Preprint
Article
Estimation and Factors Affecting Water Quality and Sustainability in the Private Dental Sector in Greece
Altmetrics
Downloads
134
Views
72
Comments
0
A peer-reviewed article of this preprint also exists.
This version is not peer-reviewed
Abstract
Dental healthcare providers, staff and patients are constantly exposed to the risk of infection or cross-infection in the dental office, particularly due to the formation of biofilms within Dental Unit Waterlines (DUWLs). Good water quality, achieved with environmentally friendly means, is essential in ensuring the safe operation of the clinic. The aim of this study was to evaluate the practices and protocols used in dental offices of Metropolitan Athens in Greece with regards to water quality in DUWLs. The questionnaire about water quality was distributed to dental practitioners in 2022 and was completed by 206 dentists. Water supplied to dental units was mainly from the public network (65.0%), with 55.8% using in-office filtration. Most dentists (71.8%) do not know the active substance of the antiseptic used for the DUWLs, while 96.1% reported having an antiseptic reservoir embedded in the dental unit. Daily flushing with a small and a large amount of fluid was practiced in approximately 83% and 61% of dental offices, respectively. Dental associations should raise awareness regarding water quality and maintenance of DUWLs in dental offices, investing in lifelong learning, while implementing protocols and green strategies.
Keywords:
Submitted:
11 May 2023
Posted:
12 May 2023
You are already at the latest version
Alerts
A peer-reviewed article of this preprint also exists.
This version is not peer-reviewed
Submitted:
11 May 2023
Posted:
12 May 2023
You are already at the latest version
Alerts
Abstract
Dental healthcare providers, staff and patients are constantly exposed to the risk of infection or cross-infection in the dental office, particularly due to the formation of biofilms within Dental Unit Waterlines (DUWLs). Good water quality, achieved with environmentally friendly means, is essential in ensuring the safe operation of the clinic. The aim of this study was to evaluate the practices and protocols used in dental offices of Metropolitan Athens in Greece with regards to water quality in DUWLs. The questionnaire about water quality was distributed to dental practitioners in 2022 and was completed by 206 dentists. Water supplied to dental units was mainly from the public network (65.0%), with 55.8% using in-office filtration. Most dentists (71.8%) do not know the active substance of the antiseptic used for the DUWLs, while 96.1% reported having an antiseptic reservoir embedded in the dental unit. Daily flushing with a small and a large amount of fluid was practiced in approximately 83% and 61% of dental offices, respectively. Dental associations should raise awareness regarding water quality and maintenance of DUWLs in dental offices, investing in lifelong learning, while implementing protocols and green strategies.
Keywords:
Subject: Public Health and Healthcare - Public, Environmental and Occupational Health
1. Introduction
Sustainable entrepreneurship in the field of health depends on the breathing space that managers and employees give to nature and its resources [1]. The recent COVID-19 pandemic made even more imperative the need to protect and restore natural resources and integrate human activities more effectively [2]. The pandemic has raised awareness of the interconnectedness of our own health and the health of ecosystems [3,4]. Even after 3 years of active presence, it demonstrates the need for sustainable supply chains and consumption standards that do not exceed the health thresholds of the planet itself and the microcosm and macrocosm of human societies [5]. As already reported, the risk of the emergence and spread of infectious diseases increases as nature and its resources are destroyed [6]. Therefore, protecting and restoring biodiversity and the proper functioning of ecosystems is the key to strengthening our resilience and preventing the emergence and spread of future diseases [1,7]. According to EU press releases, investment in nature protection and restoration will also be crucial for Europe’s economic recovery from the COVID-19 crisis [8,9,10].
It is vital that stakeholders avoid getting stuck in destructive habits of the past towards environmentalism. The European Green Deal – the EU’s growth strategy – is ensuring that the economy serves society and people, giving more to nature than it takes away [11]. Additionally, in the US, programs are used by multidisciplinary teams that include facility managers, infection prevention professionals, clinicians, and administrators [12]. The business design for biodiversity is therefore imperative in all sectors of the economy, especially in the field of health sciences [13,14].
Water pollution is a key driver of biodiversity loss [15] and has harmful effects on our health and environment [16]. Biodiversity is affected by the release of nutrients, chemical pesticides, pharmaceuticals, hazardous chemicals, municipal and industrial wastewater, and other wastes, including litter and plastics into water resources [17]. In this framework and the ambition for zero pollution and an environment free of toxic substances, important steps are being taken at the legislative level where the principle "the user pays" but even more "the polluter pays" will be on the scope for all entrepreneurships including the health sector [10,11]. In such an approach, water quality and quantity are of great importance in all health domains, including dental offices [10,18,19,20,21,22,23].
Water legislation is already extensive and well developed [10,23,24,25,26]. Even though there is an international legal framework to reduce pollution, greater efforts are still needed to ensure sufficient quantity and quality of water supplies [21]. However, there are areas where more work is needed such as the efficient use of water in buildings. Through the Eco-design Directive, the Commission is looking for ways to increase the water and energy efficiency of products [21,22,23]. The goal is not only to save water, but also to develop new technologies that will create jobs or design smart green equipment and materials. Even since December 2012, the Eco-design Work Program 2012-2014 had covered an extensive list of 12 priority product groups, which included water-related products (such as taps, showers and toilets); for which eco-design standards -among other measures- could be developed [27]. That act is meant to produce simplicity for consumers, who in the future will only find on the market more water-efficient appliances and products, which will be clearly labeled according to their efficiency. So, in the future the retrofitting of existing buildings will not be required, but there will be a gradual replacement of old products with more efficient ones, [22,23,24] that will bring significant energy savings [27]. In addition, to promote the efficient use of water in the construction sector, there are voluntary EU Ecolabel and green public procurement criteria for construction materials and products related to water networks [23,24,27].
In the field of green health organizations and especially dental offices, the reduction of water waste, the quality of water in the piping of the office and the dental unit, but also the prevention of infections, is a challenge that every dentist must face [28,29]. The trend and attention to this important part of health care is growing, in part due to the increasing needs for workplace safety for both workers and patients [15,27]. Good water quality is an important factor in ensuring the quality and safe operation of the dental clinic [30,31]. The water network participates in all clinical protocols, in the antisepsis and disinfection procedures, the operation of the dental unit as well as all other areas (doctor’s office, waiting room, toilets, laboratory, rest room or kitchen). Infections in a dental office are very easy to occur using contaminated instruments, due to poor air quality [32] or the use of contaminated water [33,34]. Therefore, there is considerable (and justified) attention to the sterilization protocols of dental instruments and handpieces [35], but less attention is usually paid to the treatment of air and water even though they participate in these protocols [36,37,38,39]. Increasingly, low water quality has been recognized as a possible cause of biohazard in the dental office. Water is the vehicle through which most of the infections that develop in the dental office are spread [40,41]. A biofilm that forms inside the pipes of a building could contaminate the entire water supply network of that building, including the dental office [42]. Furthermore, within the dental clinic, water spreads as an aerosol, increasing both bacterial spread and the risk of infection to all people in the premises [15,43,44,45,46]. Various microorganisms such as unicellular algae, bacteria and fungi can coat and colonize almost any material in the dental clinic [47,48]. Biofilms in dental clinics have been shown to comprise a hazardous bacterial deposit of contaminants, which can become resistant to various disinfectants [38,45,49,50,51,52]. Biofilms within the water lines of dental clinics originate from one of two possible sources of contamination: from the internal piping system using direct supply from public network or from the patient’s mouth [31,39].
According to the above, staff and patients are constantly exposed to risk of infection due to water installations in the dental office [53,54,55]. Therefore, this study was carried out in a sample of dentists from the wider area of Metropolitan Athens, capital of Greece, with the purpose to promote and evaluate: 1) self-assessment of water use practices in the dental office, 2) recording of the applied disinfection protocols of the water network of the dental unit, 3) analysis and comparison of factors influencing the practices of dentists, 4) investigation of continuing education needs of dentists to implement more effective hygiene protocols in the water network of the dental unit. The research questions were: 1. What are the equipment and practices that ensure water quality in dental offices in Greece? 2. How do equipment and processes differ according to the characteristics of dental practice? 3. Which equipment and practices lead to the strongest dentists’ perception of dental unit water quality?
2. Background of the Study
2.1. Water Quality of the Network in the Research Area
The research took place in the vast metropolitan area of Athens, capital of Greece during the third phase of the pandemic (March – October 2022). In the areas of Athens region, EYDAP, (Hellenic water supply and sewerage company of the capital), is responsible for the quality of water in the public network. EYDAP has two accredited laboratories in the capital, as well as laboratories for the control of intermediate stages of water treatment that use the most modern analytical methods to achieve high sensitivity, accuracy, and repeatability of water measurement [18]. EYDAP constantly certifies the water of the Athens metropolitan area, with nearly three times the sampling frequency required by law, ensuring it is of excellent quality and one of the best in Europe (EYDAP SA, n.d.). According to the Urban Water Atlas for Europe for 2017, published by the European Union and presenting the best practices in European cities, EYDAP was rated 10 (excellent) regarding the quality of drinking water for the city of Athens [56]. In the international assessment of water supply companies by the European Benchmarking Co-operation, in which EYDAP participates every year, the water quality achieves a performance of >99.8%, a value higher than the average scores of the participating Western European companies [57]. EYDAP systematically supervises and records not only the existing legislation but also the international trends in regulatory issues, which may constitute future legislative requirements or requirements of interested parties. As a result of this action, the list of monitored substances is constantly being enriched [18].
2.2. Water System of the Dental Unit
The public water supply must consist of a low bacterial load, with a complete absence of pathogenic bacteria. Thus, it is not sterile. Water circulating in the system of the city contains a diverse microbial flora which, depending on its type and concentration, is generally harmless to humans. However, under certain conditions, pathogenic microorganisms or opportunistic pathogens can reach the dental unit through the water supply chain [58]. The microbiological quality of the water samples collected throughout the city system does not necessarily correspond to the microbiological quality that could be detected at points closer to the dental office [29,47,59,60].
The risk of cross-infection between dentist and patient, or between patients, is high and therefore, must be managed with appropriate antimicrobial systems more sensitive than in other health sectors [61]. The interest in the pathologies of Legionella pneumophila [62] should also motivate us to think about other, even more alarming diseases and ways to adopt systems capable of preventing them [34,63]. Studies referring to DUWLs, biofilm formation and dental unit’s water quality have shown that DUWLs and the entire fluid transfer line of the dental unit (narrow-bore plastic tubes that carry water to the high-speed handpiece, air/water syringe, and ultrasound device) are colonized by microorganisms including bacteria, fungi, and protozoa [28,31]. Protected by a layer of polysaccharide mucus known as the glycocalyx, these microorganisms colonize and reproduce on the inner surfaces of the suction tube and form a biofilm, which serves as a reservoir that can enhance the number of floating (planktonic) microorganisms in the water used for dental treatment [51,52,64]. Although oral flora [65] and human pathogens (e.g., Pseudomonas aeruginosa [66], various Legionella species [54], non-tuberculous Mycobacterium species (Mycobacterium) [67] and Helicobacter pylori [68] have been isolated before from dental unit water systems, most organisms retrieved from dental water lines are common heterotrophic water bacteria [69].
Some earlier reports have associated waterborne infections with dental water systems, and scientific evidence supports the potential for transmission of waterborne infections and diseases in hospital settings and in the community [29,70,71]. Infection or colonization caused by Pseudomonas species or non-tuberculous mycobacteria can be transmitted to susceptible patients through direct contact with water [40] or after exposure to residual water contamination from inadequately treated medical or dental instruments and tools [30,31,60,72]. Non-tuberculous mycobacteria can also be transmitted to patients from tap water aerosols [37,38]. Healthcare-associated transmission of pathogens (e.g, Legionella species) occurs primarily through inhalation of infectious aerosols generated from drinking water sources or tap water used in respiratory therapy equipment [16]. Today, among the many infectious and pathogenic agents found in the water networks of dental clinics, both viral and bacterial, there are particularly dangerous microorganisms such as: Legionella, pseudomonas species, Candida, tuberculosis bacteria, HIV, hepatitis C and lately, COVID-19 viruses [55,73,74,75]. Many of these will be identifiable through a simple bacteriological analysis of the water. It must be considered that through the high-speed handpieces of the dental unit, viruses and bacteria present in the water supply are sprayed into the environment in the form of aerosols and come into direct contact with the wounds of the patient undergoing treatment [76]. In addition, some immunocompromised dental patients are more susceptible to contamination, in proportion to the hygienic conditions in the dental office [72,77]. Researchers have not recently demonstrated a measurable risk of adverse health effects to bystanders or patients from exposure to dental unit water [58] basically due to better disinfectants used [78].
Bacteria populations can be spread during ongoing dental procedures when dentists are using high-speed handpieces [79,80,81,82]. There is a risk of water backflow into the dental chair piping from the handpieces known under the term of suck-back phenomenon [83]. High-speed handpieces, in the deceleration phase of cutting, have a centrifugal suction effect that forces them to retract organic material especially from their head [62,84]. For this reason, many handpieces are equipped with special anti-retraction valves, which hold the suctioned material in the rotor [76]. These valves may not provide a perfect blockage (depending on how well the handpiece is maintained) and any leakage can lead to bacterial colonies inside the handpiece body [85]. This is an ideal environment for bacteria to grow, increasing the risk of cross-contamination. Consequently, all modern dental clinics need to have integrated disinfection systems [66,85,86].
There are various devices, materials, and filters within or in parallel connection with the dental machine, which make it possible to limit the risk of contamination of the water circulating within its piping. 1) Chlorine dioxide is a powerful and effective disinfecting agent capable of producing and maintaining safe drinking water through oxidation rather than a chlorination reaction [51]. 2)Reverse osmosis is the safest and most widespread water treatment system in the world and can guarantee absolute water purity for the dental unit [87]. The osmotic membrane can process water to the molecular size, making its characteristics optimal in terms of color, smell, and organoleptic purity. Osmosis is a natural process [52] where the solvent of the more dilute solution passes through the membrane to dilute the more concentrated one [63,65], producing a solution very poor in solutes [71,88,89]. 3) Electrolysis apparatuses that use only the chlorine normally present in municipal water, such as the Poseidon-S system, an additive-free disinfectant system described in the study of Fujita et al., [90] can control microbial contamination in contaminated dental unit waterlines too. It is mentioned that electrolyzed water demonstrated a broad antimicrobial spectrum and was highly efficient in the dental office disinfection against viruses, fungi, and bacteria, being compatible with most dental materials. It could further protect against SARS-CoV-2 infection and contamination in the dental office [69]. Positive relevant results can be guaranteed with plasma devices too [91] or acoustic waves at high energy [92]. It was mentioned that the efficacy of acoustic waves in preventing Streptococcus mutans adhesion on dental unit water lines can be important as retraction of human fluid in certain parts of the unit, during dental therapy is found to be the contamination source [15]. 4) For surgical procedures, sterile saline or sterile water should be used as the coolant/irrigant. Conventional dental units cannot reliably provide sterile water even when equipped with independent water tanks containing sterile water because the water-carrying path cannot be reliably sterilized [86]. Other suitable delivery devices (e.g., syringes and sterile disposables or sterile water delivery systems that bypass the dental unit using sterile disposable tubing) are typically utilized to provide sterile water during surgery [85,93].
2.3. Water Quality in the Dental Unit
The Guidelines on infection control in dental healthcare settings issued by the US Centers for Disease Control and Prevention [12] recommend that the level of heterotrophic plate counts (HPCs) in dental unit water should not exceed 500 CFU/mL [94]. Moreover, the American Dental Association (ADA) has set a limit of ≤200 CFU/mL on the heterotrophic bacterial load in water from dental unit waterlines [95]. In the EU, however, there is no current guideline regarding DUWLs, though in some countries the drinking water standard is used as a reference (≤500 colony forming units (CFU)/mL of water heterotrophic bacteria). [84]. For this reason, dental units are designed to include (Figure 1): a) Self-contained water systems (e.g., independent water tank) combined with chemical treatment (e.g., periodic, or continuous chemical microbicide treatment protocols), b) Systems in parallel connection with one or more dental units within the same dental office that clean or treat incoming water to remove or inactivate microorganisms throughout the network and c) Combinations of these methods.
Finally, hand hygiene at the dental office is important and protocols have been revised due to the COVID-19 pandemic [32,96]. When the treatment of patients is completed, specific protocols should be followed for flushing the suction network to reduce residual microbial contamination [15]. All incoming water lines of the public water supply system within the dental practice (e.g., taps, dental machine water mains and other dental equipment such as the suction mains) should be flushed [38,97]. There is no agreement on the optimal duration of flushing procedures, but the recommendations suggest that the procedures take from 1 to 5 minutes [75]. The time required may vary depending on the type and length of the network in each dental office [12,75,85]. After flushing the incoming lines of the public water system, the dental facility water lines should be disinfected according to the manufacturer’s instructions [31,54,55].
3. Materials and Methods
For this study, an e-questionnaire was designed in google forms, specifically for this study according to standards assigned to the internal water network of modern dental units shown in Figure 1. The link to the questionnaire was sent three times within a period of thirty days through the main secretariat of the Athens Regional Dental Association. A panel of 6 experts in the field (a mechanical engineer and technician of dental units, three EYDAP experts and two dentists) reviewed and revised the survey questions to be relevant to the topic and expressed them correctly as mentioned elsewhere [98]. They worked independently and on a second step in two joint meetings an exchange of ideas with the authors was performed to make final suggestions. The questionnaire was further validated through fulfillment of ten members of the academic staff and ten postgraduate students that were not involved in the study. Finally, the accuracy of the completion was checked by making all questions obligatory to submit the questionnaire while submission was allowed, only once.
The questionnaire had three parts. Part A had nine questions concerning demographic statistics of the sample (gender, age, family status, place of work, dental educational level, ways of practicing dentistry, years of professional activity, family income. Part B had thirty multiple choice questions describing ways of water circulation within the unit and handpieces, as well as attitudes and processes that dentists use for their maintenance, and disinfection. Part C had eight multiple choice questions addressing environmental and legislative issues. Finally, part D had two questions about educational approaches on water quality assurance within the dental office, one of which was an open-ended question so that participants could fill in their proposals and enquiries.
The online questionnaire included a short introductory message describing the purpose of the study and stressing voluntary participation, confidentiality, and the right to refuse participation. Consent was obtained by asking participants to confirm that they agreed to complete the questionnaire by marking a "Yes, I agree to participate” box. Ethical approval was obtained from the Ethics and Scientific Board of the Athens Regional Dental Association, metropolitan area of the capital, No:2660/08.12.2022). A QR code was assigned to the questionnaire link to provide direct access through participants‘ smartphones. No reward was given for participating in the study. The questionnaire was left open for 3 months. Inclusion criteria for the study were professional dentists of the private sector in the vast metropolitan area of Athens while exclusion criteria were non dentists, dentists of the public sector, auxiliary dental personnel, and dental students.
6. Statistical analysis
The data collected from the survey were analyzed with the statistical package IBM SPSS v. 28. Absolute and relative frequencies (N, %) were calculated for all variables of demographic and dental practice characteristics, practices, and equipment for water quality. Following, to examine the associations between demographic and dental practice characteristics with adopted practices for water quality and equipment of dental offices, chi-square tests of independence were performed with Fisher exact test correction when needed. To detect the most influential factors that lead to dentists’ perception of good water quality in their dental practice, binary logistic regression analysis with backward elimination was performed with dependent variable the feeling of confidence about water quality and independent variables the adopted practices for water quality and equipment of dental offices. Stepwise backward elimination with significance level of .10 is commonly used in situations where multiple variables are available, and the aim is to select only the variables that provide a stable, generalizable model [99]. The scale of the study has good reliability (Cronbach’s alpha =0.701). However, Cronbach’s alpha is not avoided in such questionnaires (formative measures) but in a climate that assumes that there is a latent construct that influences the answers (reflective measures). When recording practices, opinions and equipment, there is no need for a correlation between the responses (what is also called internal consistency or reliability) [100].
4. Results
The Sample
The sample consisted of 206 participants (56.8% men, 42.7% women and 0,5% other), in the age range 41-60 years old (60.2%). Most participants were married (67.5%) and were active in Athens or other urban center of Greece (92.2%). Most of the sample (56.3%) had work experience of 11-30 years, with a family income of up to 50.000 euros (77.2%). 43.2% of participants studied dentistry in Greece while 18.4% abroad, 50.0% had some postgraduate education (MSc, PhD, or postdoctoral research) and only 10.2% had been trained for a recognized specialization. Most dentists (75.7%) practiced general dentistry along with other clinical activities (e.g., prosthetic, or cosmetic dentistry) and only 24.3% practiced only other clinical processes. Most dentists had a private dental practice (66.0%), 27.7% had a dental clinic with more than one employee and 6.3% had other employment status (worked in public hospitals, universities, freelance provision of dental services etc.). 59.0% of dentists had one dental chair in their practice, while 31.1% had two dental chairs (data not shown).
Regarding the equipment and practices of Greek dentists for water quality, 62.6% of the participants reported having an equipment of 6-20 years old, while 16.5% had their equipment for more than 20 years and 20.9% less than five years. Most dentists (52.9%) do not have an assistant, were informed about water quality when acquiring the dental unit (61.2%) and are interested in learning more about water quality (78.6%). Yet only 55.3% reported that they were confident about the dental machine water quality regarding microbial load. A small percentage (21.8%) perform microbiological tests on the premises of the dental office. A continuous water supply system to the dental unit was reported by 30.1% of the dentists. A system of uninterrupted water supply to the handpieces and scalers, i.e., a feeding bottle that needs filling, was reported by 33.5% of participants. The water supply was mainly from the public network to the dental unit (65.0%), to the rotative cutting instruments (62.3%) and to ultrasonic and air scaler devices (55.8%). Only about 25% of dentists reported that the water was filtered from a filter device directly connected to the supply. 55.8% stated that the water filtered in the dental office, by a simple filter (19.4%), a reverse osmosis filter (4.9%), a deionization or ion exchange filter (2.9%) or an activated carbon filter (15.0%). Dentists reported that the water filter is replaced or cleaned every six months (18.9%) or every 12 months (11.1%). Most dentists (71.8%) do not know the active substance of the antiseptic used for the hydraulic piping of the dental unit, while only 9.4% and 14.4% report that the antiseptic is supplied to the handpieces automatically or manually respectively. 96.1% of participants reported having an antiseptic reservoir embedded in the dental unit.
94.7% of participants report being equipped with a strong surgical suction with electric motor (67.0%), air or water vacuum (8.8%), while 18.9% of dentists did not know the type of surgical suction. Before the Covid-19 pandemic, 82.6% of dentists reported cleaning the saliva suction with a small amount of fluid suctioning at least once a day. Also, 63.1% of dentists reported cleaning the saliva suction with a large amount of fluid suctioning at least once a day, and 27.7% once a week. Regarding the surgical suction, 84.0% of dentists reported cleaning with a small amount of fluid suctioning at least once a day. Also, 59.8% of dentists reported cleaning the surgical suction with a large amount of fluid suctioning at least once a day, and 28.2% once a week. Cleaning the piping of the dental unit with a large amount of liquid was reported at least once a day (46.1%) or every week (26.2%). Most dentists (91.7%) disinfected the surfaces of the dental equipment after each appointment.
The dental unit was reported to be serviced annually (or after a failure) by 61.6% of participants, while 38.4% only performed a service after a failure. 70.0% of dentists reported having up to 3 micromotors/luftmotors and 57.8% up to 3 airotors. Micromotors and airotors are cleaned between appointments by decontamination (58.30%), decontamination and sterilization (6.8%), sterilization (17.5%) or only surface cleaning (17.5%). 37.6% of dentists reported having an implantology motor. Most participants (53.8%) preferred channeling sewage into the sewer through suction, compared to connection to the central drainage.
Possession of an amalgam separator was reported by 64.6% of dentists (type: unknown 19.9%, filter cleaning 28.2%, full replacement 14.1%). Having a contract with a disposables collection company and for amalgam removal was reported by 58.2% and 26.6% of participants, respectively.
Only 14.4% declared being informed about water quality legislation in health care facilities. 69.9% of dentists spend more than 2 hours per month on the cleaning/disinfection of the dental unit. Moreover, 64.6% of dentists estimated spending up to 50 euros per month for cleaning/disinfection of the dental unit. Thus, 84.6% of dentists believe that their practices for cleaning/disinfection of the dental unit are environmentally friendly. The implementation of the disinfection protocol was the dentist’s own responsibility in 58.3% of cases while participants reported adopting more strict practices of water management after Covid-19 by 50.7%. (Data available as Appendix A)
Following, differences between demographic characteristics of dentists were examined. Table 1 presents only the significant results from the chi-square tests of associations performed between gender and variables of dentistry equipment and practices. Female dentists were more interested in additional information about water quality (females 87.5% vs males 71.8%). Water supply directly from the public network to the dental unit, the cutters and the ultrasounds was reported more frequently by female dentists (68.8% to 73.8%) compared to male dentists (51.8 to 58.3%). Moreover, female dentists were more likely to disinfect the dental office/equipment surfaces between two appointments compared to men (females 97.7% vs males 88.0%). Also, female dentists were more likely to perform annual maintenance to the dental unit (females 66.3% vs males 57.9%) and less likely to have an implantology motor (females 27.6% vs males 44.6%).
Table 2 presents only the significant results from the chi-square tests of associations performed between the dentists’ work experience and variables of dentistry equipment and practices. More experienced dentists were more likely to have water supply from a filter device directly connected to the main supply compared to less experienced dentists who were more likely to supply the dental unit, cutters, and ultrasounds directly from the public water network. More specifically, only 3.8-7.7% of dentists with less than 10 years of experience had a water filter to the dental unit, cutters, or ultrasound, compared to 34.5%-39.7% of dentists with over 30 years of experience. More experienced dentists were also more likely to clean the surgical suction with a large amount of fluid suctioning once a day (39.3%-48.3%) compared to less experienced dentists who cleaned the surgical suction with a large amount of fluid suctioning once per week (31.0%) or never (13.8%). Also, 61.1% of dentists with over 30 years of experience performed cleaning of the dental unit with a large amount of fluid suctioning at least once a day, while less experienced dentists were more likely to clean it once a week. More experienced dentists were more likely to have more micromotors (χ2=25.92, p<.05) and airotors (χ2=29.17, p<.05) and spent more time in cleaning and disinfecting the dental unit (χ2=26.21, p<.05). Yet, less experienced (and younger) dentists are more informed about water quality legislation (27.6%) compared to more experienced and older dentists (13.2%-17.5%).
Table 3 presents only the significant results from the chi-square tests of associations performed between the dentists’ educational characteristics and variables of dentistry equipment and practices. Dentists who have studied abroad were more likely to supply antiseptic to the handpieces manually (χ2=7.15, p<.05), clean the surgical suction with a small amount of fluid suctioning once per day and not between appointments (χ2=13.26, p<.05) and believe that their practices are environmentally friendly (χ2=10.93, p<.05). Dentists who had some postgraduate education, were more likely to have an assistant (χ2=13.66, p<.05), know the active substance of the antiseptic (χ2=5.86, p<.05) and supply antiseptic to the cutters automatically (χ2=5.54, p<.05). Also, most of the more educated dentists clean the surgical suction with a small amount of fluid suctioning between appointments (51.0% and 18.9%) compared to less educated dentists that clean the surgical suction with a small amount of water between appointments (40.7%) or once per day (35.2%), χ2=13.26, p<.05. Dentists who had some postgraduate education, were more likely to maintain the dental unit annually (χ2=7.24, p<.05), have more micromotors (χ2=12.72, p<.05) and airotors (χ2=8.94, p<.05), have a contract for amalgam removal (χ2=4.46, p<.05) and less likely to be responsible for the implementation of the disinfection protocol (χ2=6.57, p<.05). Finally, dentists with a recognized specialization were more likely to have an assistant (χ2=5.56, p<.05), maintain the dental unit annually (χ2=4.40, p<.05), have less airotors (χ2=22.76, p<.05) and don’t have an amalgam trap (χ2=8.56, p<.05).
In Figure 2, there is a graphical systemic presentation of factors affecting water maintenance of the dental unit.
Table 4 presents only the significant results from the chi-square tests of associations performed between the dental office characteristics and equipment/practices for water quality. Dentists who practiced general dentistry were less likely to have an assistant (χ2=25.32, p<.05), supply antiseptic to the cutters manually (χ2=4.56, p<.05), clean the surgical suction with a large amount of fluid suctioning less often (χ2=11.64, p<.05), have amalgam trap (χ2=4.38, p<.05). Dentists who practiced in a clinic (with employees) compared to a private practice, were more likely to have newer equipment (χ2=16.12, p<.05), have an assistant (χ2=44.26, p<.05), supply antiseptic to the cutters automatically (χ2=6.36, p<.05), have more micromotors (χ2=31.40, p<.05) and airotors (χ2=22.04, p<.05), have implantology motor (χ2=7.37, p<.05), have contract for amalgam removal (χ2=4.07, p<.05) and less likely to be responsible for the implementation of the disinfection protocol (χ2=26.24, p<.05). Moreover, dentists with a higher annual income were more likely to have an assistant (χ2=4.36, p<.05), perform microbiological tests (χ2=7.60, p<.05), have a continuous water supply system to the dental unit (χ2=6.38, p<.05), supply antiseptic to the cutters automatically (χ2=6.21, p<.05), clean the surgical suction with a small amount of fluid suctioning more often (χ2=23.24, p<.05), have more micromotors (χ2=24.39, p<.05) and less likely to be responsible for the implementation of the disinfection protocol (χ2=6.26, p<.05).
4. Discussion
To our best knowledge there are few studies presenting processes and practices differences for the quality of water of the dental unit according to certain demographic characteristics. Concerning gender differences found in our data, it is also elsewhere reported that female dentists have different work patterns than their male colleagues [101,102,103,104,105]. This is assigned to psychological dissimilarities [106], as well as certain differences in their practical skills and roles within society [103,107,108,109,110]. Women, being culturally responsible for the housekeeping [111,112] it is not a surprise that they are more willing to perform accurate cleaning of the dental unit as already mentioned before [113]. In our study, female dentists were more interested in additional information about water quality, more likely to disinfect the equipment between two appointments and more likely to perform annual maintenance of the unit. In another study of female dentists, it was mentioned that they provide more scaling and restorative services than males although the differences might not be statistically significant [114]. This could also explain our findings since after scaling it is known that the unit brings high levels of contaminant material through blood suction during the process [58], thus forcing dentists to perform a stricter disinfection protocol. As reported in the study of Reza et al., [114], female dentists also administered more pediatric treatments than their male colleagues though not statistically significant, while in our study too, women were less likely to have an implantology motor indicating other than implantology procedures performed in their offices. Also, women are less willing to perform technical procedures in the equipment as in many cultures this is a male’s role [115] and secondly, they usually have no time in between their other social roles [116]. Thus, it is not surprising that in our study they just directly connect their unit to the public water network, and use no filters while men are searching for different solutions (filters, equipment etc.) for achieving better quality of water for the unit.
As far as experience in the profession there are certain differences in the knowledge level among professionals [116,117]. We also found that more experienced professionals are more likely to follow detailed water quality performance such as the use of a filter device directly connected to the main supply, flush with a large amount of water the suction and the unit once per day and search for extra water quality equipment, while less experienced ones preferred simplest ways of water supply such as direct connection to the public water network and flus once per week. It is unclear whether this attitude is based on the concern of saving water rather than ignorance of safe antiseptic protocols. Further, as evidenced by the literature, possible transmission within the dental office via direct contact is the use of hollow instruments in dentistry [39,48]. So, effectively enough, more experienced dentists in our study were having more micromotors and airotors and spent more time in cleaning the unit, diminishing cross contamination possibilities between appointments as reported elsewhere too [54,118].
Several studies can report on the efficacy of methods to clean and disinfect hollow instruments such as airotors and (high speed) handpieces [34,70,82,96]. The presence of bacteria, fungi, and viruses on and inside dental hollow instruments has been determined before [40]. Cleaning these handpieces with a wipe moistened with ethanol (70%) is insufficient to eradicate microbial contamination [119]. As known from all relevant covid-19 protocols, it is not only the exterior, but also the interior of these instruments that should be cleaned and disinfected properly, since hollow instruments contain contamination of both the patient and the water/air supply [83,118]. Moreover, sufficient guidelines about how to decontaminate handpieces are available [41], but most of the dentists in our study and elsewhere [120,121] are unaware of these guidelines forgetting for example that overnight bacterial accumulation in the handpieces can be significantly reduced by allowing water-cooled handpieces to run and to discharge water into a sink or container for several minutes at the beginning of the clinic day [118]. In the study of Schalli et al. [118], though, the fact that 92.9% of water samples taken after procedures during which no spray water was used showed an increase in protein concentration, illustrates that the contamination cannot be due solely to the retraction of spray water and that differences in the maintenance and antiseptic protocols used in different offices and the rotational speed of the handpiece could explain a certain dilution [34,58,96]. Other techniques such as preprocedural mouth rinsing with chlorhexidine [122], essential oil, povidone-iodine, or water, before ultrasonic scaling could reduce bacterial contamination on aerosol formation and cross-contamination [82]. Finally, researchers seem to agree that the extent of contamination can depend on the person using the instrument also proven from our data, as well as on the patient [35]. Additional relevant factors include the number of motor stops, the rotational speed of the handpiece (controlled using the foot pedal), the extent of the lesion to be treated, and the oral hygiene of the patient. In the study of Schalli et al. [118], it was discussed that six out of seven offices had contaminated spray-water lines even before patients were treated with the handpieces. Only in the case of instruments in the office where thorough decontamination, including disinfection, had been performed, no protein was measurable before treatments [118]. An exact documentation of the decontamination procedures and storage conditions, as well as an analysis of the disinfectants and lubricants used, could be assigned for further update of the procedures [35]. In our study unfortunately, only 28.2% of the dentists knew the substance of the antiseptic they are using.
Individual handling of the instruments from assistant personnel or the dentist himself is essential too, and from our data dentists studying abroad and those performing general dentistry are more informed on performing four-hand dentistry for better antimicrobial scene and health for personnel and the patient as described also elsewhere [40]. Further, dentists in our study with some postgraduate education, were more likely to have annual maintenance habits for their equipment and unit, have more handpieces and a contract with a certified disposal company for amalgam removal. Also, it was less likely for them to be responsible for the implementation of the disinfection protocol as they work with an assistant. This is also reported elsewhere where there are significant differences in the knowledge scores between different groups of dental professionals, and between dental specialists and dental assistants too [116,117,121]. The trend for specialists and more educated dentists is to work on a team base and run bigger clinics with more than one unit as was the case in our study too. In such a scenario assistants can run safe protocols in between appointments presenting a safer antiseptic profile.
Dentists that had studied abroad supply antiseptic to the handpieces manually, clean the suction with a small amount of fluid and not between appointments believing falsely that their practices are environmentally friendly. This is attributed to differences in educational approaches in different countries and regions as mentioned elsewhere [123]. In bigger dental clinics though, equipment is newer, the supply of antiseptic to the handpieces is automatic, they have more handpieces, implantology motors and contracts with amalgam disposal companies. Economic reasons for performing cheaper and not environmentally friendly safety protocols within the dental office are also reported elsewhere [32,124].
But the cheap protocol is not scientific based, nor it is safe and can be more expensive even in a short end period. Patients are well informed after the covid-19 pandemic on the safety protocols and willing to support health units that practice these protocols [96,124]. Dentists that do not follow certain antiseptic and maintenance of equipment guidelines will disappoint stakeholders and patients sooner than in the past and they will most likely encounter sustainability issues [15].
Thus, the Centers for Disease Control and Prevention [41] recommend that manufacturers should provide dental units with a separate reservoir, typically a container of about 1-liter capacity, from which tap water, deionized water and/or distilled water can be fed to the handpiece which is the case in our study, as 96.1% of participants reported having an antiseptic reservoir embedded in the dental unit, compared to 94% in East England reported before [125]. This can also be applied to the use of biocides. In cases where dental units are still fed directly by municipal water it is even more important to adopt the various systems for preventing microbial contamination, such as, for example, the use of handpieces and turbines fitted with anti-reflux valves or flushing, which should always be carried out for 20–30s after each patient is treated [38,97]. Of course, flushing with water alone cannot guarantee water quality in the dental office as shown in the study of Alkhulaifi et al. [97]. Unfortunately, though, most dentists in our study (71.8%) do not know the active substance of the antiseptic used for the hydraulic parts of the dental unit, a point that needs further attention for continuing education courses in the field. Baudet et al. [78] found that tap water is used in the dental unit by 65% of the dentists, distilled water by 2.3% and filtered water by 19.7% compared to our 89%, 3.6% and 7%, respectively. Additionally, Chate [125], reports that water is tested by 1% of dentists, Baudet [78] reports 2,6%, whereas we found that 21,8% performs water testing, compared to 16,8% in the USA [125] and 17% in the EU, reaching as high as 70% in Germany [78]. In our study it was reported that filters are replaced every 6 months by 18.9% of dentists and every 12 months by 11.1%, both values are lower than what Baudet has reported [78].
Overall, as already discussed in the guidelines for the prevention and control of legionellosis [12,15,126], in order to reduce microbial contamination and/or the formation of biofilm in dental waterlines, the following recommendations should be implemented: a) any sections excluded from the flow currents should be eliminated from the network, b) anti-stagnation devices should be installed to keep the water circulating continuously, particularly during non-working hours, c) sterile solutions should run the network, after isolating it from the main water supply, d) slow dentistry and long appointments on the same patient as well as intervals between patients (as suggested by the covid-19 pandemic) should be followed, e) all devices that connect to a waterline and enter patients’ mouths, (handpieces, ultrasonic scalers and air/water syringes, should be switched on and flushed through before use for at least two minutes at the beginning of each working day and for at least 20–30 s before each patient), f) filters (≤0.2 μm) that can trap micro-organisms coming from inside the water supply network should be installed immediately upstream of handpieces, g) in the case of invasive surgical procedures with implantology motors, only sterile water should be used, and the supply network should also be sterile, h) if sterility of the dental unit’s supply network cannot be guaranteed, a bypass system should be created and disposable sterile devices, or sterilizable devices, should be used.
5. Conclusions
Our findings suggest that dental associations should conduct mandatory workshops, training sessions and seminars to raise the awareness of the water quality and quantity maintenance in dental offices, especially to general dentists and dentists having studied abroad. Water quality in the dental office is a big issue depending on the unit, the network of waterlines, the use of filters, the age and type of the equipment, the procedures, and materials [127,128].
The biggest impact factor though is the human factor, the professionals themselves, their overall education and water quality knowledge, experience, and willingness to invest in green procedures that may seem or are more expensive [15,128,130].Young dentists should invest in green strategies, revised protocols, and comparative legislation addressing four-handed dentistry even at the beginning of their career. Successful and water green sustainable offices can be the scope of not only those managing big clinics but also dentists less educated or specialized. Dentists should be dedicated to excellency and constantly invest in revised continuing education knowledge, financing opportunities and auxiliary staff education. They should also invest in slow dentistry procedures and better time and protocol management for all water systems of the clinic. Professionals should also decide on withdrawing old equipment not corresponding to green standards with governmental financing as done in other fields of green buildings’ philosophy. Limitations of the present study that should be taken into consideration for future coverage should include a far bigger sample to overlook residence differences (urban vs non-urban offices) since urbanism seems to affect environmentalism [131]. Due to the subjective nature of the questionnaire, the study should be repeated after an information-based campaign through official network to address possible changes in dental eco-culture.
Author Contributions
Conceptualization, Μ.A., A.Ι., V.S. and C.K.; methodology, M.A.; software, M.A.; validation, M.A., A.I., C.K.; formal analysis, M.A.; investigation, M.A., A.I., C.K., I.C., S.C., M.P., X.X., V.S.; resources, M.A.; data curation, M.A.; writing—original draft preparation, M.A., A.I., C.K., I.C., S.C., M.P.; writing—review and editing, all; visualization, M.A.; supervision, M.A.; project administration, M.A.; funding acquisition, M.A.. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partly financed by the Specific Account for Grant research of the School of Health Sciences, National and Kapodistrian University of Athens.
Institutional Review Board Statement
“The study was conducted in accordance with the Declaration of Helsinki and approved by the Scientific Board of the Athens Regional Dental Association (No:2660/08.12.2022).
Informed Consent Statement
Informed consent was obtained by filling out the questionnaire. The investigation was based on an anonymous online survey with explanations posted in the accompanying email and introduction section of the survey. Submitted responses were considered as obtained informed consent.
Data Availability Statement
Data supporting reported results can be found in Appendix A.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Table with Descriptive Statistics of Dentistry Equipment and Water Quality Practices (N=206)
Table of Descriptive statistics of dentistry equipment and water quality practices (N=206)
| N | % | ||
| Equipment How Old | 0-5 years | 43 | 20.90% |
| 6-10 years | 41 | 19.90% | |
| 11-20 years | 88 | 42.70% | |
| 21 years and older | 34 | 16.50% | |
| Has assistant | No | 109 | 52.90% |
| Yes | 97 | 47.10% | |
| Was informed when acquiring | No | 80 | 38.80% |
| Yes | 126 | 61.20% | |
| Interested in learning more | No | 44 | 21.40% |
| Yes | 162 | 78.60% | |
| Confident about water quality | No | 92 | 44.70% |
| Yes | 114 | 55.30% | |
| Performs microbiological test | No | 161 | 78.20% |
| Yes | 45 | 21.80% | |
| Continuous water supply system dental unit | No | 144 | 69.90% |
| Yes | 62 | 30.10% | |
| Continuous water supply system cutters | No | 137 | 66.50% |
| Yes | 69 | 33.50% | |
| Water supply to the dental unit | Water from public network | 130 | 65.00% |
| Distilled/Deionized water | 15 | 7.50% | |
| Water from a filter device directly connected to the supply | 55 | 27.50% | |
| Water supply to the cutters | Water from public network | 124 | 62.30% |
| Deionized/Distilled water | 22 | 11.10% | |
| Water from a filter device directly connected to the supply | 53 | 26.60% | |
| Supply to ultrasounds | Water from public network | 114 | 58.50% |
| Distilled/Deionized water | 31 | 15.90% | |
| Water from a filter device directly connected to the supply | 50 | 25.60% | |
| Has water filter | No | 91 | 44.20% |
| Yes | 115 | 55.80% | |
| Water filter replaced/cleaned | No filter/Don’t want to answer | 99 | 52.10% |
| every month | 5 | 2.60% | |
| every 6 months | 36 | 18.90% | |
| every 12 months | 21 | 11.10% | |
| every 2 years | 9 | 4.70% | |
| every 5 years + | 4 | 2.10% | |
| whenever there is a problem with the flow | 16 | 8.40% | |
| Knows the active substance of antisepticAntiseptic to the incisors (auto) | No | 148 | 71.80% |
| Yes | 58 | 28.20% | |
| No | 164 | 90.60% | |
| Antiseptic to the incisors (manually) | Yes | 17 | 9.40% |
| No | 155 | 85.60% | |
| Yes | 26 | 14.40% | |
| Antiseptic reservoir | No | 8 | 3.90% |
| Yes | 198 | 96.10% | |
| Has strong surgical suction | No | 11 | 5.30% |
| Yes | 195 | 94.70% | |
| SmallSalivary | between two patients | 78 | 39.60% |
| every few appointments (3-4) | 37 | 18.80% | |
| per day | 55 | 27.90% | |
| per week | 21 | 10.70% | |
| never before covid | 4 | 2.00% | |
| never again due to covid i let patients flush | 2 | 1.00% | |
| LargeSalivary | between two patients | 18 | 9.00% |
| every few appointments (3-4) | 23 | 11.50% | |
| per day | 89 | 44.50% | |
| per week | 57 | 28.50% | |
| per month | 6 | 3.00% | |
| Never | 7 | 3.50% | |
| SmallSuction | between two patients | 90 | 45.50% |
| every few appointments (3-4) | 30 | 15.20% | |
| per day | 53 | 26.80% | |
| per week | 14 | 7.10% | |
| per month | 5 | 2.50% | |
| Never | 6 | 3.00% | |
| LargeSuction | between two patients | 15 | 7.70% |
| every few appointments (3-4) | 24 | 12.20% | |
| per day | 84 | 42.90% | |
| per week | 58 | 29.60% | |
| per month | 7 | 3.60% | |
| Never | 8 | 4.10% | |
| LargeDentalMach | between two patients | 14 | 7.80% |
| every few appointments (3-4) | 13 | 7.30% | |
| per day | 56 | 31.30% | |
| per week | 54 | 30.20% | |
| per month | 16 | 8.90% | |
| Never | 26 | 14.50% | |
| DisinfSurfaces | between two patients | 189 | 92.20% |
| every few appointments (3-4) | 8 | 3.90% | |
| per day | 7 | 3.40% | |
| per week | 1 | 0.50% | |
| Annual maintenance | No | 76 | 38.40% |
| Yes | 122 | 61.60% | |
| Micromotors | 1 | 51 | 24.80% |
| 2 | 69 | 33.50% | |
| 3 | 24 | 11.70% | |
| 4 | 25 | 12.10% | |
| 5+ | 37 | 18.00% | |
| Airotors | 1 | 29 | 14.10% |
| 2 | 63 | 30.60% | |
| 3 | 27 | 13.10% | |
| 4 | 25 | 12.10% | |
| 5+ | 62 | 30.10% | |
| HandlesClean | Decontamination | 120 | 58.30% |
| Decontamination/Sterilization | 14 | 6.80% | |
| Sterilization | 36 | 17.50% | |
| Surface cleaning | 36 | 17.50% | |
| Has implantology motor | No | 128 | 62.40% |
| Yes | 77 | 37.60% | |
| Via suction vs central drain | No | 79 | 46.20% |
| Yes | 92 | 53.80% | |
| Has amagalm trap | No | 70 | 35.40% |
| Yes | 128 | 64.60% | |
| Has contract with sewage collection company | No | 82 | 41.80% |
| Yes | 114 | 58.20% | |
| Has contract amagalm removal | No | 141 | 73.40% |
| Yes | 51 | 26.60% | |
| Is informed about water quality legislation | No | 167 | 85.60% |
| Yes | 28 | 14.40% | |
| Time spent | no time | 5 | 2.40% |
| up to 2 hours per month | 57 | 27.70% | |
| up to 4 hours per month | 62 | 30.10% | |
| more than 4 hours | 82 | 39.80% | |
| Money spent | 0 euros per month | 8 | 3.90% |
| less than 25 euros per month | 44 | 21.40% | |
| 25-50 euros per month | 89 | 43.20% | |
| 51-75 euros per month | 38 | 18.40% | |
| more than 75 euros per month | 27 | 13.10% | |
| Environmentally friendly practices | a little bit | 28 | 15.40% |
| Satisfactorily | 85 | 46.70% | |
| Enough | 50 | 27.50% | |
| very much | 19 | 10.40% | |
| Implementation of disinfection protocol is my responsibility | No | 86 | 41.70% |
| Yes | 120 | 58.30% | |
| More strict after Covid-19 | No | 99 | 49.30% |
| Yes | 102 | 50.70% |
References
- Department of health. Environment and sustainability Health Technical Memorandum 07-04: Water management and water efficiency – best practice advice for the healthcare sector. Copyright 2013. Available online: http://www.nationalarchives.gov.uk/doc/open-government-licence/ (accessed on 15 March 2023).
- Facciolà, A.; Laganà, P.; Caruso, G. The COVID-19 pandemic and its implications on the environment. Environ. Res. 2021, 201, 111648–111648. [Google Scholar] [CrossRef] [PubMed]
- Lawler, O.K.; Allan, H.L.; Baxter, P.W.J.; Castagnino, R.; Tor, M.C.; E Dann, L.; Hungerford, J.; Karmacharya, D.; Lloyd, T.J.; López-Jara, M.J.; et al. The COVID-19 pandemic is intricately linked to biodiversity loss and ecosystem health. Lancet Planet. Heal. 2021, 5, e840–e850. [Google Scholar] [CrossRef] [PubMed]
- Marazziti, D.; Cianconi, P.; Mucci, F.; Foresi, L.; Chiarantini, I.; Della Vecchia, A. Climate change, environment pollution, COVID-19 pandemic and mental health. Sci. Total. Environ. 2021, 773, 145182–145182. [Google Scholar] [CrossRef] [PubMed]
- Nandi, S.; Sarkis, J.; Hervani, A.A.; Helms, M.M. Redesigning Supply Chains using Blockchain-Enabled Circular Economy and COVID-19 Experiences. Sustain. Prod. Consum. 2020, 27, 10–22. [Google Scholar] [CrossRef] [PubMed]
- uropean Commision. Communication from the commission to the European Parliament, the council , the European economic and social committee and the committee of the regions. EU Biodiversity Strategy for 2030. Bringing nature back into our lives. Brussels, 20.5.2020. COM(2020) 380 final.
- Intergovernmental science-policy Plaform for Biodiversity and Ecosystem Services (IPBES) (2019), Summary for policymakers of the global assessment report on biodiversity and ecosystem services of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services, pp. 12-13, A.2.
- European Commission, DG Environment. Available online: http://ec.europa.eu/environment/water/index_en.htm (accessed on 15 March 2023).
- European Environmental Bureau. EEB position for a revised Urban Waste Water Directive. Available online: https://eeb.org/wp-content/uploads/2021/07/EEB-position-for-a-revised-UWWTD.pdf (accessed on 15 April 2023).
- European Parliament. Revision of the Urban Wastewater Treatment Directive. Available online: https://www.europarl.europa.eu/legislative-train/theme-a-european-green-deal/file-revision-of-the-urban-wastewater-treatment-directive-(refit).
- European Green Deal. Available online: https://www.consilium.europa.eu/en/policies/green-deal/#:~:text=The%20European%20Green%20Deal%20is%20a%20package%20of%20policy%20initiatives,a%20modern%20and%20competitive%20economy (accessed on 15 March 2023).
- CDC. Reduce Risk from Water. Available online: https://www.cdc.gov/hai/prevent/environment/water.html.
- World Economic Forum (2020). Nature Risk Rising: Why the Crisis Engulfing Nature Matters for Business and the Economy.
- European Environment Agency. Available online: http://www.eea.europa.eu/publications/european-waters-synthesis-2012.
- Leach, R. Water Management and IP Risk. Infection Control Today, 2023; 27 (3).
- Rezania, S.; Park, J.; Din, M.F.M.; Taib, S.M.; Talaiekhozani, A.; Yadav, K.K.; Kamyab, H. Microplastics pollution in different aquatic environments and biota: A review of recent studies. Mar. Pollut. Bull. 2018, 133, 191–208. [Google Scholar] [CrossRef]
- Dulsat-Masvidal, M.; Ciudad, C.; Infante, O.; Mateo, R.; Lacorte, S. Water pollution threats in important bird and biodiversity areas from Spain. J. Hazard. Mater. 2023, 448, 130938. [Google Scholar] [CrossRef]
- EYDAP Sustainable Development Report. (2021). Sustainable Development EYDAP SA. Athens. Available online: https://www.eydap.gr/userfiles/Presentations/presentations/EYDAP_CSR_2021_21x29-7CM_F13_WEB/index.html#page=1 (accessed on 15 March 2023).
- Preliminary plan for water resources. Available online: http://ec.europa.eu/environment/water/blueprint/index_en.htm (accessed on 20 March 2023).
- Facts and figures of the WFD. Available online: http://ec.europa.eu/environment/water/water-framework/facts_figures/index_en.htm.
- Water Information System for Europe (WISE). Available online: http://water.europa.eu/ (accessed on 20 March 2023).
- European Innovation Partnership on Water. Available online: http://ec.europa.eu/environment/water/innovationpartnership/ (accessed on 20 March 2023).
- Government Gazette. (2017, Σεπτέμβριος 19). Quality of water intended for human consumption in compliance with the provisions of the Directive 98/83/ΕΚ of the Council of the European Union of as amended by Directive (ΕΕ) 2015/1787 (L260, 7.10.2015). No. Sheet 3282, Τεύχος 2. 3 November.
- Joint Research Centre. Available online: http://ec.europa.eu/dgs/jrc/index.cfm?id=10 (accessed on 20 March 2023).
- Horizon 2020. Available online: http://ec.europa.eu/programmes/horizon2020/ (accessed on 20 March 2023).
- Council of the European Union. (2015, Oκτώβριος 27). Directive 98/83/ΕΚ of 3 November 1998 on the quality of water intended for human consumption. 0199. Available online: https://eur-lex.europa.eu/legal-content/EL/TXT/PDF/?uri=CELEX:01998L0083-20151027&from=EN (accessed on 20 March 2023).
- EU. Directorate-General for Environment. Proposal for Ecodesign for Sustainable Products Regulation. Annexes - Proposal for a Regulation establishing a framework for setting Ecodesign requirements for sustainable products and repealing Directive 2009/125/EC. Available online: https://environment.ec.europa.eu/publications/proposal-ecodesign-sustainable-products-regulation_en.
- Szymańska, J.; Sitkowska, J. Bacterial contamination of dental unit waterlines. Environ. Monit. Assess. 2012, 185, 3603–3611. [Google Scholar] [CrossRef]
- Yuan, Q.; Zhang, M.; Zhou, J. To Implement A Clear-Water Supply System for Fine-Sediment Experiment in Laboratories. Water 2019, 11, 2476. [Google Scholar] [CrossRef]
- Cicciu’, M.; Fiorillo, L.; Herford, A.S.; Crimi, S.; Bianchi, A.; D’Amico, C.; Laino, L.; Cervino, G. Bioactive Titanium Surfaces: Interactions of Eukaryotic and Prokaryotic Cells of Nano Devices Applied to Dental Practice. Biomedicines 2019, 7, 12. [Google Scholar] [CrossRef]
- Cicciù, M. Water Contamination Risks at the Dental Clinic. Biology 2020, 9, 43. [Google Scholar] [CrossRef]
- ntoniadou M, Tzoutzas I, Tzermpos F, Panis V, Maltezou H, Tseroni M, Madianos F. Infection control during COVID-19 outbreak in a university dental school. J Oral Hyg Health 2020, 8, 4.
- Cataldi, M.E.; Al Rakayan, S.; Arcuri, C.; Condò, R. DENTAL UNIT WASTEWATER, A CURRENT ENVIRONMENTAL PROBLEM: A SISTEMATIC REVIEW. Oral Implant. 2017, 10, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Innes, N.; Johnson, I.; Al-Yaseen, W.; Harris, R.; Jones, R.; Kc, S.; McGregor, S.; Robertson, M.; Wade, W.; Gallagher, J. A systematic review of droplet and aerosol generation in dentistry. J. Dent. 2020, 105, 103556–103556. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, J.-I.; Imazato, S. Autoclave sterilization of dental handpieces: A literature review. J. Prosthodont. Res. 2020, 64, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Tseroni, M.; Vorou, R.; Koutsolioutsou, A.; Antoniadou, M.; Tzoutzas, I.; Panis, V.; Tzermpos, F.; Madianos, P. Preparing dental schools to refunction safely during the COVID-19 pandemic: an infection prevention and control perspective. J. Infect. Dev. Ctries. 2021, 15, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Spagnolo, A.M.; Sartini, M.; Di Cave, D.; Casini, B.; Tuvo, B.; Cristina, M.L. Evaluation of Microbiological and Free-Living Protozoa Contamination in Dental Unit Waterlines. Int. J. Environ. Res. Public Heal. 2019, 16, 2648. [Google Scholar] [CrossRef] [PubMed]
- Spagnolo, A.M.; Sartini, M.; Cristina, M.L. Microbial Contamination of Dental Unit Waterlines and Potential Risk of Infection: A Narrative Review. Pathogens 2020, 9, 651. [Google Scholar] [CrossRef]
- Senpuku, H.; Fukumoto, M.; Uchiyama, T.; Taguchi, C.; Suzuki, I.; Arikawa, K. Effects of Extraoral Suction on Droplets and Aerosols for Infection Control Practices. Dent. J. 2021, 9, 80. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K. Dental Aerosol as a Hazard Risk for Dental Workers. Materials 2020, 13, 5109. [Google Scholar] [CrossRef]
- Centers for disease control and prevention. Summary of Infection Prevention Practices in Dental Settings. Basic Expectations for Safe Care. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; October 2016. Available online: https://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care2.pdf (accessed on 20 March 2023).
- Leoni, E.; Dallolio, L.; Stagni, F.; Sanna, T.; D’Alessandro, G.; Piana, G. Impact of a Risk Management Plan on Legionella Contamination of Dental Unit Water. Int. J. Environ. Res. Public Heal. 2015, 12, 2344–2358. [Google Scholar] [CrossRef]
- Dallolio, L.; Scuderi, A.; Rini, M.S.; Valente, S.; Farruggia, P.; Sabattini, M.A.B.; Pasquinelli, G.; Acacci, A.; Roncarati, G.; Leoni, E. Effect of Different Disinfection Protocols on Microbial and Biofilm Contamination of Dental Unit Waterlines in Community Dental Practices. Int. J. Environ. Res. Public Heal. 2014, 11, 2064–2076. [Google Scholar] [CrossRef] [PubMed]
- Shajahan, I.F.; Kandaswamy, D.; Srikanth, P.; Narayana, L.L.; Selvarajan, R. Dental unit waterlines disinfection using hypochlorous acid-based disinfectant. J. Conserv. Dent. 2016, 19, 347–350. [Google Scholar] [CrossRef] [PubMed]
- Ditommaso, S.; Giacomuzzi, M.; Ricciardi, E.; Zotti, C.M. Efficacy of a Low Dose of Hydrogen Peroxide (Peroxy Ag+) for Continuous Treatment of Dental Unit Water Lines: Challenge Test with Legionella pneumophila Serogroup 1 in a Simulated Dental Unit Waterline. Int. J. Environ. Res. Public Heal. 2016, 13, 745. [Google Scholar] [CrossRef] [PubMed]
- Lizzadro, J.; Mazzotta, M.; Girolamini, L.; Dormi, A.; Pellati, T.; Cristino, S. Comparison between Two Types of Dental Unit Waterlines: How Evaluation of Microbiological Contamination Can Support Risk Containment. Int. J. Environ. Res. Public Heal. 2019, 16, 328. [Google Scholar] [CrossRef] [PubMed]
- Noopan, S.; Unchui, P.; Techotinnakorn, S.; Ampornaramveth, R.S. Plasma Sterilization Effectively Reduces Bacterial Contamination in Dental Unit Waterlines. Int. J. Dent. 2019, 2019, 1–6. [Google Scholar] [CrossRef]
- Han, P.; Li, H.; Walsh, L.J.; Ivanovski, S. Splatters and Aerosols Contamination in Dental Aerosol Generating Procedures. Appl. Sci. 2021, 11, 1914. [Google Scholar] [CrossRef]
- Fiorillo, L. Conscious Sedation in Dentistry. Medicina 2019, 55, 778. [Google Scholar] [CrossRef]
- Walker, J.T.; Bradshaw, D.J.; Bennett, A.M.; Fulford, M.R.; Martin, M.V.; Marsh, P.D. Microbial Biofilm Formation and Contamination of Dental-Unit Water Systems in General Dental Practice. Appl. Environ. Microbiol. 2000, 66, 3363–3367. [Google Scholar] [CrossRef]
- Walker, J.T.; Bradshaw, D.J.; Fulford, M.R.; Marsh, P.D. Microbiological Evaluation of a Range of Disinfectant Products To Control Mixed-Species Biofilm Contamination in a Laboratory Model of a Dental Unit Water System. Appl. Environ. Microbiol. 2003, 69, 3327–3332. [Google Scholar] [CrossRef]
- Yabune, T.; Imazato, S.; Ebisu, S. Assessment of Inhibitory Effects of Fluoride-Coated Tubes on Biofilm Formation by Using the In Vitro Dental Unit Waterline Biofilm Model. Appl. Environ. Microbiol. 2008, 74, 5958–5964. [Google Scholar] [CrossRef]
- Costa, D.; Girardot, M.; Bertaux, J.; Verdon, J.; Imbert, C. Efficacy of dental unit waterlines disinfectants on a polymicrobial biofilm. Water Res. 2016, 91, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Tuvo, B.; Totaro, M.; Cristina, M.L.; Spagnolo, A.M.; Di Cave, D.; Profeti, S.; Baggiani, A.; Privitera, G.; Casini, B. Prevention and Control of Legionella and Pseudomonas spp. Colonization in Dental Units. Pathogens 2020, 9, 305. [Google Scholar] [CrossRef] [PubMed]
- Hoogenkamp, M.A.; Brandt, B.W.; Laheij, A.M.; de Soet, J.J.; Crielaard, W. The microbiological load and microbiome of the Dutch dental unit; ‘please, hold your breath’. Water Res. 2021, 200, 117205. [Google Scholar] [CrossRef] [PubMed]
- Gawlik, BM, Easton P, Koop S, Van Leeuwen K, Elelman R. (eds.), 2017, Urban Water Atlas for Europe. European Commission, Publications Office of the European Union, Luxembourg. 160 pp. [CrossRef]
- EYDAP SA. (n.d.). Available online: https://www.eydap.gr/ (accessed on 20 March 2023).
- Engsomboon, N.; Pachimsawat, P.; Thanathornwong, B. Comparative Dissemination of Aerosol and Splatter Using Suction Device during Ultrasonic Scaling: A Pilot Study. Dent. J. 2022, 10, 142. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xu, Z.; Ma, H.; Hursthouse, A.S. Removal of Manganese(II) from Acid Mine Wastewater: A Review of the Challenges and Opportunities with Special Emphasis on Mn-Oxidizing Bacteria and Microalgae. Water 2019, 11, 2493. [Google Scholar] [CrossRef]
- Engelmann, C.; Schmidt, L.; Werth, C.J.; Walther, M. Quantification of Uncertainties from Image Processing and Analysis in Laboratory-Scale DNAPL Release Studies Evaluated by Reflective Optical Imaging. Water 2019, 11, 2274. [Google Scholar] [CrossRef]
- Yoon, H.Y.; Lee, S.Y. Susceptibility of bacteria isolated from dental unit waterlines to disinfecting chemical agents. J. Gen. Appl. Microbiol. 2018, 64, 269–275. [Google Scholar] [CrossRef]
- Ajami, B.; Ghazvini, K.; Movahhed, T.; Ariaee, N.; Shakeri, M.; Makarem, S. Contamination of a Dental Unit Water Line System by Legionella Pneumophila in the Mashhad School of Dentistry in 2009. 2012, 14, 376–378.
- Cervino, G.; Fiorillo, L.; Monte, I.P.; De Stefano, R.; Laino, L.; Crimi, S.; Bianchi, A.; Herford, A.S.; Biondi, A.; Cicciù, M. Advances in Antiplatelet Therapy for Dentofacial Surgery Patients: Focus on Past and Present Strategies. Materials 2019, 12, 1524. [Google Scholar] [CrossRef]
- Mills, S.E. THE DENTAL UNIT WATERLINE CONTROVERSY: DEFUSING THE MYTHS, DEFINING THE SOLUTIONS. J. Am. Dent. Assoc. 2000, 131, 1427–1441. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Laino, L.; Herford, A.S.; Lauritano, F.; Giudice, G.L.; Famà, F.; Santoro, R.; Troiano, G.; Iannello, G.; et al. Oral Health Impact Profile in Celiac Patients: Analysis of Recent Findings in a Literature Review. Gastroenterol. Res. Pr. 2018, 2018, 1–9. [Google Scholar] [CrossRef]
- Gawish, S.; Abbass, A.; Abaza, A. Occurrence and biofilm forming ability of Pseudomonas aeruginosa in the water output of dental unit waterlines in a dental center in Alexandria, Egypt. GERMS 2019, 9, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Pouralibaba, F.; Balaei, E.; Kashefimehr, A. Evaluation of Gram Negative Bacterial Contamination in Dental Unit Water Supplies in a University Clinic in Tabriz, Iran. J Dent Res Dent Clin Dent Prospect 2011, 5, 94–97. [Google Scholar] [CrossRef]
- Giacomuzzi, M.; Zotti, C.M.; Ditommaso, S. Colonization of Dental Unit Waterlines by Helicobacter pylori: Risk of Exposure in Dental Practices. Int. J. Environ. Res. Public Heal. 2019, 16, 2981. [Google Scholar] [CrossRef] [PubMed]
- Cárdenas, A.M.; Campos-Bijit, V.; Di Francesco, F.; Schwarz, F.; Cafferata, E.A.; Vernal, R. Electrolyzed water for the microbiologic control in the pandemic dental setting: a systematic review. BMC Oral Heal. 2022, 22, 1–43. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, A.; Smith, G.; Smith, A. Biofouling of surgical power tools during routine use. J. Hosp. Infect. 2015, 90, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Kauppinen, A.; Pitkänen, T.; Al-Hello, H.; Maunula, L.; Hokajärvi, A.-M.; Rimhanen-Finne, R.; Miettinen, I.T. Two Drinking Water Outbreaks Caused by Wastewater Intrusion Including Sapovirus in Finland. Int. J. Environ. Res. Public Heal. 2019, 16, 4376. [Google Scholar] [CrossRef] [PubMed]
- Pasquarella, C.; Veronesi, L.; Napoli, C.; Castiglia, P.; Liguori, G.; Rizzetto, R.; Torre, I.; Righi, E.; Farruggia, P.; Tesauro, M.; et al. Microbial environmental contamination in Italian dental clinics: A multicenter study yielding recommendations for standardized sampling methods and threshold values. Sci. Total. Environ. 2012, 420, 289–299. [Google Scholar] [CrossRef]
- Zhang, Y.; Ping, Y.; Zhou, R.; Wang, J.; Zhang, G. High throughput sequencing-based analysis of microbial diversity in dental unit waterlines supports the importance of providing safe water for clinical use. J. Infect. Public Heal. 2018, 11, 357–363. [Google Scholar] [CrossRef]
- Mazari, W.; Boucherit-Otmani, Z.; El Haci, I.A.; Ilahi, A.; Boucherit, K. Risk assessment for the spread of Candida sp. in dental chair unit waterlines using molecular techniques. Int. Dent. J. 2020, 68, 386–392. [Google Scholar] [CrossRef]
- Fiorillo, L. We Do Not Eat Alone: Formation and Maturation of the Oral Microbiota. Biology 2020, 9, 17. [Google Scholar] [CrossRef]
- Adedoja, O.S.; Hamam, Y.; Khalaf, B.; Sadiku, R. Development of a Contaminant Distribution Model for Water Supply Systems. Water 2019, 11, 1510. [Google Scholar] [CrossRef]
- Watanabe, A.; Tamaki, N.; Yokota, K.; Matsuyama, M.; Kokeguchi, S. Monitoring of bacterial contamination of dental unit water lines using adenosine triphosphate bioluminescence. J. Hosp. Infect. 2016, 94, 393–396. [Google Scholar] [CrossRef] [PubMed]
- Baudet, A.; Lizon, J.; Martrette, J.-M.; Camelot, F.; Florentin, A.; Clément, C. Efficacy of BRS® and Alpron®/Bilpron® Disinfectants for Dental Unit Waterlines: A Six-Year Study. Int. J. Environ. Res. Public Heal. 2020, 17, 2634. [Google Scholar] [CrossRef] [PubMed]
- Putnins, E.E.; Di Giovanni, D.; Bhullar, A.S. Dental Unit Waterline Contamination and Its Possible Implications During Periodontal Surgery. J. Periodontol. 2001, 72, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Toomarian, L.; Rikhtegaran, S.; Sadighi, M.; Oskoee, S.S.; Oskoee, P.A. Contamination of Dental Unit Water and Air Outlets Following Use of Clean Head System and Conventional Handpieces. J Dent Res Dent Clin Dent Prospect 2007, 1, 43–47. [Google Scholar] [CrossRef]
- Laino, L.; Cicciù, M.; Fiorillo, L.; Crimi, S.; Bianchi, A.; Amoroso, G.; Monte, I.P.; Herford, A.S.; Cervino, G. Surgical Risk on Patients with Coagulopathies: Guidelines on Hemophiliac Patients for Oro-Maxillofacial Surgery. Int. J. Environ. Res. Public Health 2019, 16, 1386. [Google Scholar] [CrossRef]
- Takenaka, S.; Sotozono, M.; Yashiro, A.; Saito, R.; Kornsombut, N.; Naksagoon, T.; Nagata, R.; Ida, T.; Edanami, N.; Noiri, Y. Efficacy of Combining an Extraoral High-Volume Evacuator with Preprocedural Mouth Rinsing in Reducing Aerosol Contamination Produced by Ultrasonic Scaling. Int. J. Environ. Res. Public Heal. 2022, 19, 6048. [Google Scholar] [CrossRef]
- Acosta-Gio, E.; Bednarsh, H.; Cuny, E.; Eklund, K.; Mills, S.; Risk, D. Sterilization of dental handpieces. Am. J. Infect. Control. 2017, 45, 937–938. [Google Scholar] [CrossRef]
- Walker, J.; Marsh, P. Microbial biofilm formation in DUWS and their control using disinfectants. J. Dent. 2007, 35, 721–730. [Google Scholar] [CrossRef]
- Offner, D.; Fioretti, F.; Musset, A.-M. Contamination of dental unit waterlines: assessment of three continuous water disinfection systems. BDJ Open 2016, 2, 16007. [Google Scholar] [CrossRef]
- Pawar, A.; Garg, S.; Mehta, S.; Dang, R. Breaking the Chain of Infection: Dental Unit Water Quality Control. J. Clin. Diagn. Res. 2016, 10, ZC80–4. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.K.; Mittal, S.; Kaur, P. Dental unit waterline management: historical perspectives and current trends. J. Investig. Clin. Dent. 2012, 3, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Jaywant, S.A.; Arif, K.M. A Comprehensive Review of Microfluidic Water Quality Monitoring Sensors. Sensors 2019, 19, 4781. [Google Scholar] [CrossRef] [PubMed]
- Kwietniewski, M.; Miszta-Kruk, K.; Niewitecka, K.; Sudoł, M.; Gaska, K. Certainty Level of Water Delivery of the Required Quality by Water Supply Networks. Int. J. Environ. Res. Public Heal. 2019, 16, 1860. [Google Scholar] [CrossRef] [PubMed]
- Fujita, M.; Mashima, I.; Nakazawa, F. Monitoring the decontamination efficacy of the novel Poseidon-S disinfectant system in dental unit water lines. J. Microbiol. Immunol. Infect. 2017, 50, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Noopan, S.; Unchui, P.; Techotinnakorn, S.; Ampornaramveth, R.S. Plasma Sterilization Effectively Reduces Bacterial Contamination in Dental Unit Waterlines. Int. J. Dent. 2019, 2019, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pantanella, F.; Schippa, S.; Solimini, A.; Rosa, L.; Bettucci, A.; Berlutti, F. Efficacy of acoustic waves in preventing Streptococcus mutans adhesion on dental unit water line. . 2019, 31, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Troiano, G.; Laino, L.; Cicciù, M.; Cervino, G.; Fiorillo, L.; D’amico, C.; Zhurakivska, K.; Muzio, L.L. Comparison of Two Routes of Administration of Dexamethasone to Reduce the Postoperative Sequelae After Third Molar Surgery: A Systematic Review and Meta-Analysis. Open Dent. J. 2018, 12, 181–188. [Google Scholar] [CrossRef]
- Kohn, W.G.; Collins, A.S.; Cleveland, J.L.; Harte, J.A.; Eklund, K.J.; Malvitz, D.M.; Centers for Disease Control and Prevention (CDC). Guidelines for infection control in dental health-care settings—2003. MMWR. Recomm. Rep. 2003, 52, 1–61. [Google Scholar]
- ADA STATEMENT ON DENTAL UNIT WATERLINES. J. Am. Dent. Assoc. 1996, 127, 185–186. [CrossRef]
- Rosa, V.; Agarwalla, S.V.; Tan, B.L.; Choo, S.Y.; Sim, Y.F.; Boey, F.Y.C.; Anantharaman, S.; Duggal, M.S.; Tan, K.S. Pandemic Preparedness and Response: A Foldable Tent to Safely Remove Contaminated Dental Aerosols—Clinical Study and Patient Experience. Appl. Sci. 2022, 12, 7409. [Google Scholar] [CrossRef]
- Alkhulaifi, M.M.; Alotaibi, D.H.; Alajlan, H.; Binshoail, T. Assessment of nosocomial bacterial contamination in dental unit waterlines: Impact of flushing. Saudi Dent. J. 2020, 32, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Tims, M.; Bakker, A.B.; Derks, D. Development and validation of the job crafting scale. J. Vocat. Behav. 2012, 80, 173–186. [Google Scholar] [CrossRef]
- Bursac, Z.; Gauss, C.H.; Williams, D.K.; Hosmer, D.W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 2008, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Green, H.; Weller, D.; Johnson, S.; Michalenko, E. Microbial Source-Tracking Reveals Origins of Fecal Contamination in a Recovering Watershed. Water 2019, 11, 2162. [Google Scholar] [CrossRef] [PubMed]
- Ayers, K.M.; Thomson, W.M.; Rich, A.M.; Newton, J.T. Gender differences in dentists’ working practices and job satisfaction. J. Dent. 2008, 36, 343–350. [Google Scholar] [CrossRef] [PubMed]
- McKay, J.C.; Ahmad, A.; Shaw, J.L.; Rashid, F.; Clancy, A.; David, C.; Figueiredo, R.; Quiñonez, C. Gender Differences and Predictors of Work Hours in a Sample of Ontario Dentists. J Can Dent Assoc 2016, 82, g26. [Google Scholar]
- Walker, S.; Flores-Mir, C.; Heo, G.; Amin, M.S.; Keenan, L. Work pattern differences between male and female orthodontists in Canada. J Can Dent Assoc 2016, 82, g6. [Google Scholar]
- Emrani, R.; Sargeran, K.; Shamshiri, A.R.; Hessari, H. Job Satisfaction Among Dentists According to Workplace in Tehran. Front. Dent. 2021, 18, 11. [Google Scholar] [CrossRef]
- Surdu, S.; Mertz, E.; Langelier, M.; Moore, J. Dental Workforce Trends: A National Study of Gender Diversity and Practice Patterns. Med Care Res. Rev. 2020, 78, 30S–39S. [Google Scholar] [CrossRef]
- Archer, J. The reality and evolutionary significance of human psychological sex differences. Biol. Rev. 2019, 94, 1381–1415. [Google Scholar] [CrossRef] [PubMed]
- Baptiste, D.; Fecher, A.M.; Dolejs, S.C.; Yoder, J.; Schmidt, C.M.; Couch, M.E.; Ceppa, D.P. Gender differences in academic surgery, work-life balance, and satisfaction. J. Surg. Res. 2017, 218, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Rich-Edwards, J.W.; Kaiser, U.B.; Chen, G.L.; Manson, J.E.; Goldstein, J.M. Sex and Gender Differences Research Design for Basic, Clinical, and Population Studies: Essentials for Investigators. Endocr. Rev. 2018, 39, 424–439. [Google Scholar] [CrossRef] [PubMed]
- Shannon G, Jansen M, Williams K, Cáceres C, Motta A, Odhiambo A et al. Gender equality in science, medicine, and global health: where are we at and why does it matter? Lancet 2019, 393, 560–569. [CrossRef] [PubMed]
- Nirupama YS, Boppana NK, Vinnakota NR, Thetakala RK, Kallakuri P, Karthik BK. Indian women dentists’ perspectives towards balancing professional, personal and social responsibilities. J Dent Res 2020, 31, 358–362.
- Antoniadou, M. Estimation of Factors Affecting Burnout in Greek Dentists before and during the COVID-19 Pandemic. Dent. J. 2022, 10, 108. [Google Scholar] [CrossRef] [PubMed]
- Dousin, O.; Collins, N.; Kler, B.K. The experience of work-life balance for women doctors and nurses in Malaysia. Asia Pac. J. Hum. Resour. 2021, 60, 362–380. [Google Scholar] [CrossRef]
- McCarthy, G.M.; Macdonald, J.K. Gender differences in characteristics, infection control practices, knowledge and attitudes related to HIV among Ontario dentists. Community Dent. Oral Epidemiol. 1996, 24, 412–415. [Google Scholar] [CrossRef]
- Reza E, Sargeran K, Hessari H, Masoumeh E. Differences in the work pattern of male and female dentists in Tehran in 2021. Ital J Gender-Specific Med 2022, 8, 143–146.
- Li J, de Souza R, Esfandiari S, Feine J. Have women broken the glass ceiling in North American dental leadership? J Adv Dent Res 2019, 30, 78–84. [CrossRef]
- Shahin, S.Y.; Bugshan, A.S.; Almulhim, K.S.; AlSharief, M.S.; Al-Dulaijan, Y.A.; Siddiqui, I.; Al-Qarni, F.D. Knowledge of dentists, dental auxiliaries, and students regarding the COVID-19 pandemic in Saudi Arabia: a cross-sectional survey. BMC Oral Heal. 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Qabool, H.; Sukhia, R.; Fida, M. Knowledge and awareness of dental specialists, general dentists and dental assistants regarding SARS-CoV-2. Dent. Med Probl. 2021, 58, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Schalli, M.; Kogler, B.; Miorini, T.; Gehrer, M.; Reinthaler, F.F. High-Speed Dental Instruments: An Investigation of Protein-Contaminated Dental Handpieces with the Bicinchoninic Acid Assay in Dental Offices in Styria, Austria. Int. J. Environ. Res. Public Heal. 2023, 20, 1670. [Google Scholar] [CrossRef] [PubMed]
- Pinto, F.M.G.; Bruna, C.Q.d.M.; Camargo, T.C.; Marques, M.; Silva, C.B.; Sasagawa, S.M.; Mimica, L.M.J.; Graziano, K.U. The practice of disinfection of high-speed handpieces with 70% w/v alcohol: An evaluation. Am. J. Infect. Control. 2016, 45, e19–e22. [Google Scholar] [CrossRef] [PubMed]
- Osegueda-Espinosa, A.A.D.; Sánchez-Pérez, L.D.; Perea-Pérez, B.M.; Labajo-González, E.D.; Acosta-Gio, A.E.D. Dentists Survey on Adverse Events During Their Clinical Training. J. Patient Saf. 2017, 16, e240–e244. [Google Scholar] [CrossRef]
- Hbibi, A.; Kasouati, J.; Charof, R.; Chaouir, S.; El Harti, K. Evaluation of the knowledge and attitudes of dental students toward occupational blood exposure accidents at the end of the dental training program. J. Int. Soc. Prev. Community Dent. 2018, 8, 77–86. [Google Scholar] [CrossRef]
- Agahi, R.H.; Hashemipour, M.A.; Kalantari, M.; Ayatollah-Mosavi, A.; Aghassi, H.; Nassab, A.H.G. Effect of 0.2% chlorhexidine on microbial and fungal contamination of dental unit waterlines. Dent Res 2014, 11, 351–356. [Google Scholar]
- Dupont, D.; Adamowicz, W.L.; Krupnick, A. Differences in water consumption choices in Canada: the role of socio-demographics, experiences, and perceptions of health risks. J. Water Heal. 2010, 8, 671–686. [Google Scholar] [CrossRef]
- Banakar, M.; Lankarani, K.B.; Jafarpour, D.; Moayedi, S.; Banakar, M.H.; MohammadSadeghi, A. COVID-19 transmission risk and protective protocols in dentistry: a systematic review. BMC Oral Heal. 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Chate, R.A.C. An audit improves the quality of water within the dental unit water lines of general dental practices across the East of England. Br. Dent. J. 2010, 209, E11–E11. [Google Scholar] [CrossRef]
- Italian Health Ministry. Guidelines for Prevention and Control of Legionellosis. Rome, Italy: 2015. Available online: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2362_allegato.pdf (accessed on 17 June 2020).
- Mcmanus, K.R.; Fan, P. Purchasing, installing and operating dental amalgam separators. J. Am. Dent. Assoc. 2003, 134, 1054–1065. [Google Scholar] [CrossRef] [PubMed]
- Spaveras, A.; Antoniadou, M. Awareness of Students and Dentists on Sustainability Issues, Safety of Use and Disposal of Dental Amalgam. Dent. J. 2023, 11, 21. [Google Scholar] [CrossRef] [PubMed]
- Oosthuysen, J.; Potgieter, E.; Fossey, A. Compliance with infection prevention and control in oral health-care facilities: a global perspective. Int. Dent. J. 2014, 64, 297–311. [Google Scholar] [CrossRef] [PubMed]
- Carraro E, Bonetta S, Bonetta S. Hospital Wastewater: Existing Regulations and Current Trends in Management. In: Verlicchi, P. (eds) Hospital Wastewaters. The Handbook of Environmental Chemistry, vol 60. Springer, Cham. 2017. [CrossRef]
- Antoniadou, M.; Chrysochoou, G.; Tzanetopoulos, R.; Riza, E. Green Dental Environmentalism among Students and Dentists in Greece. Sustainability 2023, 15, 9508. [Google Scholar] [CrossRef]
Figure 1.
Graph showcasing various water treatment methods and arrangements within a dental office: (i) Self-contained water systems (e.g., independent water tank) that supply the dental unit/s. (ii) Systems in-line with one or more dental units within the same dental office that filter incoming water. (iii) Systems in-line with one or more dental units within the same dental office that treat incoming water to remove or inactivate microorganisms throughout the network. These methods (i, ii, iii) can also be used sequentially in-line, e.g., tank combined with chemical treatment (periodic, or continuous chemical microbicide treatment protocols) and filters.
Figure 1.
Graph showcasing various water treatment methods and arrangements within a dental office: (i) Self-contained water systems (e.g., independent water tank) that supply the dental unit/s. (ii) Systems in-line with one or more dental units within the same dental office that filter incoming water. (iii) Systems in-line with one or more dental units within the same dental office that treat incoming water to remove or inactivate microorganisms throughout the network. These methods (i, ii, iii) can also be used sequentially in-line, e.g., tank combined with chemical treatment (periodic, or continuous chemical microbicide treatment protocols) and filters.
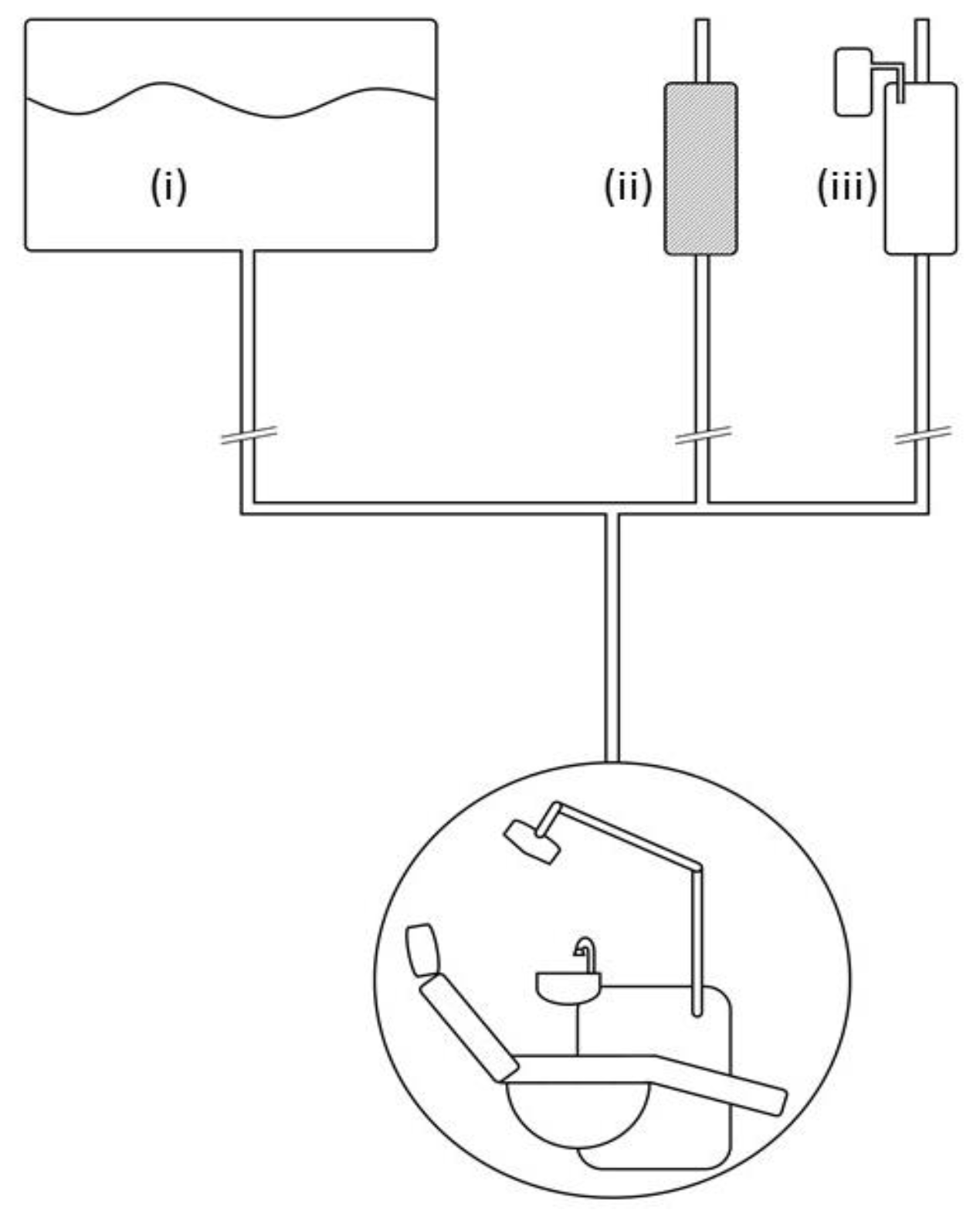
Figure 2.
Factors affecting water maintenance of a dental unit.

Table 1.
Differences between genders (male vs female) in dentistry equipment and water quality practices.
Table 1.
Differences between genders (male vs female) in dentistry equipment and water quality practices.
| Female | Male | |||||
| N | % | N | % | χ2(p) | ||
| Interested in learning more | 77 | 87.50% | 84 | 71.80% | 7.35(.006) | |
| Continuous water supply system cutters | 22 | 25.00% | 47 | 40.20% | 5.17(.023) | |
| Water supply to the dental unit | Water from public network | 62 | 73.80% | 67 | 58.30% | 8.90(.012) |
| Distilled/Deionized water | 8 | 9.50% | 7 | 6.10% | ||
| Water from a filter device directly connected to the supply | 14 | 16.70% | 41 | 35.70% | ||
| Water supply to the handpieces | Water from public network | 58 | 70.70% | 66 | 56.90% | 6.72(.035) |
| Deionized/Distilled water | 10 | 12.20% | 11 | 9.50% | ||
| Water from a filter device directly connected to the supply | 14 | 17.10% | 39 | 33.60% | ||
| Supply to ultrasonic scaler | Water from public network | 55 | 68.80% | 59 | 51.80% | 10.31(.006) |
| Distilled/Deionized water | 14 | 17.50% | 16 | 14.00% | ||
| Water from a filter device directly connected to the supply | 11 | 13.80% | 39 | 34.20% | ||
| Disinf. Surfaces | between two patients | 85 | 97.70% | 103 | 88.00% | 12.54(.028) |
| every few appointments | 0 | 0.00% | 8 | 6.80% | ||
| per day | 1 | 1.10% | 6 | 5.10% | ||
| per week | 1 | 1.10% | 0 | 0.00% | ||
| Annual maintenance | 55 | 66.30% | 66 | 57.90% | 10.10(.018) | |
| Has implantology motor | 24 | 27.60% | 52 | 44.40% | 6.07(.014) | |
Table 2.
Differences between dentists’ experience (in years) in dentistry equipment and water quality practices.
Table 2.
Differences between dentists’ experience (in years) in dentistry equipment and water quality practices.
| Experience | ||||||||||
| 0-10 έτη | 11-20 έτη | 21-30 έτη | 31 και άνω έτη | |||||||
| N | % | N | % | N | % | N | % | χ2(p) | ||
| Water supply to the dental unit | Water from public network | 25 | 89.30% | 36 | 63.20% | 37 | 64.90% | 32 | 55.20% | 13.70(.033) |
| Distilled/Deionized water | 1 | 3.60% | 7 | 12.30% | 4 | 7.00% | 3 | 5.20% | ||
| Water from filter | 2 | 7.10% | 14 | 24.60% | 16 | 28.10% | 23 | 39.70% | ||
| Water supply to the handpieces | Water from public network | 24 | 92.30% | 37 | 62.70% | 34 | 60.70% | 29 | 50.00% | 16.69(.010) |
| Deionized/Distilled water | 1 | 3.80% | 9 | 15.30% | 6 | 10.70% | 6 | 10.30% | ||
| Water from filter | 1 | 3.80% | 13 | 22.00% | 16 | 28.60% | 23 | 39.70% | ||
| Supply to ultrasonic scaler | Water from public network | 21 | 80.80% | 38 | 64.40% | 32 | 58.20% | 23 | 41.80% | 13.63(.034) |
| Distilled/Deionized water | 3 | 11.50% | 8 | 13.60% | 7 | 12.70% | 13 | 23.60% | ||
| Water from filter | 2 | 7.70% | 13 | 22.00% | 16 | 29.10% | 19 | 34.50% | ||
| Large amount of water through surgical suction to the dental unit | between two patients | 5 | 17.20% | 0 | 0.00% | 2 | 3.60% | 8 | 15.10% | 31.12(.008) |
| every few appointments (3-4) | 2 | 6.90% | 5 | 8.60% | 10 | 17.90% | 7 | 13.20% | ||
| per day | 9 | 31.00% | 28 | 48.30% | 22 | 39.30% | 25 | 47.20% | ||
| per week or more | 13 | 44.80% | 25 | 43.10% | 22 | 39.40% | 13 | 24.60% | ||
| Large amount of water to the dental unit | between two patients | 4 | 16.00% | 2 | 3.80% | 4 | 8.30% | 4 | 7.40% | 27.69(.024) |
| every few appointments (3-4) | 1 | 4.00% | 3 | 5.80% | 2 | 4.20% | 7 | 13.00% | ||
| per day | 10 | 40.00% | 11 | 21.20% | 13 | 27.10% | 22 | 40.70% | ||
| per week or more | 10 | 40.00% | 36 | 69.30% | 29 | 60.40% | 21 | 39.00% | ||
| Micromotors | 1 | 15 | 46.90% | 18 | 30.50% | 12 | 21.10% | 6 | 10.30% | 25.92(.011) |
| 2 | 5 | 15.60% | 22 | 37.30% | 19 | 33.30% | 23 | 39.70% | ||
| 3 | 3 | 9.40% | 5 | 8.50% | 9 | 15.80% | 7 | 12.10% | ||
| 4 | 3 | 9.40% | 8 | 13.60% | 3 | 5.30% | 11 | 19.00% | ||
| 5+ | 6 | 18.80% | 6 | 10.20% | 14 | 24.60% | 11 | 19.00% | ||
| Airotors | 1 | 11 | 34.40% | 8 | 13.60% | 5 | 8.80% | 5 | 8.60% | 29.17(.004) |
| 2 | 10 | 31.30% | 20 | 33.90% | 17 | 29.80% | 16 | 27.60% | ||
| 3 | 1 | 3.10% | 14 | 23.70% | 5 | 8.80% | 7 | 12.10% | ||
| 4 | 3 | 9.40% | 5 | 8.50% | 11 | 19.30% | 6 | 10.30% | ||
| 5+ | 7 | 21.90% | 12 | 20.30% | 19 | 33.30% | 24 | 41.40% | ||
| Is informed about water quality legislation | 8 | 27.60% | 3 | 5.40% | 7 | 13.20% | 10 | 17.50% | 8.34(.039) | |
| Time Spent | no time | 4 | 12.50% | 0 | 0.00% | 1 | 1.80% | 0 | 0.00% | 26.21(.002) |
| up to 2 hours per month | 13 | 40.60% | 13 | 22.00% | 15 | 26.30% | 16 | 27.60% | ||
| up to 4 hours per month | 10 | 31.30% | 22 | 37.30% | 14 | 24.60% | 16 | 27.60% | ||
| more than 4 hours | 5 | 15.60% | 24 | 40.70% | 27 | 47.40% | 26 | 44.80% | ||
Table 3.
Differences between dentists’ educational characteristics in dentistry equipment and water quality practices.
Table 3.
Differences between dentists’ educational characteristics in dentistry equipment and water quality practices.
| Education abroad | Postgraduate education | Recognized specialty | ||||||||||||||
| No | Yes | No | Yes | No | Yes | |||||||||||
| N | % | N | % | χ2(p) | N | % | N | % | χ2(p) | N | % | N | % | χ2(p) | ||
| Has assistant | 83 | 49.40% | 14 | 36.80% | ns | 41 | 35.70% | 56 | 61.50% | 13.66(<.001) | 82 | 44.30% | 15 | 71.40% | 5.56(.018) | |
| Knows the active substance of antiseptic | 45 | 31.70% | 13 | 39.40% | ns | 25 | 25.50% | 33 | 42.90% | 5.86(.016) | 55 | 35.00% | 3 | 16.70% | ns | |
| Antiseptic to the handpieces (auto) | 15 | 9.90% | 2 | 6.70% | ns | 5 | 4.90% | 12 | 15.20% | 5.54(.019) | 15 | 9.20% | 2 | 11.10% | ns | |
| Antiseptic to the handpieces (manually) | 17 | 11.30% | 9 | 30.00% | 7.15(.008) | 18 | 17.60% | 8 | 10.10% | ns | 25 | 15.30% | 1 | 5.60% | ns | |
| SmallSuction | between two patients | 80 | 50.00% | 10 | 26.30% | 13.26(.021) | 44 | 40.70% | 46 | 51.10% | 13.04(.023) | 85 | 47.80% | 5 | 25.00% | ns |
| every few appointments | 25 | 15.60% | 5 | 13.20% | 13 | 12.00% | 17 | 18.90% | 28 | 15.70% | 2 | 10.00% | ||||
| per day | 36 | 22.50% | 17 | 44.70% | 38 | 35.20% | 15 | 16.70% | 45 | 25.30% | 8 | 40.00% | ||||
| per week or more | 19 | 11.80% | 6 | 15.8% | 13 | 12.00% | 12 | 13.40% | 20 | 11.20% | 5 | 25.00% | ||||
| Annual maintenance | 103 | 64.00% | 19 | 51.40% | ns | 58 | 53.20% | 64 | 71.90% | 7.24(.007) | 114 | 64.00% | 8 | 40.00% | 4.40(.036) | |
| Micromotors | 1 | 38 | 22.60% | 13 | 34.20% | ns | 34 | 29.60% | 17 | 18.70% | 12.72(.013) | 43 | 23.20% | 8 | 38.10% | ns |
| 2 | 55 | 32.70% | 14 | 36.80% | 41 | 35.70% | 28 | 30.80% | 63 | 34.10% | 6 | 28.60% | ||||
| 3 | 20 | 11.90% | 4 | 10.50% | 8 | 7.00% | 16 | 17.60% | 22 | 11.90% | 2 | 9.50% | ||||
| 4 | 22 | 13.10% | 3 | 7.90% | 17 | 14.80% | 8 | 8.80% | 24 | 13.00% | 1 | 4.80% | ||||
| 5+ | 33 | 19.60% | 4 | 10.50% | 15 | 13.00% | 22 | 24.20% | 33 | 17.80% | 4 | 19.00% | ||||
| Airotors | 1 | 21 | 12.50% | 8 | 21.10% | ns | 21 | 18.30% | 8 | 8.80% | 8.94(.063) | 20 | 10.80% | 9 | 42.90% | 22.76(<.001) |
| 2 | 49 | 29.20% | 14 | 36.80% | 36 | 31.30% | 27 | 29.70% | 54 | 29.20% | 9 | 42.90% | ||||
| 3 | 21 | 12.50% | 6 | 15.80% | 16 | 13.90% | 11 | 12.10% | 27 | 14.60% | 0 | 0.00% | ||||
| 4 | 21 | 12.50% | 4 | 10.50% | 16 | 13.90% | 9 | 9.90% | 25 | 13.50% | 0 | 0.00% | ||||
| 5+ | 56 | 33.30% | 6 | 15.80% | 26 | 22.60% | 36 | 39.60% | 59 | 31.90% | 3 | 14.30% | ||||
| Has amalgam trap | 106 | 65.80% | 22 | 59.50% | ns | 70 | 63.60% | 58 | 65.90% | ns | 121 | 68.00% | 7 | 35.00% | 8.56(.003) | |
| Has contract for amalgam removal | 42 | 27.30% | 9 | 23.70% | ns | 22 | 20.60% | 29 | 34.10% | 4.46(.035) | 48 | 28.10% | 3 | 14.30% | ns | |
| Environment friendly practices | A little | 26 | 17.20% | 2 | 6.50% | 10.93(.012) | 18 | 17.10% | 10 | 13.00% | ns | 28 | 17.10% | 0 | 0.00% | ns |
| Satisfactory | 73 | 48.30% | 12 | 38.70% | 48 | 45.70% | 37 | 48.10% | 76 | 46.30% | 9 | 50.00% | ||||
| Enough | 41 | 27.20% | 9 | 29.00% | 30 | 28.60% | 20 | 26.00% | 43 | 26.20% | 7 | 38.90% | ||||
| Very much | 11 | 7.30% | 8 | 25.80% | 9 | 8.60% | 10 | 13.00% | 17 | 10.40% | 2 | 11.10% | ||||
| Implementation of disinfection protocol is my responsibility | 99 | 58.90% | 21 | 55.30% | ns | 76 | 66.10% | 44 | 48.40% | 6.57(.010) | 111 | 60.00% | 9 | 42.90% | ns | |
Table 4.
Differences dental office characteristics in dentistry equipment and water quality practices.
Table 4.
Differences dental office characteristics in dentistry equipment and water quality practices.
| General dentistry | Clinic vs private practice | Family Income | ||||||||||||||||
| No | Yes | No | Yes | <25.000 euros | 25.001-50.000 euros | >50.000 euros | ||||||||||||
| N | % | N | % | χ2(p) | N | % | N | % | χ2(p) | N | % | N | % | N | % | χ2(p) | ||
| Equipment’s age | 0-5 years | 12 | 24.00% | 31 | 19.90% | ns | 30 | 19.90% | 13 | 23.60% | 16.12(.001) | 19 | 27.50% | 11 | 12.20% | 10 | 57.50% | ns |
| 6-10 years | 13 | 26.00% | 28 | 17.90% | 21 | 13.90% | 20 | 36.40% | 12 | 17.40% | 17 | 18.90% | 11 | 30.30% | ||||
| 11-20 years | 17 | 34.00% | 71 | 45.50% | 70 | 46.40% | 18 | 32.70% | 30 | 43.50% | 44 | 48.90% | 11 | 30.30% | ||||
| 21 and above | 8 | 16.00% | 26 | 16.70% | 30 | 19.90% | 4 | 7.30% | 8 | 11.60% | 18 | 20.00% | 7 | 15.20% | ||||
| Has assistant | 39 | 78.00% | 58 | 37.20% | 25.32(<.001) | 50 | 33.10% | 47 | 85.50% | 44.26(<.001) | 22 | 31.90% | 45 | 50.00% | 27 | 66.70% | 14.36(<.001) | |
| Performs microbiological test | 13 | 26.00% | 32 | 20.50% | ns | 33 | 21.90% | 12 | 21.80% | ns | 17 | 24.60% | 13 | 14.40% | 14 | 56.10% | 7.60(.022) | |
| Continuous water supply system to dental unit | 15 | 30.00% | 47 | 30.10% | ns | 41 | 27.20% | 21 | 38.20% | ns | 16 | 23.20% | 26 | 28.90% | 18 | 48.50% | 6.38(.041) | |
| Antiseptic to the handpieces (auto) | 6 | 13.60% | 11 | 8.00% | ns | 8 | 6.10% | 9 | 18.40% | 6.36(.012) | 8 | 14.00% | 3 | 3.80% | 6 | 16.10% | 6.21(.045) | |
| Antiseptic to the handpieces (manually) | 2 | 4.50% | 24 | 17.50% | 4.56(.033) | 19 | 14.40% | 7 | 14.30% | ns | 9 | 15.80% | 10 | 12.50% | 6 | 16.10% | ns | |
| Clean suction Large Small | between two patients | 21 | 45.70% | 69 | 45.40% | ns | 63 | 44.10% | 27 | 49.10% | ns | 27 | 40.30% | 39 | 46.40% | 0 | 45.50% | 23.24(.010) |
| every few appointments | 3 | 6.50% | 27 | 17.80% | 24 | 16.80% | 6 | 10.90% | 13 | 19.40% | 9 | 10.70% | 1 | 18.20% | ||||
| per day | 13 | 28.30% | 40 | 26.30% | 38 | 26.60% | 15 | 27.30% | 13 | 19.40% | 30 | 35.70% | 5 | 15.20% | ||||
| per week or more | 9 | 19.5% | 16 | 10.6% | 18 | 12.6% | 7 | 12.7% | 14 | 20.9% | 6 | 7.2% | 6 | 12.1% | ||||
| between two patients | 4 | 8.50% | 11 | 7.40% | 11.64(.040) | 8 | 5.60% | 7 | 13.00% | ns | 6 | 9.10% | 3 | 3.60% | 8 | 6.10% | ns | |
| every few appointments | 3 | 6.40% | 21 | 14.10% | 14 | 9.90% | 10 | 18.50% | 9 | 13.60% | 12 | 14.30% | 1 | 9.10% | ||||
| per day | 24 | 51.10% | 60 | 40.30% | 61 | 43.00% | 23 | 42.60% | 20 | 30.30% | 38 | 45.20% | 0 | 63.60% | ||||
| per week or more | 16 | 34.00% | 57 | 38.30% | 59 | 41.50% | 14 | 25.90% | 31 | 47.00% | 31 | 37.00% | 8 | 38.00% | ||||
| Micromotors | 1 | 9 | 18.00% | 42 | 26.90% | ns | 46 | 30.50% | 5 | 9.10% | 31.40(<.001) | 23 | 33.30% | 20 | 22.20% | 15 | 18.20% | 24.39(.002) |
| 2 | 19 | 38.00% | 50 | 32.10% | 58 | 38.40% | 11 | 20.00% | 20 | 29.00% | 39 | 43.30% | 3 | 24.20% | ||||
| 3 | 5 | 10.00% | 19 | 12.20% | 16 | 10.60% | 8 | 14.50% | 9 | 13.00% | 12 | 13.30% | 11 | 9.10% | ||||
| 4 | 4 | 8.00% | 21 | 13.50% | 15 | 9.90% | 10 | 18.20% | 8 | 11.60% | 8 | 8.90% | 4 | 15.20% | ||||
| 5+ | 13 | 26.00% | 24 | 15.40% | 16 | 10.60% | 21 | 38.20% | 9 | 13.00% | 11 | 12.20% | 0 | 33.30% | ||||
| Airotors | 1 | 10 | 20.00% | 19 | 12.20% | ns | 24 | 15.90% | 5 | 9.10% | 22.04(<.001) | 13 | 18.80% | 13 | 14.40% | 2 | 6.10% | Ns |
| 2 | 16 | 32.00% | 47 | 30.10% | 53 | 35.10% | 10 | 18.20% | 23 | 33.30% | 28 | 31.10% | 1 | 30.30% | ||||
| 3 | 6 | 12.00% | 21 | 13.50% | 23 | 15.20% | 4 | 7.30% | 9 | 13.00% | 15 | 16.70% | 14 | 3.00% | ||||
| 4 | 5 | 10.00% | 20 | 12.80% | 19 | 12.60% | 6 | 10.90% | 9 | 13.00% | 10 | 11.10% | 6 | 15.20% | ||||
| 5+ | 13 | 26.00% | 49 | 31.40% | 32 | 21.20% | 30 | 54.50% | 15 | 21.70% | 24 | 26.70% | 6 | 45.50% | ||||
| Has implantology motor | 17 | 34.70% | 60 | 38.50% | ns | 48 | 32.00% | 29 | 52.70% | 7.37(.007) | 28 | 41.20% | 28 | 31.10% | 0 | 45.50% | Ns | |
| Has amalgam trap | 25 | 52.10% | 103 | 68.70% | 4.38(.038) | 90 | 62.50% | 38 | 70.40% | ns | 46 | 71.90% | 54 | 61.40% | 38 | 62.50% | Ns | |
| Has contract for amalgam removal | 10 | 21.70% | 41 | 28.10% | ns | 32 | 22.70% | 19 | 37.30% | 4.07(.044) | 16 | 27.10% | 21 | 23.90% | 20 | 34.40% | Ns | |
| MoneySpent | <25€/month | 11 | 22.00% | 33 | 21.20% | 37 | 24.50% | 7 | 12.70% | 21 | 30.40% | 18 | 20.00% | 5 | 12.10% | |||
| 25-50€/month | 18 | 36.00% | 71 | 45.50% | 73 | 48.30% | 16 | 29.10% | 30 | 43.50% | 42 | 46.70% | 8 | 30.30% | ||||
| 50-75€/month | 9 | 18.00% | 29 | 18.60% | 24 | 15.90% | 14 | 25.50% | 10 | 14.50% | 14 | 15.60% | 3 | 36.40% | ||||
| >75€/month | 9 | 18.00% | 18 | 11.50% | 12 | 7.90% | 15 | 27.30% | 6 | 8.70% | 12 | 13.30% | 1 | 18.20% | ||||
| Implementation of disinfection protocol is my responsibility | 19 | 38.00% | 101 | 64.70% | 11.14(<.001) | 104 | 68.90% | 16 | 29.10% | 26.24(<.001) | 49 | 71.00% | 47 | 52.20% | 0 | 54.50% | 6.26(.044) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Copyright: This open access article is published under a Creative Commons CC BY 4.0 license, which permit the free download, distribution, and reuse, provided that the author and preprint are cited in any reuse.
Estimation and Factors Affecting Water Quality and Sustainability in the Private Dental Sector in Greece
Maria Antoniadou
et al.
,
2023
Green Dental Environmentalism among Students and Dentists in Greece
Maria Antoniadou
et al.
,
2023
MDPI Initiatives
Important Links
© 2024 MDPI (Basel, Switzerland) unless otherwise stated










