CHAPTER-2 Sample
CHAPTER-2 Sample
Uploaded by
jeanne guarinoCopyright:
Available Formats
CHAPTER-2 Sample
CHAPTER-2 Sample
Uploaded by
jeanne guarinoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
CHAPTER-2 Sample
CHAPTER-2 Sample
Uploaded by
jeanne guarinoCopyright:
Available Formats
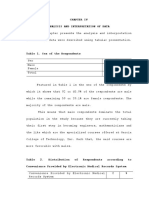
CHAPTER II
REVIEW OF RELATED LITERATURE
Chapter 2 presents the review of related literature and
studies which have the bearing on the study under
investigation. These will serve as guide and practice to
provide direction to the conduct of the study.
The Use of Electronic Medical Records: Communication
Patterns in Outpatient Encounters
By: Gregory Makoul, PhD, Raymond H. Curry, MD, & Paul C.
Tang, MD (2001).
To assess physician–patient communication patterns
associated with use of an electronic medical record (EMR)
system in an outpatient setting and provide an empirical
foundation for larger studies. Advances in electronic
medical record (EMR) technology have made it possible for
the EMR to replace many functions of the traditional paper
chart, and use of EMR systems promises significant advances
in patient care. While the promise is compelling, it is also
important to consider unanticipated effects that may be
associated with EMR use. For instance, any additional point
of focus for the doctor or patient— even a paper chart—can
be distracting. It is also possible that patients find
medical encounters involving a computer less personal or
16
fear that their confidentiality could more easily be
broached when the record is entered in a computer database.
Similarly, physicians may worry about the need to attend to
the computer rather than the patient or may find the
challenge of adapting to the new technology daunting.
Despite these concerns, empirical studies that have focused
mainly on perceptions of the medical encounter have shown
little or no adverse effect on either patient or physician
satisfaction. In fact, some patients report that having
their physicians use an EMR enhanced satisfaction with the
clinical encounter.
This study presents a focused report about
communication patterns associated with using either an
electronic or paper-based medical record in a sample of
outpatient encounters. Although some of the communication
behaviors of the EMR physicians may be a function of EMR
use, others probably reflect styles established before they
began using the EMR. It would be worth studying whether
coupling education on patient-centered communication with
EMR training would enhance the effective use of this tool.
Further communication research that extends our findings and
educational research that identifies productive training
methods will be needed to understand how to optimize the
17
potential benefit of EMR systems for both patients and
providers.
(https://link.springer.com/article/10.1186/s12911-017-0412-
x.)
The Evolution of Electronic Medical Records
By: Edward H. Shortliffe, MD, PhD (1999)
No clinical computing topic is being given more
attention than that of electronic medical records. Health-
care organizations, finding that they do not have adequate
systems for answering questions crucial to strategic
planning and for remaining competitive with other provider
groups, are looking to information technologies for help.
Many institutions are developing integrated clinical
workstations, which provide a single point of entry for
access to patient-related, administrative, and research
information.
The use of electronic medical records offers many
advantages for carrying out clinical research. Most
obviously, it helps to eliminate the manual tasks of
extracting data from charts or filling out specialized
datasheets. The data needed for a study can be derived
directly from the electronic record, making research-data
18
collection a byproduct of routine clinical record keeping.
But other advantages accrue as well. On the other hand,
there are at least four major issues that have consistently
constrained our efforts to build effective medical record
systems: (1) the need for standardized clinical terminology;
(2) concerns about data privacy, confidentiality, and
security; (3) challenges of data entry by physicians; and
(4) difficulties associated with the integration of record
systems with other information resources in the health care
setting.
The difficulty in automating medical records is best
appreciated if one analyzes the processes associated with
the creation and use of such records, rather than thinking
of the record as an object that can be moved around as
needed within an institution. For example, on the data input
side, the medical record requires the integration of
processes for data capture and for merging information from
diverse sources. In order to be useful, the record also must
provide facile mechanisms for displaying needed data, for
analyzing them, and for sharing them among different kinds
of individuals (including secondary users of the record who
are not involved in direct patient care). Thus the computer
based medical record is best viewed not as an object or a
product, but rather as a set of processes that an
19
organization must put into place, supported by technology.
Implementing electronic records is inherently a process
automation and systems integration task, and thus systems
that function well in one environment often do not transfer
well to others in which institutional processes and
traditions may have evolved in different ways.
Physicians are "horizontal" users of information
technology. That is, rather than becoming "power users" of a
narrowly defined software package, they access a wide
variety of systems and resources. Thus routine use of
computers, and of electronic medical records, will be most
easily achieved if the computing environment offers
physicians a critical mass of services that are both
smoothly integrated and useful for essentially every patient
encounter.
(https://pdfs.semanticscholar.org/d46d/1c4f5871d3c915d220c7e
0350c2c7054583b.pdf.)
Extending Feature Usage: A Study of the Post-Adoption of
Electronic Medical Records
By: Norman Shaw & Sharm Manwani (2011).
The success of their EMR adoption and subsequent use is
the responsibility of OntarioMD, which is jointly owned by
the Ontario Medical Association (OMA) and the Ministry of
Health and Long-Term Care (OntarioMD, 2009). Through
20
OntarioMD we sent out 1,800 e-mails with a request to
participate in a 30-minute interview. In order to guard the
privacy of the physicians, all e-mails were initially sent
by OntarioMD.
Several categories of benefits emerged from the
thematic analysis.
More Organized Information. Over 60 % of the
participants mentioned that they were able to provide
improved healthcare because the information about the
patient was more organized than the paper chart. Data is up
to date and diagnostic decisions are made more quickly based
on more complete information.
More Comprehensive Encounters. Over 35% of the
physicians stated that patient care was improved because the
EMR was able to function as a memory prompt for them. Some
physicians use templates in order to guide them through an
examination so that no important question or data is
forgotten. In addition, tests are scheduled on time due to
the prompts by reminders.
Patient Medications. Over 30% of the physicians stated
that the EMR’s capability to track all the medications that
the patient has taken increases the efficiency of
prescribing. It does take time at the implementation stage
to input the list of medications, but once entered, any
21
renewal is one keystroke. The EMR also records the history
of patients’ adverse reactions to drugs guiding the
physician at the time of prescribing.
Patient Education. Over 30% of the physicians actively
share results as part of their program of patient education.
Charts can be reviewed with the patient comparing their
results to the ideal as noted in health guidelines. Patients
are shown flowcharts which can be printed for the patient to
take home and reference.
Legibility. Over 20% of the physicians commented on
legibility, stating that legible notes resulted in improved
patient care. Notes in the EMR are typed and legible. The
governing body of medicine also conducts peer reviews in
order to ensure that standards are maintained and improved.
Both the reviewer and the reviewed physician can easily read
the notes.
Managing Routine Tests. Reminders are an effective way
to ensure that routine tests are not missed. Physicians
believed that preventive care was improved when they were
prompted by a reminder during the patient encounter.
Reduction of prescription errors. Patient safety is
enhanced because prescriptions are legible for pharmacists
and drug doses are checked by the computer.
22
More Efficient use of Clinical Resources. Patients can
be micromanaged and resources used more effectively. On an
individual basis, physicians can ask themselves ‘do I need
to see this patient?’ when responding to a phone call. Other
healthcare professions attached to the clinic, such as
dieticians, may be the right resource for follow-up.
Communication within the clinic is enhanced allowing for
more efficient use of all clinical resources with the
electronic record easily shared simultaneously by multiple
care providers.
Pro-active Patient Management. The search feature
within the EMR allows physicians to proactively manage their
patient population. They can find patients with a specific
condition and
schedule the desired next steps. For drug recalls, although
not frequent, the patient population can be searched and
patients contacted, which is just not possible with paper
records.
Summary. PU was a dominant factor. Physicians only
adopted those features that they perceived to be useful as
part of their everyday routine.
(https://aisel.aisnet.org/cgi/viewcontent.cgi?
article=124&context=ecis2011.)
International Symposium on Affective Science and Engineering
23
By: Chau VO, Tru CAO, Nam DOAN, Son TU, Anh NGUYEN, Binh
NGUYEN, & Bao HO (2018)
Patient progress tracking is important to a doctor in a
treatment process. In order to have enough information about
a patient and the treatment made for the patient, a doctor
has to view a lot of medical data about symptoms, test
results, drugs and their dosages in a period of time. With
electronic medical records, it is convenient for the doctor
to view and search for any information he/she needs as
compared to paper medical records. It would be even better
if all the related electronic medical records over time of
each patient are visualized appropriately to support the
doctor in patient progress tracking. Therefore, our EMR
Visualization system is proposed as a web-based application
on tablet computers for visualizing all the related medical
data in an integrative manner. The system provides an
interactive visualization with accurate data at different
detail levels, quick access and convenience for a doctor to
keep track of the progress of each patient over time. Its
demonstration with the real data of gastroenterological
Vietnamese patients in Thong Nhat Hospital, Ho Chi Minh
City, Vietnam, has been conducted and showed that every
24
interaction of a doctor can be accomplished in at most two
steps.
(https://www.jstage.jst.go.jp/article/isase/ISASE2018/0/ISAS
E2018_1_14/_article/-char/ja/.)
An Electronic Medical Record System
By: Muhammad Sarfraz, Anwar A. Al-Hussainan, Farah Mohammad
& Hanouf Al-Azmi (2020)
To become more productive, faster, smart and accurate,
almost every major organization or industry has invested for
computerizing their day to day mechanisms. It has helped
easing and smoothing everyday life. Banking, shopping,
airline booking and ticketing are just few to name.
Otherwise, virtually all businesses are going online. Yet,
despite all these advancements in our society, there are a
large number of patients who are being dealt in a
traditional way. For example, they are given handwritten lab
tests, medication prescriptions, appointments and others.
Having electronic medical record (EMR) systems is a need of
the time. It will enormously help to transform the health
care system from a traditional paper-based mechanism to
automated online systems. It will help utilizing clinical
information in delivering higher quality in terms of
25
accuracy, time, efficiency and care to the patients as well
as medical care staff. Having EMR systems has a high
probability to reduce the possibilities for errors which are
very evident in typical manual operations. It promotes human
friendly environment which improves communication of
information in the medical related activities.
(https://www.igiglobal.com/article/an-electronic-medical
record- system/245721.)
Barriers to the acceptance of electronic medical records by
physicians from systematic review to taxonomy and
interventions.
By: Albert Boonstra & Manda Broekhuis (2010)
Electronic Medical Records (EMRs) are computerized
medical information systems that collect, store and display
patient information. They are a means to create legible and
organized recordings and to access clinical information
about individual patients. Further, EMRs are intended to
replace existing (often paper based) medical records which
are already familiar to practitioners. Patient records have
been stored in paper form for centuries and, over this
period of time, they have consumed increasing space and
notably delayed access to efficient medical care. In
contrast, EMRs store individual patient clinical information
26
electronically and enable instant availability of this
information to all providers in the healthcare chain and so
should assist in providing coherent and consistent care.
(https://bmchealthservres.biomedcentral.com/articles/10.1186
/1472-6963- 10-231.)
Use of electronic medical records and quality of patient
data: different reaction patterns of doctors and nurses to
the hospital organization
M.S. Lambooij and H.W. Drewes (2017)
As the implementation of Electronic Medical Records
(EMRs) in hospitals may be challenged by different responses
of different user groups, this paper examines the
differences between doctors and nurses in their response to
the implementation and use of EMRs in their hospital and how
this affects the perceived quality of the data in EMRs.
Doctors and nurses differ in their response to the
organizational factors (support of IT, HR and administrative
departments) considering the success of the implementation.
Nurses respond to culture while doctors do not. Doctors and
nurses agree that an EMR that is easier to work with and
better aligned with their work has more added value, but for
the doctors this is more pronounced. The doctors and nurses
perceive that the quality of the patient data is better when
27
EMRs are easier to use and better aligned with their daily
routine.
(https://link.springer.com/article/10.1186/s12911-017-0412-
x.)
Patient satisfaction with the implementation of electronic
medical Records in the Western Region, Saudi Arabia.
By: R. M. Wali, R. M. Alqahtani, S. K. Alharazi, S. A.
Bukhari & S. M. Quqandi (2018)
Findings from this study demonstrated an overall
improvement in patient satisfaction due to the
implementation of EMR Compared to PMR. Similar findings have
been reported the participants experienced that the
physicians were more attentive during the medical
consultation, a finding also reported in the literature.
According to the participants, the physician explained the
reason for tests and management options and that there was
more time available to discuss various health topics.
Support for the statement is provided by a study conducted
in the USA, emphasizing that the physician and patient had
more time to discuss self-care topics and to explain health
issues and medication use. In addition, active listening by
the physician improved after implementing the EMR, and the
participants felt it was convenient to ask questions about
28
their health status and concerns this can be due to less
time spent in writing and trying to fill the documents. A
qualitative study where physicians were observed during the
clinical consultation, indicated that the physicians were
abler to take an active role, such as encouraging questions
and explaining health topics, but less effective in terms of
exploring a patient-centered agenda, for example, the effect
of the health problem on the patient’s life, ideas and
concerns compared to PMR. A similar study conducted in
Kuwait to measure the level of satisfaction of PHC attendees
reported overall satisfaction with the services except for
two aspects, including explaining the medical procedure and
being able to choose the physician they prefer.
(https://bmcfampract.biomedcentral.com/articles/10.1186/s128
75-020-1099-0)
Electronic Medical Records in Family Practice: The Time Is
Now
By: Steven M. Omstein, M D & Charleston, & South Carolina
(1997)
The advantages of electronic medical records compared
with traditional paper records have been described
previously in this Journal and are well recognized by the
prestigious National Academy of Science Institute of
29
Medicine. In a 1991 report, the Institute of Medicine called
for a national effort to develop a comprehensive computer-
based patient record system. Such a system would be a
distributed, longitudinal, information database with
features such as access to patient information across an
individual’s life span, comprehensive decision-making
support, flexible reporting, a defined vocabulary and coding
system, and transparent connectivity with other systems. At
present, work is ongoing in many academic settings,
government agencies, industrial settings, and coordinating
groups such as the Computer-Based Patient Record Institute
(Schaumburg, 111) to realize this vision, which remains
years away.
Of more practical interest to the practicing family
physician are four recent developments. First, there is
increasing empirical evidence of the clinical value of EMR
systems. Second, despite an occasional contrary report, many
case studies describe the successful application of EMR
systems. The reports are from a broad spectrum of practice
settings, including small private practice, an academic
family medicine center, and a health maintenance
organization. Third, several reports document the favorable
response that patients have to electronic records.
30
Physicians need not fear that the doctor-patient
relationship will be adversely affected by EMR systems.
Finally, tire marketplace and our professional organization,
the American Academy of Family Physicians (AAFP), have
responded to the need for EMR systems. At the October 1996
AAFP national assembly in New Orleans, more than a dozen
vendors had exhibits showing their EMR systems, and a
computer “petting zoo” gave physicians hands-on experience
with several of these systems. In addition, 3 days of
computer lectures and demonstrations were offered, both in
small group hands-on and larger group formats. Prices for
computer hardware continue to plummet, and more software
vendors enter the EMR market monthly.
Despite these developments, it is widely accepted that
only 2% to 3% of office-based physicians and approximately
5% of family medicine residency programs use EMR systems.
Family physicians, practice managers, and group
administrators need additional exposure to these systems.
Several options are available for this purpose. First,
national and some statewide AAFP meetings have both
presentations and vendor displays of EMR systems. Second,
journals such as the AAFP’s Family Practice Management have
already published and plan to update reviews of available
31
systems. Third, electronic resources are available. A
discussion group provides a lively discussion about EMR
systems and other computer applications in a practice
setting. Finally, some organizations that have successfully
implemented EMR systems provide opportunities for others to
learn from their experiences. Our department of family
medicine offers a monthly symposium, “The Computer-Based
Patient Record as a Continuous Quality Improvement Tool,”
for this purpose.
(https://mdedge-files-live.s3.us-east
2.amazonaws.com/files/s3fs-public/jfp-archived-issues/1997-
volume_44-45/JFP_199701_v44_i1_electronic- medical-records-
in-family-pra.pdf.)
The Implementation of the Electronic Medical Records System
in Health Care Facilities
By: Corey Bain (2015)
Electronic medical records (EMR) are seen as a way to
simplify the management of patient information, increase
productivity and lower costs associated with medical
information management. The implementation of the EMR system
in healthcare facilities has not only provided potential
benefits to improved quality of care, but there are
significant factors to consider associated with human
factors, ergonomics, workflows and environmental conditions.
32
These factors should be considered to improve the quality
and cost of patient care, as well as employee and patient
safety. An ever changing healthcare system includes the
transformation of medical records management to electronic
medical records(EMR). EMR are seen as a way to simplify the
management of patient information, increase productivity and
lower costs associated with medical information management.
The integration of information management to healthcare
providers has enhanced the information that is made
available to physicians. It has also provided a competitive
advantage for organizations. The implementation of the EMR
system in healthcare facilities has not only provided
potential benefits to improved quality of care, but there
are significant factors to consider associated with human
factors, ergonomics, workflows and environmental conditions.
These factors should be considered to improve the quality
and cost of patient care, as well as employee and patient
safety.
(fromhttps://www.sciencedirect.com/science/article/pii/S2351
97891500548X.)
You might also like
- Health Care Management System Project Report FullDocument79 pagesHealth Care Management System Project Report Fullhgjykhf83% (12)
- GED Maths Ready TestDocument6 pagesGED Maths Ready Testtds67057No ratings yet
- Supply Chain Management For Dummies - A Quick RefresherDocument2 pagesSupply Chain Management For Dummies - A Quick Refresherrenzoc.helixNo ratings yet
- Workshop, Repair and Service Manuals, Wiring Diagrams, Fault Codes PDF - More Than 1000+ Truck Manuals Are Available For Free Download!Document12 pagesWorkshop, Repair and Service Manuals, Wiring Diagrams, Fault Codes PDF - More Than 1000+ Truck Manuals Are Available For Free Download!Anbarasan67% (3)
- Parts List As Per Electric Service TruckDocument3 pagesParts List As Per Electric Service TruckJean Jacques ouandaNo ratings yet
- Sia RRLDocument16 pagesSia RRLPacetes Clarissa D.No ratings yet
- Nursing Informatics 1 - ScribdDocument3 pagesNursing Informatics 1 - ScribdBianca BalmoresNo ratings yet
- Patient Record TrackingDocument85 pagesPatient Record TrackingMajestyNo ratings yet
- Nursing InformaticsDocument8 pagesNursing InformaticsWac GunarathnaNo ratings yet
- Electronic Medical RecordDocument4 pagesElectronic Medical Recordemmy_lineNo ratings yet
- Perceptions of Nurses Towards The Adoption of A Computerized Documentation SystemDocument12 pagesPerceptions of Nurses Towards The Adoption of A Computerized Documentation SystemTrixia RiveraNo ratings yet
- 1) Identify The Following Impacts of Information Technology in The Society. Give ExamplesDocument14 pages1) Identify The Following Impacts of Information Technology in The Society. Give ExamplesAbeir A. C. SampornaNo ratings yet
- Improving Patient Safety and Hospital Service Quality Through Electronic Medical Record: A Systematic ReviewDocument10 pagesImproving Patient Safety and Hospital Service Quality Through Electronic Medical Record: A Systematic ReviewNurul RakhmawatiNo ratings yet
- Computerized Medical Lab Record SystemDocument41 pagesComputerized Medical Lab Record SystemUmar Ridwan saniNo ratings yet
- Research Paper Nursing InformaticsDocument8 pagesResearch Paper Nursing Informaticsgz8bjzmj100% (1)
- Improving Patient Safety and Hospital Service Quality Through Electronic Medical Record: A Systematic ReviewDocument10 pagesImproving Patient Safety and Hospital Service Quality Through Electronic Medical Record: A Systematic ReviewRAHMA JUMILANo ratings yet
- Electronic Medical RecordsDocument4 pagesElectronic Medical Recordsdew23No ratings yet
- An Overview of Electronic Medical Record Implementation in Healthcare System: Lesson To LearnDocument11 pagesAn Overview of Electronic Medical Record Implementation in Healthcare System: Lesson To Learnmayang sariNo ratings yet
- RamanujuluDocument37 pagesRamanujuluinfoway salmanNo ratings yet
- Design and Development of Online Hospital Management Information SystemDocument10 pagesDesign and Development of Online Hospital Management Information SystemRula ShakrahNo ratings yet
- Extinction: Future Model For Nursing DocumentationDocument4 pagesExtinction: Future Model For Nursing DocumentationDwi NopriyantoNo ratings yet
- WSN 180 (2023) 82-93Document12 pagesWSN 180 (2023) 82-93john carl cuerpoNo ratings yet
- Newsletter and RP STARTDocument4 pagesNewsletter and RP STARTBálint ÁrpádNo ratings yet
- Running Head: Cost-Benefit Analysis of Electronic Health RecordsDocument11 pagesRunning Head: Cost-Benefit Analysis of Electronic Health RecordsBilal Ahmad BhatNo ratings yet
- Group 4 Nursing InformaticsDocument5 pagesGroup 4 Nursing InformaticsMj GalanoNo ratings yet
- Electronic Medical RecordDocument10 pagesElectronic Medical RecordPrem Deep100% (1)
- 27 - 2014 - R.V Weeks - The Implementation of An Electronic Patient Healthcare Record System A South African Case StudyDocument19 pages27 - 2014 - R.V Weeks - The Implementation of An Electronic Patient Healthcare Record System A South African Case Studyleanemmauspolinar222No ratings yet
- Exploring Challenges and Potentials of Personal Health Records in Diabetes Self-Management: Implementation and Initial AssessmentDocument10 pagesExploring Challenges and Potentials of Personal Health Records in Diabetes Self-Management: Implementation and Initial AssessmentNita Purnama SariNo ratings yet
- Advantages and Disadvantages of EMR SystemsDocument6 pagesAdvantages and Disadvantages of EMR SystemsPatel NazzNo ratings yet
- DNPManuscript KellyDocument32 pagesDNPManuscript Kellyvralph815No ratings yet
- Paper+8+ (2021 3 2) +Electronic+Document+Management+System+ (EDMS) +Implementation+Implications+for+the+Future+of+Digital+TransformDocument9 pagesPaper+8+ (2021 3 2) +Electronic+Document+Management+System+ (EDMS) +Implementation+Implications+for+the+Future+of+Digital+Transformluilail1221No ratings yet
- The Effects of Information Technology On Perioperative NursingDocument16 pagesThe Effects of Information Technology On Perioperative NursingBagus Adi PratamaNo ratings yet
- Patient Record Management Information Sy2222Document7 pagesPatient Record Management Information Sy2222Innovator AdrianNo ratings yet
- Role of Information Technology in MedicineDocument7 pagesRole of Information Technology in MedicineFahadghaznavi100% (1)
- CCN Final SubmissionDocument8 pagesCCN Final SubmissionnishuNo ratings yet
- L3 Overview of Health InformaticsDocument3 pagesL3 Overview of Health InformaticsVera June RañesesNo ratings yet
- Hta 11 02 PDFDocument9 pagesHta 11 02 PDFgasiasiNo ratings yet
- Health Systems and Technology: Course Number: CIS 1200 Dowling CollegeDocument11 pagesHealth Systems and Technology: Course Number: CIS 1200 Dowling CollegecleodeesNo ratings yet
- Electronic Health Record Implementation StrategiesDocument10 pagesElectronic Health Record Implementation StrategiesATS100% (1)
- Issues in InformaticsDocument23 pagesIssues in InformaticsRaab ReyesNo ratings yet
- The Strategic Role of Electronic Medical Records "Emr" in Supporting Electronic Health System in Saudi HospitalsDocument11 pagesThe Strategic Role of Electronic Medical Records "Emr" in Supporting Electronic Health System in Saudi HospitalsBaru Chandrasekhar RaoNo ratings yet
- Running Head: PROJECT ASSIGNMENT 4 1Document13 pagesRunning Head: PROJECT ASSIGNMENT 4 1Farasha SSNo ratings yet
- RevisionPaper (Capstone)Document36 pagesRevisionPaper (Capstone)issei dragneelNo ratings yet
- Longitudinal Electronic Patient RecordDocument13 pagesLongitudinal Electronic Patient RecordJULIUSNo ratings yet
- Full Content 1Document29 pagesFull Content 1MuhdNoorFirdausNo ratings yet
- Chapter-1-And-2 EDITDocument21 pagesChapter-1-And-2 EDITmonzonesbrenncarloNo ratings yet
- CernerDocument10 pagesCernerazul2233No ratings yet
- Project SeminarDocument11 pagesProject SeminaribrahimNo ratings yet
- Computers and NursingDocument5 pagesComputers and NursingZharah Ruz100% (1)
- June 2000/vol. 43, No. 6 COMMUNICATIONS OF THE ACMDocument8 pagesJune 2000/vol. 43, No. 6 COMMUNICATIONS OF THE ACMDavis PunjilaNo ratings yet
- Moroccan Electronic Health Record System: Houssam BENBRAHIM, Hanaâ HACHIMI and Aouatif AMINEDocument8 pagesMoroccan Electronic Health Record System: Houssam BENBRAHIM, Hanaâ HACHIMI and Aouatif AMINESouhaïla MOUMOUNo ratings yet
- Electronic Medical Record/Electronic Health Record System: Problem Based LearningDocument13 pagesElectronic Medical Record/Electronic Health Record System: Problem Based LearningTonmoy Banerjee100% (1)
- BIS Case Study 4 - Chapter 13Document4 pagesBIS Case Study 4 - Chapter 13Hussam RajabNo ratings yet
- EMRs and The Last Mile of Clinical CommunicationsDocument7 pagesEMRs and The Last Mile of Clinical CommunicationsPeter DucklerNo ratings yet
- Integrated Electronic Medical Record Systems: Critical Success Factors For ImplementationDocument10 pagesIntegrated Electronic Medical Record Systems: Critical Success Factors For ImplementationThi KimNo ratings yet
- Electronic Health Record Research PaperDocument5 pagesElectronic Health Record Research Paperef71d9gw100% (1)
- Electronic Medical Records Literature ReviewDocument7 pagesElectronic Medical Records Literature Reviewafmztsqbdnusia100% (1)
- gjmbsv3n3spl 14Document25 pagesgjmbsv3n3spl 14areeb khanNo ratings yet
- Medical Informatics Activity No.1Document3 pagesMedical Informatics Activity No.1leomillmendiolaNo ratings yet
- Patient Management System (New Reviewed)Document39 pagesPatient Management System (New Reviewed)Ajewole Eben Tope100% (1)
- 1C1-4 EPRSwDEaFPIDocument6 pages1C1-4 EPRSwDEaFPIAlunar HartNo ratings yet
- A. Overview of Electronic Health RecordDocument10 pagesA. Overview of Electronic Health RecordmaknyoseuyNo ratings yet
- Cognitive Informatics: Reengineering Clinical Workflow for Safer and More Efficient CareFrom EverandCognitive Informatics: Reengineering Clinical Workflow for Safer and More Efficient CareKai ZhengNo ratings yet
- Chapter 3Document6 pagesChapter 3jeanne guarinoNo ratings yet
- Review of Related LiteratureDocument6 pagesReview of Related Literaturejeanne guarinoNo ratings yet
- Celebrated Every Last Week of April. Some of The Activities Are Float Contest, Cultural Shows, Pageant & Other EntertainmentDocument6 pagesCelebrated Every Last Week of April. Some of The Activities Are Float Contest, Cultural Shows, Pageant & Other Entertainmentjeanne guarinoNo ratings yet
- Analysis and Interpretation of DataDocument15 pagesAnalysis and Interpretation of Datajeanne guarinoNo ratings yet
- CHAPTER-3 SampleDocument6 pagesCHAPTER-3 Samplejeanne guarinoNo ratings yet
- Viewpoints of Grade 12 Stem Students of Garcia College of Technology in The Application of Face Recognition Technology in Library Attendance MonitoryDocument1 pageViewpoints of Grade 12 Stem Students of Garcia College of Technology in The Application of Face Recognition Technology in Library Attendance Monitoryjeanne guarinoNo ratings yet
- Adhunik Group PresentationDocument47 pagesAdhunik Group PresentationEric RoyNo ratings yet
- The Indian Wireless Telegraphy Act, 1933Document4 pagesThe Indian Wireless Telegraphy Act, 1933Ruhika KhajuriaNo ratings yet
- Ais615 Tutorial Chapter 9 QDocument3 pagesAis615 Tutorial Chapter 9 Qlianatasia ramliNo ratings yet
- HEAT EXCHANGERS MDocument143 pagesHEAT EXCHANGERS MHeet Patel100% (1)
- Institute Name: Indian Institute of Technology Hyderabad (IR-O-U-0013)Document14 pagesInstitute Name: Indian Institute of Technology Hyderabad (IR-O-U-0013)Zain RashidNo ratings yet
- Session 3Document17 pagesSession 3Rubayat AdnanNo ratings yet
- Fosroc Nitobond PVA: Multipurpose PVA Adhesive, Sealer and Cement AdmixtureDocument4 pagesFosroc Nitobond PVA: Multipurpose PVA Adhesive, Sealer and Cement AdmixtureVincent JavateNo ratings yet
- John Bullseye ExerciseDocument4 pagesJohn Bullseye ExerciseErrata BNo ratings yet
- Connecticut Voter Readiness Fact Sheet 10.28.24Document4 pagesConnecticut Voter Readiness Fact Sheet 10.28.24Editor, Hartford CourantNo ratings yet
- Umpire Career Development 01 2021Document9 pagesUmpire Career Development 01 2021CelesteCondoriCastroNo ratings yet
- MARK XII SE - EnglishDocument13 pagesMARK XII SE - Englishkronik_insanNo ratings yet
- 9335X 70Document1 page9335X 70Nia SilviharyaniNo ratings yet
- Entrepreneur Innovation (Tan Sri A.K. Nathan)Document12 pagesEntrepreneur Innovation (Tan Sri A.K. Nathan)Thava Selvy100% (1)
- Core - Security.patterns - Best.practices - And.strategies - for.J2EE - Web.services - And.identity - Management.oct.2005 0131463071Document848 pagesCore - Security.patterns - Best.practices - And.strategies - for.J2EE - Web.services - And.identity - Management.oct.2005 0131463071blackstileNo ratings yet
- D187 PDFDocument4 pagesD187 PDFJuan Diego ArizabalNo ratings yet
- Zanussi ZWY 61004 WA Washing MachineDocument36 pagesZanussi ZWY 61004 WA Washing MachineahmedNo ratings yet
- Mont Baldy: Crag GuideDocument7 pagesMont Baldy: Crag GuideClaude PoulinNo ratings yet
- FACA Template For Input On The Certification Criteria To Support MU Stage 2 Objectives and MeasuresDocument52 pagesFACA Template For Input On The Certification Criteria To Support MU Stage 2 Objectives and MeasuresBrian AhierNo ratings yet
- Ping FederateDocument1,160 pagesPing FederateN Reddy KNo ratings yet
- Brian Lara International Cricket 2005 - Manual - PCDocument18 pagesBrian Lara International Cricket 2005 - Manual - PCdoomdiver1No ratings yet
- Geo7Series UserGuide PDFDocument133 pagesGeo7Series UserGuide PDFAji SatrioNo ratings yet
- AW 6 Speeds: Valve Body Diagnosis: From The SonnaxDocument7 pagesAW 6 Speeds: Valve Body Diagnosis: From The SonnaxtejonmxNo ratings yet
- DOC-062829 Rev 01 Add Clear UDI Cover Label Process Validation ProtocolDocument7 pagesDOC-062829 Rev 01 Add Clear UDI Cover Label Process Validation ProtocolLife with a RedheadNo ratings yet
- Annex e To Multi Part Advisory Circular 119 11 and 138 2Document8 pagesAnnex e To Multi Part Advisory Circular 119 11 and 138 2Beka KarumidzeNo ratings yet
- Pasoa Parents ConsentDocument1 pagePasoa Parents ConsentRUEL VINCENT ESPINASNo ratings yet