ADHD Medications and Risk of Serious Cardiovascular Events in Young and Middle-Aged Adults
ADHD Medications and Risk of Serious Cardiovascular Events in Young and Middle-Aged Adults
Uploaded by
Gary KatzCopyright:
Available Formats
ADHD Medications and Risk of Serious Cardiovascular Events in Young and Middle-Aged Adults
ADHD Medications and Risk of Serious Cardiovascular Events in Young and Middle-Aged Adults
Uploaded by
Gary KatzOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
ADHD Medications and Risk of Serious Cardiovascular Events in Young and Middle-Aged Adults
ADHD Medications and Risk of Serious Cardiovascular Events in Young and Middle-Aged Adults
Uploaded by
Gary KatzCopyright:
Available Formats
ORIGINAL CONTRIBUTION
ONLINE FIRST
ADHD Medications and Risk
of Serious Cardiovascular Events
in Young and Middle-aged Adults
Laurel A. Habel, PhD
William O. Cooper, MD, MPH
Colin M. Sox, MD, MS
K. Arnold Chan, MD, ScD
Bruce H. Fireman, MA
Patrick G. Arbogast, PhD
T. Craig Cheetham, PharmD, MS
Virginia P. Quinn, PhD, MPH
Sascha Dublin, MD, PhD
Denise M. Boudreau, PhD, RPh
Susan E. Andrade, ScD
Pamala A. Pawloski, PharmD
Marsha A. Raebel, PharmD
David H. Smith, RPh, PhD
Ninah Achacoso, MS
Connie Uratsu, RN
Alan S. Go, MD
Steve Sidney, MD, MPH
Mai N. Nguyen-Huynh, MD, MAS
Wayne A. Ray, PhD
Joe V. Selby, MD, MPH
B
ETWEEN 2001 AND 2010, USE
of medications labeled for
treatment of attention-deficit/
hyperactivitydisorder (ADHD)
increased even more rapidly in adults
than in children.
1
According to a 2006
US Food and Drug Administration
(FDA) advisory committee briefing on
the safety of ADHDmedications, more
than 1.5 million US adults were taking
stimulants in2005, andadults received
approximately32%of all issuedprescrip-
tions.
2
The increase in ADHD diagno-
sesislikelytheprimarycauseof increased
prescribing,
3,4
althoughstimulants also
See related article.
Author Affiliations: Division of Research, Kaiser Perma-
nente Northern California, Oakland (Drs Habel, Go,
Sidney, Nguyen-Huynh, and Selby, Mr Fireman, and
Mss Achacoso and Uratsu); Department of Pediatrics
(Dr Cooper), Division of Pharmacoepidemiology, De-
partment of Preventive Medicine (Drs Cooper andRay),
and Department of Biostatistics (Dr Arbogast), Van-
derbilt University, Nashville, Tennessee; Harvard Pil-
grim Health Care Institute, Department of Popula-
tion Medicine, Harvard Medical School, Boston,
Massachusetts, and Department of Pediatrics, Bos-
ton University School of Medicine, Boston (Dr Sox);
OptumInsight Epidemiology, Waltham, Massachu-
setts (Dr Chan); Pharmacy Analytical Service, Kaiser
Permanente Southern Cal i forni a, Downy (Dr
Cheetham); Research and Evaluation Department, Kai-
ser Permanente Southern California, Pasadena (Drs
CheethamandQuinn); GroupHealthResearchInstitute,
Seattle, Washington(Drs DublinandBoudreau); Depart-
ments of Epidemiology (Dr Dublin) and Pharmacy (Dr
Boudreau), University of Washington, Seattle; Meyers
Primary Care Institute, Worcester, Massachusetts (Dr
Andrade); HealthPartners ResearchFoundation, Bloom-
ington, Minnesota (Dr Pawloski); Institute for Health
Research, Kaiser Permanente Colorado, and School of
Pharmacy, Universityof Coloradoat Denver (Dr Raebel);
Center for Health Research, Kaiser Permanente North-
west, Portland, Oregon(Dr Smith); andDepartments of
Epidemiology, Biostatistics and Medicine, University of
California, San Francisco (Dr Sidney).
Corresponding Author: Laurel A. Habel, PhD, Divi-
sion of Research, Kaiser Permanente Northern Cali-
fornia, 2000Broadway, FifthFloor, Oakland, CA94612
(laurel.habel@kp.org).
Context More than 1.5 million US adults use stimulants and other medications labeled
for treatment of attention-deficit/hyperactivity disorder (ADHD). These agents can in-
crease heart rate and blood pressure, raising concerns about their cardiovascular safety.
Objective To examine whether current use of medications prescribed primarily to
treat ADHD is associated with increased risk of serious cardiovascular events in young
and middle-aged adults.
Design, Setting, and Participants Retrospective, population-based cohort study
using electronic health care records from 4 study sites (OptumInsight Epidemiology,
Tennessee Medicaid, Kaiser Permanente California, and the HMO Research Net-
work), starting in 1986 at 1 site and ending in 2005 at all sites, with additional covar-
iate assessment using 2007 survey data. Participants were adults aged 25 through 64
years with dispensed prescriptions for methylphenidate, amphetamine, or atomox-
etine at baseline. Each medication user (n=150 359) was matched to 2 nonusers on
study site, birth year, sex, and calendar year (443 198 total users and nonusers).
Main Outcome Measures Serious cardiovascular events, including myocardial in-
farction (MI), sudden cardiac death (SCD), or stroke, with comparison between cur-
rent or new users and remote users to account for potential healthy-user bias.
Results During806182person-years of follow-up(median, 1.3years per person), 1357
cases of MI, 296 cases of SCD, and 575 cases of stroke occurred. There were 107322
person-years of current use (median, 0.33 years), with a crude incidence per 1000 person-
years of 1.34 (95% CI, 1.14-1.57) for MI, 0.30 (95% CI, 0.20-0.42) for SCD, and 0.56
(95%CI, 0.43-0.72) for stroke. The multivariable-adjusted rate ratio (RR) of serious car-
diovascular events for current use vs nonuse of ADHD medications was 0.83 (95% CI,
0.72-0.96). Among new users of ADHD medications, the adjusted RR was 0.77 (95%
CI, 0.63-0.94). The adjusted RR for current use vs remote use was 1.03 (95% CI, 0.86-
1.24); for new use vs remote use, the adjusted RR was 1.02 (95% CI, 0.82-1.28); the
upper limit of 1.28 corresponds to an additional 0.19 events per 1000 person-years at
ages 25-44 years and 0.77 events per 1000 person-years at ages 45-64 years.
Conclusions Among young and middle-aged adults, current or new use of ADHD
medications, compared with nonuse or remote use, was not associated with an in-
creased risk of serious cardiovascular events. Apparent protective associations likely
represent healthy-user bias.
JAMA. 2011;306(24):doi:10.1001/jama.2011.1830 www.jama.com
2011 American Medical Association. All rights reserved. JAMA, Published online December 12, 2011 E1
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
areapprovedfortreatment of narcolepsy
5
and may be used off-label to treat obe-
sity
6
andfatigue relatedto depression,
7
stroke,
8
ortraumaticbraininjury.
9
Adults
withADHDare commonlytreatedwith
the stimulant classes methylphenidate
andamphetamineandincreasinglywith
a nonstimulant agent, atomoxetine.
Placebo-controlled studies in chil-
dren and adults indicate that stimu-
lants and atomoxetine elevate systolic
blood pressure levels by approximately
2 to 5 mm Hg and diastolic blood pres-
sure levels by 1to3mmHg andalsolead
to increases in heart rate.
10,11
Although
theseeffects wouldbeexpectedtoslightly
increase risk for myocardial infarction
(MI), sudden cardiac death (SCD), and
stroke,
12
clinical trials have not beenlarge
enough to assess risk of these events.
In a summary fromthe FDAAdverse
Event Reporting System, cardiac arrest,
MI, andsuddenunexplaineddeathwere
among the top 50 adverse events re-
ported after use of amphetamines and
methylphenidate.
2
Although 1 study
among children suggested markedly el-
evated risks of SCD,
13
cardiovascular
safety data from pharmacoepidemio-
logic studies are limited and inconsis-
tent,
13-16
especially among adults.
17,18
The aimof this study was to examine
whether current use of medications used
primarily to treat ADHD is associated
withincreasedriskof MI, SCD, or stroke
inadults aged25through64years. Study
drugs included all agents with a labeled
indication for treatment of ADHD in
either children or adults as of Decem-
ber 31, 2005.
METHODS
The study was conducted in parallel
with a study of ADHDdrug use and se-
rious cardiovascular events in youths
aged 2 through 24 years.
19
Data Sites
Study sites included Vanderbilt Uni-
versity (Tennessee State Medicaiddata),
Kaiser Permanente (KP) California
(northern and southern KP regions),
OptumInsight Epidemiology (data from
a large health insurance plan), and the
HMO Research Network (Harvard
Pilgrim Health Care; Fallon Commu-
nity Health Plan; Group Health Coop-
erative of Puget Sound; HealthPart-
ners; KP Georgia; KP Northwest; and
KP Colorado). The selected sites pro-
vide geographic and sociodemo-
graphic diversity and have similar com-
puterized data structures.
Thestartdatefortheavailabilityofcom-
puterizeddatadifferedacrossstudysites,
ranging from 1986 to 2002. Follow-up
concludedat theendof 2005sothat mor-
talitysearches couldbeconductedusing
completestatedeathrecords andtheNa-
tional Death Index. The study was ap-
provedbytheinstitutional reviewboards
of eachparticipatinginstitutionandbythe
FDAResearchinHumanSubjects Com-
mittee. The requirement for participant
informed consent was waived.
Study Participants
Eligibleindividuals wereaged25through
64 years with at least 12 months of con-
tinuous health plan coverage and phar-
macy benefits before cohort entry (time
zero). Individuals were excluded if they
had 1 or more of the following diagno-
ses (based on International Classifica-
tion of Diseases, Ninth Revision [ICD-9]
or International Classification of Dis-
eases, Tenth Revision [ICD-10] codes)
within 365 days before cohort entry:
sickle cell disease, cancer (other than
nonmelanoma skincancer), humanim-
munodeficiency virus infection, organ
transplant, liver failure/hepatic coma,
end-stage renal disease, respiratory fail-
ure, or congestive heart failure. When
these diagnoses occurredafter cohort en-
try, follow-up time was censored.
Ateachcontributingsite, weassembled
the eligible members and periods when
all eligibility criteria were met. For each
exposedperiod(ie, at least 1ADHDpre-
scription), starting with the earliest, we
randomly selected2 unexposedperiods
fromall members withno ADHDmedi-
cation use at cohort entry and the same
sex and birth year.
Study Medications
and Exposure Categories
Medication use was based on prescrip-
tion fills from electronic pharmacy rec-
ords. ADHD medications included
stimulant-class medications (methyl-
phenidate, amphetamines, pemoline)
andatomoxetine, a selective norepineph-
rine reuptake inhibitor. Amphetamines
included dextroamphetamines and am-
phetamine salts. Although infrequently
used and not structurally similar to the
other stimulants, pemoline was in-
cluded because of its labeled indication
for ADHD. Each person-day of fol-
low-up was classified into mutually ex-
clusive exposure categories according to
ADHD drug use, based on prescription
dispensing dates and days supply.
Current use was defined as the pe-
riodbetweenprescriptionstart date and
end of days supply (including up to a
7-day carryover fromprevious prescrip-
tions). Indeterminate use was the first 89
days after end of current use. Former
use began at 90 days after end of cur-
rent use and ended at 364 days after last
current use. Greater than364days since
end of last days supply was consid-
ered remote use. Nonuse referred to per-
son-days with no current use and no
past use (back to 365 days before co-
hort entry). Past users and nonusers
could become current users during fol-
low-up; when this occurred, their per-
son-time was classified as described
above. Less than 1% of nonusers be-
came users after baseline. Current use
was further categorized based on spe-
cific medications (amphetamines,
methylphenidate, atomoxetine, mul-
tiple ADHDdrugs, or pemoline) and on
prespecified duration categories (1-30
days, 31-90 days, 91-182 days, 183-
365 days, 366 days).
We consider current use the most
etiologically relevant exposure. Risk
during current use was compared with
risk during nonuse. In addition, to ac-
count for potential selection bias or un-
measured confounding that could arise
from users being more or less healthy
than nonusers, we restricted some
analyses to ever users of ADHD medi-
cations. These analyses compared rates
during periods of current use with rates
during periods 365 days or more after
use ended(ie, remote use). These analy-
ses are less influenced by potential con-
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
E2 JAMA, Published online December 12, 2011 2011 American Medical Association. All rights reserved.
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
founders that are unmeasured and
stable over time, but analyses assume
no medication effects that remain af-
ter discontinuation.
Study End Points
Potential end points were identified
fromclaims and vital records (diagno-
ses and ICD codes provided in eTable
1, available at http://www.jama.com).
For members with death not identi-
fied from these sources and whose
health plan enrollment ended prior to
end of study period, we performed Na-
tional Death Index searches.
Medical records, including hospital-
izations, reports fromemergency medi-
cal services, autopsies, and death cer-
tificates, were requested for all potential
SCDs (n=411) andstrokes (n=980) and
for a random 31% sample of potential
MIs (n=433) for assessment by trained
adjudicators (primarycare physicians for
MI and SCD, neurologists for stroke).
Of the 371 MI cases with sufficient
records available, 353 (95%) were con-
firmed by adjudication. Myocardial in-
farction was defined as an acute event
involving hospitalization with charac-
teristic changes in cardiac enzyme lev-
els and either symptoms or character-
istic electrocardiographic changes.
20,21
Sudden cardiac death was definedas wit-
nessed sudden death in a community
setting, preceded by typical symp-
toms of cardiac ischemia. Deaths were
excluded when documentation sug-
gested a noncardiac cause (eg, motor
vehicle crash) or if clinically severe
heart disease was present and sudden
cardiac death was not unexpected (eg,
end-stage congestive heart failure).
Stroke was defined as an acute neuro-
logic deficit of sudden onset that per-
sisted more than 24 hours, corre-
sponded to a vascular territory, and was
not explained by other causes such as
trauma, infection, vasculitis, extracra-
nial hemorrhage leading to hypoten-
sion, or profoundhypotensionfroman-
other cause. Strokes that occurred
during a hospitalizationwere excluded.
All MIs, other than those deter-
mined by adjudication to be noncases
(n=18), were included in analyses. For
potential SCD cases without available
or adequate hospital or autopsy rec-
ords (n=203), we used an ICD-9/
ICD-10 codebased definition with a
previously reported positive predic-
tive value of 86%.
22
SCDcases based on
the code-based definition (n=157), as
well as those confirmed by clinical ad-
judication (n=139), were included in
primary analyses. For potential strokes
with insufficient hospital or autopsy
records for clinical adjudication
(n=179) or for which records were un-
available (n=69), we used a code-
based definition to identify probable
strokes. Probable strokes had ICD-9/
ICD-10 codes with a positive predic-
tive value of 80% or greater, based on
those strokes for which records were
available. Strokes confirmed by adju-
dication (n=451) and those with in-
sufficient records meeting the diagnos-
tic codebaseddefinition(n=124) were
included as events in primary analy-
ses (eTable 2A and B). In secondary
analyses, we included all electroni-
cally identified SCDs or strokes ex-
cept those confirmed as nonevents by
adjudication.
Confounders
To control for potential differences in
cardiovascular disease (CVD) risk be-
tween exposed and unexposed indi-
viduals, we constructed a summary car-
diovascular risk score (CRS).
23,24
The
CRS was based on inpatient and out-
patient diagnoses (from claims or
encounter databases) and pharmacy
records and included CVD and medi-
cations, mental health conditions
(excluding ADHD) and use of psycho-
tropic medications, other health con-
ditions (eg, diabetes mellitus, obesity,
smoking-related) and medications, and
health care utilization (TABLE 1 and
eTable 3).
For each end point (MI, SCD, stroke,
or any serious cardiovascular event), a
separate score was created froma Pois-
son regression model among all pa-
tients, adjusted for ADHD medica-
tions and matching variables (age, sex,
data site, calendar year at cohort en-
try). The score was the linear predic-
tor from the coefficients of the result-
ing regression model, excluding the
coefficients for ADHDmedications and
the matching variables.
Inprimary analyses, several CRS vari-
ables not thought to be on the causal
pathway between medication use and
our outcomes were treatedas time vary-
ing (eTable 3). In secondary analyses,
all CRS variables were based on diag-
noses or medication use in the 365 days
prior to cohort entry and fixed at base-
line. For the new-user analyses, we used
the CRS for comparisons of current vs
remote use and constructed a propen-
sity score
25
for current vs nonuse of
ADHD medications at cohort entry,
using variables included in the CRS.
Unmeasured Confounders
To examine the possible extent and di-
rection of unmeasured confounding by
risk factors for CVD on which infor-
mation was not or was inconsistently
available in the electronic health care
records, we conductedsensitivity analy-
ses using information on potential con-
founders from 2 sources. Race/
ethnicity, smoking, obesity, history of
CVD, and drug abuse were obtained
from the adjudicated records of MI,
SCD, andstroke cases. Inaddition, race/
ethnicity, income, education, smok-
ing, obesity, and family history of CVD
were available for approximately
200 000 KP Northern California mem-
bers aged 25 through 64 years who
completed a mailed survey for a differ-
ent study in 2007 (eMethods). Elec-
tronic pharmacy records for ADHD
medications were obtained for survey
participants.
We used multivariable logistic re-
gression to examine the association be-
tween potential confounders (from
either survey or chart reviews) and use
of ADHDmedications. For variables as-
sociated with use of ADHD medica-
tions, we assessedthe extent of their po-
tential confounding effect on rate ratios
(RRs) for MI, SCD, or stroke associ-
ated withADHDmedications, using ex-
ternal adjustment methods.
26-28
This ap-
proachassumedthat associations inour
study population were similar to those
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
2011 American Medical Association. All rights reserved. JAMA, Published online December 12, 2011 E3
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
in our external samples and did not ad-
dress joint confounding by several un-
measured covariates.
Statistical Analysis
Follow-up began at cohort entry and
endedat 1 of the 4 endpoints (MI, SCD,
stroke, or any of these serious cardio-
vascular events), death, end of insur-
ance coverage or pharmacy benefit, day
before 65thbirthday, or endof study pe-
riod (December 2005), whichever came
first. Poisson regression was used to es-
timate the association of ADHD medi-
cation use with risk of serious cardio-
vascular events, while adjusting for
potentially confounding variables. Co-
variates inthe full model includedstudy
site, age (5-year dummy categories), sex,
calendar year (1986-1992, 1993-1999,
2000-2001, 2002-2003, 2004-2005), and
CRS (specified as decile dummies).
Matching variables (site, age, sex, cal-
endar year at cohort entry) were in-
cluded in the full model because,
althoughmatchingensuredbalance with
respect to these variables at baseline, it
didnot ensure balance duringfollow-up.
To minimize biases related to under-
ascertainment of events occurring early
in therapy,
29
we also conducted analy-
ses restricted to new users of ADHD
medications (no use in the year prior
to baseline). In these analyses, risk dur-
ing periods of current use was com-
pared with risk during periods remote
from last use. Current use among new
users also was compared with nonuse
(in their matches).
To examine whether associations
could be influenced by prior disease
conditions, we conducted subgroup
analyses. In one analysis, users were re-
stricted to those with a prior diagnosis
of ADHDand compared with matched
nonusers. Additional subgroups were
based on prior CVD, prior non-ADHD
psychiatric diagnoses or medicationuse,
age (25-44 vs 45-64 years) during fol-
low-up, and data site.
When examining rates of any seri-
ous cardiovascular event in the full co-
hort, we had 80% power to detect RRs
of 1.23 for current use vs nonuse and
1.30 for current use vs remote use. In
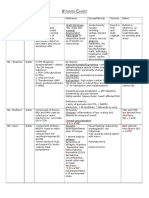
Table 1. Selected Characteristics of Study Cohort at Baseline
a
Characteristic Current Use Nonuse
No. of unique individuals 150 359 292 839
No. of membership periods
b
152 852 293 749
Year of cohort entry, median 2003 2003
Person-years during follow-up
c
107 322 533 540
Demographic and Clinical
Demographics
Age, median (IQR), y 42 (34-49) 42 (34-49)
Male sex 70 245 (46.0) 135 002 (46.0)
Medicaid enrollment 14 786 (9.7) 29 171 (9.9)
ADHD medication
Amphetamines 57 824 (37.8)
Methylphenidate 70 923 (46.4)
Atomoxetine 19 283 (12.6)
Pemoline 3973 (2.6)
Multiple 849 (0.6)
Cardiovascular disease within past year
d
Acute MI 340 (0.2) 689 (0.2)
Ischemia 3998 (2.6) 6857 (2.3)
Coronary revascularization 253 (0.2) 643 (0.2)
Congestive heart failure 1112 (0.7) 1759 (0.6)
Arrhythmia 3560 (2.3) 5076 (1.7)
Stroke/transient ischemic attack 1826 (1.2) 2075 (0.7)
Congenital heart disorder 331 (0.2) 556 (0.2)
Coronary artery anomaly 66 (0.0) 89 (0.0)
Peripheral vascular disease 1225 (0.8) 1651 (0.6)
Hypertension 22 562 (14.8) 39 011 (13.3)
Hyperlipidemia
e
28 613 (18.7) 42 601 (14.5)
Mental health claims within past year
ADHD 46 356 (30.3) 455 (0.2)
Major depression 61 417 (40.2) 23 296 (7.9)
Bipolar disorder 11 196 (7.3) 2682 (0.9)
Anxiety 30 472 (19.9) 15 670 (5.3)
Psychotic disorders 2494 (1.6) 1833 (0.6)
Other selected medical conditions within past year
Diabetes
e
8972 (5.9) 15 862 (5.4)
Obesity 9119 (6.0) 11 439 (3.9)
Smoking 11 579 (7.6) 14 717 (5.0)
Alcohol/substance abuse 7965 (5.2) 4514 (1.5)
Suicide attempt 795 (0.5) 410 (0.1)
Injury 30 655 (20.1) 37 559 (12.8)
Seizure 3062 (2.0) 2854 (1.0)
Asthma 11 627 (7.6) 12 432 (4.2)
Use of cardiovascular drug within past year
d
Loop diuretic 4328 (2.8) 4932 (1.7)
Digoxin 587 (0.4) 1130 (0.4)
Nitrates 1941 (1.3) 3298 (1.1)
Anticoagulant 1768 (1.2) 2421 (0.8)
Platelet inhibitor 996 (0.7) 1675 (0.6)
Antiarrhythmic agents 556 (0.4) 631 (0.2)
ACE inhibitor 10 719 (7.0) 19 796 (6.7)
Angiotensin receptor blocker 3652 (2.4) 5988 (2.0)
-Blocker 12 431 (8.1) 19 091 (6.5)
Calcium-channel blocker 7028 (4.6) 12 233 (4.2)
Thiazide diuretic 12 471 (8.2) 20 008 (6.8)
Other antihypertensive 1668 (1.1) 2192 (0.7)
(continued)
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
E4 JAMA, Published online December 12, 2011 2011 American Medical Association. All rights reserved.
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
new-user analyses, the least detectable
RRs were 1.31 for current use vs non-
use and 1.38 for current vs remote use.
All analyses were performed using
SAS version 9.1. For all RR estimates,
95% confidence limits were reported.
RESULTS
The study included a total of 443 198
adults, of whom150 359 were users of
ADHD medications at baseline. Meth-
ylphenidate accounted for 45%of cur-
rent use; amphetamine, for 44%; ato-
moxetine, for 8%; andpemoline, for 3%.
Characteristics of Study Population
Baseline characteristics of users and
nonusers are reported in Table 1; char-
acteristics of person-time by medica-
tion use are reported in eTable 3. Car-
diovascular diseases were generally
uncommon and similar or modestly
more prevalent in users than nonus-
ers. As expected, ADHD was substan-
tially more common among current us-
ers than nonusers. This also was true
for other psychiatric conditions. The
prevalences of cardiovascular risk fac-
tors were modestly higher during pe-
riods of remote use than during peri-
ods of current use or nonuse.
Number of Events and RRs
in the Full Cohort
During 806 182 person-years of fol-
low-up (median, 1.3 [interquartile
range, 0.6-2.6] years per person), 1357
cases of MI, 296 cases of SCD, and 575
cases of stroke occurred. There were
107 322 person-years of current use
(median, 0.33 [range, 0.0-13.5] years
per user), with a crude incidence per
1000 person-years of 1.34 (95% CI,
1.14-1.57) for MI, 0.30 (95%CI, 0.20-
0.42) for SCD, and 0.56 (95%CI, 0.43-
0.72) for stroke.
In analysis adjusted for matching
variables only, the RR of MI, SCD, or
stroke for current vs nonuse of ADHD
medications was 0.97 (95% CI, 0.84-
1.12). After also adjusting for the CRS,
the RR was modestly lower (0.83 [95%
CI, 0.72-0.96]). Results were similar for
specific medications and across end
points (FIGURE 1 and eTable 4). Rate
ratios also were similar for ischemic or
hemorrhagic stroke (eTable 5Aand B).
Findings for SCD and stroke changed
only minimally when all electroni-
cally identified cases were included ex-
cept those adjudicated as noncases
(eTable 6Aand B). Overall results were
essentially unchanged when all vari-
ables in the CRS were fixed at baseline
(eTable 7).
Table 1. Selected Characteristics of Study Cohort at Baseline
a
(continued)
Characteristic Current Use Nonuse
Demographic and Clinical (cont.)
Use of psychotropic medications within past year
Antipsychotic, any 14 618 (9.6) 5371 (1.8)
Tricyclic antidepressant 14 224 (9.3) 9907 (3.4)
Antidepressants, other or SSRI/SNRI 81 639 (53.4) 36 962 (12.6)
Benzodiazepines 43 695 (28.6) 25 956 (8.8)
Lithium 4177 (2.7) 1002 (0.3)
Modafinil 4732 (3.1) 383 (0.1)
Insomnia medications 15 270 (10.0) 6732 (2.3)
Thioridazine 307 (0.2) 181 (0.1)
Mood stabilizers, without seizure 22 426 (14.7) 8631 (2.9)
Clonidine/guanfacine, without hypertension 2000 (1.3) 659 (0.2)
Use of other selected medications within past year
-Agonist 18 971 (12.4) 20 835 (7.1)
Epinephrine 1342 (0.9) 1274 (0.4)
Asthma medications, other 39 645 (25.9) 45 102 (15.4)
Seizure medications, any 24 139 (15.8) 10 397 (3.5)
Theophylline compounds (asthma medication) 960 (0.6) 1200 (0.4)
COX-2 inhibitors 10 666 (7.0) 10 838 (3.7)
Other drugs to improve blood flow 216 (0.1) 250 (0.1)
Clonidine 2602 (1.7) 1787 (0.6)
Phosphodiesterase type 5 inhibitors 5183 (3.4) 4504 (1.5)
Triptans 7164 (4.7) 5298 (1.8)
Oral contraceptives 18 379 (12.0) 28 590 (9.7)
Hormones, menopausal 18 026 (11.8) 23 388 (8.0)
Health Care Utilization Within Past Year
Cardiovascular visits
Emergency, 1 5728 (3.7) 7697 (2.6)
Inpatient, 1 6022 (3.9) 7130 (2.4)
Physician, 1-4 43 474 (28.4) 65 256 (22.2)
Physician, 5 13 242 (8.7) 17 713 (6.0)
Psychiatric visits
f
Emergency, 1 4417 (2.9) 2897 (1.0)
Inpatient, 1 7761 (5.1) 3827 (1.3)
Physician, 1-4 43 538 (28.5) 26 703 (9.1)
Physician, 5 40 176 (26.3) 11 048 (3.8)
Other visits
Emergency, 1 7885 (5.2) 9594 (3.3)
Inpatient, 1 5812 (3.8) 5595 (1.9)
Physician, 1 55 386 (36.2) 69 134 (23.5)
No. of different medications
g
1 24 309 (15.9) 61 193 (20.8)
2 108 955 (71.3) 116 680 (39.7)
Abbreviations: ACE, angiotensin-converting enzyme; ADHD, attention-deficit/hyperactivity disorder; COX-2, cyclooxy-
genase 2; IQR, interquartile range; MI, myocardial infarction; SNRI, serotonin and norepinephrine reuptake inhibitor;
SSRI, selective serotonin reuptake inhibitor.
a
Data are presented as No. (%) unless otherwise indicated.
b
All variables in table included in cardiovascular risk score, except demographics and ADHD. Percentages are based
on membership periods. There were 299 indeterminate and former users at baseline.
c
Follow-up time based on combined end point (MI, sudden cardiac death, or stroke).
d
Variables used to define history of cardiovascular disease for subgroup analyses in Figure 2.
e
Including medications.
f
Excluding ADHD visits.
g
Excluding ADHD medications.
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
2011 American Medical Association. All rights reserved. JAMA, Published online December 12, 2011 E5
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
Analyses Restricted to Users
of ADHD Medications
(Remote Use Comparison)
Among ever users of ADHD medica-
tions, the adjusted RR of serious car-
diovascular events was nearly the same
during periods of current use as dur-
ing follow-up periods more than 1 year
after use ended(RR, 1.03[95%CI, 0.86-
1.24]) (TABLE 2). This 1.24 estimated
upper bound for the RR would corre-
spond to an absolute risk difference of
0.17 serious cardiovascular events per
1000 person-years in adults aged 25
through 44 years (ages at which the ab-
solute risk was only 0.87 per 1000 per-
son-years) and of 0.68 serious cardio-
vascular events per 1000 person-years
in adults aged 45 through 64 years
(ages at which the absolute risk dur-
ing current use was 3.5 per 1000 per-
son-years).
New-User Analyses
In the new-user cohort, baseline char-
acteristics of newusers of ADHDmedi-
cation were generally similar to charac-
teristics of all ADHD medication users
(eTable 8). Cardiovascular diseases were
similar or slightly more prevalent innew
users than nonusers. ADHD and other
psychiatric conditions were substan-
tially more common in new users than
in nonusers. In the new-user analyses,
RRs for current vs remote use were close
to 1.0 for MI, stroke, and the combined
end point (TABLE 3). Although not sta-
tistically significant, RRs for methylphe-
nidate were 1.26(95%CI, 0.88-1.80) for
MI, 1.44 (95%CI, 0.90-2.30) for stroke,
and 1.20 (95% CI, 0.91-1.59) for the
combinedendpointsomewhat higher
than the RRs for the other drugs.
For the combinedendpoint, there was
no pattern of increasing risk with in-
creasing duration of current use or for
any windowof time. For current use (all
durations combined) vs remote use, the
RRfor the combinedendpoint was 1.02.
The upper boundof the CI was 1.28; this
would amount to an additional 0.19
events per 1000 person-years at ages 25
through44 years and anadditional 0.77
events per 1000 person-years at ages 45
through 64 years.
Subgroup Analyses
Rate ratios were similar in all sub-
group analyses (FIGURE 2 and eTable
9). Although we did observe differ-
ences in event rates, cohort character-
istics, and RRs by data site, RRs for
current use were not statistically sig-
nificantly elevated at any site (eTables
10, 11, and 12).
Sensitivity Analyses
Unmeasured Confounding
Informationfromreviewof medical rec-
ords of MI, SCD, and stroke cases and
the external survey population sug-
gestedthat several factors (obesity, smok-
ing, family history of CVD) were not or
were only very weakly associated with
use of ADHD medications and there-
Figure 1. Adjusted Rate Ratios for Serious Cardiovascular Events Associated With Use vs
Nonuse of ADHD Medications
Lower Risk Higher Risk
0.2 5.0 1.0
Rate Ratio (95% CI)
No. of
Events
Outcome and ADHD
Medication Use Person-Years
Rate Ratio
(95% CI)
MI
152 Current use 113 324.2 0.88 (0.74-1.05)
86 Indeterminate use 53 896.7 1.07 (0.85-1.33)
65 Former use 47 858.5 0.78 (0.61-1.00)
147 Remote use 69 792.9 0.82 (0.68-0.97)
907 Nonuse 559 743.1 1 [Reference]
59 Amphetamines 49 080.1 0.92 (0.70-1.19)
77 Methylphenidate 51 232.8 0.89 (0.71-1.13)
11 Atomoxetine 8424.8 0.87 (0.48-1.57)
5 Pemoline 3047.3 0.71 (0.29-1.71)
0 Multiple 1539.1 NA
0.2 5.0 1.0
Rate Ratio (95% CI)
SCD
32 Current use 107 525.0 0.80 (0.55-1.18)
14 Indeterminate use 51 814.0 0.73 (0.42-1.26)
20 Former use 46 263.5 0.90 (0.57-1.44)
50 Remote use 68 102.6 0.98 (0.71-1.35)
180 Nonuse 535 515.5 1 [Reference]
13 Amphetamines 46 910.0 0.93 (0.52-1.63)
13 Methylphenidate 47 887.1 0.67 (0.38-1.18)
4 Atomoxetine 8257.6 1.04 (0.38-2.82)
2 Pemoline 2995.7 1.08 (0.27-4.37)
0 Multiple 1474.5 NA
0.2 5.0 1.0
Rate Ratio (95% CI)
Stroke
63 Current use 111 935.5 0.76 (0.58-1.00)
31 Indeterminate use 53 327.8 0.83 (0.57-1.19)
39 Former use 47 333.0 1.01 (0.73-1.41)
67 Remote use 69 202.3 0.82 (0.63-1.07)
375 Nonuse 553 458.5 1 [Reference]
19 Amphetamines 48 672.9 0.63 (0.40-1.01)
39 Methylphenidate 50 332.3 0.94 (0.68-1.32)
3 Atomoxetine 8371.1 0.44 (0.14-1.38)
2 Pemoline 3030.1 0.59 (0.15-2.39)
0 Multiple 1529.2 NA
0.2 5.0 1.0
Rate Ratio (95% CI)
MI, SCD, or stroke
234 Current use 107 322.4 0.83 (0.72-0.96)
125 Indeterminate use 51 709.6 0.94 (0.78-1.13)
121 Former use 46 120.8 0.86 (0.72-1.04)
243 Remote use 67 489.0 0.81 (0.70-0.93)
1391 Nonuse 533 540.4 1 [Reference]
88 Amphetamines 46 826.5 0.85 (0.68-1.05)
120 Methylphenidate 47 792.3 0.87 (0.72-1.04)
17 Atomoxetine 8248.2 0.74 (0.46-1.19)
9 Pemoline 2985.2 0.75 (0.39-1.45)
0 Multiple 1470.1 NA
Rate ratios are adjusted for site, age, sex, calendar year, and cardiovascular risk score (some variables
within score are time varying). ADHD indicates attention-deficit/hyperactivity disorder; MI, myocardial
infarction; NA, not applicable; SCD, sudden cardiac death.
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
E6 JAMA, Published online December 12, 2011 2011 American Medical Association. All rights reserved.
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
fore were unlikely to be important con-
founders. However, in these data, users
of ADHD medications more often had
some college education compared with
nonusers (17% vs 10%, adjusting for
age). Inaddition, 5%of the stimulant us-
ers were black or Hispanic vs 12%of the
nonusers. If similar patterns for race/
ethnicity and education were also pre-
sent in our full study cohort, and if each
of these characteristics independently
multiplied the risk of serious cardiovas-
cular events by 2.4, thenthese 2 unmea-
sured factors would yield a healthy-
user bias substantial enough to account
for an apparent RR of 0.83 (as in our
comparison of current use vs nonuse),
given a true RR of 1.0.
COMMENT
Inour population-based cohort of more
than 440 000 young and middle-aged
adults, including more than150000 us-
ers of ADHD medications identified
through filled prescriptions, we found
no evidence of an increased risk of MI,
SCD, or stroke associated with cur-
rent use compared with nonuse or re-
Table 2. Adjusted Rate Ratios for Serious Cardiovascular Events Associated With Periods of Current Use of Attention-Deficit/Hyperactivity
Disorder Medications vs Periods Remote From Last Use
Medication Status Person-Years
No. of
Events
Rate/1000
Person-Years
RR (95% CI)
Unadjusted
Adjusted
Matching-Variables
a
Adjusted
b
MI
Current use 113 324.2 152 1.34 0.64 (0.51-0.80) 0.98 (0.78-1.23) 1.08 (0.86-1.36)
Amphetamines 49 080.1 59 1.20 0.57 (0.42-0.77) 0.99 (0.73-1.34) 1.12 (0.83-1.52)
Methylphenidate 51 232.8 77 1.50 0.71 (0.54-0.94) 1.00 (0.76-1.32) 1.10 (0.83-1.45)
Atomoxetine 8424.8 11 1.31 0.62 (0.34-1.14) 0.99 (0.54-1.84) 1.06 (0.57-1.96)
Pemoline 3047.3 5 1.64 0.78 (0.32-1.90) 0.87 (0.36-2.13) 0.87 (0.36-2.12)
Multiple 1539.1 0 0.00 NA NA NA
Indeterminate use 53 896.7 86 1.60 0.76 (0.58-0.99) 1.19 (0.91-1.56) 1.31 (1.00-1.71)
Former use 47 858.5 65 1.36 0.64 (0.48-0.86) 0.92 (0.68-1.23) 0.96 (0.71-1.28)
Remote use 69 792.9 147 2.11 1 [Reference] 1 [Reference] 1 [Reference]
SCD
c
Current use 107 525.0 32 0.30 0.41 (0.26-0.63) 0.79 (0.50-1.24) 0.82 (0.52-1.29)
Amphetamines 46 910.0 13 0.28 0.38 (0.21-0.69) 0.85 (0.46-1.58) 0.94 (0.51-1.76)
Methylphenidate 47 887.1 13 0.27 0.37 (0.20-0.68) 0.66 (0.36-1.23) 0.68 (0.37-1.27)
Atomoxetine 8257.6 4 0.48 0.66 (0.24-1.83) 1.14 (0.41-3.18) 1.06 (0.38-2.95)
Pemoline 2995.7 2 0.67 0.91 (0.22-3.74) 1.11 (0.27-4.59) 1.10 (0.27-4.56)
Multiple 1474.5 0 0.00 NA NA NA
Indeterminate use 51 814.0 14 0.27 0.37 (0.20-0.67) 0.70 (0.39-1.28) 0.74 (0.41-1.35)
Former use 46 263.5 20 0.43 0.59 (0.35-0.99) 0.94 (0.56-1.58) 0.92 (0.55-1.55)
Remote use 68 102.6 50 0.73 1 [Reference] 1 [Reference] 1 [Reference]
Stroke
d
Current use 111 935.5 63 0.56 0.58 (0.41-0.82) 0.90 (0.63-1.28) 0.93 (0.65-1.31)
Amphetamines 48 672.9 19 0.39 0.40 (0.24-0.67) 0.70 (0.42-1.18) 0.77 (0.46-1.29)
Methylphenidate 50 332.3 39 0.77 0.80 (0.54-1.19) 1.15 (0.77-1.72) 1.15 (0.77-1.72)
Atomoxetine 8371.1 3 0.36 0.37 (0.12-1.18) 0.55 (0.17-1.75) 0.54 (0.17-1.71)
Pemoline 3030.1 2 0.66 0.68 (0.17-2.78) 0.74 (0.18-3.04) 0.72 (0.18-2.96)
Multiple 1529.2 0 0.00 NA NA NA
Indeterminate use 53 327.8 31 0.58 0.60 (0.39-0.92) 0.96 (0.63-1.48) 1.01 (0.65-1.54)
Former use 47 333.0 39 0.82 0.85 (0.57-1.26) 1.24 (0.85-1.85) 1.23 (0.83-1.83)
Remote use 69 202.3 67 0.97 1 [Reference] 1 [Reference] 1 [Reference]
MI, SCD, or stroke
c,d
Current use 107 322.4 234 2.18 0.61 (0.51-0.72) 0.96 (0.80-1.15) 1.03 (0.86-1.24)
Amphetamines 46 826.5 88 1.88 0.52 (0.41-0.67) 0.93 (0.73-1.19) 1.05 (0.82-1.34)
Methylphenidate 47 792.3 120 2.51 0.70 (0.56-0.87) 1.01 (0.81-1.26) 1.07 (0.86-1.34)
Atomoxetine 8248.2 17 2.06 0.57 (0.35-0.94) 0.90 (0.55-1.48) 0.92 (0.56-1.50)
Pemoline 2985.2 9 3.01 0.84 (0.43-1.63) 0.95 (0.49-1.85) 0.93 (0.48-1.82)
Multiple 1470.1 0 0.00 NA NA NA
Indeterminate use 51 709.6 125 2.42 0.67 (0.54-0.83) 1.09 (0.88-1.35) 1.17 (0.94-1.45)
Former use 46 120.8 121 2.62 0.73 (0.59-0.91) 1.06 (0.85-1.32) 1.07 (0.86-1.33)
Remote use 67 489.0 243 3.60 1 [Reference] 1 [Reference] 1 [Reference]
Abbreviations: MI, myocardial infarction; NA, not applicable; RR, rate ratio; SCD, sudden cardiac death.
a
Adjusted for site, age, sex, and calendar year (ie, matching variables).
b
Adjusted for site, age, sex, calendar year, and cardiovascular risk score (some variables within score are time varying).
c
Analyses excluded the 3 Health Maintenance Organization Research Network (HMORN) sites (Fallon Community, Kaiser Permanente [KP] Georgia, KP Northwest) that did not
provide data on SCD end points.
d
Analyses excluded the 2 HMORN sites (Fallon Community, KP Georgia) that did not provide data on stroke end points.
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
2011 American Medical Association. All rights reserved. JAMA, Published online December 12, 2011 E7
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
mote use of ADHD medications. We
also found little support for an in-
creased risk with any specific medica-
tion or with longer duration of cur-
rent use. Results were similar when
users were restricted to newusers. Rate
ratios did not appear to be influenced
by prior CVD or by prior non-ADHD
psychiatric conditions. They also were
similar across age groups. As ex-
pected, event rates were substantially
higher in the Medicaid population;
however, the RR for current use was
similar to that in other sites.
Our study has several limitations. Use
of ADHD medications was based on
electronic pharmacy records of filled
prescriptions. Filled prescriptions may
Table 3. Adjusted Rate Ratios for Serious Cardiovascular Events Associated With Periods of New Use of Attention-Deficit/Hyperactivity
Disorder Medications vs Periods Remote From Last Use
Medication Status Person-Years
No. of
Events
Rate/1000
Person-Years
RR (95% CI)
Unadjusted
Adjusted
Matching-Variables
a
Adjusted
b
MI
Current use 55 533.9 77 1.39 0.67 (0.50-0.89) 1.04 (0.77-1.39) 1.08 (0.81-1.45)
Amphetamines 23 265.6 24 1.03 0.50 (0.32-0.77) 0.86 (0.55-1.34) 0.94 (0.60-1.46)
Methylphenidate 23 930.8 42 1.76 0.84 (0.59-1.20) 1.23 (0.86-1.75) 1.26 (0.88-1.80)
Atomoxetine 6475.3 9 1.39 0.67 (0.34-1.31) 1.06 (0.54-2.10) 1.06 (0.54-2.10)
Pemoline 1114.4 2 1.79 0.86 (0.21-3.49) 0.76 (0.19-3.07) 0.75 (0.18-3.03)
Multiple 747.7 0 0.00 NA NA NA
Duration, d
c
1-30 7526.3 11 1.46 0.70 (0.38-1.30) 1.26 (0.68-2.33) 1.31 (0.70-2.43)
31-90 9656.8 11 1.14 0.55 (0.29-1.01) 1.01 (0.54-1.88) 1.06 (0.57-1.96)
91-182 9556.3 8 0.84 0.40 (0.20-1.47) 0.71 (0.35-1.47) 0.75 (0.36-1.53)
183-365 11 221.9 16 1.43 0.68 (0.41-1.15) 1.13 (0.67-1.92) 1.19 (0.70-2.01)
366 16 425.2 29 1.77 0.85 (0.56-1.27) 1.09 (0.72-1.64) 1.15 (0.76-1.73)
Indeterminate use 31 090.0 52 1.67 0.80 (0.58-1.11) 1.27 (0.92-1.77) 1.32 (0.95-1.84)
Former use 35 087.7 55 1.57 0.75 (0.55-1.04) 1.08 (0.78-1.49) 1.08 (0.78-1.49)
Remote use 55 194.2 115 2.08 1 [Reference] 1 [Reference] 1 [Reference]
SCD
d
Current use 52 203.2 15 0.29 0.34 (0.19-0.62) 0.61 (0.34-1.09) 0.62 (0.34-1.11)
Amphetamines 22 002.7 3 0.14 0.16 (0.05-0.53) 0.34 (0.11-1.10) 0.38 (0.12-1.22)
Methylphenidate 22 056.6 8 0.36 0.43 (0.20-0.92) 0.70 (0.33-1.50) 0.69 (0.32-1.46)
Atomoxetine 6348.4 3 0.47 0.57 (0.18-1.82) 0.95 (0.29-3.09) 0.90 (0.28-2.91)
Pemoline 1091.6 1 0.92 1.10 (0.15-7.96) 0.90 (0.12-6.63) 0.93 (0.13-6.77)
Multiple 703.9 0 0.00 NA NA NA
Duration, d
c
1-30 7217.4 2 0.28 0.33 (0.08-1.37) 0.67 (0.16-2.79) 0.68 (0.16-2.81)
31-90 9195.9 2 0.22 0.26 (0.06-1.07) 0.56 (0.13-2.30) 0.56 (0.14-2.33)
91-182 9026.0 4 0.44 0.53 (0.19-2.30) 1.09 (0.39-3.04) 1.11 (0.40-3.10)
183-365 10 511.3 1 0.10 0.11 (0.02-0.83) 0.22 (0.03-1.59) 0.22 (0.03-1.62)
366 15 129.8 5 0.33 0.40 (0.16-1.00) 0.57 (0.22-1.43) 0.57 (0.22-1.43)
Indeterminate use 29 752.7 13 0.44 0.52 (0.28-0.97) 0.94 (0.50-1.75) 0.96 (0.52-1.79)
Former use 33 877.6 16 0.47 0.57 (0.32-1.00) 0.89 (0.50-1.57) 0.88 (0.50-1.56)
Remote use 53 926.6 45 0.83 1 [Reference] 1 [Reference] 1 [Reference]
Stroke
e
Current use 54 569.3 41 0.75 0.73 (0.49-1.10) 1.10 (0.73-1.65) 1.09 (0.72-1.64)
Amphetamines 22 965.2 10 0.44 0.43 (0.22-0.83) 0.72 (0.37-1.41) 0.77 (0.39-1.53)
Methylphenidate 23 335.7 26 1.11 1.09 (0.68-1.73) 1.53 (0.96-2.45) 1.44 (0.90-2.30)
Atomoxetine 6429.4 3 0.47 0.46 (0.14-1.46) 0.66 (0.20-2.11) 0.64 (0.20-2.04)
Pemoline 1099.7 2 1.82 1.78 (0.43-7.28) 1.48 (0.36-6.08) 1.39 (0.34-5.72)
Multiple 739.3 0 0.00 NA NA NA
Duration, d
c
1-30 7421.0 4 0.54 0.53 (0.19-6.08) 0.93 (0.34-2.57) 0.92 (0.33-2.53)
31-90 9511.8 6 0.63 0.62 (0.27-1.43) 1.10 (0.47-2.57) 1.08 (0.46-2.51)
91-182 9398.0 9 0.96 0.94 (0.46-1.89) 1.59 (0.78-3.23) 1.55 (0.76-3.14)
183-365 11 018.6 4 0.36 0.35 (0.13-0.98) 0.56 (0.20-1.55) 0.55 (0.20-1.53)
366 16 087.6 16 0.99 0.97 (0.56-1.69) 1.19 (0.68-2.09) 1.21 (0.69-2.11)
Indeterminate use 30 657.1 20 0.65 0.64 (0.38-1.06) 1.00 (0.60-1.66) 1.0 (0.60-1.67)
Former use 34 644.6 26 0.75 0.73 (0.46-1.17) 1.05 (0.66-1.68) 1.04 (0.65-1.65)
Remote use 54 702.5 56 1.02 1 [Reference] 1 [Reference] 1 [Reference]
(continued)
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
E8 JAMA, Published online December 12, 2011 2011 American Medical Association. All rights reserved.
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
not represent medications actually con-
sumed, and days supply may not rep-
resent actual periods of use. Nonethe-
less, electronic pharmacy databases
have beenfound to be excellent sources
of information on drug use.
30
We did
not obtaindose data andtherefore could
not examine if risk varied by this fac-
tor. Although we used a strict defini-
tion of current use, minimizing mis-
classification of this exposure, we had
limited ability to assess medication ad-
herence using standard definitions. De-
spite its large size, the study had only
moderate power for several compari-
sons, including current vs remote use
in the new-user analyses and in com-
parisons for individual drugs. The study
did not include adults 65 years and
older; therefore, results cannot be gen-
eralized to this age group.
We reviewed medical records and
death certificates to confirm SCD and
stroke diagnoses. However, records
were unavailable for some of our elec-
tronically identified cases. We used an
ICD-9/ICD-10 codebased definition
for these cases, and misclassification
of some cases may have occurred. If
nondifferential with respect to ADHD
medication use, this misclassification
would bias RRs toward the null.
The accuracy of ADHDdiagnoses in
adults from claims and encounter da-
tabases is limited. However, previous
studies have validated ICD 9/ICD-10
codebased definitions of many impor-
tant covariates, including diabetes, con-
gestive heart failure, peripheral vascu-
lar disease, and hypertension, reporting
positive predictive values exceeding
90% for each condition.
31-33
Although
we adjusted for numerous established
and potential cardiovascular risk fac-
tors, there were some factors, primar-
ily psychiatric conditions and medica-
tions, for which the prevalence was
substantial in users of ADHD medica-
tions but rare innonusers. Thus, we had
limited ability to adjust for these vari-
ables. Important residual confound-
ing by psychiatric conditions and medi-
cations seems unlikely, because most
are not established risk factors for CVD,
they were not or were only modestly re-
lated to risk in our cohort, and results
were similar when we restricted analy-
ses to participants withor to those with-
out these psychiatric conditions or
medication use.
There appears to be a modest amount
of healthy-user bias influencing our RR
comparisons of current use vs nonuse.
Results are less prone to this bias when
analyses are restricted to ever users of
ADHD medications, and we compared
periods of current use withfollow-uppe-
riods remote from use. In these com-
parisons, the RR for serious cardiovas-
cular events was 1.03 in the full cohort
and 1.02 in new users, indicating that
the incidence of these events while cur-
rently receiving ADHD medications is
similar to the incidence during periods
while not receiving these medications.
In sensitivity analyses, we saw evi-
dence for 2 potential sources of a mod-
est amount of healthy-user bias: a higher
percentage of users were white and col-
lege educated.
Clinical trials have provided limited
informationonthe cardiovascular safety
of ADHD medications, primarily be-
cause these trials have been too small to
evaluate serious events suchas MI, SCD,
or stroke.
34,35
Postmarketing surveil-
lance data from the Adverse Event Re-
porting System
2
and from the National
Electronic Injury Surveillance System
36
have suggested a potential elevation in
Table 3. Adjusted Rate Ratios for Serious Cardiovascular Events Associated With Periods of New Use of Attention-Deficit/Hyperactivity
Disorder Medications vs Periods Remote From Last Use (continued)
Medication Status Person-Years
No. of
Events
Rate/1000
Person-Years
RR (95% CI)
Unadjusted
Adjusted
Matching-Variables
a
Adjusted
b
MI, SCD, or stroke
d,e
Current use 52 094.6 125 2.40 0.65 (0.52-0.81) 1.00 (0.80-1.26) 1.02 (0.82-1.28)
Amphetamines 21 955.8 37 1.69 0.46 (0.32-0.65) 0.80 (0.56-1.13) 0.87 (0.61-1.23)
Methylphenidate 22 008.8 69 3.14 0.85 (0.65-1.12) 1.22 (0.92-1.60) 1.20 (0.91-1.59)
Atomoxetine 6340.4 14 2.21 0.60 (0.35-1.03) 0.93 (0.54-1.60) 0.91 (0.53-1.56)
Pemoline 1088.1 5 4.60 1.25 (0.51-3.03) 1.07 (0.44-2.61) 1.02 (0.42-2.49)
Multiple 701.4 0 0.00 NA NA NA
Duration, d
c
1-30 7215.7 16 2.22 0.60 (0.36-1.00) 1.08 (0.65-1.80) 1.10 (0.66-1.83)
31-90 9191.7 19 2.07 0.56 (0.35-0.90) 1.04 (0.65-1.66) 1.05 (0.66-1.69)
91-182 9018.3 18 2.00 0.54 (0.33-0.88) 0.96 (0.59-1.55) 0.97 (0.60-1.57)
183-365 10 494.1 20 1.91 0.52 (0.33-0.82) 0.85 (0.53-1.34) 0.86 (0.54-1.37)
366 15 055.5 47 3.12 0.85 (0.62-1.16) 1.06 (0.77-1.46) 1.10 (0.80-1.51)
Indeterminate use 29 694.2 82 2.76 0.75 (0.58-0.97) 1.19 (0.92-1.55) 1.22 (0.94-1.58)
Former use 33 774.3 97 2.87 0.78 (0.61-0.99) 1.13 (0.88-1.44) 1.11 (0.87-1.41)
Remote use 53 450.1 197 3.69 1 [Reference] 1 [Reference] 1 [Reference]
Abbreviations: MI, myocardial infarction; NA, not applicable; RR, rate ratio; SCD, sudden cardiac death.
a
Adjusted for site, age, sex, and calendar year (ie, matching variables).
b
Adjusted for site, age, sex, calendar year, and cardiovascular risk score (some variables within score are time varying).
c
Duration does not include pemoline use (pemoline only and pemoline with other attention-deficit/hyperactivity disorder medications).
d
Analyses excluded the 3 Health Maintenance Organization Research Network (HMORN) sites (Fallon Community, Kaiser Permanente [KP] Georgia, KP Northwest) that did not
provide data on SCD end points.
e
Analyses excluded the 2 HMORN sites (Fallon Community, KP Georgia) that did not provide data on stroke end points.
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
2011 American Medical Association. All rights reserved. JAMA, Published online December 12, 2011 E9
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
risk of serious cardiovascular events.
However, with these surveillance sys-
tems, which capture only a small per-
centage of adverse events, false signals
may occur if clinicians suspect, and are
thus more likelytoreport, adverse events
for a particular drug.
The findings of the current study
were similar to those of our parallel
study in youths aged 2 through 24
years, in which we found no evidence
of increased risk for serious cardiovas-
cular events in current users of ADHD
medications compared with nonus-
ers.
19
To our knowledge, only 2 phar-
macoepidemiologic studies of ADHD
medications and CVD in adults have
reported results.
17,18
These studies,
which were substantially smaller than
ours, used electronic pharmacy rec-
ords and medical encounter data,
with similarly limited information on
some potentially important risk fac-
tors. In one study, users of ADHD
medications had a more than 3-fold
higher rate of transient ischemic
attacks but a 30% lower rate of cere-
brovascular accidents, although the
latter was not statistically significant.
17
In contrast, no increase in SCDs
among children, adolescents, or
young adults was observed in a sec-
ond cohort study conducted in the
General Practice Research Database.
18
Inconclusion, inthis cohort of young
and middle-aged adults, current or new
use of ADHD medications identified
from filled prescriptions, compared
with nonuse or remote use, was not as-
sociated with an increased risk of seri-
ous cardiovascular events. A modestly
elevated risk cannot be ruled out, given
limited power and a lack of complete
information on some potentially im-
portant risk factors and other factors re-
lated to use of these medications.
Published Online: December 12, 2011. doi:10.1001
/jama.2011.1830
Author Contributions: Dr Habel had full access to all
of the data in the study and takes responsibility for
the integrity of the data and the accuracy of the data
analysis.
Study concept and design: Habel, Cooper, Sox, Chan,
Fireman, Cheetham, Ray, Selby.
Acquisition of data: Habel, Cooper, Sox, Chan,
Cheetham, Quinn, Dublin, Boudreau, Andrade,
Pawloski, Raebel, Smith, Uratsu, Selby.
Analysis and interpretation of data: Habel, Cooper,
Sox, Chan, Fireman, Arbogast, Cheetham, Quinn,
Achacoso, Uratsu, Go, Sidney, Nguyen-Huynh, Ray,
Selby.
Drafting of the manuscript: Habel.
Critical revision of the manuscript for important in-
tellectual content: Cooper, Sox, Chan, Fireman,
Arbogast, Cheetham, Quinn, Dublin, Boudreau,
Andrade, Pawloski, Raebel, Smith, Achacoso, Uratsu,
Go, Sidney, Nguyen-Huynh, Ray, Selby.
Statistical analysis: Cooper, Fireman, Arbogast,
Achacoso, Uratsu.
Obtained funding: Habel, Cooper, Chan, Quinn, Selby.
Administrative, technical, or material support: Chan,
Quinn, Andrade, Achacoso, Uratsu, Selby.
Study supervision: Habel, Cooper, Sox, Chan, Quinn,
Andrade, Smith.
Conflict of Interest Disclosures: All authors have com-
pleted and submitted the ICMJE Form for Disclosure
of Potential Conflicts of Interest. Dr Habel reported
receiving grants fromMerck for a study of herpes zos-
Figure 2. Subgroup Analyses for Combined End Point (Myocardial Infarction, Sudden Cardiac
Death, or Stroke), Use vs Nonuse of ADHD Medications
Lower Risk Higher Risk
0.2 5.0 1.0
Rate Ratio (95% CI)
No. of
Events
Subgroup and ADHD
Medication Use Person-Years
Rate Ratio
(95% CI)
Cohort
Full
234 Current use 107 322.4 0.83 (0.72-0.95)
489 Past use 165 319.4 0.85 (0.77-0.95)
1391 Nonuse 533 540.4 1 [Reference]
New-user
125 Current use 52 094.6 0.77 (0.63-0.94)
376 Past use 116 918.7 0.85 (0.75-0.98)
957 Nonuse 317 514.4 1 [Reference]
0.2 5.0 1.0
Rate Ratio (95% CI)
No
History of CVD
79 Current use 70 748.1 0.79 (0.62-1.00)
148 Past use 106 497.1 0.79 (0.65-0.95)
562 Nonuse 391 881.9 1 [Reference]
Yes
155 Current use 36 574.2 0.87 (0.73-1.03)
341 Past use 58 822.3 0.89 (0.79-1.01)
829 Nonuse 141 658.5 1 [Reference]
0.2 5.0 1.0
Rate Ratio (95% CI)
25-44
Age, y
47 Current use 54 106.9 0.78 (0.57-1.06)
102 Past use 85 786.7 0.79 (0.63-1.00)
250 Nonuse 271 667.1 1 [Reference]
45-64
187 Current use 53 215.5 0.83 (0.71-0.97)
387 Past use 79 532.7 0.86 (0.76-0.97)
1141 Nonuse 261 873.3 1 [Reference]
0.2 5.0 1.0
Rate Ratio (95% CI)
Yes
57 Current use 37 564.9 0.76 (0.57-1.01)
55 Past use 34 264.7 0.79 (0.59-1.05)
283 Nonuse 152 357.3 1 [Reference]
No
ADHD diagnosis
177 Current use 69 757.4 0.86 (0.74-1.01)
434 Past use 131 054.7 0.87 (0.78-0.97)
1113 Nonuse 385 962.7 1 [Reference]
0.2 5.0 1.0
Rate Ratio (95% CI)
Yes
191 Current use 78 966.8 0.87 (0.73-1.03)
386 Past use 115 995.3 0.88 (0.77-1.01)
507 Nonuse 125 558.9 1 [Reference]
No
Non-ADHD psychiatric conditions
43 Current use 28 355.6 0.76 (0.56-1.04)
103 Past use 49 324.2 0.82 (0.67-1.01)
884 Nonuse 407 981.5 1 [Reference]
Rate ratios are adjusted for site, age, sex, calendar year, and cardiovascular risk score (some variables within
score are time varying), except for newusers (adjusted for propensity score). ADHDindicates attention-deficit/
hyperactivity disorder; CVD, cardiovascular disease.
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
E10 JAMA, Published online December 12, 2011 2011 American Medical Association. All rights reserved.
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
ter in patients with cancer, from Takeda for a study
of pioglitazone and cancer, and from sanofi-aventis
for a study of insulin and cancer. Dr Chan reported
receiving support for travel to meetings for the pur-
pose of the study or other purposes fromthe US Food
and Drug Administration (FDA) and that he is a part-
time employee of OptumInsight, a for-profit com-
pany that receives fundingfrommedical product manu-
facturers to provide consultation and conduct research
on medical products; because OptumInsight is a part
of UnitedHealthGroup, Dr Chan has received Unit-
edHealthGroup stock options. Dr Dublin reported re-
ceiving a Merck/American Geriatrics Society NewIn-
vestigator Award (honorarium paid directly to Dr
Dublin) for unrelated work. Dr Andrade reported that
the Meyers Primary Care Institute has received fund-
ing from GlaxoSmithKline and Novartis Pharmaceu-
ticals, manufacturers of medications used to treat
ADHD. Dr Smith reported that the Center for Health
Research received funding from Abbott Laboratories
to conduct a natural history study of patients with
chronic kidney disease and from GlaxoSmithKline to
study the burden of diabetes. Dr Sidney reported re-
ceiving grants or grants pending from the National
Heart, Lung, and Blood Institute, the National Insti-
tute of Neurological Disorders and Stroke, the Na-
tional Institute of Diabetes and Digestive and Kidney
Diseases, and the Thrasher Research Fund. Dr Nguyen-
Huynh reported receiving grants or grants pending
from the American Heart Association. No other au-
thors reported disclosures.
Funding/Support: This project was funded in part un-
der contract numbers HHSA290-2005-0042 (Van-
derbilt) and HHSA290-2005-0033 (Harvard Pilgrim
Health Care Institute) from the Agency for Health-
care Research and Quality (AHRQ), US Department
of Health and Human Services, as part of the Devel-
oping Evidence to Inform Decisions about Effective-
ness (DEcIDE) program. The project was also funded
by the FDA under contracts 223-2005-10012 (Kai-
ser Permanente Northern California), 223-2005-
10100C(Vanderbilt), 223-2005-20006C(Ingenix), and
223-2005-10012C (Harvard Pilgrim Health Care In-
stitute). The project was also funded by the National
Institute on Aging under contract K23AG028954
(Group Health Research Institute).
Role of the Sponsors: Individuals fromthe AHRQand
FDA were on the study Steering Committee and pro-
vided input into the study design and conduct of the
study and interpretation of the data. The AHRQ and
FDA had no role in the preparation, review, or ap-
proval of the manuscript.
Disclaimer: The authors of this article are responsible
for its content. Statements in the article should not be
construed as endorsement by the AHRQor the US De-
partment of Health and Human Services.
Online-Only Material: The eMethods and eTables
1-12 are available at http://www.jama.com.
Additional Contributions: We acknowledge and thank
the following individuals for their contributions to this
project: Andrew Mosholder, MD (FDA), member of
Scientific Steering Committee; James Daugherty, MS,
and Judith Dudley, BS (Vanderbilt University School
of Medicine), programming; Chantal Avila, MA (Kai-
ser Permanente Southern California), project man-
agement; Yan Luo, PhD, and Wansu Chen, MS (Kai-
ser Permanente Southern California), programming;
Mary Kershner, BSN (Kaiser Permanente Colorado),
chart reviews and abstraction; April Duddy, MS (Har-
vard Pilgrim Health Care Institute), project manage-
ment; Luana Acton, BS, Julie Munneke, BA, and Heidi
Krause, BA (Kaiser Permanente Northern California),
project management; and Jean Lee, BA, and Monica
Highbaugh, AA (Kaiser Permanente Northern Cali-
fornia), medical record retrieval and abstraction. All
individuals acknowledged were compensated for their
time.
REFERENCES
1. NewReport: Americas State of Mind. Medco Web
site. http://medco.mediaroom.com/. 2011. Accessed
November 16, 2011.
2. Food and Drug Administration. Drug Safety
and Risk Management Advisory Committee meeting.
http://www.fda.gov/ohrms/dockets/ac/cder06
.html#DrugSafetyRiskMgmt. Food and Drug Adminis-
tration Web site. February 9-10, 2006. Accessed No-
vember 21, 2011.
3. Montejano L, Sasane R, Hodgkins P, Russo L, Huse
D. Adult ADHD: prevalence of diagnosis in a US popu-
lation with employer health insurance. Curr Med Res
Opin. 2011;27(suppl 2):5-11.
4. Wilens TE, Morrison NR, Prince J. An update on the
pharmacotherapy of attention-deficit/hyperactivity dis-
order in adults. Expert Rev Neurother. 2011;11(10):
1443-1465.
5. Challman TD, Lipsky JJ. Methylphenidate: its phar-
macology and uses. Mayo Clin Proc. 2000;75(7):
711-721.
6. LeddyJJ, EpsteinLH, Jaroni JL, et al. Influenceof meth-
ylphenidate on eating in obese men. Obes Res. 2004;
12(2):224-232.
7. Frierson RL, Wey JJ, Tabler JB. Psychostimulants for
depression in the medically ill. AmFamPhysician. 1991;
43(1):163-170.
8. Tharwani HM, Yerramsetty P, Mannelli P, Patkar A,
Masand P. Recent advances in poststroke depression.
Curr Psychiatry Rep. 2007;9(3):225-231.
9. Warden DL, Gordon B, McAllister TW, et al; Neu-
robehavioral Guidelines Working Group. Guidelines for
the pharmacologic treatment of neurobehavioral se-
quelae of traumatic brain injury. J Neurotrauma. 2006;
23(10):1468-1501.
10. Hammerness PG, Surman CB, Chilton A. Adult at-
tention-deficit/hyperactivity disorder treatment andcar-
diovascular implications. Curr Psychiatry Rep. 2011;
13(5):357-363.
11. Stiefel G, BesagFM. Cardiovascular effects of meth-
ylphenidate, amphetamines and atomoxetine in the
treatment of attention-deficit hyperactivitydisorder. Drug
Saf. 2010;33(10):821-842.
12. Lewington S, Clarke R, Qizilbash N, Peto R, Collins
R; Prospective Studies Collaboration. Age-specific rel-
evance of usual blood pressure to vascular mortality: a
meta-analysis of individual data for one million adults
in 61 prospective studies. Lancet. 2002;360(9349):
1903-1913.
13. Gould MS, Walsh BT, Munfakh JL, et al. Sudden
death and use of stimulant medications in youths. Am
J Psychiatry. 2009;166(9):992-1001.
14. Winterstein AG, Gerhard T, Shuster J, Johnson M,
Zito JM, Saidi A. Cardiac safety of central nervous sys-
temstimulants inchildrenandadolescents withattention-
deficit/hyperactivity disorder. Pediatrics. 2007;120
(6):e1494-e1501.
15. Schelleman H, Bilker WB, Strom BL, et al. Cardio-
vascular events and death in children exposed and un-
exposed to ADHD agents. Pediatrics. 2011;127
(6):1102-1110.
16. Winterstein AG, Gerhard T, Shuster J, Saidi A. Car-
diac safetyof methylphenidateversus amphetaminesalts
in the treatment of ADHD. Pediatrics. 2009;124
(1):e75-e80.
17. Holick CN, Turnbull BR, Jones ME, Chaudhry S,
Bangs ME, Seeger JD. Atomoxetine and cerebrovascu-
lar outcomes in adults. J Clin Psychopharmacol. 2009;
29(5):453-460.
18. McCarthy S, Cranswick N, Potts L, Taylor E, Wong
IC. Mortality associated with attention-deficit hyperac-
tivity disorder (ADHD) drug treatment: a retrospective
cohort study of children, adolescents and young adults
using the general practice research database. Drug Saf.
2009;32(11):1089-1096.
19. Cooper WO, Habel LA, Sox CM, et al. ADHDdrugs
and serious cardiovascular events in children and
young adults. N Engl J Med. 2011;365(20):1896-
1904.
20. Alpert JS, Thygesen K, Antman E, Bassand JP. Myo-
cardial infarction redefineda consensus document of
The Joint EuropeanSociety of Cardiology/AmericanCol-
lege of Cardiology Committee for the redefinition of
myocardial infarction. J Am Coll Cardiol. 2000;36
(3):959-969.
21. Meier MA, Al-Badr WH, Cooper JV, et al. The new
definition of myocardial infarction: diagnostic and prog-
nostic implications in patients with acute coronary
syndromes. Arch Intern Med. 2002;162(14):1585-
1589.
22. Chung CP, Murray KT, Stein CM, Hall K, Ray WA.
A computer case definition for sudden cardiac death.
Pharmacoepidemiol Drug Saf. 2010;19(6):563-572.
23. Miettinen OS. Stratification by a multivariate con-
founder score. Am J Epidemiol. 1976;104(6):609-
620.
24. Arbogast PG, Ray WA. Use of disease risk scores
in pharmacoepidemiologic studies. Stat Methods Med
Res. 2009;18(1):67-80.
25. Glynn RJ, Schneeweiss S, Stu rmer T. Indications for
propensi ty scores and revi ew of thei r use i n
pharmacoepidemiology. Basic Clin Pharmacol Toxicol.
2006;98(3):253-259.
26. Suissa S, Edwardes MD. Adjusted odds ratios for
case-control studies with missing confounder data in
controls. Epidemiology. 1997;8(3):275-280.
27. Schneeweiss S. Sensitivity analysis and external ad-
justment for unmeasured confounders in epidemio-
logic database studies of therapeutics. Pharmacoepi-
demiol Drug Saf. 2006;15(5):291-303.
28. Schneeweiss S, GlynnRJ, Tsai EH, AvornJ, Solomon
DH. Adjusting for unmeasured confounders in phar-
macoepidemiologic claims data using external informa-
tion: the example of COX2 inhibitors and myocardial
infarction. Epidemiology. 2005;16(1):17-24.
29. Ray WA. Evaluating medication effects outside of
clinical trials: new-user designs. AmJ Epidemiol. 2003;
158(9):915-920.
30. West SL, StromBL, Polle C. Validity of pharmaco-
epidemiologic drug and diagnosis data. In: Strom BL,
ed. Pharmacoepidemiology. Philadelphia, PA: John Wi-
ley & Sons Ltd; 2005:709-765.
31. de Burgos-Lunar C, Sal i nero-Fort MA,
Ca rdenas-ValladolidJ, et al. Validationof diabetes melli-
tus and hypertension diagnosis in computerized medi-
cal records in primary health care. BMC Med Res
Methodol. 2011;11:146.
32. Thygesen SK, Christiansen CF, Christensen S, Lash
TL, Srensen HT. The predictive value of ICD-10 diag-
nostic coding used to assess Charlson comorbidity in-
dex conditions in the population-based Danish Na-
tional Registry of Patients. BMC Med Res Methodol.
2011;11:83.
33. Grijalva CG, Chung CP, Stein CM, et al. Comput-
erized definitions showed high positive predictive val-
ues for identifying hospitalizations for congestive heart
failure andselectedinfections inMedicaidenrollees with
rheumatoidarthritis. Pharmacoepidemiol DrugSaf. 2008;
17(9):890-895.
34. Adler LA, ZimmermanB, Starr HL, et al. Efficacy and
safety of OROS methylphenidate in adults with
attention-deficit/hyperactivity disorder: a randomized,
placebo-controlled, double-blind, parallel group, dose-
escalation study. J Clin Psychopharmacol. 2009;
29(3):239-247.
35. PetersonK, McDonaghMS, FuR. Comparativeben-
efits andharms of competingmedications for adults with
attention-deficit hyperactivity disorder: a systematic re-
view and indirect comparison meta-analysis. Psycho-
pharmacology (Berl). 2008;197(1):1-11.
36. Cohen AL, Jhung MA, Budnitz DS. Stimulant medi-
cations and attention deficit-hyperactivity disorder.
N Engl J Med. 2006;354(21):2294-2295.
ADHD MEDICATIONS AND CV EVENTS IN YOUNGER ADULTS
2011 American Medical Association. All rights reserved. JAMA, Published online December 12, 2011 E11
by guest on December 14, 2011 jama.ama-assn.org Downloaded from
You might also like
- 18 Gut Brain and Pandas PansDocument76 pages18 Gut Brain and Pandas Panslv499446100% (1)
- MTHFR MutationDocument1 pageMTHFR MutationRobin KallisNo ratings yet
- Ospolot 200 MG, Film-Coated Tablets: Summary of Product Characteristics (SPC)Document7 pagesOspolot 200 MG, Film-Coated Tablets: Summary of Product Characteristics (SPC)ddandan_2No ratings yet
- Battleground Shmuel KatzDocument167 pagesBattleground Shmuel KatzGary KatzNo ratings yet
- ACPA Chronic PainDocument126 pagesACPA Chronic PainFyan FiradyNo ratings yet
- Company ProfileDocument6 pagesCompany ProfileAhmed Eljenan100% (1)
- Law and Ethics ExamDocument22 pagesLaw and Ethics ExamMan Dip100% (1)
- Erectile Dysfunction and Comorbid Diseases, Androgen Deficiency, and Diminished Libido in MenDocument7 pagesErectile Dysfunction and Comorbid Diseases, Androgen Deficiency, and Diminished Libido in MenAfif Al FatihNo ratings yet
- Adverse Effects of FluoroquinolonesDocument10 pagesAdverse Effects of FluoroquinolonesAvelox FloxNo ratings yet
- Food For Mood: 1. Foods Rich in Omega-3 Fatty AcidsDocument7 pagesFood For Mood: 1. Foods Rich in Omega-3 Fatty AcidsakankshaNo ratings yet
- Articles On Wheat ToxicityDocument96 pagesArticles On Wheat ToxicityDr. Heath Motley100% (1)
- Repositioning of Anthelmintic Drugs For The Treatment of Cancers of The Digestive SystemDocument18 pagesRepositioning of Anthelmintic Drugs For The Treatment of Cancers of The Digestive SystemMishael PeterNo ratings yet
- Aditivos Alimentarios PDFDocument38 pagesAditivos Alimentarios PDFANTHONY FARID CABEZAS GUEVARANo ratings yet
- Health Psychology Assignment (MA201477)Document7 pagesHealth Psychology Assignment (MA201477)Syeda DaniaNo ratings yet
- Contemporary and Integrative MedicineDocument10 pagesContemporary and Integrative Medicineapi-649875164No ratings yet
- Day 3Document3 pagesDay 3Karl JohnsonNo ratings yet
- Hereditary HemochromatosisDocument6 pagesHereditary HemochromatosisVijeyachandhar DorairajNo ratings yet
- Defiency Chart and SurveyDocument2 pagesDefiency Chart and Surveyapi-232967376No ratings yet
- Start Low and Go Slow 1-21-2014Document5 pagesStart Low and Go Slow 1-21-2014Ed JonesNo ratings yet
- Vivitrol TreatmentDocument8 pagesVivitrol TreatmentHarish RathodNo ratings yet
- Mcs Under SiegeDocument16 pagesMcs Under Siegeapi-269724919No ratings yet
- An Update On Menopause ManagementDocument10 pagesAn Update On Menopause ManagementJuan FranciscoNo ratings yet
- Ophthalmologic Concerns With Alternative Medicinal TherapiesDocument26 pagesOphthalmologic Concerns With Alternative Medicinal TherapiesBaharudin Yusuf Ramadhani100% (1)
- Mind Body Medicine Mind Body Medicine MiDocument14 pagesMind Body Medicine Mind Body Medicine MiMotea IoanaNo ratings yet
- Alcoholic Liver DiseaseDocument8 pagesAlcoholic Liver DiseaseCassandra ZubeheourNo ratings yet
- Parasite Herbal RemediesDocument10 pagesParasite Herbal Remediesdonaldbrown16No ratings yet
- Magnesium Is Critical For: Balancing Blood Sugar LevelsDocument1 pageMagnesium Is Critical For: Balancing Blood Sugar LevelsmajikNo ratings yet
- The ADAPT Functional Medicine Practitioner Training Program Course GuideDocument18 pagesThe ADAPT Functional Medicine Practitioner Training Program Course Guideerica100% (1)
- Nutritional Psychiatry - Your Brain On Food - Harvard Health Blog - Harvard Health PublishingDocument9 pagesNutritional Psychiatry - Your Brain On Food - Harvard Health Blog - Harvard Health PublishingAna Rica Santiago Navarra-CruzNo ratings yet
- The Rold of Fodmap Diet in IbsDocument4 pagesThe Rold of Fodmap Diet in Ibsapi-236139728No ratings yet
- Elimination Diet Weekly Planner Metricized Sample MenuDocument44 pagesElimination Diet Weekly Planner Metricized Sample MenuAmanda JimenezNo ratings yet
- Vitamin B2Document2 pagesVitamin B2sbornicul100% (1)
- Nutrition Low Purine DietDocument4 pagesNutrition Low Purine DietHuan XinchongNo ratings yet
- Is Diet Important in Bipolar Disorder?Document13 pagesIs Diet Important in Bipolar Disorder?Giovane de PaulaNo ratings yet
- THE INTEGRATIVE MedicineDocument23 pagesTHE INTEGRATIVE MedicineBaihaqi SaharunNo ratings yet
- Alcoholism and Psychiatric - Diagnostic Challenges PDFDocument9 pagesAlcoholism and Psychiatric - Diagnostic Challenges PDFmirtaNo ratings yet
- The 3 Most Important Types of Omega-3 Fatty AcidsDocument168 pagesThe 3 Most Important Types of Omega-3 Fatty AcidsAndreea DumitrescuNo ratings yet
- Itamin Hart: No ToxicityDocument4 pagesItamin Hart: No ToxicityAnonymous Sfcml4GvZNo ratings yet
- Antidepressant Switching TableDocument1 pageAntidepressant Switching TableSimone BelfioriNo ratings yet
- Antiprotozoal Agents: PHR SangitaDocument21 pagesAntiprotozoal Agents: PHR SangitaCurex QANo ratings yet
- Collagen (Protein) PeptideDocument7 pagesCollagen (Protein) PeptideDexter OcsanNo ratings yet
- Hypnotics Anxiolytics GuidelinesDocument28 pagesHypnotics Anxiolytics GuidelinesClarissa YudakusumaNo ratings yet
- Lugol and GraveDocument6 pagesLugol and GraveSeptiandry Ade Putra100% (2)
- Diet and Dermatology: The Role of Dietary Intervention in Skin DiseaseDocument6 pagesDiet and Dermatology: The Role of Dietary Intervention in Skin Diseaseartventoure projectNo ratings yet
- Nootropics Guide101Document29 pagesNootropics Guide101markus.proxyNo ratings yet
- An Enhanced Bioavailable Formulation of Curcumin Using Fenugreek-Derived Soluble Dietary FibreDocument10 pagesAn Enhanced Bioavailable Formulation of Curcumin Using Fenugreek-Derived Soluble Dietary FibrehanaNo ratings yet
- Benefits of Vitamin C in Tumor Treatment PDFDocument11 pagesBenefits of Vitamin C in Tumor Treatment PDFRocco LamponeNo ratings yet
- Prebiotic Effect in The Healthy Infant - Recent Update: Yvan - Vandenplas@uzbrussel - BeDocument53 pagesPrebiotic Effect in The Healthy Infant - Recent Update: Yvan - Vandenplas@uzbrussel - BegazalidjawadNo ratings yet
- Do Cells Phones Cause Cancer?Document3 pagesDo Cells Phones Cause Cancer?Jed DiamondNo ratings yet
- Functional Medicine 005Document1 pageFunctional Medicine 005Iu IianoNo ratings yet
- Methionine and Methylation Chicken or The Egg PDFDocument7 pagesMethionine and Methylation Chicken or The Egg PDFPanphilaNo ratings yet
- Methylation Implications With Periodontal Disease 1 0Document107 pagesMethylation Implications With Periodontal Disease 1 0David Delgado100% (1)
- The Use of Hormones For Chronic PainDocument6 pagesThe Use of Hormones For Chronic PainPaulo SilvaNo ratings yet
- Gluten Free Nutrition Guide 2011Document44 pagesGluten Free Nutrition Guide 2011Chico Santa RosaNo ratings yet
- Psychopharmacology NewestDocument43 pagesPsychopharmacology NewestRegina PunNo ratings yet
- Mushrooms For Alzheimer's and Dementia - My Interview With Mark KaylorDocument3 pagesMushrooms For Alzheimer's and Dementia - My Interview With Mark KaylornicungNo ratings yet
- Thyroid Balancing Lifestyle Program - DR Katie Leah ND (February 2012)Document8 pagesThyroid Balancing Lifestyle Program - DR Katie Leah ND (February 2012)Dr Katie Leah NDNo ratings yet
- What Is Medical Marijuana?Document11 pagesWhat Is Medical Marijuana?ZAARA ADAMSNo ratings yet
- Detoxification: Leo Galland M.D. Foundation For Integrated MedicineDocument35 pagesDetoxification: Leo Galland M.D. Foundation For Integrated Medicinemubs10No ratings yet
- J Neurol Neurosurg Psychiatry 2002 Hadjivassiliou 560 3Document5 pagesJ Neurol Neurosurg Psychiatry 2002 Hadjivassiliou 560 3Jorge Massano RodriguesNo ratings yet
- Obesity Project 1Document20 pagesObesity Project 1api-203751052No ratings yet
- NAD Booster Supplements Review (NAD+ - NADH, Nicotinamide Riboside, NMN) - Top PicksDocument13 pagesNAD Booster Supplements Review (NAD+ - NADH, Nicotinamide Riboside, NMN) - Top PicksWaters75No ratings yet
- Complementary and Alternative Medical Lab Testing Part 11: MenFrom EverandComplementary and Alternative Medical Lab Testing Part 11: MenNo ratings yet
- Apple Cider Vinegar Recipes: Easy Apple Cider Recipes to Lose Weight Fast, Boost Energy Levels and Live HealthyFrom EverandApple Cider Vinegar Recipes: Easy Apple Cider Recipes to Lose Weight Fast, Boost Energy Levels and Live HealthyNo ratings yet
- BlackWhiteWorldIII Cox&ForkhumDocument243 pagesBlackWhiteWorldIII Cox&ForkhumGary KatzNo ratings yet
- Neighborhood Bully: by Bob Dylan, 1983 (On "Infidels" Album)Document9 pagesNeighborhood Bully: by Bob Dylan, 1983 (On "Infidels" Album)Gary KatzNo ratings yet
- FB Jere MarinesDocument3 pagesFB Jere MarinesGary KatzNo ratings yet
- Jsa 1 Clemens HeniDocument10 pagesJsa 1 Clemens HeniGary KatzNo ratings yet
- Neighborhood Bully2010Document2 pagesNeighborhood Bully2010Gary KatzNo ratings yet
- Lior Feb IDFletter 2 FujDocument1 pageLior Feb IDFletter 2 FujGary KatzNo ratings yet
- Board Psych July 2007Document2 pagesBoard Psych July 2007Gary KatzNo ratings yet
- Cartoonseditorial Job 010Document3 pagesCartoonseditorial Job 010Gary KatzNo ratings yet
- The New American - March 24, 2014Document48 pagesThe New American - March 24, 2014fabrignani@yahoo.com100% (1)
- The Regulatory Trends: Cross-Contamination in Drug ManufacturingDocument9 pagesThe Regulatory Trends: Cross-Contamination in Drug Manufacturinglina kharratNo ratings yet
- NRS 230 Pharmacology Week 1 Students - 11!22!11Document110 pagesNRS 230 Pharmacology Week 1 Students - 11!22!11angieswensonNo ratings yet
- Nursing Care Management 103 Cap MRDocument9 pagesNursing Care Management 103 Cap MRkarenfaye00No ratings yet
- 8 Reasons I Havent Vaccinated My ChildDocument4 pages8 Reasons I Havent Vaccinated My ChildMichael SmithNo ratings yet
- Immunotoxicology EvaluationDocument38 pagesImmunotoxicology EvaluationVlad TomaNo ratings yet
- 4.2 Sample Policy and Procedure For Medication ManagementDocument7 pages4.2 Sample Policy and Procedure For Medication ManagementbhongskirnNo ratings yet
- Atorvastatin 0Document7 pagesAtorvastatin 0AgronaSlaughterNo ratings yet
- Taste Masked Suspension: The Pharma InnovationDocument6 pagesTaste Masked Suspension: The Pharma InnovationFly Hitsugi Shuin KitaroNo ratings yet
- Drug Information Resources PDFDocument68 pagesDrug Information Resources PDFhark reynaldo100% (1)
- Chapter 04 - Treatment Settings and Rehabilitation ProgramsDocument7 pagesChapter 04 - Treatment Settings and Rehabilitation ProgramsMonicaNo ratings yet
- Pharma Co List 1000Document90 pagesPharma Co List 1000Naveenbabu Soundararajan100% (1)
- NeostigmineDocument4 pagesNeostigmineDonna Lyn B. DizonNo ratings yet
- Adr ReportingDocument12 pagesAdr Reportinguss uusNo ratings yet
- Living Longer, Living Well: Highlights and Key RecommendationsDocument22 pagesLiving Longer, Living Well: Highlights and Key RecommendationsRoberta PenningtonNo ratings yet
- The Early Development of Medical Licensing Laws in The United States, 1875-1900, by Ronald HamowyDocument47 pagesThe Early Development of Medical Licensing Laws in The United States, 1875-1900, by Ronald HamowyNicolas MartinNo ratings yet
- Patient Identification PolicyDocument26 pagesPatient Identification PolicyrenalgoodNo ratings yet
- Q9Document9 pagesQ9asastuffNo ratings yet
- Market Entry Plan For IndonesiaDocument11 pagesMarket Entry Plan For IndonesiaKiran Manoj100% (2)
- Arief PDFDocument8 pagesArief PDFElya AmaliiaNo ratings yet
- Savovent Company ProfileDocument8 pagesSavovent Company Profilemehta hemantNo ratings yet
- Medical System in RomaniaDocument38 pagesMedical System in Romaniabogdan ciubucNo ratings yet
- CSIPR E-Newsletter Issue 1Document8 pagesCSIPR E-Newsletter Issue 1Bar & BenchNo ratings yet
- Quick Question GuideDocument2 pagesQuick Question GuideLouisa WongNo ratings yet
- PharmaDocument37 pagesPharmaSnehal Wanjari100% (1)
- 6 GRPDocument14 pages6 GRPRhona NiloNo ratings yet
- PHC ChecklistDocument15 pagesPHC ChecklistNarendra KardileNo ratings yet