NCP
NCP
Uploaded by
Camille PinedaCopyright:
Available Formats
NCP
NCP
Uploaded by
Camille PinedaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
NCP
NCP
Uploaded by
Camille PinedaCopyright:
Available Formats
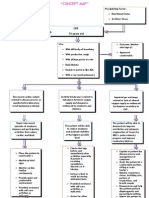
Decreased Cardiac Output The heat fails to pump enough blood to meet the metabolic needs of the body.
The blood flow that supplies the heart is also decreased thus decrease in cardiac output occurs, blood then is insufficient and making it difficult to circulate the blood to all parts of the body thus may cause altered heart rate and rhythm, weakness and paleness NDx: Decreased cardiac output r/t altered heart rate and rhythm AEB bradycardia Assessment Subjective: (none)Objectives:The patient manifested the following:
Planning Nursing Interventions Short 1. Assess for Term:After 3abnormal 4 hours of heart and lung nursing sounds. interventions, 2. Monitor blood the patient pressure and with pale pulse. conjunctiva, will 3. Assess mental nail beds and participate in status and buccal mucosa activities that reduce the level of irregular workload of consciousness. rhythm of the 4. Assess pulse heart.Long patients skin bradycardic temperature pulse rate of 34 Term:After 23 days of and peripheral beats/min nursing pulses. generalized interventions, 5. Monitor weakness the patient results of will be able to laboratory and display diagnostic hemodynamic tests. stability. 6. Monitor oxygen saturation and ABGs. 7. Give oxygen as indicated by patient symptoms, oxygen saturation and ABGs. 8. Implement strategies to treat fluid and electrolyte
Rationale Evaluation 1. Allows Short detection of Term:After left-sided nursing heart failure interventions, that may the patient occur with shall have chronic renal participated in failure activities that patients due reduce the to fluid workload of volume the excess as the heart.Long diseased Term:After 2kidneys are 3 days of unable to nursing excrete water. interventions, 2. Patients with the patient renal failure shall have are most been able to often display hypertensive, hemodynamic which is sta attributable to excess fluid and the initiation of the renninangiotensin mechanism. 3. The accumulation of waste products in the bloodstream impairs
imbalances. 9. Administer cardiac glycoside agents, as ordered, for signs of left sided failure, and monitor for toxicity. 10. Encourage periods of rest and assist with all activities. 11. Assist the patient in assuming a high Fowlers position. 12. Teach patient the pathophysiolo gy of disease, medications 13. Reposition patient every 2 hours 14. Instruct patient to get adequate bed rest and sleep 15. Instruct the SO not to leave the client unattended
oxygen transport and intake by cerebral tissues, which may manifest itself as confusion, lethargy, and altered consciousness . 4. Decreased perfusion and oxygenation of tissues secondary to anemia and pump ineffectivenes s may lead to decreased in temperature and peripheral pulses that are diminished and difficult to palpate. 5. Results of the test provide clues to the status of the disease and response to treatments. 6. Provides information regarding the hearts ability to perfuse distal tissues with oxygenated blood
7. Makes more oxygen available for gas exchange, assisting to alleviate signs of hypoxia and subsequent activity intolerance. 8. Decreases the risk for development of cardiac output due to imbalances. 9. Digitalis has a positive isotropic effect on the myocardium that strengthens contractility, thus improving cardiac output. 10. Reduces cardiac workload and minimizes myocardial oxygen consumption. 11. Allows for better chest expansion, thereby improving pulmonary capacity. 12. Provides the patient with needed
information for management of disease and for compliance. 13. To prevent occurrence of bed sores 14. To promote relaxation to the body 15. To ensure safety and reduce risk for falls that may lead to injury
Excess Fluid Volume When blood flow through the renal artery is decreased, the baroreceptor reflex is stimulated and rennin is released into the bloodstream. Renin interacts with angiotensinogen to produce angiotensin I. When angiotensin I contacts ACE, it is converted to angiotensin II, a potent vasoconstrictor. Angiotensin II increases arterial vasoconstriction, promote release of norepinephrine from sympathetic nerve endings, and stimulates the adrenal medulla to secrete aldosterone, which enhances sodium and water absorption. Stimulation of the rennin-angiotensin system causes plasma volume to expand and preload to increase. NDx: Excessive Fluid volume r/t decreased cardiac output and sodium and water retention AEB crackles on both lung field and edema on extremities secondary to CHF and IHD Assessment Planning Subjective:(none)Objective:P Short atient manifested: Term:After 3-4 hours Edema on extremities of intervention DOB s, the Crackles heard on patient will both lung fields verbalize understandi Patient may manifest: ng of causative Change in mental Interventions 1. Establish rapport 2. Monitor and record VS 3. Assess patients general condition 4. Monitor I&O every 4 hours 5. Weigh patient daily and Rationale 1. To gain patients trust and cooperatio n 2. To obtain baseline data 3. To determine what Evaluation Short Term:Pt shall have verbalized understandi ng of causative factors and demonstrat e behaviors to resolve
status (lethargy or confusion) Restlessness and anxiety
factors and demonstrat e behaviors to resolve excess fluid volume.Lo ng Term:After 3-4 days of nursing intervention s, the patient will demonstrat e adequate fluid balanced AEB output equal to exceeding intake, clearing breath sounds, and decreasing edema.
compare to previous weights. 6. Auscultate breath sounds q 2hr and pm for the presence of crackles and monitor for frothy sputum production 7. Assess for presence of peripheral edema. Do not elevate legs if the client is dyspneic. 8. Follow lowsodium diet and/or fluid restriction 9. Encourage or provide oral care q2 10. Obtain patient history to ascertain the probable cause of the fluid disturbance. 11. Monitor for distended neck veins and ascites 12. Evaluate urine output in response to diuretic therapy. 13. Assess the need for an indwelling urinary catheter. 14. Institute/instruc
approach excess fluid to use in volume.Lo treatment ng Term:Pt 4. I&O shall have balance demonstrat reflects ed adequate fluid fluid status balance 5. Body AEB output weight is a equal to sensitive exceeding indicator intake, of fluid clearing balance breath and an sounds and increase decreasing indicates ed fluid volume excess. 6. When increased pulmonary capillary hydrostati c pressure exceeds oncotic pressure, fluid moves within the alveolar septum and is evidenced by the auscultatio n of crackles. Frothy, pinktinged sputum is an indicator
t patient regarding fluid restrictions as appropriate.
that the client is developin g pulmonary edema 7. Decreased systemic blood pressure to stimulatio n of aldosteron e, which causes increased renal tubular absorption of sodium Lowsodium diet helps prevent increased sodium retention, which decreases water retention. Fluid restriction may be used to decrease fluid intake, hence decreasing fluid volume excess. 8. The client senses thirst
because the body senses dehydratio n. Oral care can alleviate the sensation without an increase in fluid intake. 9. Heart failure causes venous congestion , resulting in increased capillary pressure. When hydrostatis pressure exceeds interstitial pressure, fluids leak out of ht ecpaillarie s and present as edema in the legs, and sacrum. Elevation of legs increases venous return to the heart. 10. May include
increased fluids or sodium intake, or compromi sed regulatory mechanis ms. 11. Inidicates fluid overload 12. Focus is on monitorin g the response to the diuretics, rather than the actual amount voided 13. Treatment focuses on diuresis of excess fluid. 14. This helps reduce extracellul ar volume.
Acute Pain In ischemic heart disease, atherosclerosis develops in the coronary arteries, causing them to become narrowed or blocked. When a coronary artery is blocked, blood flow to the area of the heart supplied by that artery is reduced. If the remaining blood flow is inadequate to meet the oxygen demands of the heart, the area may become ischemic and injured and myocardial infarction may result. Neural pain receptors are stimulated by local mechanical stress resulting from abnormal myocardial contraction. Assessment Planning Subjective:PainObjective:Pat Short Interventions 1. Assess Rationale 1. To identify Evaluation Short
ient manifested:
Term:After 3-4 hours of nursing (+) DOB with a rate of 7 out of intervention s, the 10 patients with complaints of pain will chest pain decrease unprovoked from 7 to 3 as Patient may manifest: verbalized by the Restlessness patient.Lon g Term:After 2-3 days of nursing intervention s, the patient will demonstrate activities and behaviors that will prevent the recurrence of pain.
2.
3.
4.
5.
6. 7.
8.
patient pain for intensity using a pain rating scale, for location and for precipitating factors. Administer or assist with selfadministrati on of vasodilators, as ordered. Assess the response to medications every 5 minutes Provide comfort measures. Establish a quiet environment . Elevate head of bed. Monitor vital signs, especially pulse and blood pressure, every 5 minutes until pain subsides. Teach patient relaxation techniques and how to use them to reduce
2.
3.
4.
5.
6.
intensity, Term:Patie precipitating nt shall factors and have location to verbalized assist in a decrease accurate in pain diagnosis. from a The scale of 7 vasodilator to 3.Long nitroglycerin Term:The enhances patient blood flow to shall have the demonstrat myocardium. ed activities It reduces the and amount of behaviors blood that will returning to prevent the the heart, recurrence decreasing of pain. preload which in turn decreases the workload of the heart. Assessing response determines effectiveness of medication and whether further interventions are required. To provide nonpharmaco logical pain management. A quiet environment reduces the energy demands on the patient. Elevation improves
stress. 9. Teach the patient how to distinguish between angina pain and signs and symptoms of myocardial infarction.
chest expansion and oxygenation. 7. Tachycardia and elevated blood pressure usually occur with angina and reflect compensatory mechanisms secondary to sympathetic nervous system stimulation. 8. Anginal pain is often precipitated by emotional stress that can be relieved nonpharmacologi cal measures such as relaxation. 9. In some case , the chest pain may be more serious than stable angina. The patient needs to understand the differences in order to seek emergency care in a timely fashion.
Activity Intolerance As heart failure becomes more severe, the heart is unable to pump the amount of blood required to meet all of the bodys needs. To compensate, blood is diverted away from less-crucial areas, including the arms and legs, to supply the heart and brain. As a result, people with heart failure often feel weak (especially in their arms and legs), tired and have difficulty performing ordinary activities such as walking, climbing stairs or carrying groceries NDx: Activity intolerance r/t imbalance O2 supply and demand AEB limited ROM, generalized weakness and DOB Assessment Planning Subjective:Objective:Patient Short manifested: Term:After 3-4 hours of nursing interventions, generalized the patient will weakness use identified limited range of motion as observed techniques to abnormal pulse rate improve activity and rhythm intoleranceLong (+) DOB Term:After 2-3 days of nursing interventions, the patient will report measurable increase in activity intolerance.. Interventions 1. Establish Rapport 2. Monitor and record Vital Signs 3. Assess patients general condition 4. Adjust clients daily activities and reduce intensity of level. Discontinue activities that cause undesired psychological changes 5. Instruct client in unfamiliar activities and in alternate ways of conserve energy 6. Encourage patient to have adequate bed rest and sleep 7. Provide the Rationale Evaluation 1. To gain clients participati on and cooperatio n in the nurse patient interaction 2. To obtain baseline data 3. To note for any abnormali ties and deformitie s present within the body 4. To prevent strain and overexerti on 5. To conserve energy and promote safety 6. to relax the body 7. to provide
patient with a calm and quiet environment 8. Assist the client in ambulation 9. Note presence of factors that could contribute to fatigue 10. Ascertain clients ability to stand and move about and degree of assistance needed or use of equipment 11. Give client information that provides evidence of daily or weekly progress 12. Encourage the client to maintain a positive attitude 13. Assist the client in a semi-fowlers position 14. Elevate the head of the bed 15. Assist the client in learning and demonstrating appropriate safety measures
relaxation 8. to prevent risk for falls that could lead to injury 9. fatigue affects both the clients actual and perceived ability to participate in activities 10. to determine current status and needs associated with participati on in needed or desired activities 11. to sustain motivatio n of client 12. to enhance sense of well being 13. to promote easy breathing 14. to maintain an open airway 15. to prevent injuries 16. to avoid
16. Instruct the SO not to leave the client unattended 17. Provide client with a positive atmosphere 18. Instruct the SO to monitor response of patient to an activity and recognize the signs and symptoms
risk for falls 17. to help minimize frustration and rechannel energy 18. to indicate need to alter activity lev
Ineffective Airway Clearance Mucus is produced at all times by the membranes lining the air passages. When the membranes are irritated or inflamed, excess mucus is produced and it will retain in tracheobronchial tree. The inflammation and increased in secretions block the airways making it difficult for the person to maintain a patent airway. In order to expel excessive secretions, cough reflex will be stimulated. An increased in RR will also be expected as a compensatory mechanism of the body due to obstructed airways. NDx: Ineffective airway clearance RT retained secretions AEB presence of rales on both lung fields. Assessment Planning Subjective:Objective:Patie Short nt manifested: Term:After 3-4 hours of nursing with productive cough yellowish in interventions , the patient color will be able presence of rales upon auscultation to establish and maintain (+) DOB airway with pale patency conjunctiva, nail AEB beds and buccal absence of Interventions 1. Monitor and record vital signs. 2. Assess patients condition. 3. Monitor respirations and breath sounds, noting rate and sounds. 4. Position head Rationale Evaluation 1. To obtain Short baseline Term:The data patient shall 2. To know have been the patients able to general establish and condition maintain 3. To airway determine patency respiratory AEB distress and absence of accumulatio respiratory n of distress.Lon
mucosa
signs of respiratory distress.Lon g Term:After 2-3 days of NI, the patient will be able to demonstrate improve airway clearance AEB reduction of congestion with breath sounds clear and improved RR.
properly 5. Position appropriately and discourage use of oilbased products around nose. 6. Auscultate breath sounds and assess air movement. 7. Encourage deep breathing and coughing exercises 8. Elevate head of bed and encourage frequent position changes. 9. Keep back dry and loosen clothing 10. Observed for signs and symptoms of infection. 11. Instruct patient have adequate rest periods and limit activities to level of activity intolerance. 12. Give expectorants and bronchodilato rs as ordered. 13. Suction
secretions. g Term:The 4. To open or patient shall maintain have been open able to airway. demonstrate 5. To prevent improve vomiting airway with clearance aspiration AEB into lungs. reduction of 6. To ascertain congestion status and with breath note sounds clear progress. and 7. To improved maxixmize RR. effort 8. To promote maximal inspiration, enhance expectoratio n of secretions in order to improve ventilation 9. To promote comfort and adequate ventilation 10. To identify infectious process and promote timely intervention . 11. Rest will prevent fatigue and decrease oxygen demands for metabolic demands
secretions PRN 14. Administer oxygen therapy and other medications as ordered.
12. To further mobilize secretions 13. To clear airway when secretions are blocking the airway 14. Indicated to increase oxygen saturation.
You might also like
- Lab ValuesDocument3 pagesLab Valuessurviving nursing school100% (3)
- High Sensitivity CRP - IMMULITE and IMMULITE 1000 - Rev 06 DXDCM 09017fe980297730-1538194293759Document36 pagesHigh Sensitivity CRP - IMMULITE and IMMULITE 1000 - Rev 06 DXDCM 09017fe980297730-1538194293759Deqsa Corporativo0% (1)
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliNo ratings yet
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail Abaygar100% (3)
- The Impact of Social Media Powerpoint PresentationDocument36 pagesThe Impact of Social Media Powerpoint PresentationCamille Pineda60% (5)
- OSCE Station 1 Diabetic LL ExamDocument5 pagesOSCE Station 1 Diabetic LL ExamJeremy YangNo ratings yet
- Nursing Care Plan: General: Goals Met GenreralDocument3 pagesNursing Care Plan: General: Goals Met GenreralRomzy BasañesNo ratings yet
- Breast Self Exam BrochureDocument2 pagesBreast Self Exam Brochureapi-252329688100% (1)
- Impaired Tissue PerfusionDocument2 pagesImpaired Tissue PerfusionLyka Mae Imbat - PacnisNo ratings yet
- Decreased Cardiac OutputDocument4 pagesDecreased Cardiac OutputAdnan Khan100% (1)
- Healthcare - Nursing Care Plan - Excess Fluid VolumeDocument4 pagesHealthcare - Nursing Care Plan - Excess Fluid VolumeBenjamin CañalitaNo ratings yet
- Acute PainDocument3 pagesAcute PainJayr ChinNo ratings yet
- Assessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermDocument4 pagesAssessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermGensen Cu RoxasNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care Planapi-309251523No ratings yet
- NCPDocument2 pagesNCPNaidin Catherine De Guzman-AlcalaNo ratings yet
- Assessment Diagnosis Planning Nursing Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Nursing Intervention Rationale Evaluationjennelyn losantaNo ratings yet
- NCP Self CaRE DeficitDocument1 pageNCP Self CaRE Deficitnicole pageNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanCrystelle MonaresNo ratings yet
- Ineffective Airway Clearance CareplanDocument6 pagesIneffective Airway Clearance CareplanderreshaNo ratings yet
- Nursing Care Plan - Mam EkaDocument7 pagesNursing Care Plan - Mam EkaGlenn Asuncion PagaduanNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanNo ratings yet
- Imbalanced NutritionDocument3 pagesImbalanced NutritionIlisa ParilNo ratings yet
- Nursing Care PlanDocument5 pagesNursing Care PlanPaola Marie VenusNo ratings yet
- NCP PTBDocument2 pagesNCP PTBMack Jhed AnarconNo ratings yet
- Excess Fluid Volume PPT (Case Press)Document10 pagesExcess Fluid Volume PPT (Case Press)Perrilyn PereyNo ratings yet
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- NCP InfectionDocument3 pagesNCP InfectionPrince AhmirNo ratings yet
- Burns - Airway Clearance, Risk For IneffectiveDocument2 pagesBurns - Airway Clearance, Risk For Ineffectivemakyofrancis20No ratings yet
- Budget Plan For COPARDocument3 pagesBudget Plan For COPARPaolo Rafael D EsguerraNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument3 pagesAssessment Diagnosis Planning Implementation Rationale EvaluationHanz AlecNo ratings yet
- NCP AirwayDocument2 pagesNCP AirwayjlucandoNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanJobelyn TunayNo ratings yet
- Nursing Care Plan FinalDocument16 pagesNursing Care Plan FinalErickson OcialNo ratings yet
- Assignment For Oxy. Online BasedDocument5 pagesAssignment For Oxy. Online BasedNurhassem Nor AkangNo ratings yet
- NCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsDocument3 pagesNCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsSarah Ann Jamilla FaciolanNo ratings yet
- Nursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleDocument8 pagesNursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleTrysna Ayu Sukardi100% (1)
- NCP Copd4Document15 pagesNCP Copd4Alessa Marie Crisostomo Salazar100% (1)
- NCP TB MeningitisDocument1 pageNCP TB MeningitisMark Adrian D. DizorNo ratings yet
- Nursing Care Plan, Diagnosis, Interventions Hyperthermia, Fever, High TemperatureDocument2 pagesNursing Care Plan, Diagnosis, Interventions Hyperthermia, Fever, High TemperatureVanessa AbboudNo ratings yet
- NCPDocument5 pagesNCPRose AnnNo ratings yet
- Nursing Care Plan For LYING inDocument4 pagesNursing Care Plan For LYING inKarissa CiprianoNo ratings yet
- NCP BMDocument1 pageNCP BMSourabh MehraNo ratings yet
- Student NurseDocument2 pagesStudent NurseTAYABAN, KENNETH JAKE, Q.No ratings yet
- HTP of AsthmaDocument1 pageHTP of AsthmaMarland Faith Dela CruzNo ratings yet
- Rufino, Leslie Kriztel S. BSN 3-2 Group 1Document6 pagesRufino, Leslie Kriztel S. BSN 3-2 Group 1Deinielle Magdangal RomeroNo ratings yet
- Nursing Care Plan Renal FailureDocument18 pagesNursing Care Plan Renal FailureKundan KumarNo ratings yet
- NCP For StokeDocument5 pagesNCP For StokeMemedNo ratings yet
- Assessment Explanation of The Problem Planning Nursing Intervention Rationale EvaluationDocument2 pagesAssessment Explanation of The Problem Planning Nursing Intervention Rationale EvaluationRodolfo Bong SemaneroNo ratings yet
- MGH 8 - Ihd - NCPDocument12 pagesMGH 8 - Ihd - NCPSesinando Niez Quilao Jr.100% (1)
- Acute Renal Failure Nursing Care PlanDocument15 pagesAcute Renal Failure Nursing Care PlanRanusha AnushaNo ratings yet
- Impaired Physical Mobility R/T Neuromuscular ImpairmentDocument3 pagesImpaired Physical Mobility R/T Neuromuscular ImpairmentjisooNo ratings yet
- DHF NCP 2Document1 pageDHF NCP 2mavefigNo ratings yet
- NCP Blood Glucose Imbalance 4thDocument2 pagesNCP Blood Glucose Imbalance 4thRainier IbarretaNo ratings yet
- Nursing Care Plan: Group 4-Open Wound Head Injury After Debris FallDocument3 pagesNursing Care Plan: Group 4-Open Wound Head Injury After Debris FallNicole Villanueva, BSN - Level 3ANo ratings yet
- Wk2 NCP Edited2012Document6 pagesWk2 NCP Edited2012Jessely Caling SalasNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanMarielle SorianoNo ratings yet
- NCP Acute PainDocument3 pagesNCP Acute PainNathalie kate petallarNo ratings yet
- Anatomy and Physiology PneumoniaDocument4 pagesAnatomy and Physiology PneumoniaJohnson MallibagoNo ratings yet
- Assessment of Patients in CCUDocument75 pagesAssessment of Patients in CCUShubham Singh Bisht100% (1)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Objective: Short Term: Independent: Short TermDocument3 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Objective: Short Term: Independent: Short TermMicaela CrisostomoNo ratings yet
- NCPDocument3 pagesNCPJezza RequilmeNo ratings yet
- Welcome To The Case Study Presentation:-: Prostate CancerDocument22 pagesWelcome To The Case Study Presentation:-: Prostate CancerDengo ChapatieeNo ratings yet
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezNo ratings yet
- Nursing Care PlanDocument19 pagesNursing Care PlanChic Dian UsmanNo ratings yet
- NCPDocument22 pagesNCPMaricris S. Sampang100% (1)
- Health and Emergency Medical Services - MSRDocument37 pagesHealth and Emergency Medical Services - MSRCamille PinedaNo ratings yet
- Physical Assessment. - TyphoidDocument4 pagesPhysical Assessment. - TyphoidCamille PinedaNo ratings yet
- His T SpiritualityDocument83 pagesHis T SpiritualityCamille PinedaNo ratings yet
- Drug Study - LeptospirosisDocument19 pagesDrug Study - LeptospirosisCamille PinedaNo ratings yet
- Henrietta Lacks: Dr. Roz Iasillo Trinity High School River Forest, ILDocument13 pagesHenrietta Lacks: Dr. Roz Iasillo Trinity High School River Forest, ILRoz IasilloNo ratings yet
- Schizoaffective Disorder in The DSM 5 PDFDocument5 pagesSchizoaffective Disorder in The DSM 5 PDFpipiitopandabamboo247No ratings yet
- Pty 309Document2 pagesPty 309Geetanjali SaggarNo ratings yet
- Trigeminal Neuralgia (Agstri Dwi Marsela)Document11 pagesTrigeminal Neuralgia (Agstri Dwi Marsela)Agstri Dwi MarselaNo ratings yet
- Health SciencesDocument170 pagesHealth SciencesSabiran GibranNo ratings yet
- Endodontic TT OutcomesDocument22 pagesEndodontic TT OutcomesritikaNo ratings yet
- Medical EthicsDocument3 pagesMedical EthicsJona MagudsNo ratings yet
- Skradski Jaclyn CVDocument6 pagesSkradski Jaclyn CVapi-293245490No ratings yet
- Reporte Indicadores Proactivos y Reactivos Rev.2-1Document11 pagesReporte Indicadores Proactivos y Reactivos Rev.2-1Huber CallataNo ratings yet
- H21 261 2005eDocument26 pagesH21 261 2005eKartika Ramadhani BahriNo ratings yet
- Menstrual CycleDocument24 pagesMenstrual CycleMonika Bagchi100% (6)
- Aplastic AnemiaDocument16 pagesAplastic Anemiahazelposis100% (1)
- Resume 2021-6Document3 pagesResume 2021-6api-437078872100% (1)
- Vii. AssignmentDocument2 pagesVii. AssignmentRhodney BubudNo ratings yet
- MATS CurriculumDocument85 pagesMATS CurriculummamunpalashNo ratings yet
- Pharmacoeconomics: BY Mrs. K.Shailaja., M. Pharm., Lecturer Dept of Pharmacy Practice, SRM College of PharmacyDocument15 pagesPharmacoeconomics: BY Mrs. K.Shailaja., M. Pharm., Lecturer Dept of Pharmacy Practice, SRM College of Pharmacytsegaab yosephNo ratings yet
- Research EssayDocument13 pagesResearch Essayapi-609533251No ratings yet
- Laporan Diagnosa Pasien HarianDocument1 pageLaporan Diagnosa Pasien Hariansiti nurlailiyahNo ratings yet
- LP 8 Orif FemurDocument42 pagesLP 8 Orif FemurdaliaberseNo ratings yet
- The Mckenzie MethodDocument24 pagesThe Mckenzie MethodMohamed ElMeligieNo ratings yet
- The Ultimate Guide To Biohacking Exercise With Oxygen Therapy, Hypoxia, Elevation & Altitude TrainingDocument17 pagesThe Ultimate Guide To Biohacking Exercise With Oxygen Therapy, Hypoxia, Elevation & Altitude TrainingAlessandro QuercettiNo ratings yet
- Usage of Electronic Resources by The Medical, Dental and Paramedical Science Professionals in KarnatakaDocument7 pagesUsage of Electronic Resources by The Medical, Dental and Paramedical Science Professionals in KarnatakaSougata ChattopadhyayNo ratings yet
- Language For Understanding Covid19 Conversation Topics Dialogs Reading Comprehension 125476Document8 pagesLanguage For Understanding Covid19 Conversation Topics Dialogs Reading Comprehension 125476Deti Kurnia DewiNo ratings yet
- JRRMMC InternshipDocument48 pagesJRRMMC InternshipJason MontesaNo ratings yet
- Tetanus Case Discussion Draft 1Document22 pagesTetanus Case Discussion Draft 1Gio Tamaño BalisiNo ratings yet