0 ratings0% found this document useful (0 votes)
35 views1952
1952
Uploaded by
Lee Eun HyeThis study aimed to determine the correlation between the Thrombolysis in Myocardial Infarction (TIMI) risk score and the extent of coronary artery disease (CAD) in patients with acute coronary syndrome (ACS). The study found that patients with a high TIMI risk score (>4) were more likely to have significant three-vessel CAD compared to those with a low or intermediate TIMI risk score (<4). Specifically, 62% of high-risk patients had three-vessel disease versus 46.2% of low-intermediate risk patients. The study concludes that patients with a high TIMI risk score should be referred for early invasive coronary evaluation, as they are more likely to have severe mult
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
1952
1952
Uploaded by
Lee Eun Hye0 ratings0% found this document useful (0 votes)
35 views4 pagesThis study aimed to determine the correlation between the Thrombolysis in Myocardial Infarction (TIMI) risk score and the extent of coronary artery disease (CAD) in patients with acute coronary syndrome (ACS). The study found that patients with a high TIMI risk score (>4) were more likely to have significant three-vessel CAD compared to those with a low or intermediate TIMI risk score (<4). Specifically, 62% of high-risk patients had three-vessel disease versus 46.2% of low-intermediate risk patients. The study concludes that patients with a high TIMI risk score should be referred for early invasive coronary evaluation, as they are more likely to have severe mult
Original Description:
n
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
This study aimed to determine the correlation between the Thrombolysis in Myocardial Infarction (TIMI) risk score and the extent of coronary artery disease (CAD) in patients with acute coronary syndrome (ACS). The study found that patients with a high TIMI risk score (>4) were more likely to have significant three-vessel CAD compared to those with a low or intermediate TIMI risk score (<4). Specifically, 62% of high-risk patients had three-vessel disease versus 46.2% of low-intermediate risk patients. The study concludes that patients with a high TIMI risk score should be referred for early invasive coronary evaluation, as they are more likely to have severe mult
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
35 views4 pages1952
1952
Uploaded by
Lee Eun HyeThis study aimed to determine the correlation between the Thrombolysis in Myocardial Infarction (TIMI) risk score and the extent of coronary artery disease (CAD) in patients with acute coronary syndrome (ACS). The study found that patients with a high TIMI risk score (>4) were more likely to have significant three-vessel CAD compared to those with a low or intermediate TIMI risk score (<4). Specifically, 62% of high-risk patients had three-vessel disease versus 46.2% of low-intermediate risk patients. The study concludes that patients with a high TIMI risk score should be referred for early invasive coronary evaluation, as they are more likely to have severe mult
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 4
Introduction
Cardiovascular diseases have emerged as a major
health burden in developing countries and are a subject of
great concern for its significant contribution to mortality.
1
The
acute coronary syndrome is a major cause of cardiovascular
morbidity and mortality for which timely diagnosis and
appropriate therapy is of paramount importance to improve
clinical outcomes.
2
Patients presenting with acute coronary
syndrome unstable angina (UA) and Non-ST-segment
elevation myocardial infarction (NSTEMI) and STEMI, are at
risk for death, myocardial infarction or recurrent ischaemic
events.
3
Identifying such high risk patients, allows aggressive
antithrombotic treatment and early coronary angiography to
be targeted to those who will benefit.
4,5
In terms of multivariate analyses, the TIMI risk score
has proven to be an effective risk assessment tool for
predicting the risk of death and ischaemic events among
patients with ACS. The scheme of risk stratification in TIMI
risk score is based on seven independent clinical indicators
that are evaluated on patient's presentation.
3
It has the
advantage of being easy to calculate and has broad
applicability in the early assessment of patients.
Mega etal studied the association between the TIMI
risk score and high-risk angiographic findings in NSTEMI.
They showed that patients with TIMI risk score of 5 to 7 were
more likely to have a severe culprit stenosis (81%), p < 0 .001
and multivessel disease (80%), p <0.001 compared to those
with scores of 0 to 2.
6
Garcia etal also showed that the severity
of coronary artery disease increases as the TIMI risk score
increases, p <0.001.
7
Although studies have looked into the association of
TIMI risk score with different clinical parameters risk of
recurrent ischaemic events, mortality and use of glycoprotein
IIb/IIIa inhibitors, only limited studies have evaluated the
association of TIMI risk score with coronary angiographic
findings (in terms of the severity and the extent of CAD) in
ACS. Furthermore, there is no local data available. This
association is important as patients with low or intermediate
TIMI risk score and no high risk features of acute coronary
syndrome could be considered to be risk stratified by non-
invasive testing only which may prove to be cost-effective.
For this purpose we sought to determine the association
between TIMI risk score and the extent of CAD in ACS.
Patients and Methods
A cross sectional study was conducted on 200
consecutive patients who presented to the emergency
department of Tabba Heart Institute, Karachi from June to
December 2008. Written informed consent was obtained in all
cases for recruitment in the study and the procedures involved.
The study protocol was approved by the institutional review
board. Patients who had chest pain suggestive of angina or
anginal equivalent symptoms and diagnosis of ACS were
included in the study. We excluded those patients who had ST-
elevation myocardial infarction (STEMI), new left bundle
Vol. 60, No. 3, March 2010 197
Original Article
Correlation of Thrombolysis in Myocardial Infarction (TIMI) risk score with
extent of coronary artery disease in patients with acute coronary syndrome
Muhammad Shakir Lakhani,
1
Faisal Qadir,
2
Bashir Hanif,
3
Salman Farooq,
4
Moinuddin Khan
5
Department of Cardiology, Tabba Heart Institute,
1-3,5
Medical Student, Ziauddin Medical University,
4
Karachi, Pakistan.
Abstract
Objective: To determine the correlation of Thrombolysis in Myocardial Infarction (TIMI) risk score with extent of
coronary artery disease (CAD) in patients with acute coronary syndrome (ACS).
Methods: We conducted a descriptive study among 200 consecutive patients admitted with ACS at Tabba Heart
Institute, Karachi from June to December 2008. The TIMI risk score was stratified on seven standard variables.
The extent of CAD was evaluated on angiography and significant CAD was defined as > 70% stenosis in any
one of the three major epicardial vessels.
Results: The mean age of the sample was 58.53 10.64 years. Out of 200 patients, there were 142 (71%)
patients with TIMI score < 4 (low and intermediate TIMI risk score) and 58 (29%) patients with TIMI score >4
(high TIMI risk score). Patients with TIMI score > 4 were more likely to have significant three vessel CAD (62 %)
versus those with TIMI risk score < 4 (46.2 %), (p< 0.04).
Conclusion: Patients with high TIMI risk score were more likely to have severe multivessel CAD compared with
those with low or intermediate TIMI risk score. Hence, patients with TIMI score >4 should be referred for early
invasive coronary evaluation to derive clinical benefit (JPMA 60:197; 2010).
branch block on electrocardiogram (ECG), prior
revascularization either surgical/ percutaneous and definitive
non-ischaemic etiology for their chest pain at the time of
presentation.
Patients with ACS included UA, NSTEMI and
STEMI. The diagnosis of ACS was based on history,
electrocardiographic (ECG) findings and cardiac
biomarkers. All enrolled patients received standard medical
therapy for ACS and were admitted in either the coronary
care unit or in the cardiac step-down unit according to the
American College of Cardiology (ACC) /American Heart
Association (AHA) guidelines.
8
Blood samples for cardiac
troponin I were immediately drawn upon presentation to the
emergency room and a second sample was drawn 8 hours
later after admission. Cardiac troponin I was determined
using AxSYM Troponin - I ADV (Abbott Laboratories,
Abbott Park, Illinois) which is a three-step assay based on
the microparticle enzyme immunoassay (MEIA) technology
with an analytical sensitivity of 0.02 ng/ml and a diagnostic
cutoff for myocardial infarction of 0.40 ng/ml. The 99th
percentile was 0.04 ng/ml as described by the manufacturer.
The assay was designed to have a precision < 10% total
coefficient of variation with 95% confidence for
concentration from 0.27 ng/mL upto 4.00 ng/mL. All assays
were done by technologists unaware of the clinical and
angiographic data.
Patients with ACS were further risk stratified with
TIMI risk scores. The seven predictor variables for this score
are: (1) age > 65 years, (2) 3 or more cardiovascular risk
factors (family history of premature coronary artery disease,
diabetes mellitus, hypertension, dyslipidaemia or current
smoking), (3) previous CAD (> 50% stenosis at angiography)
(4) severe anginal symptoms (2 episodes in last 24 hours), (5)
use of aspirin in the last 7 days, (6) ST segment deviation > 0.5
mm and (7) elevated serum troponin I level.
Patients with ACS were further evaluated with
coronary angiograms to assess the extent of CAD. The
angiography was performed by the primary physician who
had experience of performing coronary angiography. The
extent of CAD evaluated on angiography was classified as
follows: significant CAD was defined as > 70% stenosis in
any of the three major epicardial coronary arteries or a left
main coronary artery stenosis > 50%. Angiograms
revealing coronary artery stenosis < 70% in major
epicardial coronary arteries were termed non-obstructive
CAD. Extent of CAD was defined as significant single, two
or three vessel CAD.
A proforma was designed inquiring about age, gender,
presence of major cardiac risk factors (diabetes, hypertension,
family history of premature CAD, dyslipidaemia and cigarette
smoking), chest pain episode during last 24 hours, use of
aspirin during last 7 days and prior known CAD.
The collected data was entered and analyzed by the
Statistical Package for Social Sciences version 15.0
Software (SPSS Inc., Chicago, Illinois). Descriptive
statistics were computed and presented as means and
standard deviations for continuous variables like age.
Frequencies and percentages were computed for gender,
risk factors (hypertension, diabetes, smoking, dyslipidaemia
and family history of premature CAD). Chi-square test was
applied to determine the proportions difference between
groups < 4 and >4 TIMI risk score. A p value <0.05 was
considered as significant.
Results
A total of 200 patients were included in this study. The
age range was 33-86 years, mean 58.53 10.64 years. There
were 139 (60%) males and 61 (30%) females. Of the total 98
(49%) patients were diabetics, 140 (70%) were hypertensives,
60 (30%) were smokers, 44 (22%) had positive history for
premature coronary artery disease and 127 (64%) were
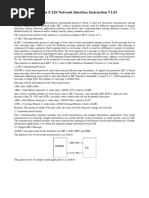
dyslipidaemic. Table-1 shows the baseline demographic and
clinical characteristics of the patients with TIMI score < 4 and
TIMI score > 4.
Table-2 shows the TIMI risk score variables in the
198 J Pak Med Assoc
Table-1: Baseline characteristics of patients according
to the TIMI risk score status.
Variable TIMI Risk score < 4 TIMI Risk score > 4
(n= 142) (n= 58)
Age (years) 56.23 9.69 64.43 10.9
Gender
Male 100 (70.4) 39 (67.2)
Female 42 (29.6) 19 (32.8)
Diabetes Mellitus 64 (45.1) 34 (58.6)
Hypertension 89 (62.7) 51 (87.9)
Family history of premature CAD 29 (20.4) 15 (25.9)
Dyslipidaemia 85 (59.9) 42 (72.4)
Smoker 41 (28.9) 10 (17.2)
Data expressed as the mean value SD or number (%) of patients.
TIMI = Thrombolysis in Myocardial Infarction, CAD= Coronary artery disease.
Table-2: TIMI Risk score variables in the study population.
TIMI Risk score TIMI Risk score < 4 TIMI Risk score > 4
variables (n= 142) (n= 58)
3 or more common risk
factors for CAD 54 (38) 39 (67.2)
Chest pain 130 (91.5) 54 (93.1)
Use of aspirin 63 (44.4) 53 (91.4)
Prior known CAD 15 (10.6) 23 (39.7)
ECG ST changes 62 (43.7) 51(87.9)
Positive Troponin I 94 (66.2) 55 (94.8)
Age > 65 years 26 (18.3) 35 (60.3)
Data expressed as the number (%) of patients.
TIMI = Thrombolysis in Myocardial Infarction,
CAD= Coronary Artery Disease, ECG= Electrocardiography.
study population divided on the basis of a score < 4 and >
4. Among the TIMI risk score variables: chest pain was
most prevalent and involved 184 (92 %) patients, troponin I
was positive in 149 (75%), 116 (58%) patients used aspirin
within seven days, ST segment depression > 0.5 mm were
observed in 113 (57%) patients. Three or more risk factors
for CAD were present in 93 (47%), age > 65 years was
found in 52 (26%) and prior known CAD figured in 38
(19%) patients.
In Table-3, one hundred and forty two (71%) patients
with TIMI score < 4, single vessel CAD occurred in 39
(27.5%) patients, while two vessel and three vessel CAD
figured in 40 (28.3 %) and 63 (44.2 %) patients respectively.
In 58 (29%) patients with TIMI risk score > 4, single vessel
CAD occurred in 7 (12%), while two vessel and three vessel
CAD figured 15 (26%) and 36 (62%) respectively. The
results showed that TIMI risk score is significantly
associated with single vessel CAD (p < 0.02) and three
vessel CAD (p < 0.04).
Regarding the predominant vessel involvement in
both the TIMI risk score groups, left anterior descending
artery (LAD) was the predominant vessel involved. It
figured in 95 (66.9%) patients in the < 4 TIMI risk score
group and in 46 (79.3%) patients in the > 4 TIMI risk score
group. Significant left main coronary artery stenosis (> 50%
stenosis) was found in 3 (2.1%) in the < 4 TIMI risk score
group and 2 (3.4%) in the > 4 TIMI risk score group.
Discussion
The study revealed that patients with higher TIMI
risk score were associated with a greater extent of
significant CAD. Risk stratification in the setting of
UA/NSTEMI has been addressed in several large studies for
predicting the risk of death and ischaemic events.
3,9,10
The
severity of CAD has been correlated with different risk
stratification schemes like the PURSUIT,
11
AHCPR
12
and
the GRACE risk scores.
13
The TIMI risk score was developed and adapted for
patients with UA and NSTEMI. The TIMI risk score is an
effective tool for predicting the risk of death and ischaemic
events. The TIMI risk score is used for objective risk
stratification of patients into one of three groups: low score
(0 to 2; 5-8% risk); intermediate (3 to 4; 13-20% risk); and
high (5 to 7; 26-41% risk).The risk corresponds to future
cardiac events including death, myocardial infarction or
urgent revascularization within 14 days.
14
It also identifies
those who are likely to benefit most from an early invasive
strategy.
3
The usefulness of this score has been validated by
the results of the PRISM-PLUS.
15
and TACTICS-TIMI 18
trials.
16
The TIMI risk score based on the TIMI IIB
14
and
ESSENCE trials,
17
incorporates the combination of age,
clinical characteristics, ECG changes and cardiac bio-
markers for risk stratification. Additional biomarkers have
also been investigated to increase the predictive accuracy of
this score. Montoliu et al investigated the role of N-
terminal pro brain natriuretic peptide (NT-proBNP), C-
reactive protein (CRP), troponin T and D-dimer in
improving the predictive accuracy of the TIMI risk score in
patients with NSTE-ACS. Troponin T, CRP and NT-
proBNP were all predictors of adverse events. In all patient
groups with a low, moderate or high risk profile based on
the TIMI risk score, the presence of two or three elevated
biomarkers increased the event rate twofold in comparison
with no or one elevated biomarkers. They also found
positive correlations between these biomarkers.
18
In our study we divided our patients into two groups
based on the TIMI risk scores of < 4 and looked at the
association with the extent of CAD. The results of our study
compare well with the findings of Mega et al,
6
who studied
the correlation between the TIMI risk score and high-risk
angiographic findings in NSTE-ACS. Patients with risk
scores of 5 to 7, were more likely to have a severe culprit
stenosis (81% vs 58%, p < 0.001) and multivessel disease
(80% vs 43%, p <0.001), compared to those with scores of
0 to 2. The probability of significant left main disease (p
<0.001), also increased progressively with rising TIMI risk
scores ( p <0.001). The authors did not find any significant
correlation between TIMI risk score and left Main Disease
because of low prevalence of left Main Disease. A
significant correlation was observed between single vessel
disease and low TIMI risk score and triple vessel disease
and high TIMI risk score.
6
Zheng and colleagues in their
study found that TIMI risk score correlated well with the
severity of CAD (p< 0.001).
19
Garcia and coworkers also
showed that the extent and severity of CAD increases as the
TIMI risk score increases (p < 0.001).
7
Risk scoring systems should ideally be validated,
practical and easy to use at the patient bedside in day-to-day
clinical practice.
20
There is presently no risk model
conforming to all the above. The simplified version of the
GRACE risk score, for instance relies on a computed
algorithm for calculation. The TIMI risk score, on the other
Vol. 60, No. 3, March 2010 199
Table-3: Extent of coronary artery disease in the study
population based on the TIMI risk scores.
Extent of CAD TIMI Risk score < 4 TIMI Risk score > 4
(n= 142) (n= 58) p value
Single vessel CAD 39 (27.5) 7 (12) 0.02
Two vessel CAD 40 (28.3) 15 (26) 0.74
Three vessel CAD 63 (44.2) 36 (62) 0.04
Data expressed as the number (%) of patients.
Extent of CAD= significant CAD > 70% stenosis of major epicardial vessels,
TIMI = Thrombolysis in Myocardial Infarction.
hand is a validated scoring system and is a useful bedside
tool in the evaluation of risk for patients presenting with
acute coronary syndromes.
Our study represents the experiences of a single
institution. The severity and location of the coronary lesions
was based on the operator visual estimation without
quantitative or physiological evaluation.
Conclusion
Our study demonstrates that among patients
presenting with ACS- UA / NSTEMI who are referred for
coronary angiography, clinical risk stratification according
to the TIMI risk score correlates with the angiographic
extent of CAD. Patients with high TIMI risk scores were
more likely to have severe multivessel CAD compared with
those who have low scores. A routine invasive strategy in
high TIMI risk score patients should be considered as the
preferred strategy.
References
1. Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in
developing countries. Circulation. 1998; 97: 596-601.
2. Terkelsen CJ, Lassen JF, Norgaard BL, Gerdes JC, Jensen T, GotzscheLB, et
al. Mortality rates in patients with ST-elevation versus non-ST-elevation acute
myocardial infarction: observations from an unselected cohort. Eur Heart J
2005; 26: 18-26.
3. Antman EM, Cohen M, Bernink PJ, McCabe CH, Horacek T, Papuchis G, et
al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for
prognostication and therapeutic decision making. JAMA 2000; 284: 835-42.
4. Bach RG, Cannon CP, Weintraub WS, DiBattiste PM, Demopoulos LA,
Anderson HV, et al. Early cardiac catheterization is associated with lower
mortality only among high-risk patients with ST- and non-ST-elevation acute
coronary syndromes: Observations from the OPUS-TIMI 16 trial. Ann Intern
Med 2004; 141: 186-95.
5. Almeda FQ, Hendel RC, Nathan S, Meyer PM, Calvin JE, Klein LW.
Improved in-hospital outcomes in acute coronary syndromes (unstable
angina/non-ST segment elevation myocardial infarction) despite similar TIMI
risk scores. J Invasive Cardiol 2003; 15: 502-6.
6. Mega JL, Morrow DA, Sabatine MS, Zhao XQ, Snapinn SM, Dibattiste PM,
et al. Correlation between the TIMI risk score and high-risk angiographic
findings in non-ST-elevation acute coronary syndromes: observations from
the Platelet Receptor Inhibition in Ischaemic Syndrome Management in
Patients Limited by Unstable Signs and Symptoms (PRISM-PLUS) trial. Am
Heart J 2005; 149: 846-50.
7. Garcia S, Canoniero M, Peter A, de Marchena E, Ferreira A. Correlation of
TIMI risk score with angiographic severity and extent of coronary artery
disease in patients with non-ST-elevation acute coronary syndromes. Am J
Cardiol 2004; 93: 813-6.
8. Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr,
et al. ACC/AHA 2007 guidelines for the management of patients with
unstable angina/non ST-elevation myocardial infarction: a report of the
American College of Cardiology/American Heart Association Task Force on
Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the
Management of Patients With Unstable Angina/Non ST-Elevation Myocardial
Infarction): J Am Coll Cardiol 2007; 14: 50; e1-e157.
9. Boersma E, Pieper KS, Steyerberg EW,Wilcox RG, Chang WC, Lee KL, et al.
Predictors of outcome in patients with acute coronary syndromes without
persistent ST-segment elevation: results from an international trial of 9,461
patients. The PURSUIT Investigators. Circulation 2000; 101: 2557-67.
10. Armstrong PW, Fu Y, Chang WC, Topol EJ, Granger CB, Betriu Aet al. Acute
coronary syndromes in the GUSTO-IIb trial: prognostic insights and impact
of recurrent ischemia. The GUSTO-IIb Investigators. Circulation 1998; 98:
1860-8.
11. Topol E, Califf R, Simoons M, Diaz R, Paolasso E, Klein W, et al. Inhibition
of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute
coronary syndromes. Platelet Glycoprotein IIb/IIIa in Unstable Angina:
Receptor Suppression Using Integrilin Therapy. N Engl J Med 1998; 339:
436-43.
12. Brotons C, Permanyer-Miralda G, Calvo F, Camprecis M, Santos MT,
Cascant P et al. Validation of the Agency for Health Care Policy and Research
(AHCPR) classification for managing unstable angina. J Clin Epidemiol
1999; 52: 959-65.
13. Fox KA, Goodman SG, Klein W, Brieger D, Steg PG, Dabbous O, et al.
Management of acute coronary syndromes. Variations in practice and
outcome; findings from the Global Registry of Acute Coronary Events
(GRACE). Eur Heart J 2002; 23: 1177-89.
14. Antman EM, McCabe CH, Gurfinkel EP, Turpie AG, Bernink PJ, Salein D, et
al. Enoxaparin prevents death and cardiac ischaemic events in unstable
angina/non-Qwave myocardial infarction: results of the Thrombolysis in
Myocardial Infarction (TIMI) IIB Trial. Circulation 1999; 100: 1593-601.
15. Morrow DA, Antman EM, Snapinn SM, McCabe CH, Theroux P, Braunwald
E. An integrated clinical approach to predicting the benefit of tirofiban in non-
ST elevation acute coronary syndromes. Application of the TIMI Risk Score
for UA/NSTEMI in PRISM-PLUS. Eur Heart J 2002; 23: 223-9.
16. Morrow DA, de Lemos JA, Sabatine MS, Murphy SA, Demopoulos LA,
DiBattiste PM, et al. Evaluation of B-type natriuretic peptide for risk
assessment in unstable angina/non-ST-elevation myocardial infarction: B-type
natriuretic peptide and prognosis in TACTICS-TIMI 18. J Am Coll Cardiol
2003; 41: 1264-72.
17. Cohen M, Demers C, Gurfinkel EP, Turpie AG, Fromell GJ, Goodman S, et al.
A comparison of low molecular- weight heparin with unfractionated heparin
for unstable coronary artery disease: Efficacy and Safety of Subcutaneous
Enoxaparin in Non-Q-Wave Coronary Events Study Group. N Engl J Med
1997; 337: 447-52.
18. Tello-Montoliu A, Marin F, Roldan V, Mainar L, Lopez MT, Sogorb F, et al.
A multimarker risk stratification approach to non-ST elevation acute coronary
syndrome: implications of troponin T, CRP, NT pro-BNP and fibrin D-dimer
levels. J Intern Med 2007; 262: 651-8.
19. Zheng XY, Meng XK, Li WG, Yang J, Wei G, Fang R. Clinical study on value
of severity of patient with coronary artery disease evaluated with the
thrombosis in myocardial infarction risk score. Zhongguo Wei Zhong Bing Ji
Jiu Yi Xue 2004; 16: 239-41.
20. Lee KL, Woodlief LH, Topol EJ, , Weaver WD, Betriu A, Col J, et al.
Predictors of 30-day mortality in the era of reperfusion for acute myocardial
infarction: results from an international trial of 41,021 patients. Circulation
1995; 91: 1659-68.
200 J Pak Med Assoc
You might also like
- An Overview Tutorial of The Vxworks Real-Time Operating System byDocument9 pagesAn Overview Tutorial of The Vxworks Real-Time Operating System byRangaRajNo ratings yet
- Capital Budgeting (Principles & Techniques)Document31 pagesCapital Budgeting (Principles & Techniques)Shashank100% (4)
- Validity of Grace Risk Score To Predict The Prognosis in Elderly Patients With Acute Coronary SyndromeDocument9 pagesValidity of Grace Risk Score To Predict The Prognosis in Elderly Patients With Acute Coronary SyndromeFachry MuhammadNo ratings yet
- KardioDocument14 pagesKardioIboy ZulhamNo ratings yet
- Factores para FNRDocument10 pagesFactores para FNRPOMYNo ratings yet
- Carotid JCPSP WaDocument4 pagesCarotid JCPSP Washakil11No ratings yet
- Body 2008Document5 pagesBody 2008brookswalshNo ratings yet
- Early Atherosclerosis in Rheumatoid Arthritis: A Case Control StudyDocument5 pagesEarly Atherosclerosis in Rheumatoid Arthritis: A Case Control StudychandanNo ratings yet
- JACC2011 58,8 - Pronostico Del TCDocument12 pagesJACC2011 58,8 - Pronostico Del TCRaul GascueñaNo ratings yet
- Jurnal Carolin SidhartaDocument13 pagesJurnal Carolin SidhartaCaroline SidhartaNo ratings yet
- Jurnal 1Document10 pagesJurnal 1fitri juliantiNo ratings yet
- Troponin Limit of Detection Plus Cardiac Risk Stratification Scores to Rule Out Acute Myocardial Infarction and 30-Day Major Adverse Cardiac Events in ED PatientsDocument5 pagesTroponin Limit of Detection Plus Cardiac Risk Stratification Scores to Rule Out Acute Myocardial Infarction and 30-Day Major Adverse Cardiac Events in ED Patientsbobbyboy23No ratings yet
- J Interven Cardiol. 2017 1-7.: Presented By: Dr. Yusrina BR Saragih Supervisor: DR - Dr. Zulfikri Mukhtar, Sp. JP (K)Document24 pagesJ Interven Cardiol. 2017 1-7.: Presented By: Dr. Yusrina BR Saragih Supervisor: DR - Dr. Zulfikri Mukhtar, Sp. JP (K)Yusrina Njoes SaragihNo ratings yet
- Preventive PCIDocument8 pagesPreventive PCIharfanmaulaNo ratings yet
- Academic Emergency Medicine - 2018 - Fernando - Prognostic Accuracy of the HEART Score for Prediction of Major AdverseDocument12 pagesAcademic Emergency Medicine - 2018 - Fernando - Prognostic Accuracy of the HEART Score for Prediction of Major Adversebobbyboy23No ratings yet
- Comparison of In-Hospital Outcome of Acute ST Elevation Myocardial Infarction in Patients With Versus Without Diabetes MellitusDocument7 pagesComparison of In-Hospital Outcome of Acute ST Elevation Myocardial Infarction in Patients With Versus Without Diabetes MellitusEsther DiazNo ratings yet
- 1459 FullDocument7 pages1459 FullBilal KabeerNo ratings yet
- Becattini 2018Document25 pagesBecattini 2018Snezana MihajlovicNo ratings yet
- TroponinDocument39 pagesTroponinBayu AgastiaNo ratings yet
- Dilbahar (Pakai)Document3 pagesDilbahar (Pakai)DamsidsahdamNo ratings yet
- Scot TrialDocument10 pagesScot TrialGP MHTGNo ratings yet
- Trombocytosis Essential PDFDocument5 pagesTrombocytosis Essential PDFKerin ArdyNo ratings yet
- Serum Concentrations of Adiponectin and Risk of Type 2 Diabetes Mellitus and Coronary Heart Disease in Apparently Healthy Middle-Aged MenDocument15 pagesSerum Concentrations of Adiponectin and Risk of Type 2 Diabetes Mellitus and Coronary Heart Disease in Apparently Healthy Middle-Aged MenEcha MagungNo ratings yet
- Correos Electrónicos jgc-16-12-880Document5 pagesCorreos Electrónicos jgc-16-12-880G RamirezNo ratings yet
- Research Article: Outcome Predictors in First-Ever Ischemic Stroke Patients: A Population-Based StudyDocument9 pagesResearch Article: Outcome Predictors in First-Ever Ischemic Stroke Patients: A Population-Based StudyFitri Amelia RizkiNo ratings yet
- Effects DMCEA01Document11 pagesEffects DMCEA01milmrch523No ratings yet
- The LancetDocument9 pagesThe LancetBarbara Sakura RiawanNo ratings yet
- Bismillah 4Document4 pagesBismillah 4kiki tuanaya1No ratings yet
- Elevated Triglycerides To High-Density Lipoprotein Cholesterol (TG/HDL-C) Ratio Predicts Long-Term Mortality in High-Risk PatientsDocument8 pagesElevated Triglycerides To High-Density Lipoprotein Cholesterol (TG/HDL-C) Ratio Predicts Long-Term Mortality in High-Risk PatientsIrwinNo ratings yet
- JKSR 74 75Document7 pagesJKSR 74 75何燕No ratings yet
- Goldstein CT-STAT JACC 2011Document11 pagesGoldstein CT-STAT JACC 2011Andiie ResminNo ratings yet
- 2017-Taravatmanesh, Et Al-2017 - Determining The Factors Associated With Cardiovascular Disease Recurrence Tehran Lipid and Glucose StudyDocument7 pages2017-Taravatmanesh, Et Al-2017 - Determining The Factors Associated With Cardiovascular Disease Recurrence Tehran Lipid and Glucose Studycipto susiloNo ratings yet
- Jccnursing v11n1p1 FaDocument9 pagesJccnursing v11n1p1 FaNoel Saúl Argüello SánchezNo ratings yet
- 1 s2.0 S0735109720344223 MainDocument12 pages1 s2.0 S0735109720344223 MainRizky AisNo ratings yet
- Background: Keywords: Endothelial Microparticles, GRACE Score, Myocardial Infarction, PlateletDocument6 pagesBackground: Keywords: Endothelial Microparticles, GRACE Score, Myocardial Infarction, PlateletLiseth Dsc BieberNo ratings yet
- Grace Steg2002Document6 pagesGrace Steg2002crsscribdNo ratings yet
- Impact of QRS Duration On Non ST-Segment Elevation Myocardial Infarction (From A National Registry)Document7 pagesImpact of QRS Duration On Non ST-Segment Elevation Myocardial Infarction (From A National Registry)galih rakasiwiNo ratings yet
- Tutorial ElectrocardiogramaDocument6 pagesTutorial ElectrocardiogramakodagaNo ratings yet
- 116 229 1 SMDocument6 pages116 229 1 SMsinlookerNo ratings yet
- Clinical Study ReportDocument5 pagesClinical Study ReportAlexandraCirlanNo ratings yet
- Comparison of Management and 30-Day Mortality of Acute Myocardial Infarction in Men Versus Women in EstoniaDocument7 pagesComparison of Management and 30-Day Mortality of Acute Myocardial Infarction in Men Versus Women in EstoniarevachaNo ratings yet
- Study of Pattern of Acute Myocardial Infarction in Tertiary Care Hospital of Ahmedabad, GujaratDocument6 pagesStudy of Pattern of Acute Myocardial Infarction in Tertiary Care Hospital of Ahmedabad, GujaratEditor_IAIMNo ratings yet
- Low Diagnostic Yield of Elective Coronary Angiography: Original ArticleDocument10 pagesLow Diagnostic Yield of Elective Coronary Angiography: Original ArticleDwitari Novalia HaraziNo ratings yet
- Keywords:-STS Score, MACE, CABGDocument6 pagesKeywords:-STS Score, MACE, CABGInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Uhr Ve MortaliteDocument8 pagesUhr Ve MortalitealitrnfbNo ratings yet
- Cardiac Risk AssessmentDocument4 pagesCardiac Risk Assessmentmonir61No ratings yet
- 302 Cardiovascular Risk: AssessmentDocument1 page302 Cardiovascular Risk: AssessmentLêHữuHoàiNo ratings yet
- Prognostic Utility of the HEART Score in the Observation UnitDocument5 pagesPrognostic Utility of the HEART Score in the Observation Unitbobbyboy23No ratings yet
- ESC Heart Failure - 2022 - Di Lisi - The New HFA ICOS Risk Assessment Tool To Identify Patients With Chronic MyeloidDocument6 pagesESC Heart Failure - 2022 - Di Lisi - The New HFA ICOS Risk Assessment Tool To Identify Patients With Chronic MyeloidLissaberti AmaliahNo ratings yet
- Clinical Study ReportDocument4 pagesClinical Study ReportTalal HajNo ratings yet
- (2016) Myocardial Infarction As A Thrombotic Complication of Essential Thrombocythemia and Polycythemia VeraDocument6 pages(2016) Myocardial Infarction As A Thrombotic Complication of Essential Thrombocythemia and Polycythemia Verarara.ppdsNo ratings yet
- Risk Factors For Ischemic Stroke Post Bone FractureDocument11 pagesRisk Factors For Ischemic Stroke Post Bone FractureFerina Mega SilviaNo ratings yet
- Association of Variability in Uric Acid and Future CliDocument7 pagesAssociation of Variability in Uric Acid and Future Clinguyenthanhluan2801No ratings yet
- Salim 2009Document6 pagesSalim 2009raden chandrajaya listiandokoNo ratings yet
- 2022 Aortic pulse wave velocity as adjunct risk marker for assessingDocument17 pages2022 Aortic pulse wave velocity as adjunct risk marker for assessingIbrahimNo ratings yet
- Principle and Practice of CT in Cardiac AssessmentDocument47 pagesPrinciple and Practice of CT in Cardiac AssessmentSofia KusumadewiNo ratings yet
- Treatment Option 1Document6 pagesTreatment Option 1Elena-Dana OpreaNo ratings yet
- Incidence of Acute Myocardial Infarction in The Evolution of Dialysis PatientsDocument8 pagesIncidence of Acute Myocardial Infarction in The Evolution of Dialysis PatientsYola NewaryNo ratings yet
- Atherosclerosis 2007Document8 pagesAtherosclerosis 2007Chalikias GeorgeNo ratings yet
- Association of Statin Use and The Risk of End-Stage Renal Disease, A Nationwide On Asia Population Based CaseDocument5 pagesAssociation of Statin Use and The Risk of End-Stage Renal Disease, A Nationwide On Asia Population Based CasezikryauliaNo ratings yet
- Original Article: Prognostic Value of TIMI Score Versus GRACE Score in ST-segment Elevation Myocardial InfarctionDocument9 pagesOriginal Article: Prognostic Value of TIMI Score Versus GRACE Score in ST-segment Elevation Myocardial InfarctionDavy JonesNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyFrom EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyRating: 1 out of 5 stars1/5 (1)
- MGL Avionics Lycoming Engine Sender InstallationDocument14 pagesMGL Avionics Lycoming Engine Sender InstallationTiago AraújoNo ratings yet
- Shock TubeDocument11 pagesShock TubeyoannlegNo ratings yet
- TCSDocument2 pagesTCSSana IqbalNo ratings yet
- Question Bank - AM - IIIDocument5 pagesQuestion Bank - AM - IIIYashi SinghNo ratings yet
- FinalDocument48 pagesFinalSujan KhadkaNo ratings yet
- Simslim Sl-8 Quick Reference Guide: Cardiac Output: Expanded Computational Constants (CC)Document1 pageSimslim Sl-8 Quick Reference Guide: Cardiac Output: Expanded Computational Constants (CC)biomedicaNo ratings yet
- Noise Pollution and Its Control in Textile Industry: A of Searc 26Document6 pagesNoise Pollution and Its Control in Textile Industry: A of Searc 26Nakib Ibna BasharNo ratings yet
- c170 TP F.H.L. Thassos White 01Document5 pagesc170 TP F.H.L. Thassos White 01Micheal B HaizenNo ratings yet
- Eye Safety of IREDsDocument17 pagesEye Safety of IREDsЕвгений МихайловNo ratings yet
- Chelating Agents-Organic Vs SyntheticDocument2 pagesChelating Agents-Organic Vs SyntheticI. Murali KrishnaNo ratings yet
- Cheatsheet X3Dom - Nodo Atributos: TransparencyDocument2 pagesCheatsheet X3Dom - Nodo Atributos: TransparencyaswdNo ratings yet
- DS HP 1000 6 Differential en Us 17171Document2 pagesDS HP 1000 6 Differential en Us 17171behnamatgNo ratings yet
- Sasmo 2017 Grade-10Document19 pagesSasmo 2017 Grade-10Angela BebeNo ratings yet
- Synopsis On "Massive Parallel Processing (MPP) "Document4 pagesSynopsis On "Massive Parallel Processing (MPP) "Jyoti PunhaniNo ratings yet
- Social and Economics Lecture NoteDocument104 pagesSocial and Economics Lecture NoteBeka SolomonNo ratings yet
- Mesoporous Materials: Presented by Mannu Kaur M.Tech NST 1 Year (2 Sem) 00740801015Document38 pagesMesoporous Materials: Presented by Mannu Kaur M.Tech NST 1 Year (2 Sem) 00740801015Zarwin FadhlinNo ratings yet
- Lis CXL ProDocument16 pagesLis CXL ProSooo NoNo ratings yet
- Lecture05 FVM2Document48 pagesLecture05 FVM2alejandrovelez100% (1)
- Autosar Sws PdurouterDocument121 pagesAutosar Sws PdurouterHunter HunterNo ratings yet
- EEE 2104 Lab Report 01Document7 pagesEEE 2104 Lab Report 01shohim603No ratings yet
- DAA Lab Using JavaDocument53 pagesDAA Lab Using JavalakaasasiNo ratings yet
- Module 3 Animated Single Cycle and Multi Cycle Data PathDocument29 pagesModule 3 Animated Single Cycle and Multi Cycle Data PathAvv ReddyNo ratings yet
- Mechanical Engineering PrinciplesDocument11 pagesMechanical Engineering PrinciplesViraj KadamNo ratings yet
- Hydranautics ESPA2 LD Low Fouling Membrane Element LenntechDocument1 pageHydranautics ESPA2 LD Low Fouling Membrane Element Lenntechzerocool86No ratings yet
- GenChem11 Q1 M6Document21 pagesGenChem11 Q1 M6kanekiNo ratings yet
- ENRG 403-Assignment 03Document4 pagesENRG 403-Assignment 03malhajry227No ratings yet
- M2 Fuel System DAIHATSUDocument105 pagesM2 Fuel System DAIHATSUDeni AlamsyahNo ratings yet
- Datasheet 53315Document30 pagesDatasheet 53315Bladimir AngamarcaNo ratings yet