pressure can be sensed by using variable inductance, temperature can be measured by
using temperature-sensitive transducer.
2. Define Endoscopes
Endoscope is a tubular optical instrument to inspect or view the body cavities which are not visible
to the naked eye normally.
3. How telemetry can be used in transmitting stimulus signals to a patient?
If an electrode is surgically implanted and connected to dead nerve endings, an electrical
impulse can sometimes cause the nerves to function as once they did. If a miniature receiver is
implanted subcutaneously, the electrical signal can be generated remotely and transmitted to the
patient. This point brings up the possibility of using telemetry therapeutically.
4. What is the use of laparoscope?
The laparoscope is used for analyzing abdominal related diseases and to perform operations in the
abdominal region.
5. What is the purpose of using resuscitation unit?
Resuscitation unit is generally used in intensive care unit (ICU). In modern hospitals the
resuscitation units are in the form of a mobile trolley.
6. What are the two methods of pulse measurement?
The methods used for measuring pulse are transmittance and reflectance methods.
7. How do insulin pump works?
A pump also replaces the need for multiple daily injections with a continuous insulin infusion, and
also helps to improve your blood sugar levels. Insulin pumps are small, computerized devices that
mimic the way the human pancreas works by delivering small doses of short
acting insulin continuously (basal rate).
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 19
�EC8073- Medical Electronics
V Semester ECE
8. Is an insulin pump better than injection?
The pump delivers insulin continuously throughout the day, causing fewer sudden highs and lows
in blood glucose levels. There will be less needle sticks. You may have one injection (hook up)
every three days versus 15-18 injections in a three-day period with injection therapy, according to
O'Donnell.
9. What are the disadvantages using an insulin pump?
The main disadvantages of pump therapy are: Risk of skin infections at the catheter site. Risk of
diabetic ketoacidosis (DKA) from pump malfunction or absorption problems. Cost: pumps are
expensive, plus the continuing cost of supplies.
10. State the applications of telemedicine.
The applications of telemedicine are
i) Teleradiology
ii) Telepathology
iii) Telecardiology
iv) Teleducation
v)
Teleconsultation
[M/J – 16]
11. List out the three main categories of telemedicine.
The main categories of telemedicine are:
i)
Remote patient monitoring - allows patients with chronic diseases to be monitored in
their homes through the use of devices that collect data about blood sugar levels, blood
pressure or other vital signs. The data can be reviewed instantly by remote caregivers.
ii)
Store and forward technology - stores clinical data, as well as X-rays and other images,
and forwards the data to other locations for evaluation.
iii)
Interactive telemedicine - allows physicians and patients to communicate in real time.
Such sessions can be conducted in the patient's home or in a nearby medical facility.
12. Write the advantages of telemedicine.
Advantages of telemedicine are :
i) Telemedicine can be beneficial to patients living in isolated communities and remote
regions, who can receive care from doctors or specialists far away without the patient
having to travel to visit them.
ii) Recent developments in mobile collaboration technology can allow healthcare
professionals in multiple locations to share information and discuss patient issues as if
they were in the same place.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 20
�EC8073- Medical Electronics
V Semester ECE
13. Write the disadvantage of telemedicine.
Disadvantage of telemedicine:
Major disadvantage of telemedicine is the inability to start treatment immediately. For example,
a patient suffering from a bacterial infection might be given an antibiotic hypodermic injection
in the clinic, and observed for any reaction, before that antibiotic is prescribed in pill form.
14. What is the principle of telemedicine?
[ A/M – 08]
Telemedicine is a rapidly developing application of clinical medicine where medical
information is transferred via telephone, the internet or other networks for the purpose of
consulting and sometimes remote medical procedures or examinations.
15. What are the essential parameters of telemedicine?
The essential parameters of telemedicine are
i) Primary patient area
ii) Patient history
iii) Clinical information
iv) Investigation
v) Data and reports
16. State the telemedicine concepts.
The telemedicine concepts are
i) Store and forward concept
ii) Real time concept
17. What is meant by store and forward concept?
The store and forward concept involves complication and storing of information relation to
audio, video and clips, ECG etc.
18. What is meant by real time concept?
The real time concept involves the real time exchange of information between the two centre’s
simultaneously and communication interactively.
19. How the data are recorded using radio-pill?
The radio-pill is passed into the gastrointestinal tract like the normal pill. The sensor in the pill
collects the required parameter and transmits it through the telemetry system. The data recorder
picks up the transmitted signal, displays it and stores the data in a solid-state memory until the
data is downloaded into the PC platform.
20. List the types of endoscopes.
Types of endoscopes are cardioscope, bronchoscope, laparoscope, otoscope, gastroscope etc.
Prepared by Dr.A.Devasena., Asso.Prof / ECE
Page 21
�
 Devasena A.
Devasena A.