Preprint
Article
The making of Surgical Guides for TADs
Altmetrics
Downloads
245
Views
56
Comments
0
A peer-reviewed article of this preprint also exists.
This version is not peer-reviewed
Abstract
In the last 20 years, TADs have become one of the topics in orthodontic science, as it becomes one of the effective anchorages in moving teeth in a 3D movement to treat malocclusion and dental-alveolar orthopedic. Problems with the collusion of the roots of the teeth and trauma have hindered the use of these TADs; one of the solutions to keep TADs safe is a step-by-step innovation of procedure to make this anchorage concept using TAD safe. Making surgical guides for single-standing TADs is essential, and in practice, it is virtually possible with the advance of today's CAD/CAM and 3D printers. The content subject in the paper contains two parts: the consideration of why a surgical guide is necessary for the implantation of TADs and the making of the Surgical guide itself.
Keywords:
Submitted:
10 July 2023
Posted:
24 July 2023
You are already at the latest version
Alerts
A peer-reviewed article of this preprint also exists.
This version is not peer-reviewed
Submitted:
10 July 2023
Posted:
24 July 2023
You are already at the latest version
Alerts
Abstract
In the last 20 years, TADs have become one of the topics in orthodontic science, as it becomes one of the effective anchorages in moving teeth in a 3D movement to treat malocclusion and dental-alveolar orthopedic. Problems with the collusion of the roots of the teeth and trauma have hindered the use of these TADs; one of the solutions to keep TADs safe is a step-by-step innovation of procedure to make this anchorage concept using TAD safe. Making surgical guides for single-standing TADs is essential, and in practice, it is virtually possible with the advance of today's CAD/CAM and 3D printers. The content subject in the paper contains two parts: the consideration of why a surgical guide is necessary for the implantation of TADs and the making of the Surgical guide itself.
Keywords:
Subject: Medicine and Pharmacology - Dentistry and Oral Surgery
Introduction
Over the past two decades, temporary anchorage devices (TADs) have become important and essential armamentariums in orthodontic practice. TADS are now recognized as one of the most effective ways to conserve anchorage and move dental units in a 3D motion to treat malocclusion (1) Problems with the collusion of the roots during TADS placement and surgical trauma have hindered the use of these TADs. One of the solutions to the safe placement of TADS is to follow step-by-step procedures and use surgical guides, which is possible with technological innovations (2~12). A surgical guide for inserting single-standing TADs facilitates placement and is integral to safe clinical practice. Creating and making a surgical guide have become possible with the advanced application of CAD/CAM technology and the affordability of 3D printers. (13)
This paper covers two main topics: the importance of using a surgical guide for TAD implantation and the process of creating the guide.
There were numerous papers discussing the issue of TADs usage success and failures. One of the critical areas is the implantation itself, causing trauma to the tooth's root, and damaged periodontal membrane to a hole in the root tooth itself. Such unwanted complications happen, especially in inter-roots implantation (Park 2006). The average TADs diameter is between 1.4 to 1.8 mm, and often, the interdental bone may not be available to accommodate these dimensions (17,18,19).
The placement of TADS is required either in interdental bone or other safe anatomical sites of the maxilla and mandible. Several factors determine the safety and stability of TAD, a significant consideration being their accurate insertion in location and angulation without hindering the other anatomical structures, such as dental roots, before and during dental movements. By having complete control over the placement, an orthodontist can conduct orthodontic biomechanics in an organized and optimized manner, resulting in reduced treatment duration and the quality of treatment outcome.
According to studies, implants placed using the freehand method had significantly higher errors. The risk of positioning errors was as high as 88% when using the freehand method. At the same time, single-type, mucosa-supported guides had the lowest error rate of only 6%, even when other factors were considered. (20) It is a time for orthodontists to learn from the past when prosthodontists started using surgical guides for dental implants. (14,15,16). A surgical guide for TADs is intended to reduce orthodontist stress, while designing the procedure for practical use in daily orthodontic practice will benefit patients and the orthodontist practitioner.
The benefit for patients is less trauma and shorter surgical appointments. With a predictable and accurate placement position of TAD with a surgical guide, the post-insertion appliance can be prepared in the laboratory with joint consults before the surgical procedure. After the TAD insertion procedure, the post-insertion appliances, which are ready beforehand, are issued in the same appointment. This is also true with CAD/CAM metallic printed appliances. (21,22,23)
Doctors can benefit from using a surgical guide as it allows for the precise placement of TADS. The laboratory technician can perform a relatively clean procedure that involves making an appliance with ease.
The first and second parts of making the Surgical Guide for TADs.
Several steps and considerations in preparing the surgical guides need to be discussed; the different placement of TADs in their use and the variety of intended use of TADs should be understood, which is the purpose of the first part of this paper.
The second part is the procedure of making the Surgical Guide for TADs.
Part 1: Rationale for using a surgical guide in the implantation of TADs.
General consideration before using TADs as anchorage in moving teeth.
- The thickness of the mucosal layer in different areas of the mouth can affect implant selection of the implant/TAD’s length. When selecting a location for implantation, choosing an attached gingival site rather than a flabby mucosa is better. However, in some cases, implantation on a flabby mucosa cannot be avoided. Using a surgical guide makes locating the initial pilot hole made during the pre-drilling process easy. This saves time and effort in searching for the insertion point, as mucosa often covers it. For optimal results, it is recommended to utilize two surgical guides during the procedure: one for the pilot drill and another for the TAD. If you are considering placing TADs in the interdental bone between the roots of two teeth, it is imperative to have 0.5mm septal bone around TAD. This means that you will need at least 2.4 mm of the interdental bone to avoid damaging the roots, considering that TADs usually have a diameter of 1.4mm.
- Different TADs come in various head designs and sizes, so a surgical guide must be created to match the chosen TAD's dimensions. Laboratory technicians and clinicians must communicate to design an appropriate surgical guide. While the body of the TADs may be self-drilling, it's still recommended to use a pilot drill surgical guide to minimize any trauma to the soft tissue. This is particularly important for angulated insertion procedures to make it easier to enter the implantation site. The angle at which screws are inserted can vary depending on personal preference. Some people prefer an angle for stability, while others aim to avoid root collisions and position the screw tip apically. However, angled screw insertion is more challenging than straight insertion. A surgical guide can assist with accurate angulation insertion, and directional drilling requires a guide to prevent slipping. Designing the insertion process for easy handpiece and bur maneuvering during implantation is crucial.
- A surgical guide should have a stable position, usually using healthy teeth structure. Avoiding teeth that are compromised; therefore, periodontal health and mobility are avoided to stabilize the surgical guide.
- The force required to penetrate bone with TADs varies from 20N to 35N, depending on the diameter. Implantation typically occurs at a speed of 25Rpm, while drilling occurs at 800Rpm with water irrigation. It is better to have an immediate loading than waiting a few weeks, and it's better to load immediately rather than waiting for weeks and leaving it unloaded.
- It is mandatory to maintain sterilization and follow the aseptic procedure during the implantation process.
Although a surgical guide is an excellent support in the correct placement of the TAD, the clinician's experience is integral and crucial to the success of TAD placement.
The collecting data, planning, and designing in consideration in the making of the surgical guide:
The site, number, and type of TADS are influenced by the nature of malocclusion and the treatment plan. However, the site and design must consider the availability of quality and quantity of the bone at the proposed anatomical site. These are assessed with volumetric data of CBCT and other X-rays.
To determine the density of a bone, the Hounsfield value of the bone at the site should be evaluated. For spongy bone, the value should be around 300 HU, while cortical bone should be above 500 HU. For optimal results, it is recommended that the thickness of the cortical bone should be at least 0.5mm.
If the values are lower than these standards, it's best to check the surrounding sites. If the density is still unsuitable for implantation, another site of TAD placement should be explored until the minimum requirements are met.
Making a secure placement site will reduce failure risk and prevent reimplantation. The digital dental impression data obtained from the intra-oral scan in SLT format and DICOM data of CBCT are shared with the professional outsourced laboratory or in-house lab for processing.
The design of the surgical guide is created in the application software. This can be done by the dental technician and then checked by the doctor; therefore, communication is the key to success. Orthodontists should check the maneuverability to position the TADs toward the desired insertion location and preferred angulation. This is important because only the doctor knows the patient's situation, such as how far the patient can open her mouth and the instruments required to be used, keeping anatomical limitations in mind, especially implantation of the posterior region. Once the planning and design are done, the laboratory will do the 3D printing of the pilot drill and the guide of the specific screw. Each placement might have a different predrilling and implant size; therefore, the technician should fully know the intended TADs, their design, and size. So, two guides must be fabricated for accurate implantation. After the 3D printing, the technician will wash and cure these to finish the laboratory procedure. The surgical guides are then sent to the orthodontist's office.
The need to place the TADs for anchorage depends on the demand for specific treatment biomechanics. Generally, it is wise to avoid interdental space implantation whenever possible and choose places without or away from the tooth. This is relatively easy on the maxillary but has fewer anatomical choices available in the mandible.
- In the maxilla, use CBCT to look for the ideal places and the palatal sites in the T-zone, as described by Wilmes (26). The Benefit’s system is two screws being used to connect a plate to make it a sturdy anchorage for a 3D movement of the upper teeth. Therefore, the two screws’ placement is critical to insert the plate easily and quickly, such as paralleling or close to the parallel to provide easy fixation. The surgical guide will facilitate the parallel insertion of TADS. TADS are placed at the best bone density in the area intended to be the anchorage placement. The other option for the TADs site in the palatal bone is between the first molar and the second bicuspid area, and the first molar has only a single palatal root (two roots on buccal) and the second bicuspid's root, which may as well be single in some clinical situations. The placement on the buccal side can also be done with the surgical guide in the anterior teeth between the central and lateral teeth for the buccal area of interdental of the bicuspids and the buccal ridge underneath the Zygomatic process.
Figure 1.
A is the area of the T-Zone where usually plates with two screws are preferred rather than single-standing implantation. The reason is that the two screws will give more assurance to endure forces for en-mass movement of various 3-dimension movements in space. B is the area of choice where there is less interference of the swallowing and deglutition but still can do en-mass retraction of the whole teeth of the maxilla.
Figure 1.
A is the area of the T-Zone where usually plates with two screws are preferred rather than single-standing implantation. The reason is that the two screws will give more assurance to endure forces for en-mass movement of various 3-dimension movements in space. B is the area of choice where there is less interference of the swallowing and deglutition but still can do en-mass retraction of the whole teeth of the maxilla.

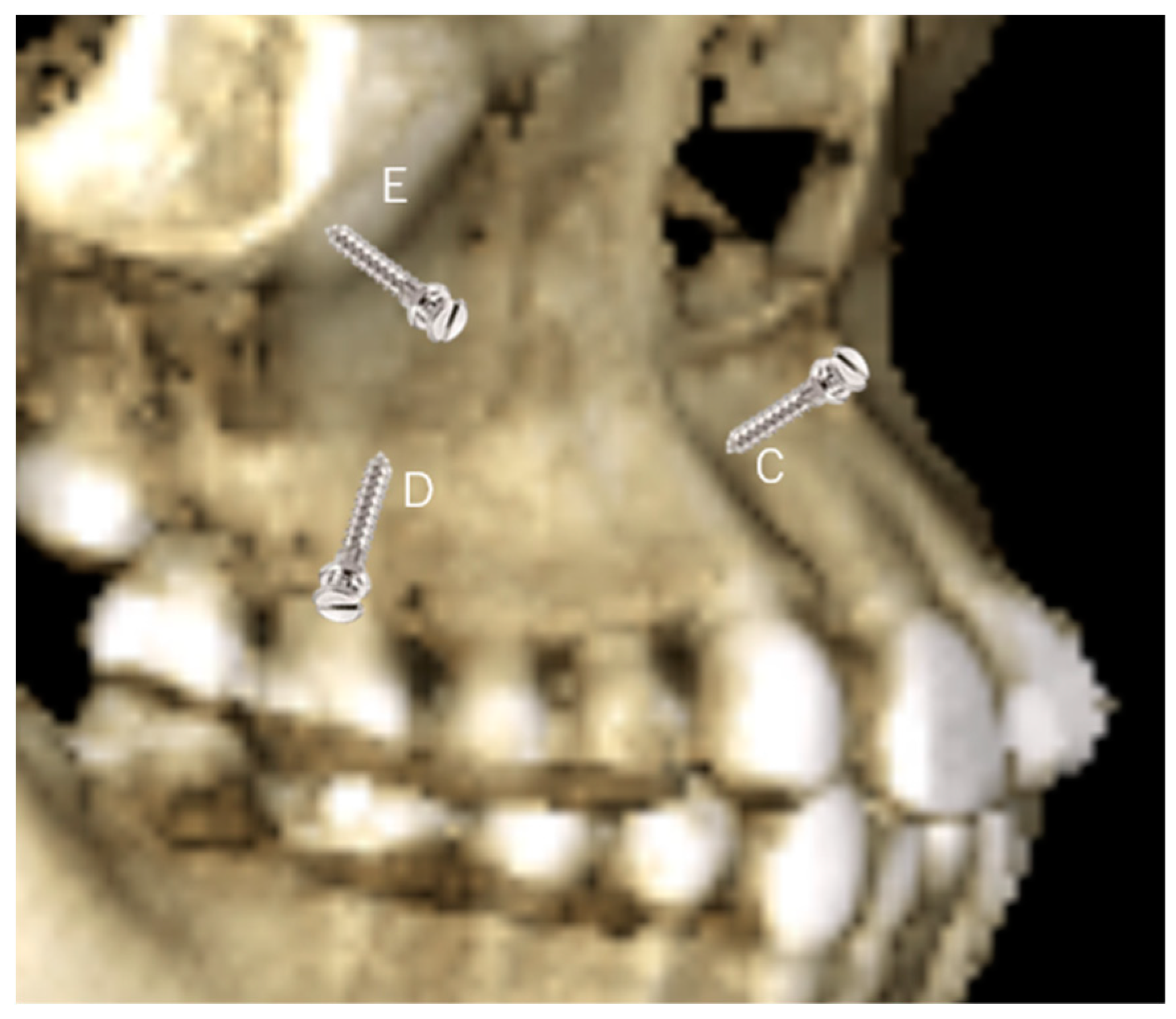
Figure 2.
C is a location between the lateral and canine to correct the Gummy Smile and the canted anterior occlusal plane. The location also benefits in correction underbite. D is interdental root placement, of the posterior buccal area, in most preferable use for single-standing TADs in retraction of the anterior teeth, especially in bicuspids extraction cases. E is at the lower part of the zygomatic bone and is a preference to retract the whole teeth without interference with the root of the maxilla. Precautions should be taken to avoid irritating the flabby mucosa and buccal papilla.
Figure 2.
C is a location between the lateral and canine to correct the Gummy Smile and the canted anterior occlusal plane. The location also benefits in correction underbite. D is interdental root placement, of the posterior buccal area, in most preferable use for single-standing TADs in retraction of the anterior teeth, especially in bicuspids extraction cases. E is at the lower part of the zygomatic bone and is a preference to retract the whole teeth without interference with the root of the maxilla. Precautions should be taken to avoid irritating the flabby mucosa and buccal papilla.
- 2.
- In the mandible, TADs placement on the lingual side in the mandibular arch will be challenging, except there are torus lingualis that are large enough to provide TADs implantation; therefore, the buccal region is the only choice. The anterior part of the dental arch will have limited interdental bone availability, and the quality of bone is often questionable. A critical evaluation of available bone width is necessary before the implantation. Interdental space can be more suitable by appropriately placing the brackets to flare the crowded roots. Changing angulation of the roots beforehand is a common practice in placing TADs in the anterior region.
- 3.
- The implantation in the interdental bone will limit the movement of the tooth, mesial and distally. Therefore, to avoid interferences with roots, the TADs are preferred on the mandible's ridge or the mandible's oblique line (Figure 3, H), especially when en-mass retraction of the arch is desirable. The ridge of the mandible between the body and the ramus of the mandible is a favorable site for TAD placement. The tricky part is that the mandible ridge may seem insignificant in women relative to men, and modification may be needed in the surgical guide’s design. Since the placement location is a steep bone wall, manual placement will be challenging, so a surgical guide is preferred. The angulated placement of the TADs in this area and the flabby mucosa also necessitates using the surgical guide. Care must be taken during the intraoral scan as the superficial mucous membrane above the ridge must be gently stretched to record this critical area. Lacking recorded data in this area will affect the visibility of the area site, and the surgical guide cannot be planned. Implantation in this area is recommended using contra-angle motorized instruments, as the buccal cheek tissue prevents using a hand screwdriver and will obstruct the surgeon's vision. The buccal musculature, maxillary teeth, and mouth opening will limit the maneuverability of the implantation procedure. These limitations should be evaluated during a clinical examination. Considering the hindrance in lower lip movements, the placement between the four incisors should be avoided as much as possible. TADS in this area can cause painful lip ulcerations with delayed healing. The location of the canine and the first bicuspid (Figure 3, F) is an area that can fit in the implantation choice. This location is between anterior and posterior dental arch segments and thus will provide an excellent place to resolve both anterior and posterior malocclusion. Depending on the extraction case or non-extraction case, considerations can be different, and placement in the extraction site of the bicuspid and adjacent area is required to avoid proximity to vital structures in the mentalis foramen. In Figure 3, G location is possible when there is a need to retract the anterior teeth after an extraction case when implantation of the ridge of the mandible is difficult or impossible due to the younger age of the patient. However, implantation at a young age, e.g., under 12, is risky as bone metabolism is still high in this area.
The clinical application of TADs using the surgical guide, an example case.
One of the problems faced in constructing surgical guides is the location of the mandible's angle on the mandible's oblique ridge. First, the flabby mucosa and second, the insertion angulation should be planned so that a contra-angle handpiece can be used easily. The first problem is holding the mucosa during the implantation, especially when making the pilot hole; the surgical guide will manage to put light pressure so that the mucosa will result in being caught and injured by the drilling process. The second problem is that we must calculate the length of the screw of the TADs, the thickness of the head of the contra-angle, and the size of the surgical guide beforehand to ensure such an implantation is possible.
Figure 4, 5, 6.
he implantation with a surgical guide of the oblique ridge of the mandible photograph of the intra-oral, lateral, and occlusal view of the X-rays CBCT.
Figure 4, 5, 6.
he implantation with a surgical guide of the oblique ridge of the mandible photograph of the intra-oral, lateral, and occlusal view of the X-rays CBCT.

Figure 7.
The surgical guide upon the model to check the position of the surgical guide upon insertion inside the mouth. The left side is the surgical guide for the TADs, and the right is the surgical guide for the pilot drill.
Figure 7.
The surgical guide upon the model to check the position of the surgical guide upon insertion inside the mouth. The left side is the surgical guide for the TADs, and the right is the surgical guide for the pilot drill.
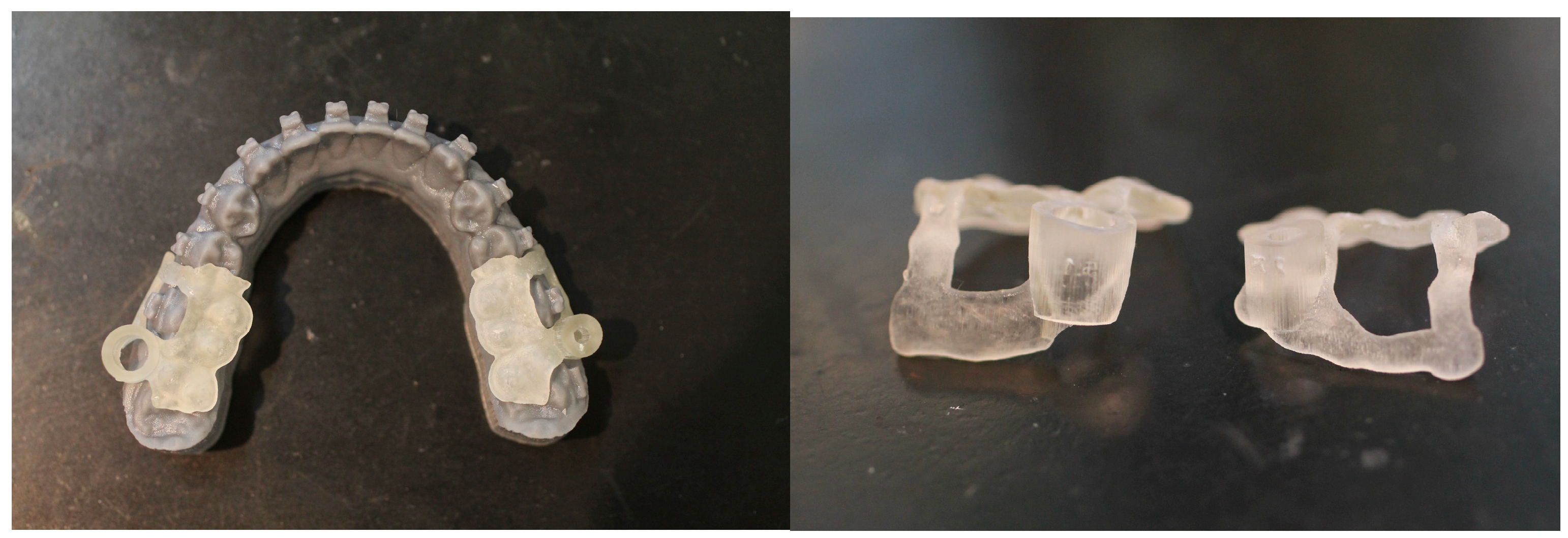
Figure 8.
The surgical guide is viewed from the side; the vertical height is the most critical part, as it should be adjusted whenever a problem arises before implantation.
Figure 8.
The surgical guide is viewed from the side; the vertical height is the most critical part, as it should be adjusted whenever a problem arises before implantation.

CBCT is also taken immediately after the surgical procedure to ensure the implantation result. A clinical error can happen in the collection of data used for the devise planning, also even when it was made correctly, the anatomical situation, such as the posterior region of the oblique ridge of the mandible where the patient cannot open his/her mouth as wide as expected. The contra-angle cannot be used for the intended angulation, and we must reconsider an alternate implantation site. The thickness of the surgical guide and the thickness of materials and sleeves on the guide is also limited. The clinician should understand those limitations. A surgical guide may need final adjustments in the mouth by selective trimming. The surgical guide must be positioned correctly in the mouth, and its location and accuracy must be double-checked before surgery. The collaboration between the laboratory technician and the clinician is necessary to make an excellent surgical guide.
Despite the advantages of using advanced technology, proper planning and sound clinical judgment of the clinician is essential to successful TADs implantation.
Part two: The procedure of making the Surgical Guide for TADs.
Integrating CAD/CAM technology in dental laboratories has also helped orthodontics. CAD CAM was introduced in dental prosthodontics, and in 1985 the first commercial system was introduced in the market by Mormann (29), who gave the name CEREC to that system, and has been developed since then. Integration of digital and CAD technology in orthodontics in doing diagnosis, treatment plan, and time scheduling of cases was first described by Impellizzeri et al. (30). In orthodontics, extensive use of digital technology, CAM and 3D printing in clear aligner therapy (31), lingual bracket system (32), and the position of TADs. (33,34,35,36,37,38)
Now the new development of TADs uses and placement and development of software call for reevaluating the technique to provide an update on the ability to various anatomical areas and give safe clinical work for orthodontists. orthodontists can safely place temporary anchorage devices (TADS) in various anatomical areas to improve treatment capabilities for complex malocclusion. This is due to advancements in scanning technology, software capabilities, and 3D volumetric analysis of implant sites, which have enhanced clinical abilities and resulted in better outcomes.
The Surgical Guide Technique for TADs Placement
The use of TADs in orthodontics has notably increased in recent years. The TADs have allowed for the simplification of several treatment plans by producing skeletal anchorage. Since these are easy to place and remove and require no cooperation from the patient, there has been an increased use of these devices in orthodontic practices. However, TADs’ stability heavily relies on bone thickness both on a vestibular and palatal level. The critical concern is that TADs are also difficult to place correctly, and there is a risk of dental damage, sinus or nasal perforation, chronic sinus inflammation, and even anchorage loss (39). Orthodontics has seen a rise in the use of TADs in recent years due to their ability to simplify treatment plans by providing skeletal anchorage. TADs are easy to install and remove and do not require patient cooperation. However, the stability of TADs depends on factors such as bone quality and quantity, as well as biological, technique-related, and clinical variables. It is important to note that TADs are challenging to implant accurately, and there is a risk of dental damage, sinus or nasal perforation, chronic sinus inflammation, and complete failure (40).
By overlaying CBCT and digital models obtained from an intraoral scan, it becomes feasible to identify the optimal position for TADs. Once the ideal location has been determined, a surgical guide can be produced using a 3D printer. These guides ensure accurate and safe placement, reducing the risk of complications typically associated with the procedure.
Sequences of digital workflow to make surgical guides.
- We used an intra-oral scan for the SLT and a CBCT X-ray machine for the DICOM data to obtain a digital impression. afterward, we superimposed the STL and DICOM data using a commercialized application.
- The 3-Shape software completes the process of designing a surgical guide. By utilizing software, the diameter of the drilling bur and screw holder can be determined, ensuring no contact with the roots during the procedure. The 3-shape software simulates the screw placement within the bone's anatomic area. This simulation helps determine the tube design required for drilling and screw implantation.
- Easy to print in a 3-D printer.
- Cleaning, washing, drying, and cutting of the supporting pillars, followed by post-curing.
- Checking and testing the surgical guide of both the drilling guide and screw holder guide is then placed upon the model of the jaw to check its fitness. When there are brackets, holes can be made to avoid retentions.
Digital TAD Guide production process
Following is the procedure with the help of an outside laboratory team of dental technicians. The application’s name software will be introduced, but another commercial brand can also be used. It was necessary to reveal the name of the products to make it easy to understand that practicing clinicians will find it difficult to follow the instructions. Our laboratories use intraoral scan data as follows:
1. For dentition, STL and CBCT (DICOM) data are superimposed using 3-Matic (Materialize, Leuven, Belgium). 3-Matic application has been used to evaluate the Three-dimensional root monitoring of root movement during orthodontic treatment by Lee et al. (41) without exposing radiation in controlling the position of the roots.
2. The designing and planning
a. Use Mimics (Materialize, Leuven, Belgium) to extract the roots of the mesiodistal teeth where the anchor screws are to be implanted and converted into 3D as Figure 2. The method has been described by Cassetta using a 3D surgical plate for corticotomy (42).
Figure 9.

b. The necessity to make three-dimensional images and analyze by using the Geomagic Studio 5 software (Raindrop Geomagic, Inc, Morrisville, NC). Create cylinder data of the same size (φ1.6 x 8.0mm) imitating the screw (product of TADs, brand OSAS by DEWIMED) to be planted as Figure 10.
c. Load the CBCT, intraoral scanner, and cylinder data into Mimics and perform an implantation simulation shown on Figure 11.
d. At this stage, the Orthodontist performs the simulation to the best bone quality that will guarantee the success of the implantation. The process below shows the simulation by the doctors. The soft tissue thickness will also dictate the length of the TADs used (Figure 12).
e. The plan was sent back to the laboratory, and the technician then confirmed whether the simulation was visible for the 3D surgical guide printing.
Figure 13.

f. The Appliance Designer of 3Shape, Copenhagen, Denmark, was used to simulate the drill and the surgical guide to easy and straightforward the TADs implantation position as below.
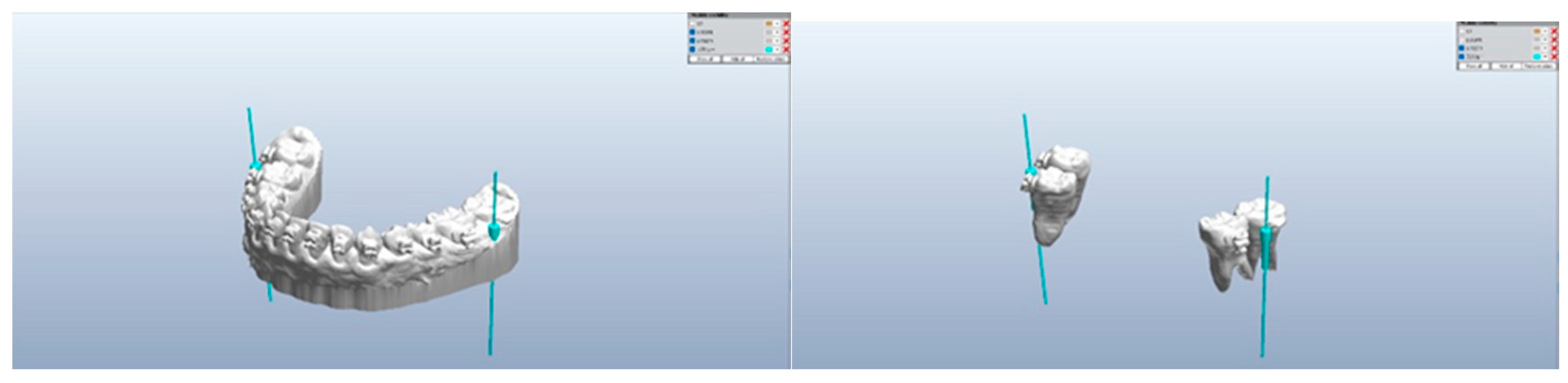
Figure 14 and 15.
The left and right side is the exact figure, and the right side is where the lower mandible was removed to show only the screws.
Figure 14 and 15.
The left and right side is the exact figure, and the right side is where the lower mandible was removed to show only the screws.
g. After the screw length and position were observed, the outer guide for both the drilling screw and the screw guide was constructed. The occlusal surface is being used for the guide to position the surgical guide. all brackets should be avoided by making a hole to make smooth repositioning. It the important to check the mucosa below the drilling guide, which should fit or light pressure without scarifying the fitness of the guide, to hold the mucosa when doing the initial drilling.
Figure 16.
The predrilling surgical guidance, and 17. The surgical screw guidance.

2. Printing
a. Print the designed data using a 3D printing machine for both the pre-drill guide and TADs screw guide. The 3D printer is a SprintRay Pro95: (SprintRay, LA, US) with the material also of SprintRay Sugical Guide3 (SprintRay, LA, US).
Figures 17, 18 and 19.

The use of Dashboard 2.0 software will help to monitor the printing process flow. The Dashborad 2.0 is also being used to communicate between designers and doctors and save the design in storage. After Printing, we need to wash and dry as there is residual that is not fully cured resin. The wash and cleaning of the pre-drill guide and TADs screw guide with ProWash/Dry (SprintRay, LA, US) to remove excess material and dry (Figure 20).
b. After cleaning/drying, remove the support (Figures 21 and 22), and the guides are ready to Post cure, process as some part is not cured. The Pro Cure (SprintRay, LA, US) makes the guide’s final cure.
Figure 20, 21 and 22.

Figures 23, 24 and 25.

c. Make the model from the STL to check the fitness of each guide to the model, paying attention to the area of the brackets to avoid any retention. In the bracket areas, make a window that also will benefit checking fitness during the implantation.
Figures 26 and 27.

The surgical guide for both the predrilling and the screw implantation guides are ready to be used. An additional window can be made to check the guide’s accuracy in clinical procedures.
Conclusion
3D printing is revolutionizing the dental and orthodontic practice. Surgical guide-making can be made easily and help orthodontists safely implant the TADs with complete placement control. The exact placement of TADs will provide the ability to produce the force of applications needed for the treatment. When using surgical guides, it is essential to stress the necessity of a Pilot Drill Guide, as it guides the first drilling step when clinicians want an accurate entry point. The pilot guide increases the predictability of implantation surgery and can be used to treat partially edentulous orthodontic patients. The surgical guide will give an accurate implant placement after the pilot drill, particularly for achieving the correct angulation of implants in a place like the oblique line of the mandible.
The benefits of using a surgical guide include hassle-free procedures minimizing stresses on practitioners, and better patient cooperation and comfort. The implantation is predictable, precise, and efficient in time. A surgical guide replicates the exact surfaces of the patient's intraoral setting and assists the surgeon in drilling implants into the bone with optimal accuracy.
The step-by-step procedure for making the surgical guide has been explained, as the new development of 3D printing has made it possible to make pre-drilling and surgical guides possible for daily orthodontic office needs for safe and comfortable implantation. If the surgical implantation procedure must be done between orthodontic and tooth movement, it should be less stressful and accurate. The recommended procedure is a good option in terms of time and effort, as the demand for TADs has been increasing recently. Good communication between laboratory technicians and the orthodontist plays a significant role in implantation success using surgical guidance. Surgical guidance for TADs is an integral part of clinical orthodontics.
References
- 1. Mah J, Bergstrand F. Temporary anchorage devices: a status report. J Clin Orthod. 2005 Mar;39(3):132-6; discussion 136; quiz 153. PMID: 15888950.
- Bearn DR, Alharbi F. British Orthodontic Society national audit of temporary anchorage devices (T.A.D.s): report of the first thousand T.A.D.s placed. J Orthod. 2015 Sep;42(3):214-9. [CrossRef]
- Ahmed V KS, Rooban T, Krishnaswamy NR, Mani K, Kalladka G. Root damage and repair in patients with temporary skeletal anchorage devices. Am J Orthod Dentofacial Orthop. 2012 May;141(5):547-55. doi: 10.1016/j.ajodo.2011.11.014. [CrossRef]
- Çelik Güler Ö, Malkoç S. Effects of orthodontic force on root surface damage caused by contact with temporary anchorage devices and on the repair process. Korean J Orthod. 2019 Mar;49(2):106-115. doi: 10.4041/kjod.2019.49.2.106. Epub 2019 Mar 19. [CrossRef]
- Marc Schätzle, Roland Männchen, Marcel Zwahlen, Niklaus P. Lang Survival and failure rates of orthodontic temporary anchorage devices: a systematic review Clinical Oral Implants Research 09 November 2009 Wiley. [CrossRef]
- Yi-Jane Chen, Hao-Hueng Chang, Hsing-Yi Lin, Eddie Hsian-Hua Lai, Hsin-Chia Hung, Chung-Chen Jane Yao Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices 16 October 2008. [CrossRef]
- Manuel Nienkemper, Björn Ludwig, Risk of root damage after using lateral cephalogram and intraoral scan for guided insertion of palatal miniscrews, Head & Face Medicine, 10.1186/s13005-022-00335-0, 18, 1, (2022). [CrossRef]
- Elena Riad Deglow, Miriam O′Connor Esteban, Álvaro Zubizarreta-Macho, Sofĺa Hernández Montero, Georgia Tzironi, Francesc Abella Sans, Alberto Albaladejo Martínez, Novel digital technique to analyze the accuracy and intraoperative complications of orthodontic self-tapping and self-drilling microscrews placement techniques: An in vitro study, American Journal of Orthodontics and Dentofacial Orthopedics, 10.1016/j.ajodo.2021.03.020, 162, 2, (201-207), (2022). [CrossRef]
- Sarah Abu Arqub, Vaibhav Gandhi, Shivam Mehta, Ledjo Palo, Madhur Upadhyay, Sumit Yadav, Survival estimates and risk factors for failure of palatal and buccal mini-implants, The Angle Orthodontist, 10.2319/090720-777.1, 91, 6, (756-763), (2021). [CrossRef]
- Amin Golshah, Kimia Gorji, Nafiseh Nikkerdar, Effect of miniscrew insertion angle in the maxillary buccal plate on its clinical survival: a randomized clinical trial, Progress in Orthodontics, 10.1186/s40510-021-00370-8, 22, 1, (2021). [CrossRef]
- Amin Golshah, Mahya Salahshour, Nafiseh Nikkerdar, Interradicular distance and alveolar bone thickness for miniscrew insertion: a CBCT study of Persian adults with different sagittal skeletal patterns, B.M.C. Oral Health, 10.1186/s12903-021-01891-8, 21, 1, (2021). [CrossRef]
- Diana Milena Ramírez-Ossa, Natalia Escobar-Correa, Maria Antonia Ramírez-Bustamante, Andrés A. Agudelo-Suárez, An Umbrella Review Of The Effectiveness Of Temporary Anchorage Devices And The Factors That Contribute To Their Success Or Failure, Journal of Evidence Based Dental Practice, 10.1016/j.jebdp.2020.101402, (101402), (2020). [CrossRef]
- Barbara Kirnbauer, Petra Rugani, Elisabeth Santigli, Philipp Tepesch, Kamran Ali, Norbert Jakse, Fully guided placement of orthodontic miniscrews— a technical report, Australasian Orthodontic Journal, 10.21307/aoj-2020-035, 35, 1, (71-74), (2021). [CrossRef]
- Vercruyssen M, Laleman I, Jacobs R, Quirynen M. Computer-supported implant planning and guided surgery: a narrative review. Clin. Oral Impl. Res. 26 (Suppl. 11), 2015, 69–76. [CrossRef]
- Hämmerle CHF, Cordaro L, van Assche N, Benic GI, Bornstein M, Gamper F, Gotfredsen K, Harris D, Hürzeler M, Jacobs R,Kapos T, Kohal RJ, Patzelt S.B.M., Sailer I, Tahmaseb A, Vercruyssen M, Wismeijer D. Digital technologies to support planning, treatment, and fabrication processes and outcome assessments in implant dentistry. Summary and consensus statements. The 4th E.A.O. consensus conference 2015. Clin. Oral Impl. Res. 26 (s11), 2015, 97–101. [CrossRef]
- Apostolakis, D., Kourakis, G. CAD/CAM implant surgical guides: maximum errors in implant positioning attributable to the properties of the metal sleeve/osteotomy drill combination. Int J Implant Dent 4, 34 (2018). [CrossRef]
- Park HS, Lee YJ, Jeong SH, Kwon TG. Bone density of the alveolar and basal bone in the maxilla and the mandible. Am J Orthod Dentofacial Orthop. 2006. [CrossRef]
- Cho WH. Influence of the operator's experience and drilling sites on the root contact during drilling for micro-implants insertion [thesis]. Daegu, Korea: Kyungpook University; 2005.
- Kuroda S, Yamada K, Deguchi T, Hashimoto T, Kyung H-M, Takano-Yamamoto T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006. [CrossRef]
- Arisan V, Karabuda CZ, Mumcu E, Özdemir T. Implant positioning errors in freehand and computer-aided placement methods: a single-blind clinical comparative study. Int J Oral Maxillofac Implants. 2013 Jan-Feb;28(1):190-204. PMID: 23377066. [CrossRef]
- Willmann, B. Wilmes, D. Drescher, Düsseldorf, Digitale Mini-Implantat getragene Suprakonstruktionen – Design und Workflows J. Compr. Dentof. Orthod. + Orthop. (COO) Umf. Dentof. Orthod. u. Kieferorthop. (UOO) No. 3-4 / 2019 (c).
- Willmann, B. Wilmes, D. Drescher, Clinical use of digital Workflow Exemplified by Mini Implant. Inf. Orthod Kieferorthop 2020; 52: 121-127.
- S. Graf, S. Vasudavan, B. Wilmes CAD/CAM Metallic Printing of a Skeletally Anchored Upper Molar Distalizer JCO/2020, 140-149.
- Petrey JS, Saunders MM, Kluemper GT, Cunningham LL, Beeman CS. Temporary anchorage device insertion variables: effects on retention. Angle Orthod. 2010 Jul;80(4):446-53. doi: 10.2319/070309-376.1. PMID: 20482347; PMCID: PMC8966450. [CrossRef]
- Yan Chen, Ji-Wan Lee, Woo-Hyung Cho, Hee-Moon Kyung Potential of self-drilling orthodontic microimplants under immediate loading. AJO-DO Vol. 137Issue 4p496–502 2010. [CrossRef]
- Wilmes B, Ludwig B, Vasudavan S, Nienkemper M, Drescher D. The T-Zone: Median vs. Paramedian Insertion of Palatal Mini-Implants. J Clin Orthod. 2016 Sep;50(9):543-551. PMID: 27809213Özer AlkanYeşim Kaya The thickness of posterior buccal attached gingiva at common miniscrew insertion sites in subjects with different facial types. AJO-DO Vol. 156Issue 6p800–807, 2019. [CrossRef]
- Ka Fai Andy WongYifan Lin. Thickness of buccal attached gingiva at miniscrew insertion sites Vol. 158Issue 2p160–161 Published online: 2020. [CrossRef]
- Chen YJ, Chang HH, Lin HY, Lai EH, Hung HC, Yao CC. Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices. Clin Oral Implants Res. 2008 Nov;19(11):1188-96. PMID: 18983323. [CrossRef]
- Mormann WH, Brandestini M, Lutz F, Barbakow F.Chairside Computer Aided Direct Ceramic Inlays. Quintessence Int 1989;20:329-339.
- Impellizzeri, A.; Horodynski, M.; De Stefano, A.; Palaia, G.; Polimeni, A.; Romeo, U.; Guercio-Monaco, E.; Galluccio, G. CBCT and Intra-Oral Scanner: The Advantages of 3D Technologies in Orthodontic Treatment. Int. J. Environ. Res. Public Healthy 2020, 17, 9428. [CrossRef]
- Aristides BM. Advances in digital technology and orthodontics: A reference to the invisalign method.Med Sci Monit 2005;11:139-142.
- Wiechmann D, Rummel V, Thalheim A, Simon JS, Wiechmann L.Customized Brackets And Arch wires For Lingual Orthodontic Treatment.Am J Orthod Dentofac Orthop 2003;124:593-599. [CrossRef]
- Liu H, Liu D, Wang G, Wang C, Zhao Z.Accuracy of surgical positioning of orthodontic mini screws with a computer-aided design and manufacturing template. Am JOrthod Dentofac Orthop 2010;137:728e1-28e10. [CrossRef]
- Bae MJ, Kim JY, Park JT, Cha JY, Kim HJ, Yu HS, Hwang CJ. Accuracy of miniscrew surgical guides assessed from cone-beam computed tomography and digital models. Am J Orthod Dentofac Orthop. 2013;143(6):893–901. [CrossRef]
- Möhlhenrich SC, Brandt M, Kniha K, Prescher A, Hölzle F, Modabber A, Wolf M, Peters F. Accuracy of orthodontic mini-implants placed at the anterior palate by tooth-borne or gingiva-borne guide support: a cadaveric study. Clin Oral Investig. 2019;23(12):4425–31. [CrossRef]
- Cassetta M, Giansanti M. Accelerating orthodontic tooth movement: a new, minimally-invasive corticotomy technique using a 3D-printed surgical template. Med Oral Patol Oral Cir Bucal. 2016;21(4):e483–7. [CrossRef]
- Cassetta M, Altieri F, Di Giorgio R, Barbato E. Palatal orthodontic miniscrew insertion using a CAD-CAM surgical guide: description of a technique. Int J Oral Maxillofac Surg. 2018;47(9):1195–8. [CrossRef]
- Iodice G, Nanda R, Drago S, Repetto L, Tonoli G, Silvestrini-Biavati A, Migliorati M. Accuracy of direct insertion of TADs in the anterior palate with respect to a 3D-assisted digital insertion virtual planning. Orthod Craniofac Res. 2022;25(2):192–8. [CrossRef]
- Möhlhenrich, S.C.; Brandt, M.; Kniha, K.; Bock, A.; Prescher, A.; Hölzle, F.; dabber, A.; Danesh, G. Suitability of virtual plaster models superimposed with the lateral cephalogram for guided paramedian orthodontic mini-implant placement with regard to the bone support. J. Orofac. Orthop. Fortschr. Der Kieferorthopädie 2020, 81, 340–349. [CrossRef]
- Davidowitz G, Kotick PG. (2011), "The use of CAD/CAM in dentistry.", Dent Clin North Am, 55 (3): 559–570, doi:10.1016/j.cden.2011.02.011, PMID 21726690. [CrossRef]
- Lee, R.J.; Weissheimer, A.; Pham, J.; Go, L.; Menezes, L.; Redmond, W.R.; Loos, J.F.; Sameshima, G.T.; Tong, H. Three-dimensional monitoring of root movement during orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 132–142. [CrossRef]
- Cassetta M, Giansanti M. Accelerating orthodontic tooth movement: A new, minimally-invasive corticotomy technique using a 3D-printed surgical template. Med Oral Patol Oral Cir Bucal. 2016 Jul 1;21(4):e483-7. PMID: 27031067; PMCID: PMC4920463. [CrossRef]
Figure 3.

Figure 10.

Figure 11.

Figure 12.
shows the TADs only when the hard and soft tissue is removed, so the final check is easy. The lower right side figure shows the intended situation.
Figure 12.
shows the TADs only when the hard and soft tissue is removed, so the final check is easy. The lower right side figure shows the intended situation.

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Copyright: This open access article is published under a Creative Commons CC BY 4.0 license, which permit the free download, distribution, and reuse, provided that the author and preprint are cited in any reuse.
The making of Surgical Guides for TADs
Michiko Aonuma
et al.
,
2023
The Surgical Guides for TADs: The Rational and Laboratory Procedures
Aonuma Michiko
et al.
,
2023
MDPI Initiatives
Important Links
© 2024 MDPI (Basel, Switzerland) unless otherwise stated







