0 ratings0% found this document useful (0 votes)
95 viewsCaregiver Nursing Interventions
Caregiver Nursing Interventions
Uploaded by
Sona AntoThe document discusses nursing interventions for stroke caregivers dealing with stress, fear, hopelessness, and insufficient knowledge and skills. It provides tips for nurses to assess caregivers' abilities and needs, encourage social support, teach stress management techniques, check in on emotional well-being, connect caregivers to resources, and ensure caregivers have the knowledge and skills to care for stroke patients. The document emphasizes providing education, emotional support, and ensuring caregivers can successfully care for patients and manage their own health and wellness.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Caregiver Nursing Interventions
Caregiver Nursing Interventions
Uploaded by
Sona Anto0 ratings0% found this document useful (0 votes)
95 views5 pagesThe document discusses nursing interventions for stroke caregivers dealing with stress, fear, hopelessness, and insufficient knowledge and skills. It provides tips for nurses to assess caregivers' abilities and needs, encourage social support, teach stress management techniques, check in on emotional well-being, connect caregivers to resources, and ensure caregivers have the knowledge and skills to care for stroke patients. The document emphasizes providing education, emotional support, and ensuring caregivers can successfully care for patients and manage their own health and wellness.
Original Title
CAREGIVER NURSING INTERVENTIONS
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
The document discusses nursing interventions for stroke caregivers dealing with stress, fear, hopelessness, and insufficient knowledge and skills. It provides tips for nurses to assess caregivers' abilities and needs, encourage social support, teach stress management techniques, check in on emotional well-being, connect caregivers to resources, and ensure caregivers have the knowledge and skills to care for stroke patients. The document emphasizes providing education, emotional support, and ensuring caregivers can successfully care for patients and manage their own health and wellness.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
95 views5 pagesCaregiver Nursing Interventions
Caregiver Nursing Interventions
Uploaded by
Sona AntoThe document discusses nursing interventions for stroke caregivers dealing with stress, fear, hopelessness, and insufficient knowledge and skills. It provides tips for nurses to assess caregivers' abilities and needs, encourage social support, teach stress management techniques, check in on emotional well-being, connect caregivers to resources, and ensure caregivers have the knowledge and skills to care for stroke patients. The document emphasizes providing education, emotional support, and ensuring caregivers can successfully care for patients and manage their own health and wellness.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 5
NURSING INTERVENTIONS STROKE CAREGIVER
CARE GIVER STRESS &STRAIN
Ascertain the caregiver’s knowledge and ability to implement patient care, including
bathing, skin care, safety, nutrition, medications, and ambulation.
Encourage the involvement of other family members to relieve pressure on the
primary caregiver.
Tell the caregiver to set aside time for self. Aid the caregiver in identifying those that
bring them peace and relaxation. Caregivers need may need reminders to attend to
own physical and emotional needs. This helps conserve physical and emotional
energy.
Introduce stress-reducing methods to the caregiver. It is important that the caregiver
has the opportunity to relax and reenergize emotionally throughout the day to assume
care responsibilities.
Allow caregiver to participate in in support group. Groups that come together for
mutual support can be advantageous in providing education and anticipatory
guidance.
Allot time for the caregiver to discuss problems, concerns, and feelings. Ask the
caregiver how he or she is managing. Nurses are in an excellent position to give
emotional support and provide guidance throughout this challenging situation.
Encourage the caregiver to know available family and friends who can assist with
caregiving. Successful caregiving should not be the sole responsibility of one person.
Recommend the use of available community resources such as respite, home health
care, adult day care, geriatric care, housekeeping services, home health aides, Meals
On Wheels, companion services, and others, as appropriate. Resources grant
opportunity for multiple competent providers and services on a temporary basis or for
a more extended period.
Provide safe and effective alternatives to medication.
FEAR
Determine the type of the fear by thorough, rational questioning and active listening.
The external cause of fear can be known. Caregiver who find it unacceptable to
expose fear may find it convenient to know that someone is willing to listen if they
choose to share their feelings at some time in the future.
Assess the behavioral and verbal expression of fear. This information provides a
foundation for planning interventions to support the Caregiver’s coping strategies.
Evaluate the measures the Caregiver practices to cope with that fear. This information
helps determine the effectiveness of coping strategies used by the Caregiver.
Open up about your awareness of the Caregiver’s fear.
Discuss the situation with the Caregiver and help differentiate between real and
imagined threats to well-being.
Tell Caregiver that fear is a normal and appropriate response to circumstances in
which pain, danger, or loss of control is anticipated or felt. This reassurance places
fear within the field of normal human experiences.
Be with the Caregiver to promote safety especially during frightening procedures or
treatment. The physical connection with a trusted person helps the patient feel secure
and safe during a period of fear.
Maintain a relaxed and accepting demeanor while communicating with the Caregiver.
The Caregiver’s feeling of stability increases in a peaceful and non-threatening
environment.
Provide accurate information if irrational fears based on incorrect information are
present. Replacing inaccurate beliefs into accurate information reduces anxiety.
If Caregiver’s fear is a reasonable response, empathize with him or her. Avoid false
reassurances and be truthful. Reassure Caregiver s that asking for help is both a sign
of strength and a step toward resolution of the problem.
Use simple language and easy to understand statements regarding diagnostic
procedures. The Caregiver may find it hard to understand any given explanations
during excessive fear. Simple, clear, and brief instructions are necessary.
Maintain a quiet environment whether at home or in a hospital setting. Drop any
unnecessary stuff around the patient. Caregiver’s fear is not reduced and resolved if
the environment is unsafe.
Support the Caregiver in recognizing strategies used in the past to deal with fearful
situations. This method allows the Caregiver to think that fear is a natural part of life
and can be dealt with successfully
As the fear subsides, encourage the Caregiver to involve himself or herself to specific
events preceding the onset of the fear. Recognition and explanation of factors leading
to fear are vital in developing alternative responses.
Allow the Caregiver to have rest periods. Relaxation improves ability to cope. The
nurse needs to pace activities, especially to older adults to conserve the Caregiver s
energy.
Access community resources to meet the fearful needs of the Caregiver and family
(e.g., spiritual counselor, social worker). Appropriate resources render organized
and regulated Caregiver that indicates supportive healthcare service.
Initiate alternative treatments. Provide verbal and nonverbal (touch and hug with
permission) reassurances of safety if safety is within control. Meditation, prayer,
music, Therapeutic Touch, and healing touch techniques help lighten fear.
HOPELESSNESS
Assess physical appearances such as the grooming, posture, and hygiene. Caregiver s
who are experiencing hopelessness may not have the urge to participate in Patient-
care activities.
Ascertain the role that illness presents in the Caregiver’s hopelessness. Caregiver’s
current situation may affect his or her physical functioning.
Assess the Caregiver’s understanding of the situation, belief in self, and his or her
own abilities.
Encourage a positive mental perspective, discourage negative thoughts, and brace
patient for negative results.
Provide openings for the Caregiver to verbalize feelings of hopelessness.
Manage to have consistency in staff appointed to care for the patient.
Assist Caregiver with looking at options and establishing goals that are relevant to
him or her.
Encourage the Caregiver to recognize his or her own strengths and abilities.
Work with the Caregiver to set small, attainable goals.
Render physical care that the Caregiver is unable to achieve and respect Caregiver’s
abilities.
Stay and spend time with the Caregiver. Use empathy; try to understand what the
Caregiver is saying, and communicate this understanding to the Caregiver.These
approaches can inspire hope. Experiencing warmth, empathy, genuineness, and
unconditional positive regard can greatly reduce feelings of hopelessness.
Assist the Caregiver in establishing realistic goals by recognizing short-term goals
and revising them as needed.
Provide time for Caregiver to initiate interactions.
Strengthen Caregiver’s relationship with significant others; allow them to take part in
Caregiver’s care.
Encourage family and significant others to display care, hope, and love for Caregiver.
Encouraging the family to present Caregiver support, to understand Caregiver’s
feelings, and to be physically present and involved in care are approaches that allow
the family to change Caregiver’s hope state.
Practice touch, if appropriate and with authority, to show care, and encourage the
family to do the same. This approach provides comfort and is necessary for the
development of hope.
Present opportunities for the Caregiver to manage care setting. When a hopeless
Caregiver is given opportunities to make choices, his or her perception of
hopelessness may be reduced.
Promote the use of spiritual resources as desired. Religious practices may provide
strength and inspiration.
Provide plant or pet therapy if possible. Taking care of pets or plants promotes
redefining Caregiver’s identity and makes him or her feel needed and loved.
Refer Caregiver to self-help groups such as I Can Cope and Make Today Count.
INSUFFICINET KNOWLEDGE AND SKILLS
Caregivers need open and honest communication about their role and stroke
survivors’ abilities
Conducting a comprehensive predischarge nursing assessment of caregiver physical
and psychological health and social, financial, and spiritual needs initially and during
follow-up is essential
nurses should develop a highly individualized case management plan to help
caregivers attain skills and services necessary to facilitate success and seamless
postdischarge transition
basic information should be provided throughout acute and chronic care in both oral
and written formats, with frequent reinforcement of specific information in the
caregiving trajectory.
caregivers need tailored nursing interventions that develop and reinforce requisite
information and skills (including handling techniques and assisting with activities of
daily living), while being attentive to caregiver responses during teaching and
allowing time for return demonstration of skills and care.
Telephone follow-up by nurses to monitor how caregivers are coping with physical
and emotional aspects of caregiving is important.3
caregivers need suggestions for setting realistic goals to improve their physical (time
to exercise, eating a heart healthy diet) and psychological (time alone to do enjoyable
activities, such as reading, church, or social activities) well-being.
Skills training to offer support and teach effective coping skills, such as relaxation
techniques and problem-solving techniques, are useful in lessening negative caregiver
outcomes.
You might also like
- Cognitive and Behavioral Interventions in the Schools: Integrating Theory and Research into PracticeFrom EverandCognitive and Behavioral Interventions in the Schools: Integrating Theory and Research into PracticeRosemary FlanaganNo ratings yet
- Sap User TypesDocument69 pagesSap User Typesandree_my7493No ratings yet
- Places That Matter: Knowing Your Neighborhood through DataFrom EverandPlaces That Matter: Knowing Your Neighborhood through DataNo ratings yet
- Forensic Mental Health Assistant: Passbooks Study GuideFrom EverandForensic Mental Health Assistant: Passbooks Study GuideNo ratings yet
- How to Help Someone with Postnatal Depression: A Practical Handbook to Postpartum Depression and Maternal Mental Health in the First YearFrom EverandHow to Help Someone with Postnatal Depression: A Practical Handbook to Postpartum Depression and Maternal Mental Health in the First YearNo ratings yet
- Teenage Health Concerns: How Parents Can Manage Eating Disorders In Teenage ChildrenFrom EverandTeenage Health Concerns: How Parents Can Manage Eating Disorders In Teenage ChildrenNo ratings yet
- Psychiatry Under the Influence: Institutional Corruption, Social Injury, and Prescriptions for ReformFrom EverandPsychiatry Under the Influence: Institutional Corruption, Social Injury, and Prescriptions for ReformRating: 2 out of 5 stars2/5 (1)
- Children's Testimony: A Handbook of Psychological Research and Forensic PracticeFrom EverandChildren's Testimony: A Handbook of Psychological Research and Forensic PracticeNo ratings yet
- Our Hearts and Minds Together: A Practical Handbook in Emotional IntelligenceFrom EverandOur Hearts and Minds Together: A Practical Handbook in Emotional IntelligenceNo ratings yet
- The Evidence-Based Practice: Methods, Models, and Tools for Mental Health ProfessionalsFrom EverandThe Evidence-Based Practice: Methods, Models, and Tools for Mental Health ProfessionalsNo ratings yet
- Collaborative Problem Solving: An Evidence-Based Approach to Implementation and PracticeFrom EverandCollaborative Problem Solving: An Evidence-Based Approach to Implementation and PracticeAlisha R. PollastriNo ratings yet
- Learning and Attention Disorders in Adolescence and Adulthood: Assessment and TreatmentFrom EverandLearning and Attention Disorders in Adolescence and Adulthood: Assessment and TreatmentNo ratings yet
- Mental Health and Wellbeing: A guide for nurses and healthcare professionals working with adults in primary careFrom EverandMental Health and Wellbeing: A guide for nurses and healthcare professionals working with adults in primary careNo ratings yet
- The Anxiety and Stress Survival Guide for Women: Practical Strategies for Thriving in a Stressful WorldFrom EverandThe Anxiety and Stress Survival Guide for Women: Practical Strategies for Thriving in a Stressful WorldNo ratings yet
- Summary of Andrew J. Wakefield's Waging War On The Autistic ChildFrom EverandSummary of Andrew J. Wakefield's Waging War On The Autistic ChildNo ratings yet
- Surviving Anxiety: How to Reduce Stress, Overcome Anxiety, and Stop Anxiety AttacksFrom EverandSurviving Anxiety: How to Reduce Stress, Overcome Anxiety, and Stop Anxiety AttacksNo ratings yet
- Focus On YOUR BEST HEALTH: Smart Guide to the Health Care You DeserveFrom EverandFocus On YOUR BEST HEALTH: Smart Guide to the Health Care You DeserveRating: 5 out of 5 stars5/5 (1)
- Perkins Activity and Resource Guide - Chapter 4: Functional Academics: Second Edition: Revised and UpdatedFrom EverandPerkins Activity and Resource Guide - Chapter 4: Functional Academics: Second Edition: Revised and UpdatedNo ratings yet
- Solution Focused Harm Reduction: Working effectively with people who misuse substancesFrom EverandSolution Focused Harm Reduction: Working effectively with people who misuse substancesNo ratings yet
- Childhood Depression: Its Causes and Ways to Overcome ItFrom EverandChildhood Depression: Its Causes and Ways to Overcome ItRating: 5 out of 5 stars5/5 (1)
- Anger Management: How to Manage Your Anger, Control Your Emotions and Handle Behavioral Issues in Adults or Children.From EverandAnger Management: How to Manage Your Anger, Control Your Emotions and Handle Behavioral Issues in Adults or Children.Rating: 5 out of 5 stars5/5 (1)
- DSM distributed system management Complete Self-Assessment GuideFrom EverandDSM distributed system management Complete Self-Assessment GuideNo ratings yet
- The Family Guide to Preventing Elder Abuse: How to Protect Your Parents?and YourselfFrom EverandThe Family Guide to Preventing Elder Abuse: How to Protect Your Parents?and YourselfNo ratings yet
- Improving the Quality of Child Custody Evaluations: A Systematic ModelFrom EverandImproving the Quality of Child Custody Evaluations: A Systematic ModelNo ratings yet
- The Five Areas of Being Human: an Assessment Tool for Therapeutic Care: A Primer Guide for Effective Interviewing Skills and the Implementation of the Five Areas of Being Human Assessment Tool Related to Enhancing Precise Therapeutic TreatmentFrom EverandThe Five Areas of Being Human: an Assessment Tool for Therapeutic Care: A Primer Guide for Effective Interviewing Skills and the Implementation of the Five Areas of Being Human Assessment Tool Related to Enhancing Precise Therapeutic TreatmentNo ratings yet
- Abuses and Excuses: How To Hold Bad Nursing Homes AccountableFrom EverandAbuses and Excuses: How To Hold Bad Nursing Homes AccountableNo ratings yet
- A Mother’S Intuition: Autism—A Journey into Forgiveness and HealingFrom EverandA Mother’S Intuition: Autism—A Journey into Forgiveness and HealingNo ratings yet
- Prescription for Laughter: Handling Health-Care Hassles with HumorFrom EverandPrescription for Laughter: Handling Health-Care Hassles with HumorNo ratings yet
- Youth at Risk: A Prevention Resource for Counselors, Teachers, and ParentsFrom EverandYouth at Risk: A Prevention Resource for Counselors, Teachers, and ParentsNo ratings yet
- Fragile X Syndrome and Premutation Disorders: New Developments and TreatmentsFrom EverandFragile X Syndrome and Premutation Disorders: New Developments and TreatmentsRandi J HagermanNo ratings yet
- Intervention: Reducing Compassion Fatigue: About to Give up on Someone Who Needs Help?From EverandIntervention: Reducing Compassion Fatigue: About to Give up on Someone Who Needs Help?No ratings yet
- Collaborative Problem Solving Group A Complete Guide - 2020 EditionFrom EverandCollaborative Problem Solving Group A Complete Guide - 2020 EditionNo ratings yet
- Be a Better Boss: Learn to build great teams and lead any organization to successFrom EverandBe a Better Boss: Learn to build great teams and lead any organization to successNo ratings yet
- Survival Guide for Racially Abused PersonsFrom EverandSurvival Guide for Racially Abused PersonsRating: 5 out of 5 stars5/5 (1)
- ANGER MANAGEMENT FOR PARENTS: Advanced Methods and Strategies to be Calmer and More Patient with Your ChildrenFrom EverandANGER MANAGEMENT FOR PARENTS: Advanced Methods and Strategies to be Calmer and More Patient with Your ChildrenNo ratings yet
- Integrative Dual Diagnosis Treatment Approach to an Individual with Alcoholism and Coexisting Endogenous DepressionFrom EverandIntegrative Dual Diagnosis Treatment Approach to an Individual with Alcoholism and Coexisting Endogenous DepressionRating: 2 out of 5 stars2/5 (1)
- Osteoporosis: Current Concepts: Ibrahim Akkawi Hassan ZmerlyDocument6 pagesOsteoporosis: Current Concepts: Ibrahim Akkawi Hassan ZmerlyDimas M IlhamNo ratings yet
- Spermatogenesis and OogenesisDocument14 pagesSpermatogenesis and OogenesisClaude Peña100% (1)
- DuterteDocument19 pagesDutertePatricia Del RosarioNo ratings yet
- 1394-120 Final NCBC Gulfport HWMPDocument228 pages1394-120 Final NCBC Gulfport HWMPfranNo ratings yet
- Ojas The Vital Nectar of LifeDocument5 pagesOjas The Vital Nectar of LifevineethNo ratings yet
- PRRD Presentation-On-Federalism-By-Atty.-Rehan-Balt-LaoDocument82 pagesPRRD Presentation-On-Federalism-By-Atty.-Rehan-Balt-LaoLia GonzalesNo ratings yet
- Socio 102 Lesson 6. Sexual Health and HygieneDocument23 pagesSocio 102 Lesson 6. Sexual Health and HygieneVivian giducosNo ratings yet
- Celebrity Drug Use - Kusinitz, MarcDocument152 pagesCelebrity Drug Use - Kusinitz, MarcRen MNo ratings yet
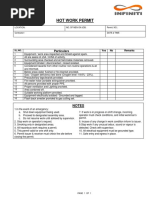
- IBSPL-HSE-F28 Hot Work PermitDocument2 pagesIBSPL-HSE-F28 Hot Work PermitAbdul RaheemNo ratings yet
- Genderen Et Al-1997-British Journal of HaematologyDocument6 pagesGenderen Et Al-1997-British Journal of HaematologyJicko Street HooligansNo ratings yet
- FMEA TemplateDocument5 pagesFMEA TemplateLeonardoVianna100% (2)
- Zurich Motor Flexible Condiciones Generales Inglés Zurich Tenerife La Palma Gran Canaria Lanzarote Fuerteventura GomeraDocument54 pagesZurich Motor Flexible Condiciones Generales Inglés Zurich Tenerife La Palma Gran Canaria Lanzarote Fuerteventura GomeraRogerfvNo ratings yet
- Materi 3. ASPEK MEDIKOLEGAL AUDIT KEMATIAN - Revised ABHDocument19 pagesMateri 3. ASPEK MEDIKOLEGAL AUDIT KEMATIAN - Revised ABHverawatiNo ratings yet
- EHS Alert 128 (Snake Bite Incident) .PubDocument1 pageEHS Alert 128 (Snake Bite Incident) .Pubrizvidawar220No ratings yet
- EnderalDocument14 pagesEnderalFulanNo ratings yet
- Bio TextDocument4 pagesBio TextNaufal Riza PurwadiNo ratings yet
- Property ReviewerDocument73 pagesProperty ReviewerJul A.No ratings yet
- Malignant & BenignDocument13 pagesMalignant & BenignJohn Carlo SuratosNo ratings yet
- Operations Final ReportDocument12 pagesOperations Final ReportMustafa SethiNo ratings yet
- 145 - Fine Motor Milestones PDFDocument2 pages145 - Fine Motor Milestones PDFhuwaina100% (3)
- Essay On Health and FitnessDocument8 pagesEssay On Health and Fitnessuiconvbaf100% (2)
- AmazingDocument18 pagesAmazingNazim DjedaaNo ratings yet
- Final Manpower PlanningDocument14 pagesFinal Manpower PlanningRohit AnandNo ratings yet
- Marcus Mcgregor Intermediate First Aid, CPR C & AED: St. John Ambulance Certifies ThatDocument1 pageMarcus Mcgregor Intermediate First Aid, CPR C & AED: St. John Ambulance Certifies Thatapi-608285654No ratings yet
- Employee's Evaluation PhrasesDocument3 pagesEmployee's Evaluation PhrasesRobert D.PalbanNo ratings yet
- Anger, Hostility, and Aggression Lecture VersionDocument65 pagesAnger, Hostility, and Aggression Lecture Versionsheliafoster50% (2)
- A Learning Material in P.E. 14 PDFDocument28 pagesA Learning Material in P.E. 14 PDFDenmark BaduaNo ratings yet
- Module 12-Private STPDocument89 pagesModule 12-Private STPPhel FloresNo ratings yet
- AAA Mixed Pain SMGDocument37 pagesAAA Mixed Pain SMGandhita96No ratings yet