5.a Missing Incisor
5.a Missing Incisor
Uploaded by
mirfanulhaqCopyright:
Available Formats
5.a Missing Incisor
5.a Missing Incisor
Uploaded by
mirfanulhaqOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
5.a Missing Incisor
5.a Missing Incisor
Uploaded by
mirfanulhaqCopyright:
Available Formats
G
Case
5
A missing incisor
SUMMARY
A 9-year-old boy is referred to you in the orthodontic
department with an unerupted upper left central
incisor. What is the cause and how may it be treated?
Medical history
The patient has suffered from asthma since he was 4 years
old. This is controlled using salbutamol (Ventolin).
Examination
Extraoral examination
There are no extraoral signs or symptoms and the patient is
an active, happy boy.
Intraoral examination
The appearance of the mouth is shown in Figure 5.1. What
do you see?
The patient is in the early mixed dentition stage and the
teeth present are:
6 1 6
6 21 12 6
EDCB BCDE
EDC DE
No upper left central incisor is present, but there is a pale
swelling high in the upper labial sulcus above the edentulous
space and the upper left B. There has been some loss of
space in the region of the absent upper central incisor.
There is a tendency to an anterior open bite which is slightly
more pronounced on the right.
There is mild upper and lower arch crowding and a unilateral
crossbite on the left. If you were able to examine the patient
you would discover that this is associated with a lateral
displacement of the mandibular position. The lower centre
line is shifted to the left.
There are no restorations but the mouth is not very clean.
What are the possible causes of an apparently absent upper
central incisor?
The incisor may be missing or have failed to erupt. Possible
causes include the following:
Missing Developmentally absent
Extracted
Avulsed
Failure to erupt Dilaceration and/or displacement as a result of trauma
Scar tissue preventing eruption
Supernumerary tooth preventing eruption
Insufcient space as a result of crowding
Pathological lesion (e.g. cyst or odontogenic tumour)
What specifc questions would you ask the parents?
The most important questions are related to trauma. Avulsion
or dilaceration would follow signifcant trauma which is likely
to be recalled by the parent. The parent should be asked
whether the deciduous predecessor was discoloured. If it was
this would provide evidence of loss of vitality, perhaps related
to trauma.
Extraction would be unusual and a cause should be readily
obtained in the history.
In response to your questioning the parent reports that the
patient fell on his face when he was much younger. At the
time of the accident there was considerable injury to his lips
Fig. 5.1 The appearance of the patient on presentation.
History
Complaint
The patients upper left central incisor has not erupted
although he is 9 years old. The mother is very concerned
about her sons appearance and is anxious for him to be
treated.
History of complaint
The upper left deciduous predecessor had been present
until about 4 months ago. It was extracted by the patients
general dental practitioner in an attempt to speed up the
eruption of the permanent successor. Despite this, there has
been no change in appearance. The upper permanent central
incisor on the opposite side erupted normally at 7 years of
age.
G
A MI S S I N G I N C I S O R
24
5 C
A
S
E
What radiographic views would you request and why?
See Table 5.1.
The radiographs of the patient are shown in Figures
5.25.4.
What do the radiographs show?
The panoramic radiograph confrms the presence of a full
complement of developing permanent successors, excluding
the third molars, which would not be expected to have
formed. However, a crypt should be present between the
ages of 8
1
/
2
and 10 years of age and there is a suggestion of
early crypt formation in the lower left quadrant. The
unerupted permanent upper left central incisor is clearly
visible on this radiograph; its shape is not normal but the root
shape cannot be seen in this view. It is not possible to
establish the labiopalatal position of the tooth in this flm nor
to detect an adjacent supernumerary tooth which may lie
outside the tomographic focal trough.
The periapical view gives considerably more detail. The upper
left central incisor has an intact but distorted root. Its apical
development appears normal and similar to that of the right
central incisor but the foreshortened appearance suggests
dilaceration. Using this flm in conjunction with the
panoramic view and applying the principle of vertical parallax
you can see that the crown of the central incisor is labially
positioned. This is consistent with the swelling in the sulcus
being caused by the crown of the tooth. No supernumerary
tooth is present.
The lateral view completes the picture and shows clearly the
displaced crown of the central incisor. From the three flms it
is possible to deduce that the crown and root of the tooth
are misaligned, the crown defected labially with its incisal
edge pointing forwards into the labial sulcus and the root
developing in the normal direction.
What is your fnal diagnosis?
The upper left central incisor is dilacerated, probably as a
result of intrusion of the deciduous predecessor in the injury
sustained in infancy.
Treatment
What are the options for treatment?
If the dilaceration were severe, the tooth would require
extraction. Then either of the following options could be
selected:
1. Align the adjacent teeth, ideally with fxed appliances,
using the central incisor space. The lateral incisor would
replace the central incisor and could be masked to
simulate it. In the short term this could be accomplished
by an adhesive restoration but in the longer term a
permanent restoration would be necessary. The canine
might also need restoration or masking so that it would
not appear incongruous, especially in a patient with
slender lateral incisors. This option is not ideal because
the fnal appearance is often poor.
and teeth, but no tooth loss was noticed and no dental
opinion was sought.
What are the likely causes of the anterior open bite and
shift in the lower centre line?
The anterior open bite is probably associated with a thumb-
sucking or similar habit. The shift in the centre line is probably
caused by the combination of crowding and early exfoliation
of the lower left C.
Give a diferential diagnosis for the cause of the missing
incisor. Explain each possibility.
Dilaceration of the central incisor as a result of the injury
appears the most likely cause. However, it is unclear whether
the injury was severe enough to cause dilaceration.
Dilaceration usually follows intrusion and the intruded tooth
might well have re-erupted into its normal position. The
swelling in the sulcus does not lie on the normal eruption
path of the central incisor, and dilaceration could explain the
abnormal position.
A supernumerary tooth or an odontome would be the
next most likely possibility if trauma is not the cause.
Supernumerary teeth are not uncommon in the premaxilla
(13% of the population), and the late-forming (tuberculate)
type which often lies adjacent to the crown of the permanent
incisor frequently causes delay or failure of eruption.
A pathological lesion appears unlikely but cannot be
excluded. There is no evidence of alveolar expansion to
suggest a cyst, which would be the most likely cause and
could arise from the tooth itself, a supernumerary or an
odontome. An unexpected lesion remains a remote possibility.
What causes have you excluded and why?
Crowding appears to be an unlikely cause. It would have to
be very severe to cause a delay of up to 2 years and this
patients teeth are only mildly crowded. Crowding is a very
unusual cause for failure of eruption of a central incisor
because resorption and loss of the B would provide enough
space for eruption.
Scarring of the alveolus delays eruption because it slows
resorption of bone over the tooth and because fbrosis and
thickening of the mucoperiosteum resists tooth movement.
This is an unlikely cause because there is no reason to suspect
scarring, the deciduous predecessor having been extracted
only 4 months ago.
Avulsion can be excluded because it seems that the tooth
has never erupted and there is no recent history of trauma.
Developmental causes of absence appear most unlikely.
The swelling in the upper sulcus would seem to indicate that
the tooth is present but has failed to erupt. A missing central
incisor without other missing teeth would be an extremely
rare fnding.
Investigations
Radiographs are required to determine whether or not the
unerupted tooth is present, to establish whether it is the
cause of the swelling in the sulcus and detect possible
supernumerary teeth.
G
A MI S S I N G I N C I S O R
25
5
C
A
S
E
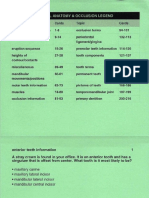
Table 5.1 Radiographic views and their purposes
View Reason
Dental panoramic radiograph To provide a general view of the developing dentition and establish the presence or absence of the permanent teeth and any supernumeraries.
Upper standard occlusal or periapicals of the
edentulous area, taken with a paralleling
technique
To provide a more detailed view of the region, in particular the root morphology and any adjacent structures such as supernumerary teeth or
pathological lesions. These may lie outside the focal trough of the radiograph or be obscured by superimposition of other structures in the panoramic
view. If periapical views are taken they should include the adjacent teeth in case these were damaged in the original accident. In addition the standard
occlusal and panoramic view can be used together to establish the relationship of unerupted structures relative to the dental arch, using the principle
of (vertical) parallax. Objects lying nearer to the X-ray tube (labially positioned) appear to move in the opposite direction to the tube relative to a fxed
point. Those further away (palatally positioned) appear to move in the same direction as the tube.
Lateral view Confrms the presence of any distortion of the tooth, if dilacerated, and confrms the relationship of the tooth to the labial swelling in a third
dimension.
Fig. 5.2 Dental panoramic
radiograph.
Fig. 5.3 Periapical views.
G
A MI S S I N G I N C I S O R
26
5 C
A
S
E
Should a fxed or removable appliance be used?
As the tooth movements are relatively simple an upper
removable appliance can be used at this stage. More control
and more accurate tooth positioning would be achieved with
a fxed appliance. However, the patient will probably require
further fxed appliance treatment at a later age and the fne
adjustment of tooth position could be performed then.
Design a suitable removable appliance.
2. Immediate replacement of the extracted central incisor
by a denture or adhesive bridge with a permanent
restoration or possibly a single tooth implant in
adulthood (see Case 35).
If, on the radiographs, the dilaceration does not appear to be
too severe or lies in the apical portion of the root,
consideration could be given to aligning the tooth
orthodontically. This would involve regaining any lost space
followed by localized surgical exposure of the crown of the
tooth and applying extrusive traction with an orthodontic
appliance.
What factors afect the selection of a particular treatment?
Position and severity of the dilaceration (see above)
The size of overjet
Degree of crowding
Position and condition of the other permanent teeth
The general condition of the mouth
The attitude of the child and parent
Assuming none of these factors prevents the ideal
treatment, what would you recommend for this case?
In this case the ideal treatment is to extrude and align the
dilacerated tooth into the arch.
The dilaceration appears to be in the root and relatively mild.
Therefore, an attempt should frst be made to regain the lost
space to accommodate the central incisor crown. This would
be best achieved by extraction of both upper Cs and the
upper left B to encourage eruption of permanent lateral
incisors. Some months later the dilacerated tooth should be
surgically exposed and an orthodontic attachment with a
length of gold chain placed on its palatal surface for
extrusion.
Fig. 5.4 Lateral view.
Fig. 5.6 After 18 months of treatment.
Fig. 5.5 The ftted extrusion appliance.
The appliance consists of:
cribs on D D (0.6-mm wire)
cribs on 6 6 (0.7-mm wire)
fnger springs on
1
and
2
(0.5-mm wire) to retract and
regain the space for the
1
a buccal arm to extrude
1
(0.7-mm wire) attached to the
gold chain bonded to
1
Figure 5.6 shows the position of the dilacerated tooth after
approximately 18 months of active treatment. What further
treatment may be necessary at a later stage of dental
development?
Ideally it would be appropriate to relieve the crowding in the
permanent dentition and align the teeth, correcting the
unilateral posterior crossbite and eliminating the mandibular
displacement. Details of appropriate treatment cannot be
fnalized until the patient passes from mixed dentition to
permanent dentition at about 1012 years of age.
You might also like
- An Illustrated Atlas of Tooth Carving and Wax-Up TechniquesDocument240 pagesAn Illustrated Atlas of Tooth Carving and Wax-Up TechniquesGlassyNo ratings yet
- Nurs FPX 4010 Assessment 1 Collaboration and Leadership Reflection VideoDocument5 pagesNurs FPX 4010 Assessment 1 Collaboration and Leadership Reflection Videofarwaamjad771100% (1)
- Very Early Orthodontic Treatment-When, Why and HowDocument47 pagesVery Early Orthodontic Treatment-When, Why and HowAnaMariaCastroNo ratings yet
- Ceramic Inlays A Case Presentation and LessonsDocument11 pagesCeramic Inlays A Case Presentation and LessonsStef David100% (1)
- 27-Discoloured Anterior TeethDocument5 pages27-Discoloured Anterior Teethmzusaq100% (3)
- 7-Differences Between Primary and Permanent TeethDocument4 pages7-Differences Between Primary and Permanent TeethAhmed AbdNo ratings yet
- Bonded Composites Versus Ceramic Veneers PDFDocument7 pagesBonded Composites Versus Ceramic Veneers PDFAndykaYayanSetiawanNo ratings yet
- Ultrasonic Periodontal Debridement: Theory and TechniqueFrom EverandUltrasonic Periodontal Debridement: Theory and TechniqueRating: 2.5 out of 5 stars2.5/5 (2)
- AD&D Healer ClassDocument8 pagesAD&D Healer Classarivne863100% (1)
- Exodontia PedodonticsDocument35 pagesExodontia PedodonticsFourthMolar.comNo ratings yet
- Development of OcclusionDocument49 pagesDevelopment of OcclusionSardarni Ramandeep KaurNo ratings yet
- D L, H R & L L: Periodontology 2000Document24 pagesD L, H R & L L: Periodontology 2000ph4nt0mgr100% (1)
- Primary Tooth Pulp Therapy - Dr. Elizabeth BerryDocument52 pagesPrimary Tooth Pulp Therapy - Dr. Elizabeth BerryMihaela TuculinaNo ratings yet
- Refacere Dinti Frontali Cu Cape de CeluloidDocument5 pagesRefacere Dinti Frontali Cu Cape de CeluloidSorina NeamțuNo ratings yet
- Compomer CrownDocument2 pagesCompomer CrownIndah SimamoraNo ratings yet
- Teeth Eruption WordDocument24 pagesTeeth Eruption WordAhmed hegazyNo ratings yet
- Pain Control and Carious Primary TeethDocument3 pagesPain Control and Carious Primary TeethmirfanulhaqNo ratings yet
- Pediatric Dental MedicineDocument273 pagesPediatric Dental MedicineTanya HernandezNo ratings yet
- Pulpitis Treatment in Primary Teeth Via Biodentine, Metapex and Zinc Oxide EugenolDocument9 pagesPulpitis Treatment in Primary Teeth Via Biodentine, Metapex and Zinc Oxide EugenolInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Procedural Dentistry For Complete DenturesDocument272 pagesProcedural Dentistry For Complete DenturesNatalia GuevaraNo ratings yet
- Atraumatic Restorative Treatment: Restorative ComponentDocument11 pagesAtraumatic Restorative Treatment: Restorative ComponentYu Yu Victor Chien100% (1)
- Treatment of Early Childhood Caries A Case Report 2 1Document6 pagesTreatment of Early Childhood Caries A Case Report 2 1SuciNo ratings yet
- Manual CariogramDocument51 pagesManual CariogramDesty DarmaNo ratings yet
- Rehabilitation of Molar-Incisor Hypomineralization (MIH) Complicated With Localized Tooth Surface Loss 2014Document3 pagesRehabilitation of Molar-Incisor Hypomineralization (MIH) Complicated With Localized Tooth Surface Loss 2014player osamaNo ratings yet
- PedodonticsDocument2 pagesPedodonticsjunquelalaNo ratings yet
- Stephen Davies - A Guide To Good Occlusal Practice - A Guide To Good Practice (BDJ Clinician's Guides) - Springer (2022)Document306 pagesStephen Davies - A Guide To Good Occlusal Practice - A Guide To Good Practice (BDJ Clinician's Guides) - Springer (2022)PabloNo ratings yet
- Introduction To Dental Anatomy: Learning Objec TivesDocument12 pagesIntroduction To Dental Anatomy: Learning Objec Tivesbalkiz mahamedNo ratings yet
- Orthodontics 1. Clinical ExaminationDocument8 pagesOrthodontics 1. Clinical Examinationmonica896No ratings yet
- Survival of Porcelain Laminate Veneers With DifferentDocument10 pagesSurvival of Porcelain Laminate Veneers With DifferentPablo BenitezNo ratings yet
- Presentation 1Document15 pagesPresentation 1ZvikyNo ratings yet
- Pulp Therapy For The Young Permanent Dentition: ApexogenesisDocument15 pagesPulp Therapy For The Young Permanent Dentition: Apexogenesisapi-3855312No ratings yet
- Current Concepts in Classification, Indication, Principles and Procedures of Cavity Preparation With Respect To Adhesive RestorationsDocument53 pagesCurrent Concepts in Classification, Indication, Principles and Procedures of Cavity Preparation With Respect To Adhesive RestorationsDr. Nikhil saran100% (7)
- Restoration of The Endo TX - 'D ToothDocument4 pagesRestoration of The Endo TX - 'D ToothAnamaria JurcaNo ratings yet
- Articol L.O.C.Document0 pagesArticol L.O.C.Anda TarasciucNo ratings yet
- Delayed Eruption PDFDocument6 pagesDelayed Eruption PDFIsharajini Prasadika Subhashni GamageNo ratings yet
- Altered Passive Eruption and Active Secondary EruptionDocument25 pagesAltered Passive Eruption and Active Secondary EruptionBenjiNo ratings yet
- Rehabilitative and Esthetics Dentistry: Case 1: PedoDocument101 pagesRehabilitative and Esthetics Dentistry: Case 1: PedoMauriceNo ratings yet
- WHT Is A VeneerDocument3 pagesWHT Is A VeneeruhvyasNo ratings yet
- MIH An OverviewDocument9 pagesMIH An OverviewLaura QuinteroNo ratings yet
- Non-Caries Dental DiseaseDocument61 pagesNon-Caries Dental Diseaseapi-19916399No ratings yet
- Deciduous Dentition: Department of Oral Biology D.I.K.I.O.H.SDocument26 pagesDeciduous Dentition: Department of Oral Biology D.I.K.I.O.H.SSyeda Kulsum Abbas ZaidiNo ratings yet
- Rubber Dam - 07 - HandoutDocument12 pagesRubber Dam - 07 - HandoutOmar Al-AboodNo ratings yet
- Anatomy of Primary TeethDocument4 pagesAnatomy of Primary Teethaphist87No ratings yet
- Tooth Development 1Document14 pagesTooth Development 1ahmedfawakh0No ratings yet
- ECC (Quebec)Document24 pagesECC (Quebec)Nadine Alfy AssaadNo ratings yet
- Indirect Composite Inlays and OnlaysDocument3 pagesIndirect Composite Inlays and OnlaysmegamarwaNo ratings yet
- June 28, 2021Document89 pagesJune 28, 202171- MURALIKRISHNANo ratings yet
- Endo Update 2006 PDFDocument21 pagesEndo Update 2006 PDFRamona MateiNo ratings yet
- Introduction To Pediatric DentistryDocument23 pagesIntroduction To Pediatric Dentistrydr parveen bathla0% (1)
- OverDocument107 pagesOverDeepak KumarNo ratings yet
- Role of A Pedodontist in Cleft Lip and Cleft Palate Rehabilitation - An OverviewDocument25 pagesRole of A Pedodontist in Cleft Lip and Cleft Palate Rehabilitation - An OverviewIJAR JOURNALNo ratings yet
- Obturating Materials For Primary TeethDocument77 pagesObturating Materials For Primary TeethSarath MohanNo ratings yet
- Attrition - OmrDocument16 pagesAttrition - OmrDrMaria Cyriac PullamkalamNo ratings yet
- Non-Restorative Cavity TreatmentDocument8 pagesNon-Restorative Cavity TreatmentQurrat-ul-AinNo ratings yet
- 2017 2018 Dental Anatomy and Occlusion 1Document435 pages2017 2018 Dental Anatomy and Occlusion 1Aura UrbayoNo ratings yet
- Restorative MaterialDocument91 pagesRestorative MaterialShivani DubeyNo ratings yet
- Reference: Shillingburg Funamentals of Fixed Prosthodontics, Third Edition Chapter OneDocument14 pagesReference: Shillingburg Funamentals of Fixed Prosthodontics, Third Edition Chapter Oneوا إسلاماه100% (1)
- Tanvi Shah - Maaz ShaikhDocument29 pagesTanvi Shah - Maaz ShaikhTanvi ShahNo ratings yet
- Tests Orthodontics Ex - An.v en 2018-2019 in Lucru LazarevDocument31 pagesTests Orthodontics Ex - An.v en 2018-2019 in Lucru LazarevAndrei Usaci100% (1)
- Oral and Dental HistologyDocument6 pagesOral and Dental HistologyCésar HelenoNo ratings yet
- The Dental Pulp and Periradicular TissuesDocument43 pagesThe Dental Pulp and Periradicular TissuesmirfanulhaqNo ratings yet
- Alveolar Bone/ Alveolar ProcessDocument16 pagesAlveolar Bone/ Alveolar ProcessmirfanulhaqNo ratings yet
- Pros Exam 1 2002Document8 pagesPros Exam 1 2002mirfanulhaqNo ratings yet
- Gingival InflammationDocument19 pagesGingival InflammationmirfanulhaqNo ratings yet
- Pulp ProtectionDocument13 pagesPulp ProtectionmirfanulhaqNo ratings yet
- Peds Restorative PDFDocument4 pagesPeds Restorative PDFmirfanulhaqNo ratings yet
- Complications in Dentoalveolar Surgery PDFDocument37 pagesComplications in Dentoalveolar Surgery PDFmirfanulhaqNo ratings yet
- Pulp ProtectionDocument13 pagesPulp ProtectionmirfanulhaqNo ratings yet
- G Fluoridetherapy PDFDocument4 pagesG Fluoridetherapy PDFmirfanulhaqNo ratings yet
- Oral RadiologyDocument15 pagesOral RadiologymirfanulhaqNo ratings yet
- Periodon TicsDocument201 pagesPeriodon TicsmirfanulhaqNo ratings yet
- Orthodontics: T Glossary of Dentofacial Orthopedic Terms - Orthodontic Glossary A A O - T - Y - I 19Document12 pagesOrthodontics: T Glossary of Dentofacial Orthopedic Terms - Orthodontic Glossary A A O - T - Y - I 19mirfanulhaq100% (1)
- Oral Surgery Board ReviewDocument26 pagesOral Surgery Board ReviewmirfanulhaqNo ratings yet
- Documentation and SBARDocument25 pagesDocumentation and SBARmahmoud ShakriaNo ratings yet
- HookwormDocument30 pagesHookwormGhea IrawanNo ratings yet
- General ObjectivesDocument13 pagesGeneral ObjectiveskevinNo ratings yet
- PESCI /physical ExaminationsDocument5 pagesPESCI /physical ExaminationslaureeateNo ratings yet
- Fracturi de Coloana Cervicala, Toracala Si LombaraDocument770 pagesFracturi de Coloana Cervicala, Toracala Si Lombaracomir2002100% (3)
- 56 Anaesthesia For Carotid Endarterectomy PDFDocument10 pages56 Anaesthesia For Carotid Endarterectomy PDFHarish BhatNo ratings yet
- LMR - J. AndresDocument19 pagesLMR - J. AndresJAY LAPAZ ANDRES, RN, BSN, MAN (C), MAEd.. (C)No ratings yet
- Chandio PDFDocument3 pagesChandio PDFAdilMunirNo ratings yet
- ATTILA Case Report FormsDocument37 pagesATTILA Case Report FormsFrancisco Alfonso Burgos JuliánNo ratings yet
- RSDH Confirms Three COVID-19 Cases at SJMC PDFDocument2 pagesRSDH Confirms Three COVID-19 Cases at SJMC PDFAlywin AlweeNo ratings yet
- CholangitisDocument4 pagesCholangitisNarianne Mae Solis Bedoy100% (1)
- Consensus From The 10th European Bifurcation Club MeetingDocument16 pagesConsensus From The 10th European Bifurcation Club MeetingMichael Jansen SulaimanNo ratings yet
- The CS Mistakes The People MadeDocument4 pagesThe CS Mistakes The People MadeJason SteelNo ratings yet
- Anaphylactic ShockDocument36 pagesAnaphylactic ShockCarmelli Mariae Calugay100% (1)
- Anesthesia Considerations For Neuromuscular DiseaseDocument42 pagesAnesthesia Considerations For Neuromuscular Diseasesamrox54No ratings yet
- Supra Ventricular TachycardiaDocument10 pagesSupra Ventricular TachycardiaJohn RobinsonNo ratings yet
- Divalproex Sodium (Depakote ER)Document1 pageDivalproex Sodium (Depakote ER)karenmichellelecarozNo ratings yet
- Diificult AirwayDocument13 pagesDiificult AirwayBhi-An BatobalonosNo ratings yet
- Reliability of Growth Prediction With Hand - Wrist RadiographsDocument5 pagesReliability of Growth Prediction With Hand - Wrist Radiographscalmua1234No ratings yet
- Icu Nurse Crash CourseDocument3 pagesIcu Nurse Crash CourseSERA B.100% (2)
- 1Document4 pages1Surendra SainiNo ratings yet
- American Well Case StudyDocument4 pagesAmerican Well Case StudyAnuj ChandaNo ratings yet
- Perioperative Nursing Management Ksu 0Document35 pagesPerioperative Nursing Management Ksu 0moath qadourah100% (1)
- Health Facilities and Services Regulatory Bureau: Republic of The Philippines Department of HealthDocument23 pagesHealth Facilities and Services Regulatory Bureau: Republic of The Philippines Department of HealthChamee MallillinNo ratings yet
- Policies and Procedures On Facility Management And-Safety PDFDocument15 pagesPolicies and Procedures On Facility Management And-Safety PDFshubham solanki100% (2)
- Domain 3 - Nursing Practice and Decision Making PDFDocument15 pagesDomain 3 - Nursing Practice and Decision Making PDFLip Stick100% (1)
- PP v. Abbott - 5th Circuit Decision March 2014Document34 pagesPP v. Abbott - 5th Circuit Decision March 2014Dan McConchieNo ratings yet
- Modified Interview For Deterioration in Daily Living Activities in Dementia (IDDD)Document5 pagesModified Interview For Deterioration in Daily Living Activities in Dementia (IDDD)CristiNo ratings yet