0 ratings0% found this document useful (0 votes)
40 viewsAdpie Pediatrics Diarrhea Vomiting
Adpie Pediatrics Diarrhea Vomiting
Uploaded by
Jamie Lemons1. The nursing care plan addresses a child with fluid volume deficit due to diarrhea and vomiting.
2. Assessment findings include increased heart rate and decreased blood pressure. The plan involves monitoring stool characteristics and frequency of vomiting and assessing for dehydration.
3. The goal is for the child to no longer have diarrhea and vomiting within an 8 hour shift and to tolerate feedings and normal elimination patterns. Interventions include observation, assessment, providing rest and skin care.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Adpie Pediatrics Diarrhea Vomiting
Adpie Pediatrics Diarrhea Vomiting
Uploaded by
Jamie Lemons0 ratings0% found this document useful (0 votes)
40 views2 pages1. The nursing care plan addresses a child with fluid volume deficit due to diarrhea and vomiting.
2. Assessment findings include increased heart rate and decreased blood pressure. The plan involves monitoring stool characteristics and frequency of vomiting and assessing for dehydration.
3. The goal is for the child to no longer have diarrhea and vomiting within an 8 hour shift and to tolerate feedings and normal elimination patterns. Interventions include observation, assessment, providing rest and skin care.
Original Title
ADPIE PEDIATRICS DIARRHEA VOMITING
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
1. The nursing care plan addresses a child with fluid volume deficit due to diarrhea and vomiting.
2. Assessment findings include increased heart rate and decreased blood pressure. The plan involves monitoring stool characteristics and frequency of vomiting and assessing for dehydration.
3. The goal is for the child to no longer have diarrhea and vomiting within an 8 hour shift and to tolerate feedings and normal elimination patterns. Interventions include observation, assessment, providing rest and skin care.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
40 views2 pagesAdpie Pediatrics Diarrhea Vomiting
Adpie Pediatrics Diarrhea Vomiting
Uploaded by
Jamie Lemons1. The nursing care plan addresses a child with fluid volume deficit due to diarrhea and vomiting.
2. Assessment findings include increased heart rate and decreased blood pressure. The plan involves monitoring stool characteristics and frequency of vomiting and assessing for dehydration.
3. The goal is for the child to no longer have diarrhea and vomiting within an 8 hour shift and to tolerate feedings and normal elimination patterns. Interventions include observation, assessment, providing rest and skin care.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 2
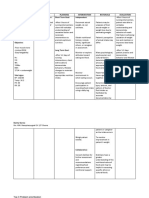
Nursing of the Childbearing Family
Nursing Care Plan (ADPIE)
Assessment Diagnosis Planning Implementation Rationale Evaluation
Objective Data Fluid volume deficit Client Goal Independent Interventions
Bp 96/68, RR20, r/t diarrhea, vomiting Pt. will be free of 1.Observe stools for
Aids in determining
HR120 diarrhea and vomiting amount, color, Child’s bowel function
and in monitoring the
T 37.2C (98.9F), an consistency, odor and will return to normal
child’s status
BUN 20 frequency
Creatinine 0.9 Child will have normal
Contributes to fluid
2. Assess for vomiting fluid and electrolyte
volume deficit
balance
3.
4.
5.
Subjective Data Theory Goal Evaluation Interdependent Interventions
(cite references) Healthcare Profession Rationale Evaluation
Parent reports Gastroenteritis is the Client will tolerate
vomiting and diarrhea inflammation of the feeding and 1.
x 2-3 days stomach and the elimination patterns
intestines, typically will return to normal 2.
resulting from within an 8hr shift
bacterial toxins or 3.
viral infection and
causing nausea and
diarrhea. Children
with gastroenteritis
may waken freq. with
bouts of vomiting. IF
the child is
hospitalized it is
important to assess
onset, frequency,
color, amount and
consistency of stools.
If the child is vomiting
it is important to
monitor the amount
and type of vomitus.
Observe the child for
signs and symptoms
of dehydration, which
reflect underlying
fluid and electrolyte
imbalances Evaluate
urinary output and
specific gravity. An
accurate weight must
be obtained on
admission and daily
thereafter. Monitor
VS every 4 hrs.
promote rest and
comfort. Provide skin
care after each bout
of diarrhea. Liquids
are offered , small
amount of normal
diet for age are
provided. Discharge
teaching teaches the
parents the s/s of
dehydration and what
actions to take if the
diarrhea reoccurs.
Cited: Ball & Bindler,
6th edition, Chapter 25
Alteration in GI
Function
You might also like
- A008 MicroVue C4d EnglishDocument15 pagesA008 MicroVue C4d EnglishAlisNo ratings yet
- NCP Risk For Deficient Fluid Volume PotentialDocument4 pagesNCP Risk For Deficient Fluid Volume PotentialArian May Marcos100% (1)
- Presentation On Dengue FeverDocument31 pagesPresentation On Dengue FeverDrMuhammad Ishfaq Habib100% (2)
- NCP High Risk PregnancyDocument7 pagesNCP High Risk PregnancyRica ParcasioNo ratings yet
- Nursing-Care-Plan - AgeDocument7 pagesNursing-Care-Plan - AgePanda JocyNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument7 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationpamelaideaNo ratings yet
- Nursing Care Plan 1Document2 pagesNursing Care Plan 1Denise GabatoNo ratings yet
- College of Nursing: University of The EastDocument8 pagesCollege of Nursing: University of The EastroblesNo ratings yet
- Nursing Care Plan For Diarrhea 2Document1 pageNursing Care Plan For Diarrhea 2Skyla Fiesta0% (1)
- 8NCP S For ColostomyDocument23 pages8NCP S For ColostomylovelykissNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermLorie May GuillangNo ratings yet
- NCP-CKD LabcoDocument5 pagesNCP-CKD Labcojay kusainNo ratings yet
- Sumaoang, Chris Deinielle M - Imbalance Nutrition, Less Than Body RequirementsDocument3 pagesSumaoang, Chris Deinielle M - Imbalance Nutrition, Less Than Body RequirementsMina SumaoangNo ratings yet
- JVJV NCP Risk For Fluid Volume DeficitDocument2 pagesJVJV NCP Risk For Fluid Volume DeficitvicenteturasNo ratings yet
- Case Study: Subjective: Objective: General Objective: Independent IndependentDocument10 pagesCase Study: Subjective: Objective: General Objective: Independent IndependentChristine EmanNo ratings yet
- Nursing Care Plan: Saint Louis University School of Nursing Bonifacio Street, Baguio CityDocument3 pagesNursing Care Plan: Saint Louis University School of Nursing Bonifacio Street, Baguio CitySoniaMarieBalanayNo ratings yet
- Improved NutritionDocument2 pagesImproved NutritionDaintyGarciaNo ratings yet
- NCP RiskDocument2 pagesNCP RiskPaolo Vittorio Perdigueros GonzalesNo ratings yet
- Gestational Diabetes - Case Study 2Document13 pagesGestational Diabetes - Case Study 2Bb RabbitNo ratings yet
- NCP FormatDocument2 pagesNCP FormatellisequeenieNo ratings yet
- NRS456 - Malnutrition - Written Assignment-2Document12 pagesNRS456 - Malnutrition - Written Assignment-2najwaNo ratings yet
- Fluid Volume Deficit R/T Diarrhea & VomitingDocument4 pagesFluid Volume Deficit R/T Diarrhea & Vomitingjisoo100% (3)
- Ate Gabs Nyo Pagod NaDocument3 pagesAte Gabs Nyo Pagod NaGabrielle EvangelistaNo ratings yet
- FNCP SampleDocument2 pagesFNCP SampleDonna Mae BoolNo ratings yet
- Imbalanced Nutrition Less Than Body Requirement R/T Insufficient Intake of Food Rich in Potassium and Intestinal DisturbancesDocument22 pagesImbalanced Nutrition Less Than Body Requirement R/T Insufficient Intake of Food Rich in Potassium and Intestinal DisturbancesJor GarciaNo ratings yet
- Clint NCPDocument2 pagesClint NCPCrisza HalosNo ratings yet
- A Nursing Care Plan On: Loose Bowel MovementDocument6 pagesA Nursing Care Plan On: Loose Bowel MovementakoitsmeNo ratings yet
- Lactoferrin and lysozyme to promote nutritional, clinical and enteric recovery: a protocol for a factorial, blinded, placebocontrolled randomised trial among children with diarrhoea and malnutrition (the Boresha Afya trial)Document14 pagesLactoferrin and lysozyme to promote nutritional, clinical and enteric recovery: a protocol for a factorial, blinded, placebocontrolled randomised trial among children with diarrhoea and malnutrition (the Boresha Afya trial)Sofia SPNo ratings yet
- Risk NCP - PESCADERO 4CDocument1 pageRisk NCP - PESCADERO 4COrlando VillanuevaNo ratings yet
- CareplanconstipationDocument2 pagesCareplanconstipationRachel ByersNo ratings yet
- ROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPDocument6 pagesROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPkimberly quitonNo ratings yet
- NCP Nausea and VomitingDocument4 pagesNCP Nausea and VomitingKingJayson Pacman06No ratings yet
- NCP TyphoidDocument2 pagesNCP TyphoidMae Arra Lecobu-anNo ratings yet
- Risk For Imbalanced NutritionDocument3 pagesRisk For Imbalanced Nutritionaudreyann.acobNo ratings yet
- NCP (Acute Gastroenteritis) Vizconde, Ehreiz Raiden C. BSN2-ADocument5 pagesNCP (Acute Gastroenteritis) Vizconde, Ehreiz Raiden C. BSN2-ARaiden VizcondeNo ratings yet
- Prince NCPDocument9 pagesPrince NCPALVARADO, KRISTINE JOYNo ratings yet
- Assessment Diagnosis Background Study Planning Intervention Rationale EvaluationDocument4 pagesAssessment Diagnosis Background Study Planning Intervention Rationale Evaluationahz_kerian2No ratings yet
- NCP 1 & 2Document7 pagesNCP 1 & 2Jessica GlitterNo ratings yet
- "Nilalagnat Ang Anak Ko." AsDocument2 pages"Nilalagnat Ang Anak Ko." AsgeorgiaNo ratings yet
- Diarrhea Case PresentationDocument15 pagesDiarrhea Case Presentationmary cruzNo ratings yet
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation Subjective: STO: Within 4 Hour of DX: DX: Sto: Goal MetDocument5 pagesAssessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation Subjective: STO: Within 4 Hour of DX: DX: Sto: Goal MetRussel SantosNo ratings yet
- Hydatidiform Mole (H. Mole) : I. DescriptionDocument9 pagesHydatidiform Mole (H. Mole) : I. DescriptionKristina Ana ClaudioNo ratings yet
- Health Problem Family Nusing Problem Goals of Care Objectives of CareDocument2 pagesHealth Problem Family Nusing Problem Goals of Care Objectives of CareShai IbrahimNo ratings yet
- GC ncp1 and 2Document4 pagesGC ncp1 and 2Jobelle AcenaNo ratings yet
- Conley Plan of Care Nur 320Document3 pagesConley Plan of Care Nur 320api-458494853No ratings yet
- Final Carotenoid Status in College StudentsDocument21 pagesFinal Carotenoid Status in College Studentsapi-665569952No ratings yet
- NCP PediatricDocument5 pagesNCP PediatricSL Hanna NebridaNo ratings yet
- NCP TemplateDocument3 pagesNCP TemplateAlvin John BarramedaNo ratings yet
- Nursing Care Plan NewDocument8 pagesNursing Care Plan NewhdubcmchNo ratings yet
- Nursing Care Plan Patient's Name: Age: Sex: Address:: Nursing-Notes/communicable - Diseases - Notes/amoebiasisDocument4 pagesNursing Care Plan Patient's Name: Age: Sex: Address:: Nursing-Notes/communicable - Diseases - Notes/amoebiasisGILIANNE MARIE JIMENEANo ratings yet
- GASTRITISDocument11 pagesGASTRITIStamannaNo ratings yet
- Electolyte ImbalanceDocument2 pagesElectolyte ImbalanceFouzia GillNo ratings yet
- Sample Case Pres - ScenarioDocument15 pagesSample Case Pres - ScenariogustomonglemonNo ratings yet
- NCP For Fluid Volume Deficit and MyomaDocument5 pagesNCP For Fluid Volume Deficit and MyomaRhyle John JimenezNo ratings yet
- LeeTinYanEmma 21002276Document4 pagesLeeTinYanEmma 21002276emmaleowendyNo ratings yet
- NCP Deficit Fluid VolumeDocument4 pagesNCP Deficit Fluid VolumeKingJayson Pacman06No ratings yet
- BEHS ExecutiveSummaryDocument4 pagesBEHS ExecutiveSummaryMayra ParrillaNo ratings yet
- Nursing Plan of Care - FinalDocument3 pagesNursing Plan of Care - Finalapi-642989736No ratings yet
- MRS. A CaseDocument9 pagesMRS. A CasehaibaraNo ratings yet
- Facto NCPDocument3 pagesFacto NCPkkd nyleNo ratings yet
- Clinical Learning Log 3 Go Solo - Docx-1Document11 pagesClinical Learning Log 3 Go Solo - Docx-1JezraleFame AntoyNo ratings yet
- Fluid Therapy in DengueDocument54 pagesFluid Therapy in DengueVithiya Chandra SagaranNo ratings yet
- WD 3d November WK 3 Tracking ToolDocument22 pagesWD 3d November WK 3 Tracking ToolGeorge ApaNo ratings yet
- Nodular Swelling of The Buccal Mucosa: Clinical PresentationDocument7 pagesNodular Swelling of The Buccal Mucosa: Clinical Presentationotoralla1591No ratings yet
- Nsaids and DmardsDocument59 pagesNsaids and DmardsBaidawu Weso-amo IbrahimNo ratings yet
- ERAS For Vascular SurgeryDocument24 pagesERAS For Vascular Surgerybayuaa100% (1)
- Cap 1 EndoDocument33 pagesCap 1 EndoDaniela SosaNo ratings yet
- American Cancer Society, 2018Document8 pagesAmerican Cancer Society, 2018Julio GomezNo ratings yet
- DR Drishti Oct LogbookDocument7 pagesDR Drishti Oct LogbookDrishti chautaniNo ratings yet
- Schist o SomaDocument9 pagesSchist o SomaROHITNo ratings yet
- Lewis Medical Surgical Nursing Chapter 1Document7 pagesLewis Medical Surgical Nursing Chapter 1JimNo ratings yet
- Chapter 25 The Child With Cardiovascular DysfunctionDocument20 pagesChapter 25 The Child With Cardiovascular DysfunctionJill Hill100% (3)
- Approach To Balanitis/balanoposthitis: Current Guidelines: Residents PageDocument4 pagesApproach To Balanitis/balanoposthitis: Current Guidelines: Residents PageTeja Laksana NukanaNo ratings yet
- Comparison of Two Different Matrix Band Systems in Restoring Two Surface Cavities PDFDocument6 pagesComparison of Two Different Matrix Band Systems in Restoring Two Surface Cavities PDFel verdaderoNo ratings yet
- What Exactly Is Uterine Prolapse?Document3 pagesWhat Exactly Is Uterine Prolapse?Ika SriNo ratings yet
- Types of AnemiaDocument3 pagesTypes of Anemiaflex gyNo ratings yet
- Drugs Post PartumDocument3 pagesDrugs Post PartumanreilegardeNo ratings yet
- Pedo 4-DikonversiDocument7 pagesPedo 4-DikonversiFeby ElisabethNo ratings yet
- Long Covid DR Edt - Pit Ipd - 07.08.21Document36 pagesLong Covid DR Edt - Pit Ipd - 07.08.21Pamela JenniferNo ratings yet
- UltramageDocument12 pagesUltramagegi vrgs0% (1)
- 1683 PDFDocument297 pages1683 PDFBianca Lacramioara Florea100% (1)
- Summary of Diagnosis and Treatment of Genital UlcerDocument4 pagesSummary of Diagnosis and Treatment of Genital UlceryolandadwiooNo ratings yet
- MumpsDocument19 pagesMumpsAmri RizalNo ratings yet
- Survanta 25mg - ML Suspension - Summary of Product Characteristics (SMPC) - (Emc)Document7 pagesSurvanta 25mg - ML Suspension - Summary of Product Characteristics (SMPC) - (Emc)Mohadese hosseini zabetNo ratings yet
- Mobile Blood DonationDocument10 pagesMobile Blood DonationChristine ApoloNo ratings yet
- Falcons OpthalmologyDocument20 pagesFalcons Opthalmology175 Yellamraju VidhatriNo ratings yet
- New Anticancer Agents: in Vitro and in Vivo EvaluationDocument13 pagesNew Anticancer Agents: in Vitro and in Vivo Evaluationandi tiaNo ratings yet
- Nursing Process and Critical Thinking Review Test - ProProfs QuizDocument1 pageNursing Process and Critical Thinking Review Test - ProProfs QuizDeborah Rhoda AcheampongNo ratings yet
- New Drug Approval From Cdsco Till DateDocument5 pagesNew Drug Approval From Cdsco Till DateAshish1pharmaNo ratings yet