0 ratings0% found this document useful (0 votes)
49 viewsIncreased ICP: A) Headache
Increased ICP: A) Headache
Uploaded by
mohamed nagyThis document summarizes information about cerebrospinal fluid (CSF), including its physiology, production, absorption, circulation, factors affecting flow, and functions. It also discusses lumbar puncture (LP) procedures, indications, contraindications, and complications. Finally, it provides information on the analysis of CSF, mechanisms and signs/symptoms of increased intracranial pressure, types of brain herniation, mechanisms and types of brain edema, and idiopathic intracranial hypertension (IIH, also known as benign intracranial hypertension or pseudotumor cerebri).
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Increased ICP: A) Headache
Increased ICP: A) Headache
Uploaded by
mohamed nagy0 ratings0% found this document useful (0 votes)
49 views5 pagesThis document summarizes information about cerebrospinal fluid (CSF), including its physiology, production, absorption, circulation, factors affecting flow, and functions. It also discusses lumbar puncture (LP) procedures, indications, contraindications, and complications. Finally, it provides information on the analysis of CSF, mechanisms and signs/symptoms of increased intracranial pressure, types of brain herniation, mechanisms and types of brain edema, and idiopathic intracranial hypertension (IIH, also known as benign intracranial hypertension or pseudotumor cerebri).
Original Title
csf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
This document summarizes information about cerebrospinal fluid (CSF), including its physiology, production, absorption, circulation, factors affecting flow, and functions. It also discusses lumbar puncture (LP) procedures, indications, contraindications, and complications. Finally, it provides information on the analysis of CSF, mechanisms and signs/symptoms of increased intracranial pressure, types of brain herniation, mechanisms and types of brain edema, and idiopathic intracranial hypertension (IIH, also known as benign intracranial hypertension or pseudotumor cerebri).
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
49 views5 pagesIncreased ICP: A) Headache
Increased ICP: A) Headache
Uploaded by
mohamed nagyThis document summarizes information about cerebrospinal fluid (CSF), including its physiology, production, absorption, circulation, factors affecting flow, and functions. It also discusses lumbar puncture (LP) procedures, indications, contraindications, and complications. Finally, it provides information on the analysis of CSF, mechanisms and signs/symptoms of increased intracranial pressure, types of brain herniation, mechanisms and types of brain edema, and idiopathic intracranial hypertension (IIH, also known as benign intracranial hypertension or pseudotumor cerebri).
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 5
At a glance
Powered by AI
The key takeaways are that CSF is produced and absorbed continuously, its flow is affected by pulsations of arteries and movement of ependymal cells, and it serves to provide support and a stable environment for neurons.
The factors that affect CSF flow are pulsations of cerebral and spinal arteries in the subarachnoid space, movement of cilia of ependymal cells, and the continuous production and absorption of CSF which creates positive and negative pressures.
The causes of increased intracranial pressure include cerebral or extracerebral masses, generalized brain swelling, increased venous pressure, obstruction of CSF flow or absorption, and increased CSF volume from conditions such as subarachnoid hemorrhage or meningitis.
CSF
Physio Vol 120 ml
Rate of formation: 0.35ml/ min = 21-22 ml/hour = 500 ml/ day.
CSF renewed 4-5 times daily.
Secret Choroid plexus ventricles
Absorp Arachnoid villi in venous sinuses (mainly SSS)
Spinal nerve pockets into lymphatic system.
Gap junctions () ependymal cells & () pial cells → into brain extracellular space.
Small vein in SAS → venous blood
Circ Lat vent→ Monro → 3rd → cerebral aqueduct of sylvius → 4th →foramen of Lushka,
Magendi → SAS
Factors Pulsations of cerebral, spinal arteries in SAS.
Affect Movement of cilia of ependymal cells.
flow + ve and -ve pressure created by continuous production and absorption.
Funct support, stable env for neurons, transporter metabolites
LP Proced Lt lat, flexed hip, knee, L345, lignocaine local anasth, needle 22G
Indicat D: Infection (3), SAH (xanthochromia), Ms (OCB), Mg, sarcoidosis, vasculitis, IIH
Th: ↓CSF pressure, contrast media, spinal anasth
CI IC SOL, local skin infect, anticoagulant, coagulation defect, spinal block
Comp 1) Headache after few hr→ throbbing, associated with
N, V, giddiness, pain in the neck & back.
2) Diplopia due to transient uni or bilateral 6th nerve palsy.
3) S.A. bleeding disorder, throbbing pain.
4) Introduction of leukaemic cells or microorganisms into SAS, prolapsed
intervertebral disc.
Analysis Normal, infection (3), SAH, MS
Increased ICP
Mech 1)Cerebral/extracerebral mass: tumor, infarction, contusion, abscess
2)Generalized brain swelling: Anoxia, HTN, Encephalopathy, trauma, acute liver failure
3)venous pressure: HF, SVC obst, mediastinal syndrome, cerebral venous thrombosis
4)Obstruction of CSF flow or absorption: hydrocephalus
5)CSF volume: SAH, meningitis, production (choroid plexus tumor)
C/P A)Headache:
D2 distortion of pain sensitive structures (dura & blood vessels)
Throbbing, ↑in the morning,
Frontal or occipital or both, may be unilateral
↑by exertion, cough, straining, sudden postural change.
B)Vomiting:
More in the morning with headache (d2 compression or ischemia of vomiting center in medulla)
C)Papilloedema:
D2 to CSF pressure in optic nerve sheath→ prevent venous drainage, axoplasmic flow in
optic neurons) → not cause neuronal damage with maintenance of CBF.
D)Bradycardia: D2 cardiac center dysfunction or Tachycardia in infratentorial lesions
E)Breathing control:
Sudden ICP slow deep resp
Late, chyne stokes, shallow rapid in deep coma
F)False localizing signs
Uni or bilateral 6th , bilateral extensor planter, grasp reflex, 3rd N palsy
Brain Herniation
Uncal Unilateral expanding mass → tentorial PCA occluded→ HH, (BS infarct)
(tentorial lateral) (uncal) herniation as the medial edge of RF →conscious level.
temporal lobe herniates through the tentorial Pressure on opposite cerebral
hiatus peduncle (Kernhan's notch) → ∆ limb
e Continuous ↑ICP→ central herniation weak on same side of lesion (false
locating sign).
Compression 3rd → pupil dilatation,
failure to react to light.
Central Midline lesion or diffuse swelling of cerebral Pressure on dorsal aspect
(tentorial hemispheres → ventral displace of midbrain , (pretectum, superior colliculi) →
central) diencephalon through tentorial hiatus → impairs eye movements → upward
damage of these structures by mechanical gaze is initially lost.
distortion , ischemia 2ry to stretching of Diencephalon, midbrain damage
perforating vessels → conscious level
May progress to tonsillar herniation. Pupil→ initially small →
moderately dilated and fixed to light.
Downward traction on pituitary
stalk, hypothalamus → D.I.
Subfalcine Occur early as SOL→ angulate gyrus under Seldom produces any clinical effect.
Cingulate falx Ipsilateral ACA occlusion.
(midline shift)
Trans-calvarial Brain, #, surgical site
Tonsillar Subtentorial expanding mass → herniation of Tonsillar impaction in foramen
(↓cerebellar) cerebellar tonsils through foramen magnum + magnum → neck stiffness, head tilt.
3 Chiari malf A degree of upward herniation through Brain stem pressure :
tentorial hiatus a) Conscious level.
- Clinical picture difficult to differential b) Resp irregularities; chyne
diagnosed from direct brain stem strokes, central
compression. hyperventilation, ataxic,
gasping, arrest.
Reversed Cerebellum, tentorium Push MB up
tentorial
(↑cerebellar)
Brain edema
Vasogenic (Open barrier) Cytotoxic (Cellular) Interstitial
Path Cap permeability & open Disruption of cell memb Block CSF brain fluids
BBB cellular swelling
AE Tumor Hypoxia with IC osmoles Obstructive
Abscess (Na, H, lactate) hydrocephalus
Hge, infarction, contusion Acute hypoosmolatity Pseudotumor cerebri
Acute demyelination (SIADH)
Purulent meningitis Dysequilibrium synd
Site Mainly white matter Grey> white Periventricular white matter
Path Open BBB Intact BBB Intact BBB
↑cap permeability Disruptn cell memb → cell swell Block CSF → ↑brain fluid
MRI Contrast enhancement No enhancement CT: perivent hypodensity
↑diffusion coefficient ↓ diffusion coefficient
CSF protein Normal protein
C/P Focal deficit, consc, ICP consc, myoclonus, seizures Severdementia, gait dist
TTT Steroid: in tumor, abscess Steroid: not effective Steroid: uncertain role
Osmotherapy Osmotherapy Osmotherapy: rarely used
Treatment of brain edema:
1) Treatment of the cause
2) Care of comatose patient
3) Pharmacological ttt:
Corticosteroid: in vasogenic edemad2 tumor, ICH, head trauma, meningitis (4mg/6hr)
Osmotherapy (mannitol)
Drugs CSF formation: actozolamide
4) Others: hyperventilation, hypothermia, barbiturate ttt
IIH = BIH = PseudoTm cerebri
Def Persistent ↑CSF pressure in absence SOL é ventricles N or ↓size
Incid ♀, 3rd-4th decade
AE: Idiopathic
Arachnoid grandulation: d2 previous inflam, SAH
Obstruction of venous drainage: d2 DST, hypercoagulable state
Endocrine Preg, menarch, menst irreg, Addison, acromegaly, ↓thyroid, ↓PTG
Diet Obesity, ↑vitA
Drug OCP, steroid édrawal, amiodarone, danazole, tetracycline, nitrofurantoin
Hematoloic IDA, Polycythemia rubra vera
Others SLE, meningism é systemic infection, polyneuritis, empty sella syndrome
Path ↑CSF formation
↓CSF absorption
↑Venous pressure from ↑I.Abd.P
Abn cerebral microvasculature é ↑water content brain (sort of brain edema)
Symp Headache:
Diffuse, but may be bitemporal or bioccipital
Constant, severe > any previous H/A,
↑at night, on awakening, by cough, straining, ↓by tapping
Vomiting (occasional)
Transient visual obscuration:
D2 intermittent ischemia optic disc
Uni or bilateral
Brief episodes (seconds) of greying, blackening
by change in posture or valsalva maneuver, by tap & medical ttt
Ocular: ↓VA, diplopia,
Self-audible bruit in ears (pressure diff in cranial, jug V)
Signs Papilledema
6th, 3rd CN palsy
Field defect: enlarged blind spot, central/centrocecal periph field constriction
DD Other causes papilledema
Inv CT, MRI: small, slit like vent, no shift (exclude SOL, DST)
LP: after exclusion SOL, coagulation profile, opening pressure >250mmH2O
Visual field (perimetry)
TTT Medical ↓Wt, Analgesics H/A, Avoid causative drugs
CAI (acetazolamide 1-4gm/d),
Diuretic (Lasix 40-160mg/d),
Osmotic agent: Glycerol ¼-½ml/kg/4-6hr, mannitol
Steroid not used d2 rec papilledema after édrawal, ↑wt (used for short course)
LP Series of CSF édrawal (15-30ml)
Surgic Indication: failed medical ttt, threatened vision
Types: ventriculoperit shunt, optic sheath fenestration, subtemporal decompression
HCP
Def ↑CSF vol éin skull d2 abnormal production, circulation, absorption
AE Obstructive Communicating
Intravent: obst MSLM ↑CSF production: ch plexus papilloma
Extravent: obst base brain, tentorial level
Congenital: Arnold chiari, IU infection Impaired CSF absorption:
Post-inflam: TB, M, carcinomatous M Congenital: arach villi agenesis
Post-Hge: SAH, IVH ↑CSF Pr (SC Tm, polyneuritis)
Mass lesion: SOL, ICH, Cerebellar hge, infarct Tm seeding (ependymoma)
Venous insufficiency (Sinus thrombosis)
CP Before closure fontanells After closure fontanels
↑ICT (mild, late) ↑ICT: 3B
Skull: ↑head circumf all diameter> 75cm Skull: No enlargement if >3yr
F&O bossing, craniofacial disproportion Venous congestion scalp
Sun setting eye Cracked pot
Wide suture, enlarged ant fontanel
Cracked pot on percussion
M: weakness, wasting, spasticity LL>UL M: clumsiness, no gross weakness
↑Rx, ext planter ↨Rx, ext planter
S: intact S: intact
CN: optic atrophy, rarely papilledema, ↓VA CN: 5, 6, 7
Squint, sluggish pup Rx,
Loss upward, lateral gaze
↓Cognition, memory, N IQ (in mild cases) Giddiness, Mild MR
Convulsions (common) Convulsions (↓)
Obesity, DI (hypoth, pit) Obesity, genital atrophy (pit)
CSF rhinorrhea (rare) Otitic HCP:
Bobble head doll synd: Purulent ear disch,
2-4 oscillation of head movement with Ipsilateral 6th N palsy
psychomotor retardation Papilledema
rd
D2 obst in or near 3 vent or aquiduct
Inv Skull transillumination
Skull US: follow up infant for progressive HCP (supependymal & IVH)
Skull measurement: for follow up
Skull X-ray: clavarium, suture diastasis, thinning of convolutional markings, eroded clinoid
process, deepened sella turcica
CT, MRI
Pressure monitoring LP: CSF pulse wave analysis is more reliable
TTT Medical Limited value (acetazolamide, lasix)
Surgical TTT AE (excision ch plexus)
Obstructive: ventricular drain, ventriculoperit shunt, ventriculostomy
Communicating: LP, lumboperitoneal shunt
NPH (Adam Hakim)
AE CP ∆ Inv
SAH Gait apraxia CT: enlarged ventricle, dilated T horn
Post-M Subcortical dementia MRI: measure vol ventric/SAS CSF
Achondroplasia Urgency, frequency, incontinence CSF flowmetry, No WM changes
Mucopolysaccharoidosis LP: continous IC monitoring
of meninges (if B wave >5% → need drainage operat)
You might also like
- Surgery Quest OCRDocument401 pagesSurgery Quest OCRKhankir cheleNo ratings yet
- STEP 1 CluesDocument3 pagesSTEP 1 CluesRaji NaamaniNo ratings yet
- Nervous System AlterationsDocument62 pagesNervous System AlterationsAsal SalahNo ratings yet
- Cerebrovascular Diseases Risk Factors:: o o o o oDocument4 pagesCerebrovascular Diseases Risk Factors:: o o o o otrinaNo ratings yet
- CHT DMARDDocument3 pagesCHT DMARDkoolaberNo ratings yet
- DD Nyeri Kepala Skenario 1Document8 pagesDD Nyeri Kepala Skenario 1Ika Putri YulianiNo ratings yet
- NeurologyDocument62 pagesNeurologyActeen MyoseenNo ratings yet
- Meninges, Ventricles - CSF - Study GuideDocument3 pagesMeninges, Ventricles - CSF - Study Guideshivani patelNo ratings yet
- MS Myasthenia Gravis Gillian-Barre Syndrome Parkinson's: Ascending Reversible ParalysisDocument5 pagesMS Myasthenia Gravis Gillian-Barre Syndrome Parkinson's: Ascending Reversible ParalysishaxxxessNo ratings yet
- M A N A G E M E NT OF H E A D I NJ UR Y & I NT R A CR A N I A L P RE SS UR EDocument19 pagesM A N A G E M E NT OF H E A D I NJ UR Y & I NT R A CR A N I A L P RE SS UR EmugihartadiNo ratings yet
- REV PharmaDocument21 pagesREV PharmaCarl Angelo SuaybaguioNo ratings yet
- D Evaluation For Resective Epilepsy SurgeryDocument104 pagesD Evaluation For Resective Epilepsy SurgeryYusuf BrilliantNo ratings yet
- UPDRS (Data Sheet)Document2 pagesUPDRS (Data Sheet)CNS WARDNo ratings yet
- Headache: Differential Diagnosis of HeadacheDocument139 pagesHeadache: Differential Diagnosis of Headachemero1983No ratings yet
- 03 TumoursDocument50 pages03 TumoursMalinda KarunaratneNo ratings yet
- Hem/Onc USML Organization ChartDocument1 pageHem/Onc USML Organization ChartJJNo ratings yet
- Symptom Onset Arrival: Circle Yes, No or Not Known As AppropriateDocument2 pagesSymptom Onset Arrival: Circle Yes, No or Not Known As AppropriateB-win IrawanNo ratings yet
- 05 Degenerative - Demyelinating DiseasesDocument26 pages05 Degenerative - Demyelinating DiseasesMalinda KarunaratneNo ratings yet
- Characterstic Drug ToxicitiesDocument3 pagesCharacterstic Drug ToxicitiesJorge PalazzoloNo ratings yet
- Stroke Inclusion Exclusion StrokeDocument1 pageStroke Inclusion Exclusion Strokecdeepak71No ratings yet
- Neurology 5Document5 pagesNeurology 5Loyla RoseNo ratings yet
- Donepezil in Vascular Dementia: A Randomized, Placebo-Controlled StudyDocument9 pagesDonepezil in Vascular Dementia: A Randomized, Placebo-Controlled StudyDian ArdiansyahNo ratings yet
- Neuro DDXDocument5 pagesNeuro DDXDDXNo ratings yet
- Infections Diseases of The Central Nervous System: Chapter VI - J. RuscalledaDocument11 pagesInfections Diseases of The Central Nervous System: Chapter VI - J. RuscalledaArif BudimanNo ratings yet
- Neurology ReviewerDocument72 pagesNeurology ReviewerPeter InocandoNo ratings yet
- Pharm TableDocument35 pagesPharm TableHannah BaldwinNo ratings yet
- Imaging Alzheimer PDFDocument22 pagesImaging Alzheimer PDFSuman SharmaNo ratings yet
- Therapeutics of Alzheimer's DiseaseDocument24 pagesTherapeutics of Alzheimer's DiseaseArtemis LiNo ratings yet
- (MicroB) Brainstem Lesions - Dr. Bravo (Nico Castillo)Document4 pages(MicroB) Brainstem Lesions - Dr. Bravo (Nico Castillo)miguel cuevas100% (1)
- Amyl Oidos IsDocument13 pagesAmyl Oidos IsJose Joey Jumaoas Jr.No ratings yet
- Nanomedicine: A Promising Way To Manage Alzheimer's DiseaseDocument20 pagesNanomedicine: A Promising Way To Manage Alzheimer's Diseasesara salamaNo ratings yet
- Jpad 2023 30Document16 pagesJpad 2023 30Dr. Stan Wardel BA, MA, MChem, MBA, DPhil, DSc.No ratings yet
- Endocrine Anatomy 4Document16 pagesEndocrine Anatomy 4Snehal JayaramNo ratings yet
- SchizopDocument43 pagesSchizopapi-548578435No ratings yet
- ParkinsonDiseaseFarter2017Document103 pagesParkinsonDiseaseFarter2017DISKA YUNIAROHIMNo ratings yet
- DIT Pharmacology MnemonicsDocument5 pagesDIT Pharmacology MnemonicsqiqizNo ratings yet
- Safety and Tolerability of BAN2401 - A Clinical Study in Alzheimer's Disease With a Protofibril Selective Aβ AntibodyDocument10 pagesSafety and Tolerability of BAN2401 - A Clinical Study in Alzheimer's Disease With a Protofibril Selective Aβ AntibodyPau Fer Mujica CNo ratings yet
- Kathynotes PDFDocument103 pagesKathynotes PDFvarrakeshNo ratings yet
- Journal MDPI Role Oxidative Damage in Alzheimer DiseasesDocument22 pagesJournal MDPI Role Oxidative Damage in Alzheimer Diseaseswisang geniNo ratings yet
- Amyloid-β in Alzheimer's Disease: Effects on Disease Pathogenesis and Recent Advances in Clinical TrialsDocument8 pagesAmyloid-β in Alzheimer's Disease: Effects on Disease Pathogenesis and Recent Advances in Clinical TrialsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Disorders of The Brainstem and Cranial Nerves SY 2022-2023Document141 pagesDisorders of The Brainstem and Cranial Nerves SY 2022-2023Geraldine Teopy100% (1)
- Pa Ears-Nose-MouthDocument108 pagesPa Ears-Nose-MouthDenniellePaulineKwonNo ratings yet
- Approach To A Case of Respiratoey SystemDocument105 pagesApproach To A Case of Respiratoey SystemprashuNo ratings yet
- Alzheimer 'S Disease Profiled by Uid and Imaging Markers: Tau PET Best Predicts Cognitive DeclineDocument11 pagesAlzheimer 'S Disease Profiled by Uid and Imaging Markers: Tau PET Best Predicts Cognitive DeclineChouaib OujhainNo ratings yet
- Neurology: Timothy E. Welty, Pharm.D., FCCP, BCPSDocument68 pagesNeurology: Timothy E. Welty, Pharm.D., FCCP, BCPSAlmaha AlfakhriNo ratings yet
- GI BLEED - Medicine - Internal MedicineDocument11 pagesGI BLEED - Medicine - Internal Medicinezezma GamingNo ratings yet
- Chest X-RayDocument39 pagesChest X-Rayendah cahya sufianyNo ratings yet
- Rosh NeuroDocument11 pagesRosh NeuroSoni AliNo ratings yet
- Integrated Therapeutics-Ii For 3 Year STS: Chapter-1Document69 pagesIntegrated Therapeutics-Ii For 3 Year STS: Chapter-1Geleta GalataaNo ratings yet
- Optimal Anti-Amyloid-beta Therapy For AlzheimersDocument19 pagesOptimal Anti-Amyloid-beta Therapy For AlzheimersCarolina RibeiroNo ratings yet
- New Molecular Targets For PET and SPECT Imaging in Neurodegenerative DiseasesDocument12 pagesNew Molecular Targets For PET and SPECT Imaging in Neurodegenerative DiseasesMihaela ToaderNo ratings yet
- PDR 2020Document1 pagePDR 2020api-506024957No ratings yet
- Reproductive PhysiologyDocument122 pagesReproductive PhysiologyShashwat GaurNo ratings yet
- CNS Pathology Course: - Recommended TextbookDocument39 pagesCNS Pathology Course: - Recommended TextbookchinnnababuNo ratings yet
- Uworld DermatDocument64 pagesUworld DermatRatnam hospitalNo ratings yet
- Concept AnalysisDocument18 pagesConcept AnalysisRolan MangiwetNo ratings yet
- 00 Chest NotesDocument38 pages00 Chest NotesENINE RESTAURANT CompanyNo ratings yet
- Review To CNS Radiology Including SSDocument52 pagesReview To CNS Radiology Including SSBisher Al-halabiNo ratings yet
- Clinical Neurology Answers OnlyDocument68 pagesClinical Neurology Answers Onlyanas kNo ratings yet
- Therapeutic Hypothermia - Principles, Indications, Practical ApplicationFrom EverandTherapeutic Hypothermia - Principles, Indications, Practical ApplicationNo ratings yet
- 1.MSE Part 1Document9 pages1.MSE Part 1sisqaNo ratings yet
- 3M 9105 Wear It Right Poster PDFDocument2 pages3M 9105 Wear It Right Poster PDFScott KramerNo ratings yet
- Warm Vs Cold ShockDocument8 pagesWarm Vs Cold ShockmarleeramirezNo ratings yet
- Assignment No. 1Document1 pageAssignment No. 1Clau MagahisNo ratings yet
- Mini-OSCE Internal PicturesDocument108 pagesMini-OSCE Internal PicturesCheru TadesseNo ratings yet
- Day 4 Special NeedsDocument8 pagesDay 4 Special NeedsRidwan OlivaNo ratings yet
- Class II Cavity Preparation - 2Document28 pagesClass II Cavity Preparation - 2Tarteel MagdiNo ratings yet
- TNCCDocument15 pagesTNCCmarkkerwinNo ratings yet
- 10 4292@wjgpt v8 I1 26Document14 pages10 4292@wjgpt v8 I1 26Syawal PratamaNo ratings yet
- Department of General Practice - Family MedicineDocument122 pagesDepartment of General Practice - Family Medicinesteven hkNo ratings yet
- Quiz Bee Level I EasyDocument22 pagesQuiz Bee Level I EasyLaica A. LunetaNo ratings yet
- Tannery and Tobacco Workers in Bangladesh - Mansib Yaman AzamDocument15 pagesTannery and Tobacco Workers in Bangladesh - Mansib Yaman AzamMansib YamanNo ratings yet
- p2 CHN ReviewerDocument9 pagesp2 CHN Revieweruzca.gurbuxani.swuNo ratings yet
- 11-English-Practice Book Full Guide by Brilliant Publication's Way To Centum in English-Cell 9443663752Document98 pages11-English-Practice Book Full Guide by Brilliant Publication's Way To Centum in English-Cell 9443663752Balaji DeeviNo ratings yet
- Urinary Tract Infection PIAG 84Document3 pagesUrinary Tract Infection PIAG 84madimadi11No ratings yet
- Laporan Bulanan Surveilans Kasus PTM 2019Document144 pagesLaporan Bulanan Surveilans Kasus PTM 2019ROYALNo ratings yet
- Glaucoma, Cataract, Otitis Lippincot Questions-1Document3 pagesGlaucoma, Cataract, Otitis Lippincot Questions-1Rammy KhanNo ratings yet
- LC459 CW1 SOH (Jubair) (Feedback)Document10 pagesLC459 CW1 SOH (Jubair) (Feedback)Death StrokeNo ratings yet
- Dewantoro, Kurniawan. Acceptance and Commitment Therapy Untuk Meningkatkan Acceptance of Illnes Pasien Positif HivDocument16 pagesDewantoro, Kurniawan. Acceptance and Commitment Therapy Untuk Meningkatkan Acceptance of Illnes Pasien Positif HivgitatungawiNo ratings yet
- Day 2 Training PlanningDocument106 pagesDay 2 Training PlanningVijay BhaskarNo ratings yet
- CNS and ANSDocument36 pagesCNS and ANSLEBADISOS KATE PRINCESSNo ratings yet
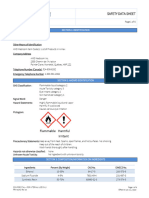
- Varnish Fluoride Sds 2Document6 pagesVarnish Fluoride Sds 2api-736239240No ratings yet
- NCM 114 Unit 1 To 4 GeriaDocument85 pagesNCM 114 Unit 1 To 4 GeriaJohn Van Dave Taturo100% (1)
- Charaka Samhitha Critical ReviewDocument3 pagesCharaka Samhitha Critical ReviewSamhitha Ayurvedic ChennaiNo ratings yet
- Internship Report (747) 5Document32 pagesInternship Report (747) 5indian meme templatesNo ratings yet
- BPT PDFDocument206 pagesBPT PDFQwertNo ratings yet
- Group Activity (Prenatal Assessment Form)Document8 pagesGroup Activity (Prenatal Assessment Form)The Mortal HowlerNo ratings yet
- Lymphocyte - WikiDocument6 pagesLymphocyte - Wiki12F 24 Renu SinghNo ratings yet
- Makalah Kel 2 Bhs. InggrisDocument15 pagesMakalah Kel 2 Bhs. Inggriswardi irmahNo ratings yet