NSTP
NSTP
Uploaded by
arrianne lou narral FerolinoCopyright:
Available Formats
NSTP
NSTP
Uploaded by
arrianne lou narral FerolinoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
NSTP
NSTP
Uploaded by
arrianne lou narral FerolinoCopyright:
Available Formats
Introduction
The foundations of lifelong responsibility for the maintenance of
personal hygiene are laid down in childhood, which is important for a
healthy childhood, for a healthy adulthood and for the development of
positive values about health and the use of health services.
The Philippines has a large population of children and young people. In
2010, there were 36,615,596 children aged 0–17 in the population which
is 39.7 per cent of the total population. About 18,862,159 (51.5 per cent)
were male and 17,753, 437 (48.5 per cent) were female.25 Unfortunately,
the 2015 census data available does not contain figures on the child
population. The fertility rate in the Philippines has been steadily dropping,
from 6.0 children per woman in 1973 to 3.5 in 2003 and 2.94 in 2016.26
The Poor health among school children is resulted from the lack of
awareness of the health benefits of personal hygiene. Diarrhea diseases,
skin diseases, worm infestations and dental diseases are most commonly
associated with poor personal hygiene. One of the major problems faced
by school children are infections. The primary causes of infections are
contaminated water and poor sanitation, as well as poor hygienic
practices. Lack of personal hygiene coupled with poor sanitation favor
person-to-person transmission of infection. Infection and malnutrition
form a vicious circle and retard children’s physical development.
Repeated attacks of infections often compound the existing poor health of
children, compromising children’s attendance and performance at school
and not uncommonly, can result in death [1]. The condition may even be
worse in a slum community with poor socio-economic condition and
compromised living situation. The origins of many of the illnesses of
adulthood also have their roots in the health behaviors of childhood and
adolescence.
However, majority of the childhood illnesses are preventable by
promotion of hygienic practices among school children through proper
health education by their parents and teachers. Children in their primary
schooling age can learn specific health-promoting behaviors, even if they
do not fully understand the connections between illness and behavior [2].
Health habits can be developed in this period. More research on this
ground is needed. The present inadequate knowledge base hinders the
development of improved strategies for enhancing the maintenance of
personal hygiene, which is of great importance to decrease the burden of
communicable diseases in the developing countries. The increased burden
of communicable diseases among school children due to poor personal
hygiene practices and inadequate sanitary conditions remains a concern
on the public health agenda in developing countries [1]. School children
are particularly vulnerable to neglect of basic personal hygiene due lack
of knowledge and practice [2]. Poor knowledge, practice of and attitudes
to personal hygiene such as hand washing play major roles in the high
incidence of communicable diseases and therefore has negative
consequences for a child’s long term overall development [3]. Improved
awareness and hand hygiene practices especially among children have
effectively reduced gastrointestinal and respiratory tract infections by up
to 50% the two leading causes of childhood morbidity and mortality
around the world [4-6]. In addition, studies have also shown that school
children with better knowledge and practices of personal hygiene have
fewer sick days and absenteeism in school and achieve higher grades [2,
7]. School is the place where health education regarding important aspects
of hygiene, environment and sanitation, as well as social customs is being
imparted [8]. Health is a key factor in school entry, as well as continued
participation and attainment in school. The teacher is the guardian of the
child in school and plays a pivotal role in the whole process of primordial
prevention [9]. Bearing in mind that school children have been
consistently implicated in the spread of communicable diseases and that
the school has been recognized as a vital setting for health promotion [10],
this study was planned to assess personal hygiene in primary school
children in Sharjah, United Arab Emirates. The aim of this study was to
investigate existing knowledge and practices related to personal hygiene
among primary school children between grade 1 and 5. The results from
the study will help to understand the factors influencing the personal
hygiene behaviors in primary school children and to overcome barriers in
acquisition of proper knowledge and practices.
Background of the study
Adequate nutrition during early childhood is fundamental to the
development of each
child’s potential. It is established that the period from birth to two years
of age is a
“critical window” for the promotion of optimal growth, health and overall
survival of
children (Ali, et al 2006).
Good food is important for good health. Children who are well fed during
the first two
years of life are more likely to stay healthy for the rest of their childhood.
During the
first six months of a child’s life, breast milk alone is the ideal food. It
contains all the
nutrients needed for healthy growth as well as immune factors that protect
against
common childhood infections (Ashworth, 2002).
Good nutrition is the cornerstone for survival, health and development for
current and
succeeding generations. Well-nourished children perform better in school,
grow into
healthy adults and in turn give their children a better start in life (UNICEF,
2006). The
United Nations Children’s Fund (UNICEF) and the Ministry of Health
(MoH), Ghana
recommend exclusive breastfeeding for the first six months of the infant’s
life. Children
between the ages of six months and four years who do not get enough of
the right types
of food to eat easily become malnourished
According to UNICEF (2006), each year under-nutrition contributes to
the deaths of
about 5.6 million children under- 5 in the developing world and 146
million children
younger than 5 are underweight and at increased risk of early death,
illness, disability,
and underachievement. UNICEF reports that, in the least developed
countries, 42% of
children are stunted and 36% are underweight as a result of poor nutrition
or under
nutrition.
The World Health Organization (WHO) refers to malnutrition as “Failure
of cells to
perform their physical functions due to inability to receive and use the
energy and
nutrients needed in terms of amount, mix and timeliness. Waterlow and
Insel (1995)
described malnutrition as “Failing Health that results from long standing
faulty
nutrition that either fails to meet or greatly exceeds nutritional needs. This
description
could mean inappropriateness of the food taken. Again, Harrison and
Waterlow (1990)
defined malnutrition as “The effects of any nutrient deficiency including
energy, protein
and micronutrients.”
Malnutrition can be operationally defined as a lack of essential nutrients
or failure to
use available foods to best advantage (Barasi, 1997). Malnutrition affects
physical
growth, morbidity, mortality, cognitive development, reproduction and
physical work
capacity and it consequently impacts on human performance, health and
survival. A
well- nourished child is one whose weight and height measurements
compare very well
with the standard normal distribution of heights and weighs of healthy
children of the
RRL
The children of today will be the adults of tomorrow. By focusing
on children today, by giving them tools and knowledge to change
behavior, future generations can be stronger and healthier [1]. In the
present study, it has been observed that the female students obtained
significantly higher average score than the male students regarding the
knowledge of personal hygiene. This study shows that 98 (94.23%)
primary school children washed their hands after visiting toilet and 88
(84.62%) washed their hands before eating. Also, 50 (48.08%) primary
school children combed their hair, 52 (50%) brushed their teeth, 80
(76.92%) trimmed their nails, 44 (42.31%) took daily bath, 58 (55.77%)
wore shoes and only 13 (12.5%) wore clean clothes. These observations
clearly indicate that hygienic practices for all the indicators of personal
hygiene were not adequate among the study population. A study
conducted in Philippines (1996) indicated that 71.4% school children
washed their hands after using toilet and 75.9% washed their hands before
eating. Also, 65.2% school children took daily bath and 63.8% wore
slippers and shoes most of the time. Only 39.5% regularly trimmed their
nails [3]. A study conducted by Dongre et al. (2006) among tribal school
children in India reported that only 27.6% students (6-14 years) had clean
and combed hair, 29.7% had clean and cut nails, 42.8% wore clean clothes
and 33.8% had clean teeth before implementing the school health
education program [4]. Another study by Dongre et al. (2007) in rural
India documented that 63.6% school going children (6-14 years) had
practice of hand washing with soap after defecation and 67.8% had clean
and cut nails before initiating hygiene education [5]. A study done in rural
Ethiopia by Vivas et al. (2010) shows that 99% of primary school children
(mean age 10.8 years) washed their hands before meals, whereas only
15% washed their hands after defecation on the day prior to the
interview [6]. Therefore, the present study and similar studies from the
developing countries show that the practices of personal hygiene are not
satisfactory among primary school children in the developing world. The
present study also shows that there was a wide gap between practice and
knowledge regarding most of the indicators of personal hygiene. This
finding corroborates with the study done in Philippines (1996) [3], as well
as with a study by Oyibo (2012) done in Nigeria among school children
aged 6-14 years [7]. It is quite expected that a lesser percentage of students
having correct knowledge will be able to translate their knowledge into
practice. This has been observed clearly in the present study, and this
observation supports the principle of health education that knowledge
does not necessarily lead to practice. In addition, lack of proper resources,
i.e. soap and water, as well as inadequate sanitation facilities in a slum
community with low socio-economic condition may negatively affect
personal hygiene practices. Moreover, it has been observed that a good
fraction of students have adopted to the right practices regarding some of
the indicators, e.g. wearing shoes, without having correct knowledge on
it. Even, misconceptions regarding the maintenance of personal hygiene
were not uncommon among the primary school children, as observed in
this study. This indicates that enhancement of knowledge is necessary,
and the depth to which the knowledge is imparted to the students is not
adequate. This calls for immediate attention of measures so that the
knowledge is enhanced, as well the depth of knowledge is increased
among primary school children. In this regard, the school teachers, parents
and other family members could play a vital role. Even, children can also
be the agents of change subsequently by spreading what they have learned
in school to their family and community members. In this connection, the
Total Sanitation Campaign (TSC) as launched by Government of India in
1999 worth acknowledgement. The TSC gave emphasis on personal
Tab. III. distribution of students having misconceptions regarding
personal hygiene (n = 104). Misconceptions among students regarding*
Number (%) Combing hair 1 (0.96) Studying under adequate light 62
(59.62) Brushing teeth 14 (13.46) Washing mouth after eating 3 (2.88)
Washing hands before eating 4 (3.85) Washing hands after visiting toilet
1 (0.96) Trimming nails 2 (1.92) Taking bath daily 14 (13.46) Wearing
shoes 78 (75.00) Wearing clean clothes 89 (85.58) * multiple responses.
Tab. IV. distribution of students according to morbidities related to poor
personal hygiene (n = 104). Morbidities related to poor personal hygiene*
(history over last 15 days) Number (%) Fever with or without cough / cold
57 (54.81) diarrhea 59 (56.73) passage of worms in stool 47 (45.19) head
lice 42 (40.38) dental caries 10 (9.62) Scabies 41 (39.42) multiple boils 8
(7.69) * multiple responses.
Personal Hygiene among school children hygiene, home sanitation, safe
water, garbage disposal and wastewater disposal. It emphasized more on
health education, human resource development, and capacity
development activities to increase awareness and sanitation demand [1].
The TSC also laid strong focus on school sanitation and hygiene
promotion. Among the main objectives of the TSC, accelerating sanitation
coverage and promoting hygiene behavior among students and teachers
are worth mentioning [8]. In this study, almost 75% of the primary school
children were suffering from one or more morbidities related to poor
personal hygiene. The most common morbidity reported by them was
diarrhoea (56.73%), followed by fever with or without cough / cold
(54.81%), passage of worms in stool (45.19%), head lice (40.38%),
scabies (39.42%), dental caries (9.62%) and multiple boils (7.69%). These
observations are quite similar to that of the study by Dongre et al. (2006)
among tribal school children in India [4], where 56.6% students had
diarrhoea, fever and upper RTI (respiratory tract infections), followed by
head lice (42.8%), scabies (36.6%), multiple boils (8.9%), dental caries
(8.3%) and history of worm infestation (28.9%) before implementing the
school health education program. In the present study, more than half of
the primary school children (59.15%) with illiterate mothers obtained
good score, followed by poor score (25.35%). Whereas, almost half of the
primary school children (48.48%) with maternal education primary and
above obtained very good score. Nine primary school children (8.65%)
obtained excellent score and their mothers had middle school education
and above. Only one primary school children (out of 33) with maternal
education primary and above obtained poor score, whereas no primary
school children (out of 71) with illiterate mother obtained excellent score.
Statistically significant association was observed between practices of
personal hygiene among primary school children and literacy status of
their mother (p < 0.001). In this connection, it can be said that maternal
education can play a vital role in the practices of hygiene and health
among their children. As an illiterate or uneducated mother may be less
knowledgeable about teaching her children proper personal hygiene
practices. So, continuing health education program directed to the parents
with a special emphasis on their role to improve the health habits of their
children may hold promise.
The Author acknowledges the limitations of this study and implications
for future improvement. First, the sample size was small. Second, the
nutritional status of the children was not studied, which might be related
to the state of personal hygiene as well as related morbidities. Third,
morbidity pattern of the children was assessed by history and clinical
examination. No attempt was made to perform any laboratory test, e.g.
stool examination for parasites to detect the presence of any parasitic
infection. These aspects need to be taken care of in future. This study was
undertaken among the primary school children in a slum area of Kolkata,
India. The findings of the study might not corroborate with similar studies
from non-slum areas of Kolkata, as the low socio-economic condition and
the compromised living situation in a slum community along with
inadequate primary health care services do not allow its people to adopt
proper hygienic behavior and to observe good health.
Conclusions
It can be concluded from the present study that knowledge and practice of
personal hygiene among the primary school children in a slum area of
Kolkata, India is not satisfactory. Although, female students appear to be
more knowledgeable than the male students. Sadly, knowledge and
practice on all the indicators of personal hygiene are not commensurate
and they are not equally good on all the indicators of personal hygiene
among the primary school children. Even, misconceptions do exist on
certain indicators of personal hygiene among the students. Students with
poor hygienic practices mostly suffer from diarrhea, fever with or without
cough / cold, passage of worms in stool, head lice, scabies, dental caries
and multiple boils. Therefore, there is an immediate need for enhancement
of knowledge among the primary school children, where teachers and
parents can play a pivotal role. School based health education program
may be a useful effort in this regard. In this connection, the role of parent-
teacher associations in all the schools should be emphasized. Maternal
education appears to have a direct relation with the practices of personal
hygiene among the primary school children.
Health financing
In the Philippines, health financing is fragmented with insufficient
government investment, inappropriate incentives for providers, weak
social protection and high inequity. Figures on coverage by PhilHealth
vary, compounded by an inadequate information system on membership.
In 2008 the Demographic Household Survey indicates a PhilHealth
coverage rate of 38%.
In 2007 expenditures on health services were paid for by the government
(33%) and out-of-pocket payments (57.00%) and total health expenditure
per capita was US$68. Government funding is a share from general
taxation. Several earmarked taxes are also directed to PhilHealth; these
include: value added tax, sin tax, stamp tax and excise tax. A small
proportion of funding comes from private insurance, HMOs,
employment-based plans and private schools. Foreign assisted projects
comprise only 1.7% of health finances.
Both public and private facilities operate on a fee-for-service basis,
although public services receive greater subsidy from PhilHealth. The
PhilHealth benefits scheme pays for a defined set of services at
predetermined rates, beyond which patients pay out-of-pocket. PhilHealth
reimbursements are paid directly to service providers. Public hospital
professional fees and stays are free of charge, but the cost of medicines,
supplies, and diagnostics while in hospital are covered by PhilHealth
within the predetermined rate. Public hospitals have private rooms and
pay-wards that can be partly covered by PhilHealth. A few government
agencies and charity organizations offer further subsidies or discounts for
the poor and indigent, but no standard policy exists. Senior citizens and
the disabled also have additional discounts. PhilHealth subsidizes direct
medical costs up to a certain level in private hospitals through direct
reimbursement to providers. Patients make out-of-pocket co-payments.
Outpatient consultations and ongoing requirements for drugs are not yet
included in the benefits package although additional benefits that include
outpatient TB DOTS, outpatient care for sponsored program (SP)
members, and maternity care are now provided.
PhilHealth contributions are compulsory for formally employed
individuals, but there are difficulties in enrolling the informal sector. Poor
households are progressively being enrolled and paid for through
earmarked taxes. PhilHealth premium levels continue to be regressive
since their low ceiling means that those in the upper salary brackets
contribute proportionately less compared to those with lower income. The
limited population and service coverage means that the high out-of-pocket
payments is a major barrier to accessing health services. In general, the
health financing system does not provide a safety net from the financial
consequences of illness. People who get sick can easily slide into poverty
since PhilHealth cannot provide full insurance coverage. During 2011,
PHP34,885 million (approx USD840 million) was paid out by PhilHealth
in benefits on 3,941,412 claims – an average of 1 claim for each 23 people
and PHP8,197 (approx USD195) per claim. However, it is likely that a
smaller number of people have multiple claims. PhilHealth data does not
seem to be available by income quintile for monitoring equity.
You might also like
- The Problem and A Review of Related LiteratureNo ratings yetThe Problem and A Review of Related Literature44 pages
- Nutritional Status of Grade Pupils of San Roque Elementary School San Jacinto, PangasinanNo ratings yetNutritional Status of Grade Pupils of San Roque Elementary School San Jacinto, Pangasinan39 pages
- Observance of Personal Hygine Among Junior High School Students100% (1)Observance of Personal Hygine Among Junior High School Students59 pages
- Oral Health Among Junior High School Student in Saints John and Paul Educational FoundationNo ratings yetOral Health Among Junior High School Student in Saints John and Paul Educational Foundation15 pages
- Personal Hygiene Components in Iranian Children and Adolescent MagazinesNo ratings yetPersonal Hygiene Components in Iranian Children and Adolescent Magazines7 pages
- Health and Sanitation Practices Among Secondary Schools in Division of Batangas.67% (3)Health and Sanitation Practices Among Secondary Schools in Division of Batangas.61 pages
- Journal Pre-Proofs: International Journal of Africa Nursing SciencesNo ratings yetJournal Pre-Proofs: International Journal of Africa Nursing Sciences51 pages
- Household Structure, Maternal Characteristics and Children's Stunting in Sub-Saharan Africa: Evidence From 35 CountriesNo ratings yetHousehold Structure, Maternal Characteristics and Children's Stunting in Sub-Saharan Africa: Evidence From 35 Countries9 pages
- Effect of Health Teaching On Knowledge and Practice of Postnatal Mother Admitted in Selected Hospital Regarding Using Diaper in Children To Prevent Systemic Bacterial InfectionNo ratings yetEffect of Health Teaching On Knowledge and Practice of Postnatal Mother Admitted in Selected Hospital Regarding Using Diaper in Children To Prevent Systemic Bacterial Infection7 pages
- Menstrual Hygiene Among Adolescent School Students: An In-Depth Cross-Sectional StudyNo ratings yetMenstrual Hygiene Among Adolescent School Students: An In-Depth Cross-Sectional Study5 pages
- Research Article: An Assessment of The Breastfeeding Practices and Infant Feeding Pattern Among Mothers in MauritiusNo ratings yetResearch Article: An Assessment of The Breastfeeding Practices and Infant Feeding Pattern Among Mothers in Mauritius9 pages
- The Role of Each Component of Coordinated School Health ProgramsNo ratings yetThe Role of Each Component of Coordinated School Health Programs2 pages
- Literature Review Penatalaksanaan Kasus Stunting Pada BalitaNo ratings yetLiterature Review Penatalaksanaan Kasus Stunting Pada Balita11 pages
- Determinants of Stunting in Children Aged 12-59 MonthsNo ratings yetDeterminants of Stunting in Children Aged 12-59 Months10 pages
- Dietary Diversity Practice and Associated Factors Among Infants and Young Children in Haramaya Town, EthiopiaNo ratings yetDietary Diversity Practice and Associated Factors Among Infants and Young Children in Haramaya Town, Ethiopia8 pages
- Persepsi Anak Usia Sekolah Terhadap Kesehatan Diri Dan Upaya Phbs Di Kabupaten BoyolaliNo ratings yetPersepsi Anak Usia Sekolah Terhadap Kesehatan Diri Dan Upaya Phbs Di Kabupaten Boyolali11 pages
- Correlation Between Dietary Habits Physical Activity and Nutritional Status of Adolescents Schooling in YaoundNo ratings yetCorrelation Between Dietary Habits Physical Activity and Nutritional Status of Adolescents Schooling in Yaound6 pages
- Bibliometric Mapping of Research Developments On The Topic of Efforts To Accelerate Stunting Reduction On Proquest Using VosviewerNo ratings yetBibliometric Mapping of Research Developments On The Topic of Efforts To Accelerate Stunting Reduction On Proquest Using Vosviewer17 pages
- Impact of Malnutrition on Students Academic Performance: A Study about MalnutritionNo ratings yetImpact of Malnutrition on Students Academic Performance: A Study about Malnutrition12 pages
- Obesity Prevention for Children: Before It's Too Late: A Program for Toddlers & PreschoolersFrom EverandObesity Prevention for Children: Before It's Too Late: A Program for Toddlers & PreschoolersNo ratings yet
- Case Chronic Renal Failure Discharge PlanningNo ratings yetCase Chronic Renal Failure Discharge Planning2 pages
- 2016 Annual Report - HSC Diagnostic Imaging - FULL REPORTNo ratings yet2016 Annual Report - HSC Diagnostic Imaging - FULL REPORT65 pages
- Predicting Covid-19 Using External Symptoms With Fuzzy Logic.No ratings yetPredicting Covid-19 Using External Symptoms With Fuzzy Logic.23 pages
- 6431804203 - Measurements in EpidemiologyNo ratings yet6431804203 - Measurements in Epidemiology8 pages
- Sample Exam On Community Health Nursing (Communicable Diseases)No ratings yetSample Exam On Community Health Nursing (Communicable Diseases)3 pages
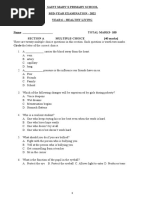
- Healthy Living-Mid-Year Examination - 2022No ratings yetHealthy Living-Mid-Year Examination - 20226 pages
- Nutritional Status of Grade Pupils of San Roque Elementary School San Jacinto, PangasinanNutritional Status of Grade Pupils of San Roque Elementary School San Jacinto, Pangasinan
- Observance of Personal Hygine Among Junior High School StudentsObservance of Personal Hygine Among Junior High School Students
- Oral Health Among Junior High School Student in Saints John and Paul Educational FoundationOral Health Among Junior High School Student in Saints John and Paul Educational Foundation
- Personal Hygiene Components in Iranian Children and Adolescent MagazinesPersonal Hygiene Components in Iranian Children and Adolescent Magazines
- Health and Sanitation Practices Among Secondary Schools in Division of Batangas.Health and Sanitation Practices Among Secondary Schools in Division of Batangas.
- Journal Pre-Proofs: International Journal of Africa Nursing SciencesJournal Pre-Proofs: International Journal of Africa Nursing Sciences
- Household Structure, Maternal Characteristics and Children's Stunting in Sub-Saharan Africa: Evidence From 35 CountriesHousehold Structure, Maternal Characteristics and Children's Stunting in Sub-Saharan Africa: Evidence From 35 Countries
- Effect of Health Teaching On Knowledge and Practice of Postnatal Mother Admitted in Selected Hospital Regarding Using Diaper in Children To Prevent Systemic Bacterial InfectionEffect of Health Teaching On Knowledge and Practice of Postnatal Mother Admitted in Selected Hospital Regarding Using Diaper in Children To Prevent Systemic Bacterial Infection
- Menstrual Hygiene Among Adolescent School Students: An In-Depth Cross-Sectional StudyMenstrual Hygiene Among Adolescent School Students: An In-Depth Cross-Sectional Study
- Research Article: An Assessment of The Breastfeeding Practices and Infant Feeding Pattern Among Mothers in MauritiusResearch Article: An Assessment of The Breastfeeding Practices and Infant Feeding Pattern Among Mothers in Mauritius
- The Role of Each Component of Coordinated School Health ProgramsThe Role of Each Component of Coordinated School Health Programs
- Literature Review Penatalaksanaan Kasus Stunting Pada BalitaLiterature Review Penatalaksanaan Kasus Stunting Pada Balita
- Determinants of Stunting in Children Aged 12-59 MonthsDeterminants of Stunting in Children Aged 12-59 Months
- Dietary Diversity Practice and Associated Factors Among Infants and Young Children in Haramaya Town, EthiopiaDietary Diversity Practice and Associated Factors Among Infants and Young Children in Haramaya Town, Ethiopia
- Persepsi Anak Usia Sekolah Terhadap Kesehatan Diri Dan Upaya Phbs Di Kabupaten BoyolaliPersepsi Anak Usia Sekolah Terhadap Kesehatan Diri Dan Upaya Phbs Di Kabupaten Boyolali
- Correlation Between Dietary Habits Physical Activity and Nutritional Status of Adolescents Schooling in YaoundCorrelation Between Dietary Habits Physical Activity and Nutritional Status of Adolescents Schooling in Yaound
- Bibliometric Mapping of Research Developments On The Topic of Efforts To Accelerate Stunting Reduction On Proquest Using VosviewerBibliometric Mapping of Research Developments On The Topic of Efforts To Accelerate Stunting Reduction On Proquest Using Vosviewer
- Impact of Malnutrition on Students Academic Performance: A Study about MalnutritionImpact of Malnutrition on Students Academic Performance: A Study about Malnutrition
- Obesity Prevention for Children: Before It's Too Late: A Program for Toddlers & PreschoolersFrom EverandObesity Prevention for Children: Before It's Too Late: A Program for Toddlers & Preschoolers
- 2016 Annual Report - HSC Diagnostic Imaging - FULL REPORT2016 Annual Report - HSC Diagnostic Imaging - FULL REPORT
- Predicting Covid-19 Using External Symptoms With Fuzzy Logic.Predicting Covid-19 Using External Symptoms With Fuzzy Logic.
- Sample Exam On Community Health Nursing (Communicable Diseases)Sample Exam On Community Health Nursing (Communicable Diseases)