Environmental Emergencies Heat Exhaustion Heatstroke
Environmental Emergencies Heat Exhaustion Heatstroke
Uploaded by
pauchanmnlCopyright:
Available Formats
Environmental Emergencies Heat Exhaustion Heatstroke
Environmental Emergencies Heat Exhaustion Heatstroke
Uploaded by
pauchanmnlOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Environmental Emergencies Heat Exhaustion Heatstroke
Environmental Emergencies Heat Exhaustion Heatstroke
Uploaded by
pauchanmnlCopyright:
Available Formats
ENVIRONMENTAL EMERGENCIES
Heatstroke
Heat Exhaustion
Heatstroke is a medical emergency that can result in significant
morbidity and mortality. It is defined as the combination of
hyperpyrexia (105 F [40.6 C]) and neurologic symptoms. It is
caused by a shutdown or failure of the heat-regulating mechanisms of
the body.
Heat exhaustion is the inadequacy or the collapse of peripheral
circulation due to volume and electrolyte depletion. Heat exhaustion
is one condition in the spectrum of heat-related illnesses, including
heat rash, heat edema, heat cramps, and heat syncope. Untreated heat
exhaustion may progress to heatstroke.
Primary Assessment and Interventions
Expect the patient to be alert without significant
cardiorespiratory or neurologic compromise.
If vital functions are significantly impaired, suspect
secondary condition, such as MI or stroke.
Subsequent Assessment
Obtain history of headache, fatigue, dizziness, muscle
cramping, and nausea.
Inspect skin usually pale, ashen, and moist.
The temperature may be normal, slightly elevated, or as
high as 104 F (40 C).
Measure vital signs for hypotension, orthostatic changes,
tachycardia, and tachypnea.
The patient will be awake but may give a history of syncope
or confusion.
Laboratory analysis will show hemoconcentration and
hyponatremia (if sodium depletion is the primary problem)
or hypernatremia (if water depletion is the primary
problem).
The ECG may show dysrhythmias without evidence of
infarction.
General Interventions
Move the patient to a cool environment, and remove all
clothing.
Position the patient supine with the feet slightly elevated.
If the patient complains of nausea or vomiting, do not give
fluids by mouth.
Start an I.V. line with Ringer's lactate or normal saline until
electrolyte results are confirmed.
Monitor the patient for changes in the cardiac rhythm and
vital signs. Vital signs should be taken at least every 15
minutes until the patient is stable.
Provide fans and cool sponge baths as cooling methods.
Provide patient education.
o
Advise the patient to avoid immediate reexposure
to high temperatures; the patient may remain
hypersensitive to high temperatures for a
considerable length of time.
Emphasize the importance of maintaining an
adequate fluid intake, wearing loose clothing, and
reducing activity in hot weather.
Athletes should monitor fluid losses, replace fluids,
and use a gradual approach to physical
conditioning, allowing sufficient time for
acclimatization.
Primary Assessment and Interventions
Assess airway, breathing, and circulation.
LOC may be altered.
Expect to intervene immediately if cardiovascular collapse
occurs.
Subsequent Assessment
Obtain a history from accompanying person about
environmental conditions, activity, underlying health, and
medications that may have contributed to heatstroke.
Perform a neurologic assessment.
o
Initially, the patient may exhibit bizarre behavior or
irritability. This may progress to confusion,
combativeness, deliriousness, and coma.
Other central nervous system (CNS) disturbances
include tremors, seizures, fixed and dilated pupils,
and decerebrate or decorticate posturing.
Assess vital signs.
o
Temperature greater than 105 F.
Hypotension.
Rapid pulse; may be bounding or weak.
Rapid respirations.
The skin may appear flushed and hot; in early heatstroke,
the skin may be moist, but, as the heatstroke progresses, the
skin will become dry as the body loses its ability to sweat.
ABGs show metabolic acidosis.
General Interventions
Provide cooling measures.
o
o
o
o
o
o
o
o
Reduce the core (internal) temperature to 102 F
(38.9 C) as rapidly as possible.
Evaporative cooling is the most efficient. Spray
tepid water on the skin while electric fans are used
to blow continuously over the patient to augment
heat dissipation.
Apply ice packs to neck, groin, axillae, and scalp
(areas of maximal heat transfer).
Soak sheets/towels in ice water and place on
patient,
using
fans
to
accelerate
evaporation/cooling rate.
Immersion in cold water is contraindicated.
If the temperature fails to decrease, initiate core
cooling: iced saline lavage of stomach, cool fluid
peritoneal dialysis, cool fluid bladder irrigation, or
cool fluid chest irrigations.
Place the patient on a hypothermia blanket.
Discontinue active cooling when the temperature
reaches 102 F. In most cases, this will reduce the
chance of overcooling because the body
temperature will continue to fall after cessation of
cooling.
Oxygenate patient to supply tissue needs that are
exaggerated by the hypermetabolic condition: 100%
nonrebreather mask or intubate the patient if necessary to
support a failing cardiorespiratory system.
Monitor condition.
o
Replace fluids.
o
o
o
Start I.V. infusion using Ringer's lactate to replace
fluid losses, maintain adequate circulation, and
facilitate cooling.
At least one I.V. line should be a central line.
Fluid replacement is based on the patient's
response and laboratory results.
Other measures:
o
Dialysis for renal failure.
Diuretics, such as mannitol (Osmitrol), to promote
diuresis.
Anticonvulsant agents to control seizures.
o
o
Monitor and record the core temperature
continually during cooling process to avoid
hypothermia; also, hyperthermia may recur
spontaneously within 3 to 4 hours.
Monitor the vital signs continuously, including
ECG, CVP, blood pressure, pulse, and respiratory
rate.
Perform frequent (every 30 minutes) neurologic
assessments.
Potassium for hypokalemia and sodium
bicarbonate to correct metabolic acidosis,
depending on laboratory results.
Antipyretics are not useful in treating heatstroke.
They may contribute to the complications of
coagulopathy and hepatic damage.
Intense shivering may be controlled by diazepam
(Valium). Shivering will generate heat and increase
the metabolic rate.
Patients with depleted clotting factors may be
treated with platelets or fresh frozen plasma.
Insert an indwelling catheter with a urometer, and measure
urine output at least hourly acute tubular necrosis is a
complication of heatstroke.
Perform continuous ECG monitoring and frequent
cardiovascular assessments for possible ischemia,
infarction, and dysrhythmias.
Perform serial laboratory testing (clotting parameters,
electrolytes, glucose, and serum enzymes).
The patient should be admitted to an intensive care unit
(ICU); complications can occur, including heart failure,
cardiovascular collapse, hepatic failure, renal failure,
disseminated
intravascular
coagulation,
and
rhabdomyolysis.
Monitor the patient for the development of seizures, and
provide for a safe environment in case of seizures.
Frostbite
Frostbite is trauma due to exposure to freezing temperatures that
cause actual freezing of the tissue fluids in the cell and intracellular
spaces, resulting in vascular damage. The areas of the body most
likely to develop frostbite are the earlobes, cheeks, nose, hands, and
feet. Frostbite may be classified as frostnip (initial response to cold,
reversible), superficial frostbite, and deep frostbite.
Primary Assessment and Interventions
If not alert, assess airway, breathing, and circulation.
Deficits may indicate coexisting hypothermia or underlying
condition.
Protect frostbitten
interventions.
tissue
while
performing
other
Subsequent Assessment
Frostnip
History of gradual onset.
Skin appears white.
Numb, pain-free.
Superficial Frostbite
Damage is limited to the skin and subcutaneous tissue.
The skin will appear white and waxy.
On palpation, the skin will feel stiff but the underlying
tissue will be pliable, soft, and have its normal bounce.
Sensation is absent.
Deep Frostbite
Skin will appear white, yellow-white, or mottled blue-white.
On palpation, the surface will feel frozen and the underlying
tissue will feel frozen and hard.
The affected part is completely insensitive to touch.
General Interventions
Frostnip may be treated by placing a warm hand over the
chilled area.
Leave the frostbitten area alone until definitive rewarming is
undertaken. Pad the extremity to prevent damage from
trauma.
Handle the part gently to avoid further mechanical injury.
Remove all constricting clothing that can impair circulation,
including watchbands and rings.
Rewarming:
o
Rewarm the extremity by controlled and rapid
rewarming. Rewarm with a temperature of 98.6 F
to 104 F (37 C to 40 C) in a fairly large, tepid
water bath where the part can be fully immersed
without touching the side or bottom. If clothing,
socks, or gloves are frozen to the extremity, they
should be left on and removed after rewarming.
More warm water may be added to the container by
removing some cooled water and adding warm
water.
Slow rewarming is less effective and may increase
tissue damage.
Dry heat is not recommended for rewarming.
The rewarming procedure may take 20 to 30
minutes.
Rewarming is complete when the area is warm to
the touch and pink or flushed.
Do not rub or massage a frostbitten extremity. The
ice crystals in the tissue will lacerate delicate
tissue.
o
o
Opioids for pain control.
Antibiotics if there is an open wound.
Tetanus prophylaxis.
Protect the thawed part from infection. Large blisters may
develop in 1 hour to a few days after rewarming; these
blisters should not be broken.
Place sterile gauze or cotton between affected fingers/toes to
absorb moisture.
Use strict aseptic technique during dressing changes.
Frostbite injuries make the patient susceptible to infection.
Make sure any dressings are loosely applied.
Elevate the part to help control swelling.
Use a foot cradle to prevent contact with bedding if the feet
are involved prevents further tissue injury.
Perform a physical assessment to look for concomitant
injury (soft-tissue injury, dehydration, alcohol coma, fat
embolism due to fracture, immobility).
Restore electrolyte balance; dehydration and hypovolemia
occur frequently in frostbite victims.
Whirlpool bath for the affected extremity to aid circulation,
debride dead tissue, and help prevent infection.
Escharotomy (incision through the eschar) to prevent further
tissue damage, allow for normal circulation, and permit joint
motion.
Fasciotomy (incision in fascia to release pressure on the
muscles, nerves, blood vessels) to treat compartment
syndrome.
Encourage hourly active motion of the affected digits to
promote maximum restoration of function and to prevent
contractures.
Advise patient not to use tobacco because of the
vasoconstrictive effects of nicotine, which further reduce the
already deficient blood supply to injured tissues.
Perform serial laboratory testing (urinalysis and serum
enzymes) to monitor for the complications of
rhabdomyolysis and subsequent renal failure.
Hypothermia
Hypothermia is a condition in which the core (internal)
temperature of the body is less than 95 F (35 C) as a result
of exposure to cold. In response to a decreased core
temperature, the body will attempt to produce or conserve
more heat by (1) shivering, which produces heat through
muscular activity; (2) peripheral vasoconstriction, to
decrease heat loss; and (3) raising the basal metabolic rate.
Hypothermia may be classified as mild, moderate, or severe.
Assess airway and breathing.
o
o
Pharmacologic interventions:
Primary Assessment and Interventions
Spontaneous respirations may be extremely slow
and imperceptible.
Assist
breathing
and
oxygenation
with
supplemental O2 at 100% or a bag-valve mask
device.
If intubation is necessary, extreme caution should
be used because ventricular fibrillation may be
precipitated.
Assess circulation.
o
If the body temperature falls below 86 F (30 C),
the heart sounds may not be audible even if the
heart is still beating. Tissues conduct sound poorly
at low temperatures.
Blood pressure readings may be extremely difficult
to hear because cold tissue conducts sound waves
poorly.
Pupil reflexes may be blocked by a decrease in
cerebral blood flow, so the pupils may appear fixed
and dilated.
A patient with a heartbeat may present like a
patient in cardiac arrest with fixed dilated pupils,
no pulse, and no blood pressure. Provide CPR until
further evaluation through ECG and hemodynamic
monitoring.
Subsequent Assessment
There is progressive deterioration marked by apathy, poor
judgment, ataxia, dysarthria, drowsiness and, eventually,
coma.
Speech is slow and may be slurred.
Shivering may be suppressed below a temperature of 90 F
(32.2 C).
Cardiac dysrhythmias cold disrupts the conduction system
of the heart, and a variety of dysrhythmias may be seen. A
hypothermic heart is extremely susceptible to ventricular
fibrillation. Very cold hearts do not respond to drugs or
defibrillation.
The heartbeat and the blood pressure may be so weak that
the peripheral pulsations become undetectable.
Urine output may increase in response to peripheral
vasoconstriction cold diuresis.
Initial tachypnea followed by slow and shallow respirations,
possibly two or three per minute in severe hypothermia.
Fruity or acetone odor to the breath because the body may
be metabolizing fat as a result of decreased insulin levels.
General Interventions
Goal: rewarm without precipitating cardiac dysrhythmias.
Supportive Measures
Handle the patient carefully and gently to avoid triggering
ventricular fibrillation.
Continuously monitor core temperatures with a low reading
rectal thermometer.
Continuously monitor ECG. Because you may be unable to
obtain a pulse due to the hypothermia, rely on the cardiac
monitor to determine the need for CPR.
Monitor the patient's condition through vital signs, CVP,
urine output, ABG values, and blood chemistry
determinations.
Maintain an arterial line for recording blood pressure and to
facilitate blood sampling allows rapid detection of
acidbase disturbances and assessment of adequacy of
ventilation and oxygenation.
Start I.V. therapy with normal saline. Ringer's lactate is not
recommended because the cold liver may not be able to
metabolize the lactate.
Rewarming Techniques
The type of rewarming depends on the degree of hypothermia.
Rewarming should continue until the core temperature is 93.2 F
(34 C). If the patient is in cardiac arrest, rewarming should continue
until a temperature of 89.6 F (32 C) has been reached. Death in
hypothermia is defined as a failure to revive after rewarming.
Passive external rewarming (temperature above 82.4 F [28
C]).
o Remove all the wet or cold clothing, and replace
with warm clothing.
o Provide insulation by wrapping the patient in
several blankets.
o Provide warmed fluids to drink.
o
Toxicology is the study of the harmful effect of various substances on
the body. Poisons are substances that are harmful to the body no
matter how much or in what manner they enter the body. Drugs
become toxic when they are taken in excess quantities or manners
that are not therapeutic. Alcohol is considered a drug. The treatment
goals of toxicologic emergencies are first, supportive; second, to
prevent or minimize absorption; third, to provide an antidote.
Ingested Poisons
Ingested poisons can produce immediate or delayed effects.
Immediate injury is caused when the poison is caustic to the body
tissues (ie, a strong acid or a strong alkali). Other ingested poisons
must be absorbed into the bloodstream before they become harmful.
Ingested poisoning may be accidental or intentional.
Primary Assessment and Interventions
Maintain an open airway some ingested substances may
cause soft tissue swelling of the airway.
Attain control of the airway, ventilation, and oxygenation; in
the absence of cerebral or renal damage, the patient's
prognosis depends largely on successful management and
support of vital functions.
Subsequent Assessment
Disadvantage: slow process.
Provide external heat for the patient warm hot
water bottles to the armpits, neck, or groin. (Do not
apply hot water bottles directly to the skin.)
Warm water immersion.
Disadvantages:
Causes peripheral vasodilation, returning
cool blood to the core, causing an initial
lowering of the core temperature.
Acidosis due to the washing out of lactic
acid from the peripheral tissues.
An increase in the metabolic demands
before the heart is warmed to meet these
needs.
Active core rewarming (temperature below 82.4 F).
Identify the poison.
o
Active external rewarming (temperature above 82.4 F).
o
TOXICOLOGIC EMERGENCIES
Try to determine the product taken: where, when,
why, how much, who witnessed the event, time
since ingestion.
Call the poison control center in the area if an
unknown toxic agent has been taken or if it is
necessary to identify an antidote for a known toxic
agent.
Continue the focused assessment, observing any significant
deviations from normal. Different poisons will affect the
body in different ways.
Obtain blood and urine tests for toxicology screening.
Gastric contents may also be sent for toxicology screening
in serious ingestions.
Monitor neurologic status, including mentation; monitor the
course of vital signs and neurologic status over time.
Monitor for fluid and electrolyte imbalance.
General Interventions
Supportive Care
Initiate large-bore I.V. access.
Administer oxygen for respiratory depression.
Inhalation of warmed, humidified oxygen by mask
or ventilator.
Warmed I.V. fluids.
Warmed gastric lavage.
Monitor and treat shock.
Peritoneal dialysis with warmed standard dialysis
solution.
Mediastinal irrigation through open thoracotomy
has been used successfully but has serious
complications.
Cardiopulmonary bypass.
Prevent aspiration of gastric contents by positioning (on side
with head down), use of oropharyngeal airway, and
suctioning.
Give supportive care to maintain vital organ systems.
Insert an indwelling urinary catheter to monitor renal
function.
Support the patient having seizures; many poisons excite the
CNS, or the patient may convulse from oxygen deprivation.
Monitor and treat for complications: hypotension, coma,
cardiac dysrhythmias, and seizures.
o
o
Disadvantage of active core rewarming is the
invasiveness of the procedures.
Minimizing Absorption
The primary method for preventing or minimizing
absorption is to administer activated charcoal with a
cathartic to hasten excretion. Newer superactivated
charcoals can reduce absorption of a toxic substance by as
much as 50%. Administering activated charcoal plus a
cathartic is just as effective or more effective than gastric
lavage.
o Administration of oral-activated charcoal absorbs
the poison on the surface of its particles and allows
it to pass with the stool. Multiple doses may be
administered.
o Activated charcoal is usually mixed tap water to
make a slurry.
If the carbon monoxide poisoning is due to smoke
inhalation, stridor (indicative of laryngeal edema
due to thermal injury) may be present.
Primary Interventions
Provide 100% oxygen by tight-fitting mask. (The
elimination half-life of carboxyhemoglobin, in serum, for a
person breathing room air is 5 hours 20 minutes. If the
patient breathes 100% oxygen, the half-life is reduced to 80
minutes; 100% oxygen in a hyperbaric chamber will reduce
the half-life to 23 minutes [treatment of choice].)
Intubate if necessary to protect the airway.
Subsequent Assessment
A thorough history is important: determine the type and
length of exposure as well as possible other fumes inhaled.
An underlying anemia, cardiac disease, or pulmonary
disease may place a person at higher risk.
Gastric lavage for the obtunded patient (see Procedure
Guidelines 35-5, pages 1164 and 1165). Save gastric
aspirate for toxicology screens. This procedure is
controversial.
Determine LOC the patient may appear intoxicated from
cerebral hypoxia; confusion may progress rapidly to coma.
Assess complaints of headache, muscular weakness,
palpitation, dizziness.
Procedures to enhance the removal of the ingested substance
if the patient is deteriorating.
o Forced diuresis with urine pH alteration to enhance
renal clearance.
o Hemoperfusion (process of passing blood through
an extracorporeal circuit and a cartridge containing
an adsorbent, such as charcoal, after which the
detoxified blood is returned to patient).
o Hemodialysis used in selected patients to purify
blood and accelerate the elimination of circulating
toxins.
o Repeated doses of charcoal for binding
nonabsorbed drugs/toxins.
o Gastric lavage may be used in conjunction with
activated charcoal and a cathartic to maximize
elimination of the substance.
Inspect skin: may be pink, cherry red, or cyanotic and pale
skin color is not a reliable sign.
Monitor vital signs: increased respiratory and pulse rates are
generally present. Be alert for altered breathing patterns and
respiratory failure.
Listen for rales or wheezes in the lungs (with smoke
inhalation, indicates acute respiratory distress syndrome).
Obtain arterial blood samples for carboxyhemoglobin
levels.
o Normal is less than 12%.
Providing an Antidote
An antidote is a chemical or physiologic antagonist that will
neutralize the poison.
Administer the specific antidote as early as possible to
reverse or diminish effects of the toxin.
Carbon Monoxide Poisoning
Carbon monoxide poisoning is an example of an inhaled poison and
is the result of the inhalation of the products of incomplete
hydrocarbon combustion. It may occur as an industrial or household
accident or as an attempted suicide. Carbon monoxide exerts its toxic
effect by binding to circulating hemoglobin to reduce the oxygencarrying capacity of the blood. The affinity between carbon
monoxide and hemoglobin is 200 to 300 times that between oxygen
and hemoglobin. (Carbon monoxide combines with hemoglobin to
form carboxyhemoglobin.) As a result, tissue anoxia occurs.
Primary Assessment
Psychiatric evaluations may be done after the patient is
stabilized.
Assess airway and breathing.
o
Respiratory depression may be present.
Severe carbon monoxide poisoning is present when
levels are greater than 30% to 40%.
General Interventions
History of exposure to carbon monoxide justifies immediate
treatment.
Goals are to reverse cerebral and myocardial hypoxia and
hasten carbon monoxide elimination.
Give 100% oxygen at atmospheric or hyperbaric pressures
to reverse hypoxia and accelerate elimination of carbon
monoxide. Patients should receive hyperbaric oxygen for
CNS or cardiovascular system dysfunction.
Use continuous ECG monitoring, treat dysrhythmias, and
correct acidbase and electrolyte abnormalities.
Observe the patient constantly psychoses, spastic paralysis,
visual disturbances, and deterioration of personality may
persist after resuscitation and may be symptoms of
permanent CNS damage.
Insect Stings
Insect stings or bites are injected poisons that can produce either
local or systemic reactions. Local reactions are characterized by pain,
erythema, and edema at the site of injury. Systemic reactions usually
begin within minutes and produce mild to severe and life-threatening
reactions.
Primary Assessment and Interventions
Assess airway, breathing, and circulation.
Anaphylactic reactions may produce unconsciousness,
laryngeal edema, and cardiovascular collapse.
Epinephrine is the drug of choice the amount and route
depend on the severity of the reaction.
Administer a
bronchospasm.
Initiate an I.V. with Ringer's lactate.
Prepare for CPR.
bronchodilator
to
help
relieve
the
Subsequent Assessment
Obtain history of insect sting, previous exposure, and
allergies.
Inspect skin for local reaction erythema, edema, pain at site
of injury as well as generalized pruritus, urticaria, and
angioedema.
Continue to monitor blood pressure and respiratory status
for dyspnea, wheezing, and stridor.
General Interventions
Apply ice packs to site to relieve pain.
Elevate extremity with large edematous local reaction.
Administer oral antihistamine for local reactions.
Clean the wound thoroughly with soap and water or an
antiseptic solution.
Administer tetanus prophylaxis if not up to date.
Provide patient education.
Spray garbage cans with rapid-acting
insecticide, and keep areas meticulously
clean.
Snakebites
The majority of snakes in the United States are not poisonous. The
poisonous varieties are pit vipers (rattlesnakes and copperheads) and
coral snakes. Bites by these snakes may result in envenomation, an
injected poisoning.
Primary Assessment and Interventions
Assess airway, breathing, and circulation if patient is not
alert.
Severe envenomation may lead to neurotoxicity with
respiratory paralysis, shock, coma, and death.
Be prepared to resuscitate and provide advanced life
support.
Subsequent Assessment
Get a description of the snake, the time of the snakebite, and
the location of the bite. Bites to the head and trunk may
progress more rapidly and be more severe.
o Pit vipers have triangular heads, vertical pupils,
indentations between the eyes and nostrils, and
long fangs.
o Coral snakes are small, brightly colored, with short
fangs and teeth behind them, and with a series of
bands of yellow, red, yellow, and black (in that
order).
Always have epinephrine on hand (EpiPen).
Wear medical emergency bracelets indicating
hypersensitivity.
Instructions when sting occurs:
Assess for local reactions burning, pain, swelling, and
numbness at the site. Local reactions to coral snakebites
may be delayed several hours and may be very mild.
A few hours after the bite, hemorrhagic blisters may occur
at the site, and the entire extremity may become edematous.
Watch for signs of systemic reactions, including nausea,
sweating, weakness, lightheadedness, initial euphoria
followed by drowsiness, difficulty in swallowing, paralysis
of various muscle groups, signs of shock, seizures, and
coma.
Monitor vital signs closely because tachycardia or
bradycardia may develop.
Take epinephrine immediately if stung.
Remove stinger with one quick scrape of
fingernail.
Do not squeeze venom sac because this
may cause additional venom to be
injected.
Report to nearest health care facility for
observation.
Avoid exposure.
Avoid locales with stinging insects (camp
and picnic sites).
Stay away from insect feeding areas
flower beds, ripe fruit orchards, garbage,
fields of clover.
Avoid going barefoot outdoors yellow
jackets may nest on ground.
Avoid perfumes, scented soaps, bright
colors attract bees.
Keep car windows closed.
General Interventions
Keep the patient calm and at rest in a recumbent position
with the affected extremity immobilized.
Administer oxygen.
Start an I.V. line with normal saline or Ringer's lactate.
Administer antivenin and be alert to allergic reaction
(antivenin is horse serum-based).
Administer vasopressors in the treatment of shock.
Monitor for bleeding, and administer blood products for
coagulopathy.
You might also like
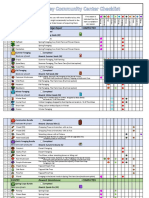
- Stardew Valley Community Center ChecklistDocument7 pagesStardew Valley Community Center Checklistpauchanmnl100% (2)
- AMEN-RA'S AGE INHIBITION REGIMEN (AIR), AN ABSTRACT - (Summer 2015)Document4 pagesAMEN-RA'S AGE INHIBITION REGIMEN (AIR), AN ABSTRACT - (Summer 2015)everydaywarriorsNo ratings yet
- Mental Health Conditions (Summarized Test Submitted by Melvin M. Pernez)Document29 pagesMental Health Conditions (Summarized Test Submitted by Melvin M. Pernez)Melvin Pernez100% (3)
- 4B - Specific Heat: Part 1 - Different MaterialsDocument5 pages4B - Specific Heat: Part 1 - Different MaterialsYessenia Velasquez ZuñigaNo ratings yet
- National TB ProgramDocument54 pagesNational TB Programarlian malihanNo ratings yet
- Heat StrokeDocument22 pagesHeat StrokeCrizza Maglasang100% (2)
- Environmental Emergencies ParamedicDocument90 pagesEnvironmental Emergencies ParamedicPaulhotvw67100% (2)
- Contraceptive TechnologyDocument68 pagesContraceptive TechnologySravanthi Karingula100% (1)
- Intern Note 終極版Document168 pagesIntern Note 終極版楊芷No ratings yet
- DRUG STUDY - Sodium BicarbonateDocument1 pageDRUG STUDY - Sodium Bicarbonatejulesubayubay54280% (1)
- Bizmanualz Medical Office Policies and Procedures SampleDocument7 pagesBizmanualz Medical Office Policies and Procedures SampleYe Phone0% (1)
- HANDOUT1Document6 pagesHANDOUT1Mark Elben TeodoroNo ratings yet
- Environmental EmergenciesDocument38 pagesEnvironmental EmergenciesIshaBrijeshSharmaNo ratings yet
- Basicfirstaid0808 111113200207 Phpapp02Document46 pagesBasicfirstaid0808 111113200207 Phpapp02Liezel CauilanNo ratings yet
- Man Made DisastersDocument4 pagesMan Made DisastersMichelle Andreina Robalino RonquilloNo ratings yet
- SLRC Pedia PresentationDocument141 pagesSLRC Pedia Presentationapi-3764215100% (2)
- DO's and Dont's During DisasterDocument79 pagesDO's and Dont's During Disasterblack holeNo ratings yet
- Environmental EmergenciesDocument11 pagesEnvironmental EmergenciesDaily Ride Ph “Siege Custodio”No ratings yet
- Oxygen TherapyDocument20 pagesOxygen TherapyBeri NyuydzefonNo ratings yet
- RLE NCMB 314-M2-CU8 Cardiovascular ChangesDocument5 pagesRLE NCMB 314-M2-CU8 Cardiovascular ChangesJordz PlaciNo ratings yet
- Jemal Yimam Jibril Berhanu Kalkidan Zenebe: Presented byDocument57 pagesJemal Yimam Jibril Berhanu Kalkidan Zenebe: Presented byVincent SerNo ratings yet
- Family Preparedness PlanDocument14 pagesFamily Preparedness PlanDanica FrancoNo ratings yet
- Family Emergency Communication Plan - Create Your OwnDocument17 pagesFamily Emergency Communication Plan - Create Your OwnAgustin PeraltaNo ratings yet
- Environmental EmergenciesDocument8 pagesEnvironmental EmergenciesJanfreid BaniquedNo ratings yet
- Student Version Skin Wounds 1119 9 11 13Document68 pagesStudent Version Skin Wounds 1119 9 11 13brandywestonNo ratings yet
- NCP (Burn)Document2 pagesNCP (Burn)Maricel R. ManabatNo ratings yet
- Gay Lussac's Law 12 3Document9 pagesGay Lussac's Law 12 3FFF100% (2)
- Dengue Fever PresentationDocument11 pagesDengue Fever Presentationhira khanNo ratings yet
- Disaster Management: Submitted To - Mrs. Bindu Submitted by - Jagwinder Singh Sekhon Roll No. - 37Document39 pagesDisaster Management: Submitted To - Mrs. Bindu Submitted by - Jagwinder Singh Sekhon Roll No. - 37Jai SinghrandhawaNo ratings yet
- FrostbiteDocument19 pagesFrostbiteKhadim Hussain Shah100% (2)
- Oxygenation and Fluids 2023Document129 pagesOxygenation and Fluids 2023Ted ChrisNo ratings yet
- Heat Stroke, Cramps and Exhaustion (Report)Document29 pagesHeat Stroke, Cramps and Exhaustion (Report)Operio AndreaNo ratings yet
- NCM 118 - Lesson 8 (Acute Ischemic Heart Diseases)Document9 pagesNCM 118 - Lesson 8 (Acute Ischemic Heart Diseases)Bobby Christian DuronNo ratings yet
- Body Mass IndexDocument15 pagesBody Mass Indexapi-266437595100% (1)
- Body TemperatureDocument26 pagesBody TemperatureChinniah RamkumarNo ratings yet
- Introduction To Critical Care NursingDocument33 pagesIntroduction To Critical Care NursingIbrahim RegachoNo ratings yet
- Head and Neck ExaminationDocument25 pagesHead and Neck ExaminationDarryl Betts100% (1)
- Acute Ischaemic StrokeDocument37 pagesAcute Ischaemic StrokeDr. Sarthak MishraNo ratings yet
- Endocrine SystemDocument43 pagesEndocrine Systemwieka mawie100% (1)
- Nursing - CS - Bipolar I Vs Bipolar II Comparison - 04Document1 pageNursing - CS - Bipolar I Vs Bipolar II Comparison - 04TUALLA KAL-EL JOHNRAY 3ANo ratings yet
- Checklist 66: Priming Iv Tubing: Disclaimer: Always Review and Follow Your Hospital Policy Regarding This Specific SkillDocument8 pagesChecklist 66: Priming Iv Tubing: Disclaimer: Always Review and Follow Your Hospital Policy Regarding This Specific SkillMarie FatimaNo ratings yet
- By: Aileen C. Contreras-Limjoco M.DDocument48 pagesBy: Aileen C. Contreras-Limjoco M.Dclara jocomilNo ratings yet
- Ret DemsDocument103 pagesRet DemsPRECIOUS LOVE LAGRIMASNo ratings yet
- Communicable and Infectious Disease Nursing-NewDocument15 pagesCommunicable and Infectious Disease Nursing-NewShandz de RosasNo ratings yet
- Burn & Scald: Pathophysiology Assessment of Burn WoundDocument19 pagesBurn & Scald: Pathophysiology Assessment of Burn WoundSyidah RoslanNo ratings yet
- NCM 102 Lec RespiDocument26 pagesNCM 102 Lec RespiLindsay NateNo ratings yet
- Tetanus PresentationDocument132 pagesTetanus PresentationRinrin de BelenNo ratings yet
- Vital Signs NCM 100 Skills Laboratory - EditedDocument175 pagesVital Signs NCM 100 Skills Laboratory - EditedrnrmmanphdNo ratings yet
- Quiz For Burn ManagementDocument3 pagesQuiz For Burn Managementfarmasi_hmNo ratings yet
- Unit - 2 Types of DisasterDocument52 pagesUnit - 2 Types of Disasterfree fireNo ratings yet
- Activity 2 NCM 117 SkillsDocument1 pageActivity 2 NCM 117 SkillsKyle Audrie ArcalasNo ratings yet
- Drowning: David Slocum MD Albany Medical CenterDocument39 pagesDrowning: David Slocum MD Albany Medical CenterPawan SujaneNo ratings yet
- When The Situation of Hazard Arise?: Hide Answer WorkspaceDocument5 pagesWhen The Situation of Hazard Arise?: Hide Answer WorkspaceChannelGNo ratings yet
- NCM 112 LEC Topic 13 Respiratory Infectious DiseasesDocument12 pagesNCM 112 LEC Topic 13 Respiratory Infectious DiseasesViviene Faye FombuenaNo ratings yet
- Family Disaster Plan: Here Will Your Family Be When Disaster Strikes? They Could Be AnywhereDocument4 pagesFamily Disaster Plan: Here Will Your Family Be When Disaster Strikes? They Could Be AnywhereJayTeeS6100% (1)
- Raynaud's DISEASEDocument3 pagesRaynaud's DISEASEkondame aisheeNo ratings yet
- Management of Patients With Burn InjuryDocument36 pagesManagement of Patients With Burn Injuryraghad awwad100% (1)
- Heart DiseaseDocument4 pagesHeart DiseasefidaauddinNo ratings yet
- First Aid: PoisoningDocument82 pagesFirst Aid: PoisoningSmaili TotoNo ratings yet
- Bioethics Lecture 1 NotesDocument5 pagesBioethics Lecture 1 NotesKyreliaNo ratings yet
- Heatstroke Sun Stroke Acute Management and PreventionDocument44 pagesHeatstroke Sun Stroke Acute Management and PreventionDedy SavradinataNo ratings yet
- Introduction To Psychiatric Nursing: Module 2: ConceptsDocument26 pagesIntroduction To Psychiatric Nursing: Module 2: ConceptsJoric MagusaraNo ratings yet
- Article 166320-PrintDocument21 pagesArticle 166320-PrintDoganNo ratings yet
- Nur 111 Session 21 Sas 1Document8 pagesNur 111 Session 21 Sas 1Zzimply Tri Sha UmaliNo ratings yet
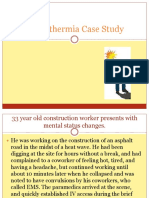
- Hyperthermia Case StudyDocument28 pagesHyperthermia Case StudyJanelle GimenezNo ratings yet
- 15-Temperature-Related-InjuriesDocument35 pages15-Temperature-Related-InjuriesKhirsten kaycee MillerNo ratings yet
- Frostbite and HypothermiaDocument43 pagesFrostbite and HypothermiaBlade DarkmanNo ratings yet
- Anime RecommendationsDocument8 pagesAnime Recommendationspauchanmnl100% (1)
- Sparkle - Kimi No Na WaDocument1 pageSparkle - Kimi No Na WapauchanmnlNo ratings yet
- Insights and Journal - CHANDocument7 pagesInsights and Journal - CHANpauchanmnlNo ratings yet
- Mass SongsDocument3 pagesMass SongspauchanmnlNo ratings yet
- Checklist For Technical CommitteeDocument2 pagesChecklist For Technical CommitteepauchanmnlNo ratings yet
- Progress NotesDocument2 pagesProgress NotespauchanmnlNo ratings yet
- Stanhope: Public Health Nursing, 9th EditionDocument2 pagesStanhope: Public Health Nursing, 9th EditionpauchanmnlNo ratings yet
- Competency Appraisal II Respiratory ExamDocument5 pagesCompetency Appraisal II Respiratory ExampauchanmnlNo ratings yet
- National Patient Safety Goals Effective January 1, 2015: Hospital Accreditation ProgramDocument17 pagesNational Patient Safety Goals Effective January 1, 2015: Hospital Accreditation ProgrampauchanmnlNo ratings yet
- QA Daily Report (Septmeber 9, 2016)Document2 pagesQA Daily Report (Septmeber 9, 2016)pauchanmnlNo ratings yet
- Handoff: Kurt A. Patton, MS, RPHDocument18 pagesHandoff: Kurt A. Patton, MS, RPHpauchanmnl100% (1)
- Communication Competencies For CliniciansDocument7 pagesCommunication Competencies For ClinicianspauchanmnlNo ratings yet
- SbarDocument2 pagesSbarpauchanmnlNo ratings yet
- Interpretation: S02 - Akshay Kumar-Fpsc Gurgaon Sector-57-GurgaonDocument4 pagesInterpretation: S02 - Akshay Kumar-Fpsc Gurgaon Sector-57-Gurgaonujjwal guptaNo ratings yet
- Fijación Occipito-Cervical PosteriorDocument2 pagesFijación Occipito-Cervical PosteriorJuan José BarretoNo ratings yet
- Reflection Paper Establishing Efficacy Based Single Arm Trials Submitted Pivotal Evidence Marketing - enDocument15 pagesReflection Paper Establishing Efficacy Based Single Arm Trials Submitted Pivotal Evidence Marketing - enMarcel Alexandru GainaNo ratings yet
- Endo Perio LesionsDocument24 pagesEndo Perio LesionsAneen Suresh0% (1)
- CHCCS305A Assist Clients With Medication WBKDocument252 pagesCHCCS305A Assist Clients With Medication WBKsareeee100% (2)
- Oxygen For Cluster Headaches: A GuideDocument25 pagesOxygen For Cluster Headaches: A GuidetriaclaresiaNo ratings yet
- Preoperative FastingDocument5 pagesPreoperative FastingsilviaemohNo ratings yet
- Dahl ConceptDocument3 pagesDahl ConceptmusaabsiddiquiNo ratings yet
- Color and LearningDocument9 pagesColor and LearningRodrigo HolguínNo ratings yet
- Cladribine V4 6.14Document2 pagesCladribine V4 6.14GabrielNo ratings yet
- Seligman 1995 PDFDocument10 pagesSeligman 1995 PDFEdy WallerNo ratings yet
- Fluid Ruminant AnalysisDocument5 pagesFluid Ruminant AnalysisGabriel Ivan Pantoja NuñezNo ratings yet
- Rabicip & I.V.Document51 pagesRabicip & I.V.buffetishere100% (2)
- α2-Adrenergic Agonists or Stimulants for Preschool-Age ChildrenDocument9 pagesα2-Adrenergic Agonists or Stimulants for Preschool-Age ChildrenZary GarcíaNo ratings yet
- House: Season One Episode 21: Three Stories These Observations Took Place Over An Hour Long EpisodeDocument2 pagesHouse: Season One Episode 21: Three Stories These Observations Took Place Over An Hour Long EpisodeAnonymous 5s6LNcyhSNo ratings yet
- Re Feeding SyndromeDocument18 pagesRe Feeding SyndromeHaoKeat HoeNo ratings yet
- Magnetic Elliptical StriderDocument15 pagesMagnetic Elliptical StriderJsuksNo ratings yet
- Group-Based Cardiac Rehabilitation Interventions. A Challenge For Physical and Rehabilitation Medicine Physicians: A Randomized Controlled TrialDocument32 pagesGroup-Based Cardiac Rehabilitation Interventions. A Challenge For Physical and Rehabilitation Medicine Physicians: A Randomized Controlled TrialKings AndrewNo ratings yet
- Spa Centers SlovakiaDocument8 pagesSpa Centers SlovakiaAsen NestorovNo ratings yet
- Role of Yogasanas and Naturopathy in PilesDocument2 pagesRole of Yogasanas and Naturopathy in PilesAbhaya Raj UpadhayaNo ratings yet
- Effectiveness of Oral Albendazole As A Treatment For Pediculosis CapitisDocument8 pagesEffectiveness of Oral Albendazole As A Treatment For Pediculosis CapitisFlorensia WodaNo ratings yet
- Ivf - in Vitro FertilizationDocument32 pagesIvf - in Vitro FertilizationMinmint TanyanurakNo ratings yet
- Bahan Ajar 1 - AfasiaDocument2 pagesBahan Ajar 1 - Afasiasuhada.akmalNo ratings yet
- Psychoeducation in Psychiatric DisorderDocument23 pagesPsychoeducation in Psychiatric Disorderishita aggarwal100% (1)