Seminar: Joachim Sieper, Denis Poddubnyy
Seminar: Joachim Sieper, Denis Poddubnyy
Uploaded by
Daniel FernandezCopyright:
Available Formats
Seminar: Joachim Sieper, Denis Poddubnyy
Seminar: Joachim Sieper, Denis Poddubnyy
Uploaded by
Daniel FernandezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Seminar: Joachim Sieper, Denis Poddubnyy
Seminar: Joachim Sieper, Denis Poddubnyy
Uploaded by
Daniel FernandezCopyright:
Available Formats
Seminar
Axial spondyloarthritis
Joachim Sieper, Denis Poddubnyy
The term axial spondyloarthritis covers both patients with non-radiographic and radiographic axial spondyloarthritis, Lancet 2017; 390: 73–84
which is also termed ankylosing spondylitis. The disease usually starts in the third decade of life with a male to female Published Online
ratio of two to one for radiographic axial spondyloarthritis and of one to one for non-radiographic axial spondyloarthritis. January 19, 2017
http://dx.doi.org/10.1016/
More than 90% heritabilty has been estimated, the highest genetic association being with HLA-B27. The pathogenic
S0140-6736(16)31591-4
role of HLA-B27 is still not clear although various hypotheses are available. On the basis of evidence from trials the
Department of
cytokines tumour necrosis factor (TNF)-α and interleukin-17 appear to have a relevant role in pathogenesis. The Gastroenterology, Infectious
mechanisms of interaction between inflammation and new bone formation is still not completely understood but Diseases and Rheumatology,
clarification will be important for the prevention of long-term structural damage of the bone. The development of new Campus Benjamin Franklin,
Charité Universitätsmedizin
criteria for classification and for screening of patients with axial spondyloarthritis have been crucial for the early
Berlin, Berlin, Germany
indentification and treatment of such patients, with MRI being the most important existing imaging method. (Prof J Sieper MD,
Non-steroidal anti-inflammatory drugs and TNF blockers are effective therapies. Blockade of interleukin-17 is a new Prof D Poddubnyy MD)
and relevant treatment option. Correspondence to:
Prof Joachim Sieper, Department
Introduction second part of the night. Different sets of criteria have of Gastroenterology. Infectious
Diseases and Rheumatology,
Axial spondyloarthritis is a chronic inflammatory disease been developed for the classification of inflammatory Charité, Campus Benjamin
that mainly affects the axial skeleton. It is a type of back pain, which are largely overlapping.7–9 However, the Franklin, Hindenburgdamm 30,
spondyloarthritis, which also includes psoriatic arthritis, sensitivity and specificity of any of these criteria for the Berlin 12203, Germany
joachim.sieper@charite.de
arthritis associated with inflammatory bowel disease, diagnosis of axial spondyloarthritis is not higher than
and reactive arthritis. The term axial spondyloarthritis about 80%, meaning that not every axial spondyloarthritis
covers both patients who have already developed patient has this kind of back pain and that this symptom
structural damage in the sacroiliac joints or spine visible is also present in a substantial proportion of patients with
on radiographs (radiographic axial spondyloarthritis, also chronic back pain of other causes. Inflammation and, as a
termed ankylosing spondylitis) and patients without consequence of inflammation, structural damage can
such structural damage, labelled as non-radiographic occur in the axial skeleton, which can result in restriction
axial spondyloarthritis. of spinal mobility. This restriction can be quantified by
Non-radiographic axial spondyloarthritis can be seen applying established methods (such as the modified
as an earlier or milder part of axial spondyloarthritis Schober test for measurement of lumbar flexion).10,11
and patients might or might not develop structural Arthritis and enthesitis are the most common
boney damage in the axial skeleton. The Assesment peripheral manifestations (found in 30–50% of axial
in Spondylo-Arthriits international Society (ASAS) spondyloarthritis at presentation or in the past), which
has published new classificaiton criteria for axial can occur at any time in the course of the disease. These
spondyloarthritis.1 The development of the new criteria manifestations are predominantly found in the lower
was necessary because the older modified New York limbs, frequently in an asymmetrical fashion. The joints
criteria for anklyosing spondylitis2 did not allow are generally swollen and painful. Inflammation at the
identification of axial spondyloarthritis patients early in insertion of tendons, ligaments, or capsule into bone is
the course of the disease in the absence of radiographic called enthesitis. A typical location is at the insertion of
changes in the sacroiliac joints, which can take years the Achilles tendon or the plantar fascia at the calcaneus,
to manifest. Other criteria such as the European but inflammation is possible at any enthesial site.
Spondyloarthropathy Study Group (ESSG)3 and the A rather rare peripheral manifestation in axial is
Amor criteria4 had not yet included MRI assessment. The
term axial spondyloarthritis should be used preferentially
for diagnosis and classification, unless medical reasons Search strategy and selection criteria
are present to differentiate between ankylosing We searched for original English language articles and reviews
spondylitis or non-radiographic axial spondyloarthritis.5,6 in MEDLINE (via PubMed) published between Jan 1, 2000,
and April 30, 2016, using the following search terms:
Clinical presentation “ankylosing spondylitis” or “spondyloarthritis” in
Patients present with chronic back pain and stiffness combination with the terms “diagnosis”, “pathogenesis”,
predominantly of the pelvis and the lower back, but any “imaging”, “management”, “treatment”. We largely selected
part of the spine can be involved. Typical is inflammatory publications in the past 5 years, but did not exclude
back pain, which is clinically defined. Patients complain commonly referenced and highly regarded older publications.
of morning stiffness mostly of the lower back with We also searched the reference lists of articles identified by
improvement on exercise but not by rest. They can also be the search strategy and selected those we judged relevant.
awakened by back pain in the night, typically in the
www.thelancet.com Vol 390 July 1, 2017 73
Seminar
dactylitis, which is a swelling of a finger or toe as the in African-Americans, ankylosing spondylitis occurs
consequence of tendovaginitis. Disease activity is less frequently.20 The pooled prevalence for all types of
generally quantified by the Bath Ankylosing Spondylitis spondyloarthritis (including peripheral forms) ranges
Disease Activity Index (BASDAI)12 or the Ankylosing from 0·20% in South-East Asia to 1·61% in Northern
Spondylitis Disease Activity Score (ASDAS)13—both are Arctic communities.19 The reported prevalence of axial
composite scores. ASDAS contains an acute phase spondyloarthritis is between 0·32% and 1·4% in
reactant, usually C-reactive protein (CRP), in addition to different surveys.21–23
a patient’s reported outcome indices.
Uveitis is the most frequent extra-articular Pathogenesis
manifestation and presents typically as uveitis anterior, is Most studies of pathogenesis, especially those of genetics,
limited in duration, acute in onset, unilaterally, and have focused in the past on ankylosing spondylitis, which
frequently alternating from one eye to the other. Psoriasis constitutes a more homogeneous group than do all
and inflammatory bowel disease are less frequent patients with axial spondyloarthritis (figure 1). On the
See Online for appendix extra-articular findings (appendix).14–16 basis of studies of twins with ankylosing spondylitis
greater than 90% heritabilty has been estimated.24
Epidemiology Genome-wide association studies (GWAS) have detected
The disease usually starts in the third decade of life, and several genes associated with ankylosing spondylitis.
about 5 years earlier in HLA-B27 positive patients than In one large such study,25 20·44% of the genetic
in HLA-B27-negative patients.15,17 Slightly more patients predispositon was attributable to major histocompatibility
with ankylosing spondylitis are male than female complex (MHC) variants (mainly HLA-B27, but also
(approximate male to female ratio is 2–3:1); whereas the HLA-B40, HLA-B51, HLA-B7, HLA-A2, and HLA-DPB1),
sex distribution among patients with non-radiographic and 7·38% to non-MHC variants. The remaining 72% of
axial spondyloarthritis is equal.15,18 Accurate prevalence genetic predisposition remains to be identified.
figures are difficult to obtain for axial spondyloarthritis In addition to HLA-B27, two further genetic loci have
because studies rely on a selection of patients or been associated with ankylosing spondylitis and might be
population-based surveys that generally do not include of functional relevance: endoplasmic reticulum amino
imaging investigations and HLA-B27 testing. More data petidase (ERAP),26 which encodes an aminopeptidase
are available for the prevalence of ankylosing spondylitis expressed in the endoplasmic reticulum and is involved in
than are for axial spondyloarthritis as a whole. The preparing peptides for MHC class 1 presentation to
prevalence of ankylosing spondylitis mirrors the immune effector cells, and the interleukin-23 receptor,26
prevalence of HLA-B27 in a given population. In which activates T-helper cells secreting the cytokine
populations of European descent HLA-B27 is present interleukin-17 but also other proinflammatory cells. The
in about 8% and ankylosing spondylitis in about 0·5%.19 ERAP1-association—but not the ERAP2-association—is
In those with a lower HLA-B27 prevalence, for example confined to HLA-B27-positive cases, indicating that
peptides presented by HLA-B27 might be of relevance.27
Axial spondyloarthritis is clincially associated with
Genetic background Disturbed Disturbed Infection inflammatory bowel disease, psoriasis, or reactive
HLA-B27
ERAP-positive
+ gut barrier
(Crohn’s)
Or skin barrier
(psoriasis)
Or
arthritis in about 15–20% of cases.14,15 However, any of
Interleukin-23 receptor these diseases can be clinically silent;28,29 therefore, this
Other identified and unidentified genes association might be much higher. Thus, barrier damage
of dermal (psoriasis) and mucosal (inflammatory bowel
Exposure to microbes disease) surfaces and the subsequent exposure of the
immune system to microorganisms seems to be of
relevance for the pathogenesis. Considerable overlap
Mediated by mechanical stress
between ankylosing spondylitis susceptibility loci and
inflammatory bowel disease loci has been found.26 An
altered microbiota has been identified in patients with
Sacroiliitis/spondylitis/enthesitis (inflammation) inflammatory bowel disease30 and intestinal microbiota
could also play an important part in spondyloarthritis.31,32
Anti-CD74 antibodies (directed against the class
Facultative
Repair: fibrous tissue invaded subchronal area 2-associated invariantchain peptide, CLIP), might play a
part in the diagnosis of axial spondyloarthritis and might
New bone formation: activation of osteoblasts
be implicated in its pathogenesis by binding to CD74 on
the surface of immune competent cells.33,34 However,
these findings need confirmation in larger studies.
Figure 1: Pathogenesis of axial spondyloarthritis
Inflammation might or might not (facultative) lead to repair and new bone formation. Molecular and cellular On the basis of therapeutic successes, two pathways in
aspects are not presented. ERAP=endoplasmic reticulum aminopeptidase. the inflammatory responses, probably located rather at
74 www.thelancet.com Vol 390 July 1, 2017
Seminar
the end of the immune response hierarchy, have attracted in the serum of patients with ankylosing spondylitis were
a lot of interest over past years—ie, the tumour necrosis associated with more syndesmophyte formation in the
factor (TNF)-α-axis and the the interleukin-23/ spine. Furthermore, higher levels of noggin-IgG, or
interleukin-17-axis. T-helper-17 cells release the cytokine sclerostin-IgG, or both, immune complexes have been
interleukin-17 on stimulation with interleukin-23. identified in the serum of patients with ankylosing
However, interleukin-17 is not only released by T cells but spondylitis, which might contribute to the increase
is also expressed by cells of the innate immune system in new bone formation in such patients.48 Several
such as mast cells and granulocytes in affected tissue biomarkers positively associated with the development of
of patients with ankylosing spondylitis35 and psoriatic structural damage in the spine have also been identified:
arthritis, and by mucosal-associated invariant cells in C-reactive protein (CRP),49 matrix-metalloproteinase-3,50
such patients.36 Human mast cells do not produce vascular endothelial growth factor,51 calprotectin,52 and
interleukin-17 themselves but actively capture exogenous visfatin.53 These biomarkers might help to identify
interleukin-17 through receptor-mediated endocytosis, patients at high risk for radiographic spinal progression;
which can then subsequently be released on stimulation.37 however, only CRP is currently recommended for use in
How the TNFα and interleukin-17-pathways are clinical practice.
connected and whether or not there is a hierachical MRI studies have been used to get a better idea about
order between the two is not clear.38 Interleukin-17 also the sequence of events from inflammation to new bone
inhibits bone formation, an effect that might be formation in the axial skeleton. These studies have
blocked pharmacologically by inhibiting interleukin- suggested that active inflammatory lesions (bone marrow
17A,39 although the exact effect of interleukin-17 on new oedema visible on MRI) later evolve into repair lesions
bone formation still needs to be clarified. (visible as fatty lesions on MRI) from which stimuli
Systemic overexpression of interleukin-23 in an animal for new bone formation are released.54,55 A recent
model induced an enthesitis, which resembles the one immunohistological study56 from facet joints from
seen in spondyloarthritis, supporting the idea that patients with ankylosing spondylitis, showed that a
interleukin-23 might play a pathogenic part for fibroblast-rich granulation tissue erodes the subchondral
enthesitis.40 In the context of axial spondyloarthritis it bone plate but also has bone-forming capacities. This
was of special interest that these cells ([ROR-γt]+CD3+CD4– granulation tissue was only partly associated with
CD8– T-cells) secrete interleukin-17 to activate osteoclasts adipocytes and fat vacuoles and might therefore evade
but could also release interleukin-22 upon stimulation detection by MRI T1-weighted sequence.55,57
with interleukin-23, which can induce osteoproliferation.
Interleukin-23 is expressed in the subchondral bone Classification criteria for axial spondyloarthritis
marrow in a higher amount in the spine from patients In 2009, the ASAS criteria for axial spondyloarthritis1
with ankylosing spondylitis than in subchondral bone (figure 2) and in 2011 for peripheral spondyloarthritis,58
marrow in the spine from osteoarthritis patients.41 were published, which differentiate between patients
The characteristic inflammation of spondyloarthritis with predominantly axial and patients with predominantly
occurs at the interface between cartilage and bone in the peripheral manifestations and that include MRI findings
sacroiliac joints, the spine, and the entheses. Mechanical
stress might be important for the initiation (and possibly In patients with ≥3 months back pain and age at onset <45 years
the maintainance) of inflammation42 and might explain
why the disease process most affects the weight bearing Sacroiliitis on imaging* HLA-B27
parts of the skeleton. In addition to inflammation, axial plus or plus
spondyloarthritis is also characterised by new bone ≥1 feature of spondyloarthritis ≥2 other features of
spondyloarthritis
formation in the sacroiliac joints and spine. New
bone formation seems to be the consequence of previous
bone damage42 and might be part of a repair process
aiming for stabilisation.43 Investigation of facet joints Spondyloarthritis features:
• Inflammatory back pain • Dactylitis • Family history
obtained from patients with ankylosing spondylitis showed • Arthritis • Psoriasis for SpA
that cartilaginous fusion and ankylosis of facet joints in • Enthesitis (heel) • Crohn’s/colitis • HLA-B27
such patients is promoted by cartilage degeneration and • Uveitis • Good response to NSAIDs • Elevated CRP
not mediated by chondrocyte hypertrophy.44
Figure 2: The ASAS classification criteria for axial spondyloarthritis
At the molecular level, osteoproliferation in axial
Adapted from Rudwaleit and colleagues.1 Overall sensitivity of the criteria is
spondyloarthritis seems to be directed by bone 82·9%, overall specificity is 84·4%. Imaging arm alone: sensitivity, 66·2%;
morphogenetic proteins, Wingless pathway proteins, specificity, 97·3%. Clinical arm alone: sensitivity, 56·6%; specificity, 83·3%.
hedgehog proteins, and fibroblast growth factors and ASAS=Assessment of SpondyloArthritis International Society. CRP=C-reactive
protein. NSAIDs=non-steroidal anti-inflammatory drugs. SpA=spondyloarthritis.
their respective signalling cascades.43,45 Osteoproliferation
*Sacroiliitis on imaging refers to definite radiographic sacroiliitis according to
is inhibited43 by molecules such as sclerostin, dickkopf 1, the modified New York criteria or sacroiliitis on MRI according to the ASAS
and noggin, and low levels of sclerostin46 and dickkopf 147 consensus definition.
www.thelancet.com Vol 390 July 1, 2017 75
Seminar
and HLA-B27 testing. However, because axial and spondyloarthritis and related disorders), and several
peripheral spondyloarthritis can overlap and exist laboratory indices (HLA-B27 and acute phase reactants
together, criteria were also developed for patients testing, and imaging findings) have to be combined for
presenting with both axial and peripheral classification and diagnosis of axial spondyloarthritis
spondyloarthritis.58 Because the disease usually starts in with only a moderate overlap between the two.
the sacroiliac joints, chronic or active inflammatory bony The same clinical, laboratory, and imaging indices are
changes of the spine are not part of the classification used for classification and diagnosis but clear differences
criteria but involvement of the spine without sacroiliac exist in their application.67,68 Classification criteria are
joints can occur in a small percentage of patients and developed to get a clear yes or no answer, to create a rather
could be used for diagnosis. The so-called clinical arm, homogeneous group of patients, usually for inclusion into
for which the presence of a positive HLA-B27 test is a clinical trial or cohort. For diagnosis, negative findings
mandatory, was added to the classification criteria to are also taken into account (appendix) and other reasons
increase sensitivity, resulting in an acceptable senstivitiy why typical indices of spondyloarthritis are positive have
of 82·9% and specificity of 84·4%. to be considered for differential diagnosis.69
Discussion is ongoing about whether these
classification criteria need modification, mostly for the Imaging
improvement of specificity.5,6,59–61 When patients from the Imaging is crucial for the correct (and early) diagnosis as
original study1 were followed up over 3–5 years and seen well as differential diagnosis of axial spondyloarthritis.
again by the local rheumatologist the positive predictive Because the disease affects sacroiliac joints (as opposed
value that patients who fulfilled the criteria initially to the spine) in most patients, imaging of sacroiliac
would still be diagnosed as axial spondyloarthritis by the joints has a pivotal role for diagnosis (and to a further
rheumatologist was 93·3%.62 Futhermore, when the extent in classification) of axial spondyloarthritis.10
ASAS classification criteria were tested in other cohorts Conventional radiography of the sacroiliac joints
with the rheumatologist’s diagnosis as the gold standard, (figure 3, appendix) is recommended as the first imaging
an acceptable sensitivity and specificity was comparable method to diagnose sacroiliitis as part of axial
with the initial study, resulting in a sensitivity of spondyloarthritis.2,69,70 Even in patients with short disease
between 68% and 87% and a specificity of between 62% duration (up to 3 years), a definite radiographic
and 95%.63–66 sacroiliitis could be seen in 30–50%, which would make
further diagnostic procedures unnecessary.71 Generally,
Diagnosis of axial spondyloarthritis this number depends predominantly on the duration of
Classification criteria are often wrongly used for disease at time of first diagnosis and has been reported
diagnostic purposes because separate diagnostic criteria to vary between 22% and 77%.60
are generally not available. Because of the lack of Nonetheless, radiography of sacroiliac joints has
gold standards in rheumatology, including axial limitations in patients with early axial spondyloarthritis,
spondyloarthritis, several clinical indices (presence of because structural changes generally take months to years
chronic back pain started at an age ≤45 years, to take place.72 Furthermore, the interpretation of
inflammatory back pain, peripheral and extraarticular radiographs of the sacroiliac joints is often challenging.
manifestations, response of symptoms to non-steroidal Indeed, a considerable inter-reader variation has repeatedly
anti-inflammatory drugs [NSAIDs], family history of been reported, even among experienced readers.73,74
A B C
T1
Figure 3: Radiograph of the sacroiliac joints
MRI of sacroiliac joints in a STIR and T1-weighted sequences of a 25-year-old patient with inflammatory back pain for about 1·5 years, positive HLA-B27, and slightly
raised C-reactive protein levels (7·2 mg/L). (A) Conventional pelvic radiograph shows some subchondral sclerosis on the right side, otherwise the joint is difficult to
assess; the latter is also true for the entire left sacroiliac joints, where an overlap with intestinal gas could be seen. No definite judgment on the presence or absence of
radiographic sacroiliitis could be made. (B) MRI in the STIR sequence shows two areas of bone marrow oedema (green arrows); the lesion in the right sacroiliac joint is
large and localised subchondrally and is therefore compatible with spondyloarthritis. The lesion on the left side is localised not directly subchondrally and might
represent the rest of a larger lesion or enthesitis. (C) MRI in the T1-weighted sequence shows large areas of fat metaplasia of bone marrow—so-called fatty lesions
(white arrows) localised subchondrally, sharply boarded, and homogeneous; further, subchondral sclerosis (pink arrows) and cortical bone defects (erosions, blue
arrow) are evident. Final diagnosis: axial spondyloarthritis. STIR=short TI-weighted inversion recovery.
76 www.thelancet.com Vol 390 July 1, 2017
Seminar
Normal or ambiguous radiographic results of sacroiliac anterior or posterior spondylitis in at least three sites;79
joints examination in the context of a possible diagnosis however, the presence of five or more inflammatory
of spondyloarthritis (figure 3, appendix) require MRI lesions might discriminate even better from control
investigation of the sacroiliac joints as the next step.70 groups.80 The diagnostic value of other imaging methods
The following MRI sequences are useful for diagnosis such as skeletal scintigraphy,81 ultrasonography of the
and differential diagnosis of axial spondyloarthritis sacroiliac joints, and positron emission tomography is
(figure 3, appendix): a T2-weighted sequence with fat low or undetermined in axial spondyloarthritis and,
suppression (such as a short tau inversion recovery therefore, these methods are not recommended
[STIR] sequence) for detection of active inflammatory for diagnosis.70
changes (bone marrow oedema) (figure 3, appendix); a
T1-weighted sequence for detection of post-inflammatory Screening in patients with chronic back pain
changes, such as erosions, sclerosis, ankyloses, and fatty A major delay of several years remains between the start
lesions (figure 3, appendix). A gradient echo sequence of chronic back pain and a final diagnosis in patients
(appendix),75 which allows better detection of erosions with axial spondyloarthritis. In addition to relying on
than a T1-weighted sequence because of improved the presence of radiographic changes that can take
contrast between bone and cartilage, can be helpful but is several years to develop, another reason is the difficulty
not yet used in routine care. The application of a contrast of diagnosing patients with axial spondyloarthritis in
agent is only rarely needed and does not usually provide the large number of chronic back pain patients in
more information in addition to the T2-weighted primary care.
sequence with fat suppression. Studies have tested different screening methods using
The ASAS group recently updated76 the definition of the presence of chronic (≥3 months) back pain starting at
an active sacroiliitis on MRI for classification of axial up to 45 years as an entry criterion in primary care.
spondyloarthritis. According to this definition, clear Generally one or a combination of possible screening
presence of bone marrow oedema on MRI in subchondral idicators have been applied. In nearly all these studies a
bone is mandatory (figure 3). Importantly, the appearance final diagnosis of axial spondyloarthritis was possible in
of bone marrow oedema has to be highly suggestive of 25–45%82–86 of patients referred from primary care to
spondyloarthritis, taking into account the size of the the rheumatologist. The percentage of patients with
lesions, its subchondral location and the exclusion of non-radiographic axial spondyloarthritis among those
other—mostly mechanical reasons—that could explain a diagnosed with axial spondyloarthritis after referral was
positive finding. The presence of post-inflammatory between 20% and 80%.60,84
structural changes, especially erosions, but also ASAS subsequently developed international recom
subchondral sclerosis, fatty lesions, changes of the joint mendations for the early referral of patients with a
space should also be taken into account.70,76,77 suspicion of axial spondyloarthritis (appendix).87 These
CT of sacroiliac joints is regarded as a gold standard of recommendations include the entry criteria together
structural damage detection (especially erosions), but with any additional spondyloarthritis indices, which
conventional radiography and MRI of sacroiliac joints allows a more flexible approach and a selection of one or
usually allow a comprehensive assessment of structural several of these measures88 dependent on the regional
damage. However, CT of these joints (including a conditions.
so-called low-dose CT, which is associated with a low
radiation exposure) might be considered in cases of Management
inconclusive results.70 The existing international management recom
The most common differential diagnoses for axial mendations (ASAS/EULAR89 and ACR/SAA/
spondyloarthritis are degenerative or mechanical problems SPARTAN ) are similar (figure 4). The approval of the
90
(degenerative disc disease, spondylosis, congenital interleukin-17 inhibitor secukinumab for treatment of
vertebral anomalies, diffuse skeletal hyperostosis, osteitis ankylosing spondylitis has already been integrated into
condensans [appendix], and osteoarthritis of sacroiliac the ASAS/EULAR recommendations.89 Treat-to-target
joints); other differential diagnoses such as fractures, recommendations for spondyloarthritis, including axial
infectious sacroiliitis, and bone metastasis or primary spondyloarthritis, psoriatic arthritis, and peripheral
bone tumours are less frequent. spondyloarthritis in general, were formulated in 2014 by
Imaging of the spine (radiography or MRI, appendix) an international task force.91 The main treatment target
is not usually required78 for early diagnosis because was defined as remission, with low disease activity
active inflammatory changes and structural damage regarded as a secondary target. For both radiographic
generally arise in the sacroiliac joints first, but might and non-radiographic forms axial spondyloarthritis,
also be considered as a part of differential diagnosis. On remission was defined by a low BASDAI score plus
the basis of a literature review and expert consensus, normal CRP values or by a low ASDAS,13 which includes
ASAS defined a positive (for active inflammation) spinal the results of measurements of CRP or erythrocyte
MRI in axial spondyloarthritis as the presence of sedimentation rate.
www.thelancet.com Vol 390 July 1, 2017 77
Seminar
cardiovascular, gastrointestinal, and renal risks.92 A
Predominant Axial manifestations: Peripheral manifestations: meta-analysis100 of randomised trials in patients with any
manifestation Back pain and stiffness arthritis, enthesitis, dactylitis
disease who were treated with NSAIDs for at least
First-line therapy NSAIDs
4 weeks, the relative risks of major adverse cardiovascular
events were 1·37 for celecoxib and 1·41 for diclofenac,
Non-pharmacological treatment: education, exercise, physical therapy,
rehabilitation, patient associations, self help groups
indicating no difference between cyclooxygenase (COX)-2
selective and non-selective NSAIDs—with the exception
Local steroids of naproxen, which was not associated with an increase.
DMARDs sulfasalazine, methotrexate
Conventional disease modifying antirheumatic drugs
Second-line therapy TNF α blocker or IL-17 blocker and glucocorticoids
Conventional disease modifying antirheumatic drugs
Additional therapy Analgesics (DMARDs; as opposed to biological DMARDs—TNF and
and therapy in special
clinical situations Surgery interleukin-17 antagonists in axial spondyloarthritis),
such as methotrexate, sulfasalazine, or leflunomide, are
Figure 4: Recommendations for the treatment of axial spondyloarthritis generally not effective in the treatment of axial
Based on ASAS/EULAR89 and ACR/AAS/SPARTAN,90 including the current approval status for the interleukin-17 manifestations of spondyloarthritis, but these agents
blocker secukinumab. Secukinumab—an interleukin-17-antagonist—is currently approved only for ankylosing
might have a limited role for the treatment of peripheral
spondylitis. NSAIDs=non-steroidal anti-inflammatory drugs. DMARDs=disease modifying antirheumatic drugs.
TNF=tumour necrosis factor. manifestations when it coexists with axial disease.88,90
Discussion is ongoing over whether a combination of a
Non-steroidal anti-inflammatory agents conventional DMARD with a biological drug might
Non-steroidal anti-inflammatory agents (NSAIDs) are prevent the development of anti-drug antibodies (ADAs)
highly effective in reducing back pain and stiffness in directed against the biological drug and thus increases
patients with axial spondyloarthritis and are therefore the drug survival rate in these patients. However, such an
recommended as first-line treatment for these patients. advantage for a combination of a DMARD (mostly
There is no clear difference in the effectiveness of methotrexate) with a TNF blocker was shown in some
NSAIDs,92 and they are similarly effective in patients investigations101,102 of patients with axial spondyloarthritis
with ankylosing spondylitis and non-radiographic axial but not in others.103–105 Therefore, such a combination is
spondyloarthritis. Patients generaly respond in the first not recommended, which is also in line with current
2 weeks of NSAID therapy but in responders the response treatment recommendations.89,90
rate increases further during the first 24 weeks.93 NSAIDs Long-term systemic glucocorticoid therapy is not
should be used according to the patient’s symptoms. recommended because high doses of prednisolone of
Dose reduction or discontinuation should be tried if the about 50 mg per day106 or higher are needed to achieve a
patient is in remission. NSAIDs seem to be more effective measurable effect on disease acitvity.
if patients with axial spondyloarthritis are treated early in
the course of their disease, achieving a clinicial remission TNF inhibitors
rate of 35% in patients with early disease (<3 years of Five TNF inhibitors are available with approval for
disease duration)93 in comparison with about 12–15% in ankylosing spondylitis in the EC, USA, and most
patients with longstanding disease.94,95 other parts of the world: infliximab,107 etanercept,108
The safety of long-term NSAIDs therapy has been a adalimumab,109 golimumab,110 and certolizumab (table).111
concern. Longterm data for ankylosing spondylitis are Treatment with any of these TNF blockers leads to a good
limited and these data are mostly available for or very good improvement in all articular manifestations,
osteoarthritis and rheumatoid arthritis.92 Two reviews96,97 CRP levels, and MRI-detectable inflammation in the
of randomised controlled trials did not show increased sacroiliac joints or spine in active patients with ankylosing
side effects of NSAIDs therapy in ankylosing spondylitis spondylitis in whom conventional treatment with NSAIDs
compared with placebo during 12 weeks. Infrequent failed. Etanercept is not effective for active inflammatory
NSAID use was even associated with increased mortality bowel disease, by contrast with monoclonal antibodies,
in a Norwegian cohort of patients with long-term and evidence favouring monoclonal antibodies rather
ankylosing spondylitis,98 and in a population-based than etanercept is better for uveitis than for psoriasis.89,90
retrospective study99 of administrative health data from TNF blockers, with the exception of infliximab, have
Canada NSAID use was also associated with reduced also been approved for the other clinical subset of axial
cardiovascular risk in this population. NSAID treatment spondyloarthritis, non-radiographic spondyloarthritis, in
is associated with a decrease in inflammation and the European Union (EU) and elsewhere on the basis of
increased mobility in patients with axial spondyloarthritis, the results of phase 3 trials111,115–117 (table), but not yet in the
factors that might reduce cardiovascular morbidity. USA. The European label is restricted to patients with
Nonetheless, patients should be informed about the objective signs of inflammation, such as positive CRP or
potential risks of long-term treatment, including active MRI-inflammation in the sacroiliac joint or spine
78 www.thelancet.com Vol 390 July 1, 2017
Seminar
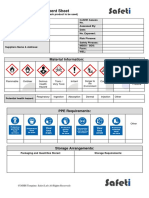
Dosing regimen Assessment Drug response Placebo response Difference, %
timepoint (ASAS40), % (n/N) (ASAS40), %
(week) (n/N)
Ankylosing spondylitis
Adalimumab109 40 mg, every other week, subcutaneous 12 40 (83/208) 13 (14/107) 27
Certolizumab pegol111 200 mg, every other week, subcutaneous 12 40 (26/65) 19 (11/57) 21
Certolizumab pegol111 400 mg, every 4 weeks, subcutaneous 12 50 (28/56) 19 (11/57) 31
Etanercept112 25 mg, twice weekly, subcutaneous 12 45 (58/128) 16 (21/129) 29
Golimumab110 50 mg, every 4 weeks, subcutaneous 14 45 (62/138) 15 (12/78) 30
Infliximab113 5 mg/kg, weeks 0, 2, and 6, and every 6 weeks thereafter, 24 47 (93/201) 12 (9/78) 35
intravenous
Secukinumab114 150 mg, subcutaneous, every 4 weeks, after initial 16 42 (52/125) 13 (16/122) 29
intravenous loading dose of 10 mg/kg at baseline, week 4
and 8
Secukinumab114 150 mg, subcutaneous, every 4 weeks, after initial loading 16 36 (26/72) 11 (8/74) 25
with 150 mg, subcutaneous, weekly through week 4
Non-radiographic axial spondyloarthritis (all included patients)*
Adalimumab115 40 mg, every other week, subcutaneous 12 36 (33/91) 15 (14/94) 21
Certolizumab pegol111 200 mg, every other week, subcutaneous 12 48 (22/46) 16 (8/50) 32
Certolizumab pegol111 400 mg, every 4 weeks, subcutaneous 12 47 (24/51) 16 (8/50) 31
Etanercept116 50 mg, weekly, subcutaneous 12 33 (35/105) 15 (16/108) 18
Golimumab117 50 mg, every 4 weeks, subcutaneous 16 57 (55/97) 23 (23/100) 34
Non-radiographic axial spondyloarthritis (with raised CRP, or active sacroiliitis on MRI, or both)*
Adalimumab115 40 mg, every other week, subcutaneous 12 41 (28/69) 14 (10/73) 27
Certolizumab pegol111 200 mg, every other week, subcutaneous 12 48 (22/46) 16 (8/50) 32
Certolizumab pegol111 400 mg, every 4 weeks, subcutaneous 12 47 (24/51) 16 (8/50) 31
Etanercept116,118† 50 mg, weekly, subcutaneous 12 35 (33/94) 17 (16/93) 18
Golimumab117 50 mg, every 4 weeks, subcutaneous 16 60 (47/78) 23 (18/80) 37
No data are available for infliximab and secukinumab for non-radiographic axial spondyloarthritis. These are not head-to-head trials and, therefore, comparison of results is
limited. Only the certolizumab trial was stratified for radiographic and non-radiographic axial spondyloarthritis, whereas the other trials for TNF blockers in radiographic and
non-radiographic axial spondyloarthritis were undertaken separately and at different timepoints. n=number of patients responding. N=number of patients in this group.
TNF=tumour necrosis factor. CRP=C-reactive protein. *Target population according to the approval status for anti-TNF drugs in non-radiographic axial spondyloarthritis in
the European Union and some other countries: patients with non-radiographic axial spondyloarthritis with raised CRP, or active sacroiliitis on MRI, or both. †Approximate
response rates calculated on the basis of the information obtained from the cited sources.
Table: ASAS40 response to biologicals in phase 3 clinical trials in patients with axial spondyloarthritis
(figure 5). Presence of positive CRP or MRI inflammation Other biological disease modifying antirheumatic drugs
is not mandatory for the treatment of ankylosing Anakinra, an interleukin-1 receptor antagonist, and
spondylitis, although those patients do also respond abatacept, a T-cell modulator, were tested in small
better than patients negative for these indices.119 If the prospective open-label trials89,90 in patients with
treatment results between ankylosing spondylitis and ankylosing spondylitis and did not have a better effect
non-radiographic spondyloarthritis are compared for than an expected (historical) placebo response. A similar
those patients who are treated according to the label in prospective open-label study127,128 with rituximab, a
the EU, the results are similar (table).120 For patients with monoclonal antibody directed against CD20 on B cells,
axial spondyloarthritis, raised CRP, short symptom produced inconclusive results. Tocilizumab129 and
duration (or young age), and active MRI inflammation sarilumab,130 both monoclonal antibodies directed
seem to be the best predictors for a good response to against the interleukin-6 receptor, were tested in two
TNF blockers.120 placebo-controlled double-blind studies in anti-TNF-
Discontinuation of TNF blocker in patients with axial naive patients with active ankylosing spondylitis, with
spondyloarthritis who had had a good response generally no efficacy compared with placebo.
resulted in a relapse in 75–90% of cases,121–123 without any By contrast, treatments targeting the interleukin-23–
major differences if NSAID therapy was continued or interleukin-17 axis seem to be very promising in patients
not,124 but a reduction of the TNF-blocker dose in good with axial spondyloarthritis. Until now, all completed
responders was tolerated by 52–86% of patients.125,126 studies of these treatments have been done in patients
However, these results are based on small numbers of with ankylosing spondylitis, but studies including those
patients and this question should be further examined in with non-radiographic axial spondyloarthritis are
larger trials. ongoing. In two phase 3 trials, the anti-interleukin-17
www.thelancet.com Vol 390 July 1, 2017 79
Seminar
interleukin-12 and interleukin-23) has been undertaken
Diagnosis* Ankylosing spondylitis Non-radiographic axial spondyloarthritis in patients with ankylosing spondylitis showing good
efficacy. This efficacy is being assessed further in
ongoing placebo-controlled trials in ankylosing
spondylitis and non-radiographic axial spondyloarthritis.
The oral Janus kinase inhibitor tofacitinib has been
tested in one phase 2 double-blind placebo-controlled
dose-ranging study134 in patients with ankylosing
spondylitis, providing a positive signal for a good
clinical and MRI response that needs confirmation in a
Failure of the At least 2 NSAIDs given for At least 2 NSAIDs given for larger trial. Apremilast, an oral PDE4 inhibitor, was
previous treatment 4 weeks in total 4 weeks in total tested in a small proof of concept trial135 in active
patients with ankylosing spondylitis for 12 weeks either
High disease activity BASDAI ≥4 or ASDAS ≥2·1† BASDAI ≥4 or ASDAS ≥2·1† with apremilast or placebo showing a moderate
and reduction of the disease activity but a larger
Objective signs of inflammatory activity: placebo-controlled phase 2 trial136 in patients with
ankylosing spondylitis did not show a response superior
to placebo treatment.
or CRP+
Treatment options for inhibition of radiographic
Active sacroiliitis progression
Possible treatments to stop radiographic progression
Figure 5: Current approval status for TNF-blocker treatment of axial spondyloarthritis patients in the involve early suppression of inflammation and targeting
European Union of molecules stimulating bone formation. TNF-blocker
No current approval for non-radographic axial spondyloarthritis in the USA; approval also in many other parts of treatment does not have an effect on radiographic
the world, but note that in some non-European Union countries the presence of objective signs of inflammation is
not mandatory. TNF=tumour necrosis factor. NSAIDs=non-steroidal anti-inflammatory drugs. ASDAS=Ankylosing
progression over 2 or 4 years of treatment in patients
Spondylitis Disease Activity Score. CRP=C-reactive protein. BASDAI=Bath Ankylosing Spondylitis Disease Activity with established longstanding ankylosing spondylitis.137,138
Index. *Based on a combination of clinical, laboratory, and imaging parameters. †According to the ASAS/EULAR But evidence shows that early treatment139 and treatment
recommendations.89 for more than 4 years140 might affect radiographic
inhibitor secukinumab was effective in patients with progression by suppression of inflammation and the
ankylosing spondylitis,114 and—on the basis of the results avoidance of subchondral granulation tissue.54 Direct
of these trials—have now been approved for ankylosing targeting of new bone formation might be associated
spondylitis in the EU, USA, and other parts of the world with too many side-effects affecting the general bone
(table). The positive treatment response was maintained metabolism. Biomarkers that predict new bone formation
throughout 52 weeks of treatment in both studies. A are needed to identify patients who would benefit from
dose of 300 mg secukinumab, which is more effective such treatments.
than 150 mg for the treatment of psoriasis, has not yet An inhibitory effect of contiuous NSAID therapy for
been investigated for ankylosing spondylitis. Although 2 years was reported in patients with ankylosing
no head-to-head trials have been done so far, the spondylitis in one randomised prospective trial.141 This
demonstrated effectiveness of secukinumab seems to be effect was backed by additional data from a retrospective
close to the response rates seen in TNF-blocker trials analysis,142 and from a prospective observational
undertaken in a similar patient group. Secukinumab spondyloarthritis cohort.143 A direct inhibitory effect of
was also effective in a subgroup of patients in whom NSAIDs on osteoblasts, mediated by prostaglandin
TNF-blocker therapy failed or was discontinued for inhibition, was postulated as a possible mechanism to
other reasons.131 explain these results. However, these findings could not
Nevertheless, the place of interleukin-17 inhibitors in be confirmed by another randomised prospective trial.144
the treatment of axial spondyloarthritis remains to be In the trial by Sieper and colleagues,144 most patients
determined as larger clinical experience grows. The were treated with diclofenac, whereas in the trial by
efficacy of secukinumab treatment in patients who failed Wanders and colleagues,141 most were given celecoxib.
to respond to a first TNF blocker needs to be compared Thus it is unclear whether the inhibitory effect was
with the effectiveness of treatment with a second TNF COX-2-specific (or even celecoxib-specific effect) in the
blocker. Additionally, whether interleukin-17 blockade trial by Wanders and colleagues141 or whether NSAIDs
might reduce the progression of new bone formation, as are just not effective for the inhibiton of new bone
was speculated on the basis of the results of one formation. Until additonal data become available,
uncontrolled ankylosing spondylitis trial,132 is unknown. NSAID treatment is only recommended for the
One prospective open-label trial133 of ustekinumab treatment of signs and symptoms but not to inhibit
(a monoclonal antibody against the p40 subunit of syndesmophyte growth.89,90
80 www.thelancet.com Vol 390 July 1, 2017
Seminar
Controversies and outstanding research 14 Vander Cruyssen B, Ribbens C, Boonen A, et al. The epidemiology
questions of ankylosing spondylitis and the commencement of anti-TNF
therapy in daily rheumatology practice. Ann Rheum Dis 2007;
More of the genes involved in the pathogenesis of axial 66: 1072–77.
spondyloarthritis need to be identified, the functional 15 Rudwaleit M, Haibel H, Baraliakos X, et al. The early disease stage
mechanisms of the known genetic associations should in axial spondylarthritis: Results from the german spondyloarthritis
inception cohort. Arthritis Rheum 2009; 60: 717–27.
be determined, and understanding of the interaction 16 Dougados M, Etcheto A, Molto A, et al. Clinical presentation of
between genetic predispositon and environment, such as patients suffering from recent onset chronic inflammatory back pain
exposure to microbes, needs to be improved. Discussion suggestive of spondyloarthritis: The DESIR cohort. Joint Bone Spine
2015; 82: 345–51.
will continue as to whether and how classification and 17 Jaakkola E, Herzberg I, Laiho K, et al. Finnish HLA studies confirm
diagnosis, with a focus on early identification, can be the increased risk conferred by HLA-B27 homozygosity in
improved—and the role of MRI in this process should ankylosing spondylitis. Ann Rheum Dis 2006; 65: 775–80.
18 van Tubergen A. The changing clinical picture and epidemiology of
be further specified. The proven effectiveness of spondyloarthritis. Nat Rev Rheumatol 2015; 11: 110–18.
interleukin-17 inhbition for the treatment of axial 19 Stolwijk C, van Onna M, Boonen A, van Tubergen A. The global
spondyloarthritis raises the question of whether the prevalence of spondyloarthritis: A systematic review and
same or different patients respond to TNF-blockade and meta-regression analysis. Arthritis Care Res (Hoboken) 2016;
68: 1320–31.
interleukin-17 inhibiton and about the potential of a 20 Khan MA, Kushner I, Braun WE. Letter: Low incidence of
combination of these two treatments. Finally, which HLA-B27 in American Blacks with spondyloarthropathies. Lancet
treatment can stop radiographic progression remains to 1976; 1: 483.
21 Reveille JD, Witter JP, Weisman MH. Prevalence of axial
be shown and how best to identify patients who will spondylarthritis in the United States: estimates from a cross-sectional
benefit most from such an intervention. survey. Arthritis Care Res (Hoboken) 2012; 64: 905–10.
References 22 Bakland G, Alsing R, Singh K, Nossent JC. Assessment of
1 Rudwaleit M, van der Heijde D, Landewe R, et al. The development SpondyloArthritis International Society criteria for axial
of Assessment of SpondyloArthritis international Society spondyloarthritis in chronic back pain patients with a high
classification criteria for axial spondyloarthritis (part II): prevalence of HLA-B27. Arthritis Care Res (Hoboken) 2013;
validation and final selection. Ann Rheum Dis 2009; 68: 777–83. 65: 448–53.
2 van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic 23 Costantino F, Talpin A, Said-Nahal R, et al. Prevalence of
criteria for ankylosing spondylitis. A proposal for modification of spondyloarthritis in reference to HLA-B27 in the French population:
the New York criteria. Arthritis Rheum 1984; 27: 361–68. results of the GAZEL cohort. Ann Rheum Dis 2015; 74: 689–93.
3 Dougados M, van der Linden S, Juhlin R, et al. The European 24 Brown MA, Kennedy LG, MacGregor AJ, et al. Susceptibility to
Spondylarthropathy Study Group preliminary criteria for the ankylosing spondylitis in twins: the role of genes, HLA, and the
classification of spondylarthropathy. Arthritis Rheum 1991; 34: 1218–27. environment. Arthritis Rheum 1997; 40: 1823–28.
4 Amor B, Dougados M, Mijiyawa M. Criteria of the classification of 25 Ellinghaus D, Jostins L, Spain SL, et al. Analysis of five chronic
spondylarthropathies. Rev Rhum Mal Osteoartic 1990; 57: 85–89. inflammatory diseases identifies 27 new associations and
highlights disease-specific patterns at shared loci. Nat Genet 2016;
5 Deodhar A, Strand V, Kay J, Braun J. The term ‘non-radiographic
48: 510–18.
axial spondyloarthritis’ is much more important to classify than to
diagnose patients with axial spondyloarthritis. Ann Rheum Dis 2016; 26 International Genetics of Ankylosing Spondylitis C, Cortes A,
75: 791–94. Hadler J, et al. Identification of multiple risk variants for
ankylosing spondylitis through high-density genotyping of
6 Deodhar A, Reveille JD, van den Bosch F, et al. The concept of axial
immune-related loci. Nat Genet 2013; 45: 730–38.
spondyloarthritis: joint statement of the spondyloarthritis research
and treatment network and the Assessment of SpondyloArthritis 27 Evans DM, Spencer CC, Pointon JJ, et al. Interaction between
international Society in response to the US Food and Drug ERAP1 and HLA-B27 in ankylosing spondylitis implicates peptide
Administration‘s comments and concerns. Arthritis Rheumat 2014; handling in the mechanism for HLA-B27 in disease susceptibility.
66: 2649–56. Nat Genet 2011; 43: 761–67.
7 Calin A, Porta J, Fries JF, Schurman DJ. Clinical history as a 28 Carter JD, Gerard HC, Espinoza LR, et al. Chlamydiae as etiologic
screening test for ankylosing spondylitis. JAMA 1977; 237: 2613–14. agents in chronic undifferentiated spondylarthritis. Arthritis Rheum
2009; 60: 1311–16.
8 Rudwaleit M, Metter A, Listing J, Sieper J, Braun J. Inflammatory
back pain in ankylosing spondylitis: a reassessment of the clinical 29 Van Praet L, Jans L, Carron P, et al. Degree of bone marrow oedema
history for application as classification and diagnostic criteria. in sacroiliac joints of patients with axial spondyloarthritis is linked
Arthritis Rheum 2006; 54: 569–78. to gut inflammation and male sex: results from the GIANT cohort.
Ann Rheum Dis 2014; 73: 1186–89.
9 Sieper J, van der Heijde D, Landewe R, et al. New criteria for
inflammatory back pain in patients with chronic back pain: a real 30 Nagalingam NA, Lynch SV. Role of the microbiota in inflammatory
patient exercise by experts from the Assessment of SpondyloArthritis bowel diseases. Inflamm Bowel Dis 2012; 18: 968–84.
international Society (ASAS). Ann Rheum Dis 2009; 68: 784–88. 31 Asquith M, Elewaut D, Lin P, Rosenbaum JT. The role of the gut
10 Sieper J, Rudwaleit M, Baraliakos X, et al. The Assessment of and microbes in the pathogenesis of spondyloarthritis.
SpondyloArthritis international Society (ASAS) handbook: a guide Best Pract Res Clin Rheumatol 2014; 28: 687–702.
to assess spondyloarthritis. Ann Rheum Dis 2009; 32 Costello ME, Ciccia F, Willner D, et al. Intestinal dysbiosis in
68 (suppl 2): ii1–44. ankylosing spondylitis. Arthritis Rheumatol 2014; published online
11 Ramiro S, van Tubergen A, Stolwijk C, van der Heijde D, Royston P, Nov 21. DOI:10.1002/art.38967.
Landewe R. Reference intervals of spinal mobility measures in 33 Baraliakos X, Baerlecken N, Witte T, Heldmann F, Braun J.
normal individuals: the MOBILITY study. Ann Rheum Dis 2015; High prevalence of anti-CD74 antibodies specific for the HLA
74: 1218–24. class II-associated invariant chain peptide (CLIP) in patients with
12 Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, axial spondyloarthritis. Ann Rheum Dis 2014; 73: 1079–82.
Calin A. A new approach to defining disease status in ankylosing 34 Baerlecken NT, Nothdorft S, Stummvoll GH, et al. Autoantibodies
spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. against CD74 in spondyloarthritis. Ann Rheum Dis 2014; 73: 1211–14.
J Rheumatol 1994; 21: 2286–91. 35 Appel H, Maier R, Wu P, et al. Analysis of IL-17(+) cells in facet joints
13 Machado P, Landewe R, Lie E, et al. Ankylosing Spondylitis Disease of patients with spondyloarthritis suggests that the innate immune
Activity Score (ASDAS): defining cut-off values for disease activity pathway might be of greater relevance than the Th17-mediated
states and improvement scores. Ann Rheum Dis 2010; 70: 47–53. adaptive immune response. Arthritis Res Ther 2011; 13: R95.
www.thelancet.com Vol 390 July 1, 2017 81
Seminar
36 Gracey E, Qaiyum Z, Almaghlouth I, et al. IL-7 primes IL-17 in 57 Machado PM, Baraliakos X, van der Heijde D, Braun J, Landewe R.
mucosal-associated invariant T (MAIT) cells, which contribute to MRI vertebral corner inflammation followed by fat deposition is
the Th17-axis in ankylosing spondylitis. Ann Rheum Dis 2016; the strongest contributor to the development of new bone at the
published online May 10. DOI:10.1136/annrheumdis-2015-208902. same vertebral corner: a multilevel longitudinal analysis in patients
37 Noordenbos T, Blijdorp I, Chen S, et al. Human mast cells capture, with ankylosing spondylitis. Ann Rheum Dis 2016; 75: 1486–93.
store, and release bioactive, exogenous IL-17A. J Leukoc Biol 2016; 58 Rudwaleit M, van der Heijde D, Landewe R, et al. The Assessment
100: 453–62. of SpondyloArthritis International Society classification criteria for
38 Miossec P, Kolls JK. Targeting IL-17 and TH17 cells in chronic peripheral spondyloarthritis and for spondyloarthritis in general.
inflammation. Nat Rev Drug Discov 2012; 11: 763–76. Ann Rheum Dis 2011; 70: 25–31.
39 Uluckan O, Jimenez M, Karbach S, et al. Chronic skin 59 Robinson PC, Wordsworth BP, Reveille JD, Brown MA.
inflammation leads to bone loss by IL-17-mediated inhibition of Axial spondyloarthritis: a new disease entity, not necessarily early
Wnt signaling in osteoblasts. Sci Transl Med 2016; 8: 330ra37. ankylosing spondylitis. Ann Rheum Dis 2013; 72: 162–64.
40 Sherlock JP, Joyce-Shaikh B, Turner SP, et al. IL-23 induces 60 Sieper J, van der Heijde D. Review: nonradiographic axial
spondyloarthropathy by acting on ROR-gammat+ CD3+CD4-CD8- spondyloarthritis: new definition of an old disease? Arthritis Rheum
entheseal resident T cells. Nat Med 2012; 18: 1069–76. 2013; 65: 543–51.
41 Appel H, Maier R, Bleil J, et al. In situ analysis of interleukin-23- 61 van der Linden S, Akkoc N, Brown MA, Robinson PC, Khan MA.
and interleukin-12-positive cells in the spine of patients with The ASAS Criteria for Axial Spondyloarthritis: Strengths, Weaknesses,
ankylosing spondylitis. Arthritis Rheum 2013; 65: 1522–29. and Proposals for a Way Forward. Curr Rheumatol Rep 2015; 17: 62.
42 Jacques P, Lambrecht S, Verheugen E, et al. Proof of concept: 62 Sepriano A, Landewe R, van der Heijde D, et al. Predictive validity
enthesitis and new bone formation in spondyloarthritis are driven of the ASAS classification criteria for axial and peripheral
by mechanical strain and stromal cells. Ann Rheum Dis 2014; spondyloarthritis after follow-up in the ASAS cohort: a final
73: 437–45. analysis. Ann Rheum Dis 2016; 75: 1034–42.
43 Lories R. The balance of tissue repair and remodeling in chronic 63 van den Berg R, de Hooge M, van Gaalen F, Reijnierse M,
arthritis. Nat Rev Rheumatol 2011; 7: 700–07. Huizinga T, van der Heijde D. Percentage of patients with
44 Bleil J, Maier R, Hempfing A, et al. Histomorphologic and spondyloarthritis in patients referred because of chronic back pain
histomorphometric characteristics of zygapophyseal joint and performance of classification criteria: experience from the
remodeling in ankylosing spondylitis. Arthritis Rheumatol 2014; Spondyloarthritis Caught Early (SPACE) cohort.
66: 1745–54. Rheumatology (Oxford) 2013; 52: 1492–99.
45 Ruiz-Heiland G, Horn A, Zerr P, et al. Blockade of the hedgehog 64 Molto A, Paternotte S, Comet D, et al. Performances of the
pathway inhibits osteophyte formation in arthritis. Ann Rheum Dis Assessment of SpondyloArthritis International Society axial
2012; 71: 400–07. spondyloarthritis criteria for diagnostic and classification purposes
in patients visiting a rheumatologist because of chronic back pain:
46 Appel H, Ruiz-Heiland G, Listing J, et al. Altered skeletal expression
results from a multicenter, cross-sectional study.
of sclerostin and its link to radiographic progression in ankylosing
Arthritis Care Res (Hoboken) 2013; 65: 1472–81.
spondylitis. Arthritis Rheum 2009; 60: 3257–62.
65 Tomero E, Mulero J, de Miguel E, et al. Performance of the
47 Heiland GR, Appel H, Poddubnyy D, et al. High level of functional
Assessment of Spondyloarthritis International Society criteria for
dickkopf-1 predicts protection from syndesmophyte formation in
the classification of spondyloarthritis in early spondyloarthritis
patients with ankylosing spondylitis. Ann Rheum Dis 2012;
clinics participating in the ESPERANZA programme.
71: 572–74.
Rheumatology (Oxford) 2014; 53: 353–60.
48 Tsui FW, Tsui HW, Las Heras F, Pritzker KP, Inman RD.
66 Strand V, Rao SA, Shillington AC, Cifaldi MA, McGuire M,
Serum levels of novel noggin and sclerostin-immune complexes are
Ruderman EM. Prevalence of axial spondyloarthritis in United
elevated in ankylosing spondylitis. Ann Rheum Dis 2014;
States rheumatology practices: Assessment of SpondyloArthritis
73: 1873–79.
International Society criteria versus rheumatology expert clinical
49 Poddubnyy D, Haibel H, Listing J, et al. Baseline radiographic diagnosis. Arthritis Care Res (Hoboken) 2013; 65: 1299–306.
damage, elevated acute-phase reactant levels, and cigarette smoking
67 Rudwaleit M, Khan MA, Sieper J. The challenge of diagnosis and
status predict spinal radiographic progression in early axial
classification in early ankylosing spondylitis: do we need new
spondylarthritis. Arthritis Rheum 2012; 64: 1388–98.
criteria? Arthritis Rheum 2005; 52: 1000–08.
50 Maksymowych WP, Landewe R, Conner-Spady B, et al. Serum matrix
68 Aggarwal R, Ringold S, Khanna D, et al. Distinctions between
metalloproteinase 3 is an independent predictor of structural damage
diagnostic and classification criteria? Arthritis Care Res (Hoboken)
progression in patients with ankylosing spondylitis. Arthritis Rheum
2015; 67: 891–97.
2007; 56: 1846–53.
69 van den Berg R, de Hooge M, Rudwaleit M, et al. ASAS modification
51 Poddubnyy D, Conrad K, Haibel H, et al. Elevated serum level of
of the Berlin algorithm for diagnosing axial spondyloarthritis:
the vascular endothelial growth factor predicts radiographic spinal
results from the SPondyloArthritis Caught Early (SPACE)-cohort
progression in patients with axial spondyloarthritis. Ann Rheum Dis
and from the Assessment of SpondyloArthritis international Society
2014; 73: 2137–43.
(ASAS)-cohort. Ann Rheum Dis 2013; 72: 1646–53.
52 Turina MC, Sieper J, Yeremenko N, et al. Calprotectin serum level is
70 Mandl P, Navarro-Compan V, Terslev L, et al. EULAR
an independent marker for radiographic spinal progression in axial
recommendations for the use of imaging in the diagnosis and
spondyloarthritis. Ann Rheum Dis 2014; 73: 1746–48.
management of spondyloarthritis in clinical practice.
53 Syrbe U, Callhoff J, Conrad K, et al. Serum adipokine levels in Ann Rheum Dis 2015; 74: 1327–39.
patients with ankylosing spondylitis and their relationship to
71 Poddubnyy D, Brandt H, Vahldiek J, et al. The frequency of
clinical parameters and radiographic spinal progression.
non-radiographic axial spondyloarthritis in relation to symptom
Arthritis Rheumat 2015; 67: 678–85.
duration in patients referred because of chronic back pain: results
54 Maksymowych WP, Morency N, Conner-Spady B, Lambert RG. from the Berlin early spondyloarthritis clinic. Ann Rheum Dis 2012;
Suppression of inflammation and effects on new bone formation in 71: 1998–2001.
ankylosing spondylitis: evidence for a window of opportunity in
72 Poddubnyy D, Rudwaleit M, Haibel H, et al. Rates and predictors of
disease modification. Ann Rheum Dis 2013; 72: 23–28.
radiographic sacroiliitis progression over 2 years in patients with
55 Baraliakos X, Heldmann F, Callhoff J, et al. Which spinal lesions axial spondyloarthritis. Ann Rheum Dis 2011; 70: 1369–74.
are associated with new bone formation in patients with ankylosing
73 van Tubergen A, Heuft-Dorenbosch L, Schulpen G, et al.
spondylitis treated with anti-TNF agents? A long-term observational
Radiographic assessment of sacroiliitis by radiologists and
study using MRI and conventional radiography. Ann Rheum Dis
rheumatologists: does training improve quality? Ann Rheum Dis
2014; 73: 1819–25.
2003; 62: 519–25.
56 Bleil J, Maier R, Hempfing A, Sieper J, Appel H, Syrbe U.
74 van den Berg R, Lenczner G, Feydy A, et al. Agreement between
Granulation tissue eroding the subchondral bone also promotes
clinical practice and trained central reading in reading of sacroiliac
new bone formation in ankylosing spondylitis. Arthritis Rheumat
joints on plain pelvic radiographs. Results from the DESIR cohort.
2016; 68: 2456–65.
Arthritis Rheumatol 2014; 66: 2403–11.
82 www.thelancet.com Vol 390 July 1, 2017
Seminar
75 Krohn M, Braum LS, Sieper J, et al. Erosions and fatty lesions of 94 Sieper J, Klopsch T, Richter M, et al. Comparison of two different
sacroiliac joints in patients with axial spondyloarthritis: evaluation of dosages of celecoxib with diclofenac for the treatment of active
different MRI techniques and two scoring methods. J Rheumatol ankylosing spondylitis: results of a 12-week randomised,
2014; 41: 473–80. double-blind, controlled study. Ann Rheum Dis 2008; 67: 323–29.
76 Lambert RG, Bakker PA, van der Heijde D, et al. Defining active 95 van der Heijde D, Baraf HS, Ramos-Remus C, et al. Evaluation of
sacroiliitis on MRI for classification of axial spondyloarthritis: update the efficacy of etoricoxib in ankylosing spondylitis: results of a
by the ASAS MRI working group. Ann Rheum Dis 2016; 75: 1958–63. fifty-two-week, randomized, controlled study. Arthritis Rheum 2005;
77 Weber U, Ostergaard M, Lambert RG, et al. Candidate lesion-based 52: 1205–15.
criteria for defining a positive sacroiliac joint MRI in two cohorts of 96 Kroon FP, van der Burg LR, Ramiro S, et al. Non-steroidal
patients with axial spondyloarthritis. Ann Rheum Dis 2015; 74: 1976–82. anti-inflammatory drugs (NSAIDs) for axial spondyloarthritis
78 Weber U, Zubler V, Zhao Z, et al. Does spinal MRI add incremental (ankylosing spondylitis and non-radiographic axial spondyloarthritis).
diagnostic value to MRI of the sacroiliac joints alone in patients Cochrane Database Syst Rev 2015; 7: CD010952.
with non-radiographic axial spondyloarthritis? Ann Rheum Dis 2015; 97 Wang R, Dasgupta A, Ward MM. Comparative efficacy of
74: 985–92. non-steroidal anti-inflammatory drugs in ankylosing spondylitis:
79 Hermann KG, Baraliakos X, van der Heijde DM, et al. Descriptions a Bayesian network meta-analysis of clinical trials. Ann Rheum Dis
of spinal MRI lesions and definition of a positive MRI of the spine 2016; 75: 1152–60.
in axial spondyloarthritis: a consensual approach by the ASAS/ 98 Bakland G, Gran JT, Nossent JC. Increased mortality in ankylosing
OMERACT MRI study group. Ann Rheum Dis 2012; 71: 1278–88. spondylitis is related to disease activity. Ann Rheum Dis 2011;
80 Weber U, Zhao Z, Rufibach K, et al. Diagnostic utility of candidate 70: 1921–25.
definitions for demonstrating axial spondyloarthritis on magnetic 99 Haroon NN, Paterson JM, Li P, Inman RD, Haroon N. Patients with
resonance imaging of the spine. Arthritis Rheumatol 2015; 67: 924–33. ankylosing spondylitis have increased cardiovascular and
81 Song IH, Carrasco-Fernandez J, Rudwaleit M, Sieper J. cerebrovascular mortality: a population-based study. Ann Intern Med
The diagnostic value of scintigraphy in assessing sacroiliitis in 2015; 163: 409–16.
ankylosing spondylitis: a systematic literature research. 100 Coxib and traditional NSAID Trialists’ Collaboration. Vascular and
Ann Rheum Dis 2008; 67: 1535–40. upper gastrointestinal effects of non-steroidal anti-inflammatory
82 Poddubnyy D, Vahldiek J, Spiller I, et al. Evaluation of 2 screening drugs: meta-analyses of individual participant data from
strategies for early identification of patients with axial randomised trials. Lancet 2013; 382: 769–79.
spondyloarthritis in primary care. J Rheumatol 2011; 38: 2452–60. 101 Lie E, Kristensen LE, Forsblad-d‘Elia H, et al. The effect of
83 Sieper J, Srinivasan S, Zamani O, et al. Comparison of two referral comedication with conventional synthetic disease modifying
strategies for diagnosis of axial spondyloarthritis: the Recognising antirheumatic drugs on TNF inhibitor drug survival in patients
and Diagnosing Ankylosing Spondylitis Reliably (RADAR) study. with ankylosing spondylitis and undifferentiated spondyloarthritis:
Ann Rheum Dis 2013; 72: 1621–27. results from a nationwide prospective study. Ann Rheum Dis 2015;
84 Rudwaleit M, Sieper J. Referral strategies for early diagnosis of axial 74: 970–78.
spondyloarthritis. Nat Rev Rheumatol 2012; 8: 262–68. 102 Nissen MJ, Ciurea A, Bernhard J, et al. The effect of comedication
85 van Hoeven L, Vergouwe Y, de Buck PD, Luime JJ, Hazes JM, with a csDMARD on drug retention and clinical effectiveness of
Weel AE. External validation of a referral rule for axial anti-TNF therapy in patients with axial spondyloarthritis.
spondyloarthritis in primary care patients with chronic low back Arthritis Rheumat 2016; 68: 2140–50.
pain. PLoS One 2015; 10: e0131963. 103 Breban M, Ravaud P, Claudepierre P, et al. Maintenance of
86 Deodhar A, Mittal M, Reilly P, et al. Ankylosing spondylitis infliximab treatment in ankylosing spondylitis: results of a one-year
diagnosis in US patients with back pain: identifying providers randomized controlled trial comparing systematic versus
involved and factors associated with rheumatology referral delay. on-demand treatment. Arthritis Rheum 2008; 58: 88–97.
Clin Rheumatol 2016; 35: 1769–76. 104 Heiberg MS, Koldingsnes W, Mikkelsen K, et al. The comparative
87 Poddubnyy D, van Tubergen A, Landewe R, Sieper J, one-year performance of anti-tumor necrosis factor alpha drugs in
van der Heijde D, for the Assessment of Spondylo Arthritis patients with rheumatoid arthritis, psoriatic arthritis, and
international group. Development of an ASAS-endorsed ankylosing spondylitis: results from a longitudinal, observational,
recommendation for the early referral of patients with a suspicion of multicenter study. Arthritis Rheum 2008; 59: 234–40.
axial spondyloarthritis. Ann Rheum Dis 2015; 74: 1483–87. 105 Sepriano A, Ramiro S, van der Heijde D, et al. Effect of
88 Poddubnyy D, van Tubergen A, Landewe R, Sieper J, comedication with conventional synthetic DMARDs on TNF
van der Heijde D. Defining an optimal referral strategy for patients inhibitors-retention in patients with spondyloarthritis:
with a suspicion of axial spondyloarthritis: what is really important? A prospective cohort. Arthritis Rheumat 2016; 68: 2671–79.
Response to: ‘Evaluating the ASAS recommendations for early 106 Haibel H, Heldmann F, Braun J, Listing J, Kupper H, Sieper J.
referral of axial spondyloarthritis in patients with chronic low back Long-term efficacy of adalimumab after drug withdrawal and
pain; is one parameter present sufficient for primary care practice?’ retreatment in patients with active non-radiographically evident
by van Hoeven et al. Ann Rheum Dis 2015; 74: e69. axial spondyloarthritis who experience a flare. Arthritis Rheum 2013;
89 Van Heijde D, Ramiro S, Landewé R, et al. 2016 update of the 65: 2211–13.
ASAS/EULAR management recommendations for axial 107 Braun J, Brandt J, Listing J, et al. Treatment of active ankylosing
spondyloarthritis. Ann Rheum Dis 2017; published online Jan 13. spondylitis with infliximab: a randomised controlled multicentre
DOI:10.1136/annrheumdis-2016-210770. trial. Lancet 2002; 359: 1187–93.
90 Ward MM, Deodhar A, Akl EA, et al. American College of 108 Davis JC Jr, Van Der Heijde D, Braun J, et al. Recombinant human
Rheumatology/Spondylitis Association of America/Spondyloarthritis tumor necrosis factor receptor (etanercept) for treating ankylosing
Research and Treatment Network 2015 Recommendations for the spondylitis: a randomized, controlled trial. Arthritis Rheum 2003;
Treatment of Ankylosing Spondylitis and Nonradiographic Axial 48: 3230–36.
Spondyloarthritis. Arthritis Care Res (Hoboken) 2016; 68: 151–66. 109 van der Heijde D, Kivitz A, Schiff MH, et al. Efficacy and safety of
91 Smolen JS, Braun J, Dougados M, et al. Treating spondyloarthritis, adalimumab in patients with ankylosing spondylitis: results of a
including ankylosing spondylitis and psoriatic arthritis, to target: multicenter, randomized, double-blind, placebo-controlled trial.
recommendations of an international task force. Ann Rheum Dis Arthritis Rheum 2006; 54: 2136–46.
2014; 73: 6–16. 110 Inman RD, Davis JC Jr, Heijde D, et al. Efficacy and safety of
92 Song IH, Poddubnyy DA, Rudwaleit M, Sieper J. Benefits and risks golimumab in patients with ankylosing spondylitis: results of a
of ankylosing spondylitis treatment with nonsteroidal randomized, double-blind, placebo-controlled, phase III trial.
antiinflammatory drugs. Arthritis Rheum 2008; 58: 929–38. Arthritis Rheum 2008; 58: 3402–12.
93 Sieper J, Lenaerts J, Wollenhaupt J, et al. Efficacy and safety of 111 Landewe R, Braun J, Deodhar A, et al. Efficacy of certolizumab
infliximab plus naproxen versus naproxen alone in patients with pegol on signs and symptoms of axial spondyloarthritis including
early, active axial spondyloarthritis: results from the double-blind, ankylosing spondylitis: 24-week results of a double-blind
placebo-controlled INFAST study, Part 1. Ann Rheum Dis 2014; randomised placebo-controlled Phase 3 study. Ann Rheum Dis 2014;
73: 101–07. 73: 39–47.
www.thelancet.com Vol 390 July 1, 2017 83
Seminar
112 Davis JC, van der Heijde DM, Braun J, et al. Sustained durability 129 Sieper J, Porter-Brown B, Thompson L, Harari O, Dougados M.
and tolerability of etanercept in ankylosing spondylitis for 96 weeks. Assessment of short-term symptomatic efficacy of tocilizumab in
Ann Rheum Dis 2005; 64: 1557–62. ankylosing spondylitis: results of randomised, placebo-controlled
113 van der Heijde D, Dijkmans B, Geusens P, et al. Efficacy and safety trials. Ann Rheum Dis 2014; 73: 95–100.
of infliximab in patients with ankylosing spondylitis: results of a 130 Sieper J, Braun J, Kay J, et al. Sarilumab for the treatment of
randomized, placebo-controlled trial (ASSERT). Arthritis Rheum ankylosing spondylitis: results of a Phase II, randomised,
2005; 52: 582–91. double-blind, placebo-controlled study (ALIGN). Ann Rheum Dis
114 Baeten D, Sieper J, Braun J, et al. Secukinumab, an Interleukin-17A 2015; 74: 1051–57.
Inhibitor, in Ankylosing Spondylitis. N Engl J Med 2015; 131 Sieper J, Deodhar A, Marzo-Ortega H, et al. Secukinumab Efficacy
373: 2534–48. in Anti–TNF-naïve and Anti–TNF-experienced Subjects with Active
115 Sieper J, van der Heijde D, Dougados M, et al. Efficacy and safety of Ankylosing Spondylitis: Results from the MEASURE 2 Study.
adalimumab in patients with non-radiographic axial Ann Rheum Dis 2016; published online Aug 31. DOI:10.1136/
spondyloarthritis: results of a randomised placebo-controlled trial annrheumdis-2016-210023.
(ABILITY-1). Ann Rheum Dis 2013; 72: 815–22. 132 Braun J, Baraliakos X, Deodhar A, et al. Effect of secukinumab on
116 Dougados M, van der Heijde D, Sieper J, et al. Symptomatic efficacy clinical and radiographic outcomes in ankylosing spondylitis: 2-year
of etanercept and its effects on objective signs of inflammation in results from the randomised phase III MEASURE 1 study.
early nonradiographic axial spondyloarthritis: a multicenter, Ann Rheum Dis 2016; published online Dec 13. DOI:10.1136/
randomized, double-blind, placebo-controlled trial. annrheumdis-2016-209730.
Arthritis Rheumat 2014; 66: 2091–102. 133 Poddubnyy D, Hermann KG, Callhoff J, Listing J, Sieper J.
117 Sieper J, van der Heijde D, Dougados M, et al. a randomized, Ustekinumab for the treatment of patients with active ankylosing
double-blind, placebo-controlled, sixteen-week study of spondylitis: results of a 28-week, prospective, open-label,
subcutaneous golimumab in patients with active nonradiographic proof-of-concept study (TOPAS). Ann Rheum Dis 2014; 73: 817–23.
axial spondyloarthritis. Arthritis Rheumat 2015; 67: 2702–12. 134 van der Heijde D, Deodhar A, Wei J, et al. Tofacitinib in patients with
118 Brown MD, Bird PA, Robinson PC, et al. Baseline MRI/CRP as ankylosing spondylitis: A phase 2, 16 week, randomized,
predictors of response to etanercept in the management of patients placebo-controlled, dose-ranging study. American College of
with non-radiographic axial spondyloarthritis. Ann Rheum Dis 2015; Rheumatology conference 2015; San Francisco, CA;
74 (suppl 2): 752. Nov 6–11, 2015; 5L.
119 Rudwaleit M, Schwarzlose S, Hilgert ES, Listing J, Braun J, Sieper J. 135 Pathan E, Abraham S, Van Rossen E, et al. Efficacy and safety of
MRI in predicting a major clinical response to anti-tumour necrosis apremilast, an oral phosphodiesterase 4 inhibitor, in ankylosing
factor treatment in ankylosing spondylitis. Ann Rheum Dis 2008; spondylitis. Ann Rheum Dis 2013; 72: 1475–80.
67: 1276–81. 136 US National Library of Science. 2016. https://clinicaltrials.gov/ct2/
120 Sieper J, Poddubnyy D. New evidence on the management of show/results/NCT01583374?sect=X3401256%23wrapper
spondyloarthritis. Nat Rev Rheumatol 2016; 12: 282–95. (accessed Dec 19, 2016).
121 Baraliakos X, Listing J, Brandt J, et al. Clinical response to 137 van der Heijde D, Landewe R, Baraliakos X, et al. Radiographic
discontinuation of anti-TNF therapy in patients with ankylosing findings following two years of infliximab therapy in patients with
spondylitis after 3 years of continuous treatment with infliximab. ankylosing spondylitis. Arthritis Rheum 2008; 58: 3063–70.
Arthritis Res Ther 2005; 7: R439–44. 138 Braun J, Baraliakos X, Hermann KG, et al. The effect of
122 Song IH, Althoff CE, Haibel H, et al. Frequency and duration of two golimumab doses on radiographic progression in ankylosing
drug-free remission after 1 year of treatment with etanercept versus spondylitis: results through 4 years of the GO-RAISE trial.
sulfasalazine in early axial spondyloarthritis: 2 year data of the Ann Rheum Dis 2014; 73: 1107–13.
ESTHER trial. Ann Rheum Dis 2012; 71: 1212–15. 139 Haroon N, Inman RD, Learch TJ, et al. The impact of tumor
123 Haibel H, Heldmann F, Listing J, Kupper H, Braun J, Sieper J. necrosis factor alpha inhibitors on radiographic progression in
Long-term efficacy of adalimumab after drug withdrawal and ankylosing spondylitis. Arthritis Rheum 2013; 65: 2645–54.
retreatment of flare patients in active non-radiographic, axial 140 Baraliakos X, Haibel H, Listing J, Sieper J, Braun J. Continuous
spondyloarthritis. Arthritis Rheum 2013; 65: 2211–13. long-term anti-TNF therapy does not lead to an increase in the rate
124 Sieper J, Lenaerts J, Wollenhaupt J, et al. Maintenance of of new bone formation over 8 years in patients with ankylosing
biologic-free remission with naproxen or no treatment in patients spondylitis. Ann Rheum Dis 2014; 73: 710–15.
with early, active axial spondyloarthritis: results from a 6-month, 141 Wanders A, Heijde D, Landewe R, et al. Nonsteroidal
randomised, open-label follow-up study, INFAST Part 2. antiinflammatory drugs reduce radiographic progression in
Ann Rheum Dis 2014; 73: 108–13. patients with ankylosing spondylitis: a randomized clinical trial.
125 Cantini F, Niccoli L, Cassara E, Kaloudi O, Nannini C. Duration of Arthritis Rheum 2005; 52: 1756–65.
remission after halving of the etanercept dose in patients with 142 Boersma JW. Retardation of ossification of the lumbar vertebral
ankylosing spondylitis: a randomized, prospective, long-term, column in ankylosing spondylitis by means of phenylbutazone.
follow-up study. Biologics 2013; 7: 1–6. Scand J Rheumatol 1976; 5: 60–64.
126 Yates M, Hamilton LE, Elender F, et al. Is etanercept 25 mg once 143 Poddubnyy D, Rudwaleit M, Haibel H, et al. Effect of non-steroidal
weekly as effective as 50 mg at maintaining response in patients anti-inflammatory drugs on radiographic spinal progression in
with ankylosing spondylitis? a randomized control trial. J Rheumatol patients with axial spondyloarthritis: results from the German
2015; 42: 1177–85. Spondyloarthritis Inception Cohort. Ann Rheum Dis 2012;
127 Song IH, Heldmann F, Rudwaleit M, et al. Different response to 71: 1616–22.
rituximab in tumor necrosis factor blocker-naive patients with active 144 Sieper J, Listing J, Poddubnyy D, et al. Effect of continuous versus
ankylosing spondylitis and in patients in whom tumor necrosis on-demand treatment of ankylosing spondylitis with diclofenac over
factor blockers have failed: a twenty-four-week clinical trial. 2 years on radiographic progression of the spine: results from a
Arthritis Rheum 2010; 62: 1290–97. randomised multicentre trial (ENRADAS). Ann Rheum Dis 2016;
128 Song IH, Heldmann F, Rudwaleit M, et al. One-year follow-up of 75: 1438–43.
ankylosing spondylitis patients responding to rituximab treatment
and re-treated in case of a flare. Ann Rheum Dis 2013; 72: 305–06.
84 www.thelancet.com Vol 390 July 1, 2017
You might also like
- EspondiloartritisDocument16 pagesEspondiloartritisyirsongamita002No ratings yet
- Ankylosing Spondylitis Review JournalDocument12 pagesAnkylosing Spondylitis Review Journaloccha_fun08100% (1)
- Espondiloartritis NEJMDocument12 pagesEspondiloartritis NEJMJosué Nando BucioNo ratings yet
- IndianJClinAnaesth 9 3 374 378Document5 pagesIndianJClinAnaesth 9 3 374 378bhaskaracharya dontabhaktuniNo ratings yet
- Os 15 1454Document14 pagesOs 15 1454tugas rendyNo ratings yet
- Infectious Spondylodiscitis - A Case Series AnalysisDocument4 pagesInfectious Spondylodiscitis - A Case Series AnalysisCarlos Pacichana AgudeloNo ratings yet
- Ankylosing Spondylitis BMJ RevDocument5 pagesAnkylosing Spondylitis BMJ RevsamarqandiNo ratings yet
- Enthesitis in Psoriatic Arthritis 2013Document10 pagesEnthesitis in Psoriatic Arthritis 2013micamart.94No ratings yet
- bmj33300581 PDFDocument5 pagesbmj33300581 PDFLiisa ApriliaNo ratings yet
- البحثDocument36 pagesالبحثabdelazimlabib1982No ratings yet
- Out 5Document7 pagesOut 5abdelazimlabib1982No ratings yet
- 1 s2.0 S266654842300077X MainDocument7 pages1 s2.0 S266654842300077X MainOncología CdsNo ratings yet
- Ankylosing Spondylarthritis PDFDocument3 pagesAnkylosing Spondylarthritis PDFMa OlayaNo ratings yet
- EpicondilteDocument7 pagesEpicondilteRicardo fariaNo ratings yet
- Preferred Examination: Spondylitis Ankylosing SpondylitisDocument6 pagesPreferred Examination: Spondylitis Ankylosing SpondylitischrisantyNo ratings yet
- Professor Maxime ComicsDocument3 pagesProfessor Maxime ComicsZeeshan IslamNo ratings yet
- 2017 SpondyloarthritisDocument2 pages2017 SpondyloarthritisGer Maine ApalisokNo ratings yet
- ARTROGRIPOSISDocument7 pagesARTROGRIPOSISAna ChazarraNo ratings yet
- Spondylodiscitis Severity Code: Scoring System For The Classification and Treatment of Non-Specific SpondylodiscitisDocument9 pagesSpondylodiscitis Severity Code: Scoring System For The Classification and Treatment of Non-Specific SpondylodiscitisEduardo RodriguezNo ratings yet
- Physiotherapy Management of SciaticaDocument6 pagesPhysiotherapy Management of SciaticaMuly Arafah ZakariaNo ratings yet
- Diagnosis and Management of Spinal InfectionsDocument6 pagesDiagnosis and Management of Spinal Infectionsdr.maulanahutabaratNo ratings yet
- Spondylodiscitis Revisited: SpineDocument15 pagesSpondylodiscitis Revisited: SpineLeonleashNo ratings yet
- Pola 2017Document10 pagesPola 2017RobertoNo ratings yet
- Hip Spine Syndrome - A Case Series and Literature ReviewDocument6 pagesHip Spine Syndrome - A Case Series and Literature ReviewCar MartNo ratings yet
- Differential Diagnosis of Polyarticular ArthritisDocument7 pagesDifferential Diagnosis of Polyarticular ArthritismedicabrujaNo ratings yet
- Patient - Info/doctor/ankylosing Spondylitis ProDocument8 pagesPatient - Info/doctor/ankylosing Spondylitis ProJasleen KaurNo ratings yet
- Presentation - JointsDocument21 pagesPresentation - JointsAlejandra MorenoNo ratings yet
- Suspecting and Diagnosing The Patient With Spondyloarthritis 2021. CLINICSDocument15 pagesSuspecting and Diagnosing The Patient With Spondyloarthritis 2021. CLINICSluisa100% (1)
- Psoriatic ArthritisDocument14 pagesPsoriatic ArthritisRoberto López Mata100% (2)
- POTT's DiseaseDocument3 pagesPOTT's DiseaseFema Jill AtrejenioNo ratings yet
- Clasificación EspondilopatiasDocument5 pagesClasificación EspondilopatiasHeidyxer OsorioNo ratings yet
- 1 s2.0 S1297319X21002062 MainDocument7 pages1 s2.0 S1297319X21002062 Mainabood softNo ratings yet
- Bydon 2019Document6 pagesBydon 2019julyanetorquatoNo ratings yet
- Zarghooni2012 Article TreatmentOfSpondylodiscitisDocument7 pagesZarghooni2012 Article TreatmentOfSpondylodiscitisRoxana StanciuNo ratings yet
- Nejmcp 2032396Document10 pagesNejmcp 2032396juan carlosNo ratings yet
- Psoriatic ArthritisDocument12 pagesPsoriatic ArthritisSelvia RosadiNo ratings yet
- SpondilodiscytisDocument16 pagesSpondilodiscytischristinawiyaniputriNo ratings yet
- An Approach To A Child With ArthritisDocument9 pagesAn Approach To A Child With Arthritispadamati govardhan reddy reddyNo ratings yet
- Axial Psoriatic Arthritis An UpdateDocument10 pagesAxial Psoriatic Arthritis An Updateproject zoroNo ratings yet
- Bland 1984Document28 pagesBland 1984Hellmann Adrian Escobar CNo ratings yet
- Koes2006 PDFDocument5 pagesKoes2006 PDFDewi FathmahNo ratings yet
- Pyogenic Spinal InfectionsDocument16 pagesPyogenic Spinal InfectionsFrancisco Escobar MoralesNo ratings yet
- SpondyloarthritisDocument22 pagesSpondyloarthritisIFREEN IMDAD HUSAIN QURESHINo ratings yet
- General Principles in The Medical and Surgical Management of Spinal Infections A Multidisciplinary ApproachDocument16 pagesGeneral Principles in The Medical and Surgical Management of Spinal Infections A Multidisciplinary Approachdr.maulanahutabaratNo ratings yet
- Apyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiDocument131 pagesApyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiFathimathNo ratings yet
- Aapm 11 1 112825Document8 pagesAapm 11 1 112825david ahmad wibowoNo ratings yet
- Protrusio Acetabuli Diagnosis and TreatmentDocument10 pagesProtrusio Acetabuli Diagnosis and TreatmentFerney Leon BalceroNo ratings yet
- IDSADocument21 pagesIDSADiana AvilesNo ratings yet
- The Classification and Diagnostic Criteria of Ankylosing SpondylitisDocument6 pagesThe Classification and Diagnostic Criteria of Ankylosing SpondylitisAnggita RifkyNo ratings yet
- 2016NMCDISHSDocument6 pages2016NMCDISHSthanawatsimaNo ratings yet
- Psoriatic ArthritisDocument14 pagesPsoriatic Arthritisamirra92No ratings yet
- Ankylosing Spondylitis...Document6 pagesAnkylosing Spondylitis...mfahrizaNo ratings yet
- Diagnostics 12 00618Document9 pagesDiagnostics 12 00618macox77No ratings yet
- Sjogren ReviewDocument11 pagesSjogren ReviewMariano AlbertalNo ratings yet
- Polymyalgia Rheumatica - Lancet (2023)Document14 pagesPolymyalgia Rheumatica - Lancet (2023)1DMANUEL Suarez MejiaNo ratings yet
- 264 2023 Article 5805Document9 pages264 2023 Article 5805Samanta Catalina Egaña TabiloNo ratings yet
- Brief Review Piriformis Syndrome Etiology DiagnosiDocument11 pagesBrief Review Piriformis Syndrome Etiology DiagnosiyonisfuadNo ratings yet
- Lumbar Spinal Stenosis: Syndrome, Diagnostics and Treatment: Nature Reviews Neurology August 2009Document13 pagesLumbar Spinal Stenosis: Syndrome, Diagnostics and Treatment: Nature Reviews Neurology August 2009Surya PangeranNo ratings yet
- Neuropathic Diabetic Foot Ulcers: Clinical PracticeDocument8 pagesNeuropathic Diabetic Foot Ulcers: Clinical PracticeAnisa SafutriNo ratings yet
- Small Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationFrom EverandSmall Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationSung-Tsang HsiehNo ratings yet
- ResumeDocument2 pagesResumeapi-374835380No ratings yet
- Guidance On Ethics of TBDocument38 pagesGuidance On Ethics of TBRhea Derije100% (1)
- Herpes Virus Association Press Release (RV Golding) 2014Document2 pagesHerpes Virus Association Press Release (RV Golding) 2014HIV Justice NetworkNo ratings yet
- Current Treatment Modalities and Role of NurseDocument42 pagesCurrent Treatment Modalities and Role of NurseHemantNo ratings yet
- LeukemiaDocument8 pagesLeukemiaIrmaNo ratings yet
- I-Mbbs Practical Time TableDocument2 pagesI-Mbbs Practical Time TablealienofmarzNo ratings yet
- US RU EN Fin2Document189 pagesUS RU EN Fin2Constantinescu DragosNo ratings yet
- International Emergency Nursing: A D A B CDocument9 pagesInternational Emergency Nursing: A D A B CPUSKESMAS KECAMATAN KEPULAUAN SERIBU UTARANo ratings yet
- Explained: Cost-Utility AnalysisDocument12 pagesExplained: Cost-Utility AnalysisCandraNo ratings yet
- 2024 ACVIP 0-18yrs-Child-Combined-ScheduleDocument15 pages2024 ACVIP 0-18yrs-Child-Combined-ScheduleboriyawalamNo ratings yet
- Oral Malodor: Nidhi Sharma InternDocument21 pagesOral Malodor: Nidhi Sharma InternRichaNo ratings yet
- 03.practical Session-Evidence Based Medicine-Jarir at Thobari-CEBU (2015)Document17 pages03.practical Session-Evidence Based Medicine-Jarir at Thobari-CEBU (2015)JipeeZedNo ratings yet
- 14.7pulse Polio ProgrammeDocument5 pages14.7pulse Polio Programmevenkat krishnan100% (1)
- Emergency Medical Services Agency Lessons Learned: To: AlDocument4 pagesEmergency Medical Services Agency Lessons Learned: To: AlMega MuzdalifahNo ratings yet
- Literatur 2Document7 pagesLiteratur 2aninuraniyahNo ratings yet
- Key Skills For Hospital DoctorsDocument3 pagesKey Skills For Hospital DoctorsMustafaNo ratings yet
- Bedside Handover SOP PDFDocument20 pagesBedside Handover SOP PDFDewi Ratna Sari100% (1)
- 2nd Quarter Exam - PEDocument6 pages2nd Quarter Exam - PENhedzCaidoNo ratings yet
- Sitxwhs004 Assessment Project 1 Assessor Guide: Task 2 InstructionsDocument5 pagesSitxwhs004 Assessment Project 1 Assessor Guide: Task 2 InstructionsUsman HassanNo ratings yet
- Jurnal Kebijakan Kesehatan Indonesia: Halaman JudulDocument10 pagesJurnal Kebijakan Kesehatan Indonesia: Halaman Judulmaulana rosyNo ratings yet
- A Case of Intravaginal Foreign BodyDocument3 pagesA Case of Intravaginal Foreign BodyNara SafaNo ratings yet
- Assessment Nursing Diagnosis Analysis Goals and Objectives Nursing Interventions Rationale Evaluation EffectivenessDocument3 pagesAssessment Nursing Diagnosis Analysis Goals and Objectives Nursing Interventions Rationale Evaluation EffectivenessYnah Sayoc75% (4)
- AtherosclerosisDocument19 pagesAtherosclerosissanjivdasNo ratings yet
- COSHH Assessment Sheet: Material InformationDocument2 pagesCOSHH Assessment Sheet: Material InformationSelvaNo ratings yet
- Difficult Labor (Dystocia) : Disproportion Between The Presenting Part of The Fetus and The Birth CanalDocument9 pagesDifficult Labor (Dystocia) : Disproportion Between The Presenting Part of The Fetus and The Birth CanalMohammad Hadi AlghuraifiNo ratings yet
- 11 Suturing21012015Document30 pages11 Suturing21012015Putri Sari SeptirianiNo ratings yet
- Gardasil VAERS Adverse ReactionsDocument1,824 pagesGardasil VAERS Adverse Reactionsmcdonald.rr100% (2)
- Nurses, Negligence, Malpractice: An Analysis Based On More Than 250 Cases Against NursesDocument10 pagesNurses, Negligence, Malpractice: An Analysis Based On More Than 250 Cases Against NursesLesterNo ratings yet
- Why Do We Fall Ill Class 9 Mcqs Questions With AnswersDocument7 pagesWhy Do We Fall Ill Class 9 Mcqs Questions With AnswersSCIENCE WORK [AMP] ActivitiesNo ratings yet
- Categorizing The Stage of Glaucoma From Pre-Diagnosis To End-Stage DiseaseDocument7 pagesCategorizing The Stage of Glaucoma From Pre-Diagnosis To End-Stage DiseaseKatrina ChauNo ratings yet