NCP Dengue
NCP Dengue
Uploaded by
Richmund Earl GeronCopyright:
Available Formats
NCP Dengue
NCP Dengue
Uploaded by
Richmund Earl GeronOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
NCP Dengue
NCP Dengue
Uploaded by
Richmund Earl GeronCopyright:
Available Formats
Nursing Care Plan
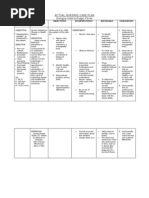
Cues Subjective :Ang init init ng pakiramdam ko As verbalized by the client Objective: Temp = 39 C Flushed skin Warm to touch Nuring Diagnosis Hyperthermia related to physiological factors secondary to dengue hemorrhagic fever Analysis Body temperature elevated above normal level that is usually caused by several factors related to illness. As inoculation occurs, proliferation of virus follows and multiplication occurs. Once the virus starts to grow in number, it will soon reach it pathogenic level that will result into pyrexia or fever as a defense mechanism of the body. Nursing Objective After 4 hours of nursing intervention client will be able to maintain core temperature within normal range as evidenced by:- body temperature is lowered to 37 C Nursing Rationale Intervention Monitor vital signs Serves as baseline data Evaluation September 21, 2012 1:00pm GOAL MET After 4 hours of nursing intervention client was able to maintain core temperature within normal range as evidenced by:- body temperature is lowered to 37C
Perform tepid sponge bath
Heat loss by means of evaporation and conduction
Provide cool environment Maintain bed rest or minimize movementIncrease oral fluid intake
Heat loss by means of convection To reduce metabolic demands of oxygen consumption- to To prevent dehydration and support circulating volume To decrease the patients body temperature
Administer medications as ordered by physicians such as Paracetamol and other anti pyretic drugs
Objective: Irritable Poor skin turgor assessed at the abdomen Dry mucous membranes including the buccal and oral mucosa Passed out stool once in the mor ning. Stool was semisoft, yellow in color and not watery. BP= 120/80 mmHg CR=90bpm PR= 20cpmDeficient fluid
Deficit fluid volume related to the migration of intravascular fluid into extravascular fluid
Water content of the human body progressively decreases from birth to old age. In the neonate, fluid accounts for as much as 75% of body weight. Most of the decrease occurs in the first 10 years of life. Hypovolemia or extracellular fluid volume deficitis the isotonic loss of body fluids, that is, relatively equal losses of sodium and water. Pediatric clients are more at risk of hypovolemia and dehydration because their bodies need to have a higher proportion of water to total body weight. Excessive fluid loss reduced fluid intake, third-space fluid shift, and a combination of these factors causes
After an 8hour shift, client will be able to demonstrate adequate fluid balance as evidenced by good skin turgor, moist skin and mucous membranes
Note potential sources of fluid loss/intake
Causative/ contributing factors for fluid imbalances
September 22, 2012 12:00am GOAL MET
Continue monitor the vital signs, mucous membranes, weight, skin turgor, breath sounds, urinary and gastric output. Review patients intake of fluids. Hydrate with water after every feeding Determine childs normal pattern of elimination
Indicators of hydration After an 8-hour shift, client status was able to demonstrate adequate fluid balance as evidenced by good skin turgor, moist skin and mucous membranes
Provides baseline and comparison
Provides information for baseline and comparison
Continue monitor the patients weight and compare the result on the next days. Weigh on the same
Consistency with weight measurement helps ensure more accurate results. Weight is a useful indicator
fluid volume loss. Fluid loss causes include abdominal surgery, diabetes mellitus, diarrhea, vomiting, excessive diuretic therapy, excessive use of laxatives, excessive perspiration and crying, fever, fistulas, hemorrhage, nasogastric drainage and renal failure with polyuria.
scale at the same time of day &wearing same amount of clothing
of fluid balance. Weig ht loss indicates that child is not receiving adequate fluid replacement and adjustments need to bemade Provides fluid & nutritional support to replace active fluid loss. Close monitoring and regulation is required to prevent fluid overload while correcting fluid balance.
Administer and monitor IV fluids as ordered
You might also like
- Dengue Fever Nursing Care Plan-High Risk For Fluid Volume Deficit100% (2)Dengue Fever Nursing Care Plan-High Risk For Fluid Volume Deficit1 page
- NCP Dengue Fever Hyperthermia and Acute Pain100% (1)NCP Dengue Fever Hyperthermia and Acute Pain4 pages
- Dengue Fever Nursing Care Plan-High Risk For Fluid Volume Deficit100% (5)Dengue Fever Nursing Care Plan-High Risk For Fluid Volume Deficit1 page
- Assessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveNo ratings yetAssessment Diagnisis Planning Intervention Rationale Evaluation Subjective2 pages
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation100% (1)Assessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation3 pages
- 3 Nursing Care Plans For Dengue Hemorrhagic Fever100% (3)3 Nursing Care Plans For Dengue Hemorrhagic Fever8 pages
- Short Term: Independent: Independent: Short TermNo ratings yetShort Term: Independent: Independent: Short Term2 pages
- Cues/Data Nursing Diagnosis Scientific Basis Goals of Care Nursing Interventions Rationale Evaluation100% (1)Cues/Data Nursing Diagnosis Scientific Basis Goals of Care Nursing Interventions Rationale Evaluation4 pages
- Nursing Diagnosis Objectives Nursing Interventions Rationale EvaluationNo ratings yetNursing Diagnosis Objectives Nursing Interventions Rationale Evaluation9 pages
- Nursing Diagnosis For Pediatrics Gastroenteritis 1100% (4)Nursing Diagnosis For Pediatrics Gastroenteritis 12 pages
- Simulation Lab 20 Instructions With Answers100% (3)Simulation Lab 20 Instructions With Answers5 pages
- Cerebral Palsy: Classification and Etiology: Beyin Felci: Sını Ama Ve EtyolojiNo ratings yetCerebral Palsy: Classification and Etiology: Beyin Felci: Sını Ama Ve Etyoloji4 pages
- Planning Equipments and Supplies For Nursing Care in Hospital100% (10)Planning Equipments and Supplies For Nursing Care in Hospital14 pages
- Cardiology Discharge Summary Escription Edited FileNo ratings yetCardiology Discharge Summary Escription Edited File4 pages
- Summer Training ON: Biomedical EquipmentsNo ratings yetSummer Training ON: Biomedical Equipments20 pages
- Ceramic Restorations: Bonded Porcelain Veneers - Part 1: PerspectiveNo ratings yetCeramic Restorations: Bonded Porcelain Veneers - Part 1: Perspective5 pages
- Instant Download MCQs in Pediatrics Review of Nelson Textbook of Pediatrics 20th Edition Zuhair M Almusawi PDF All Chapters100% (4)Instant Download MCQs in Pediatrics Review of Nelson Textbook of Pediatrics 20th Edition Zuhair M Almusawi PDF All Chapters55 pages
- AAPD Guideline On Management of The Developing Dentition and Occlusion100% (1)AAPD Guideline On Management of The Developing Dentition and Occlusion13 pages
- Healthcare Savings: Michelle S. Tolentino 2F-PharmacyNo ratings yetHealthcare Savings: Michelle S. Tolentino 2F-Pharmacy2 pages
- Dr. Sudhir Shah: M.D., D.M. (Neurology)No ratings yetDr. Sudhir Shah: M.D., D.M. (Neurology)55 pages