Acid Base and Electrolyte Balance
Acid Base and Electrolyte Balance
Uploaded by
Muhammad Hamza AlviCopyright:
Available Formats
Acid Base and Electrolyte Balance
Acid Base and Electrolyte Balance
Uploaded by
Muhammad Hamza AlviCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Acid Base and Electrolyte Balance
Acid Base and Electrolyte Balance
Uploaded by
Muhammad Hamza AlviCopyright:
Available Formats
ACID BASE AND ELECTROLYTE BALANCE Some blood gas analyzers correct for the patient's body Normal
rect for the patient's body Normal Acid/Base Mechanisms
temperature. These corrections can significantly alter the To use acid-base lab data clinically, you must have a basic
Suggested Reading results so it’s good to record (or remember!) the patient’s understanding of some physiological mechanisms. If you have
Stockham and Scott, Fundamentals of Veterinary Clinical Pathology: body temperature at the time the sample is taken. forgotten these, you can review your Physiology notes or text, or
Chapter 9-10, pp 337-400 - read the suggested readings for this section.
The pH, PO2, and PCO2 are measured directly. The HCO3
Latimer, Mahaffey, and Prasse, Veterinary Laboratory Medicine: The following few points are those that you need to remember
Chapter 5, pp.136-161, cases 6,18, 22, 23, 24. (bicarbonate) can be either measured or calculated using a as you go through cases and interpret the lab values given for each
Additional Reading nomogram or the Henderson-Hasselbach equation: patient.
Thrall, MA. Veterinary Hematology and Clinical Chemistry, By definition, pH is related only to [H+].
Chapter 22, pp 329-353 pH = 6.1 +log [HCO3-] Buffer systems exist to minimize changes in pH as H+ ions are
PCO2 (0.03) produced during metabolism.
Objectives NOTE: Do not memorize the Henderson-Hasselbach equation There are many important buffer systems in the body. The most
At the end of this section, you should be able to: unless you just can’t help yourself. I can almost 100% guarantee you important to know for clinical evaluation is the
Describe the correct procedure for collecting a sample for blood that you will never have to do this calculation while diagnosing or bicarbonate/carbonic acid system:
gas analysis. treating a patient. On the other hand, it’s good to review physiology,
List the 4 major types of acid base abnormalities and their right? -
H+ + HCO3 Û H2CO3 Û H2O + CO2
primary causes.
When given acid base data, describe the existing acid base Results bicarbonate carbonic acid
abnormalities and determine if there is a compensatory The following information is given in a blood gas (acid base)
response. analysis: This buffer system is important because it allows the body to control
Describe the traditional versus nontraditional approach to acid- pH: measure of [H+] different components of the equation to help maintain H+ balance.
base analysis. PO2: partial pressure of oxygen in blood (in mm Hg)
Describe the clinical disorders that can lead to alterations in a PCO2: partial pressure of carbon dioxide in blood (in mm Hg) bicarbonate carbonic acid
given electrolyte. - -
HCO3 : bicarbonate concentration of blood (mEq/L) H + HCO3 Û H2CO3 Û H2O + CO2
+
Contrast the anion gap to the osmolal gap. metabolic control respiratory control
TCO2: total carbon dioxide (mEq/L)
ACID- BASE BALANCE TCO2 is a good estimate of the concentration of bicarbonate,
The respiratory system can control [CO2] by hyperventilation or
The goal of this section is for you to be able to diagnostically which comprises about 96% of TCO2. The other 4% consists
hypoventilation.
evaluate acid/base changes. This includes 2 things: of H2CO3 and CO2. TCO2 is measured by the blood gas
machine but can also be measured in the field or in- Increased [CO2] will shift the equilibrium of the equation to the
First, you should be able to classify the changes present in the left and result in increased [H+] and acidosis.
results of an acid base analysis (e.g. "this animal has a house laboratories from plasma or serum . TCO2 is stable
and does not have to be measured immediately nor kept on Decreased [CO2] will shift equilibrium to the right and cause
titrational metabolic acidosis"). decreased [H+] and alkalosis.
Second, having classified the changes, you should be able to list ice. Keep in mind that TCO2 is only an estimate of the bicarb
concentration and doesn’t really give you the full blood gas -
possible causes of the particular problem present. The kidneys (metabolic system) can control [HCO3 ] and [H+}by
picture. excretion into or reabsorption from the urine.
Sample Collection O2 Sat: O2 saturation; the % of Hgb that is oxygenated
Venous or arterial blood can be used, but only arterial blood can Base excess: "actual" bicarbonate concentration minus "normal" The traditional approach to acid base balance, using pH,
be used for interpreting PO2. Venous blood is OK for pH, bicarbonate concentration (+) results are base excess; (-) -
PCO2, and HCO3 to describe abnormalities, is a simplified approach
- results are really a base deficit, though they're often reported
HCO3 and PCO2 and is the sample most commonly used to for looking at a very complex system. Other variables, such as
as a negative base excess. A base deficit means there is too
evaluate acid base status (because it’s easier to get). electrolyte and protein concentrations, can also affect the body pH.
little bicarbonate in the blood whereas a base excess means
Blood should be collected directly into a heparinized syringe; We’ll talk later about other approaches to acid base balance that take
there is too much. This information is used in determining
using 0.2 ml of heparin (1000 units/ml)for each 2-3 mls of into account more variables.
the amount of HCO - to give to an acidotic animal. The
3
blood. Hand held instruments such as the i-STAT analyzer®
following are the "classic" normals. There is actually a range Primary Acid-Base Abnormalities and Compensation
may use non-anticoagulated blood.
of normals for each parameter for each species. You can use Four basic primary abnormalities can occur.
It’s important not to get room air into the sample. Once the blood these "classic" normals in interpreting problems. -
is drawn, cap the syringe with a rubber stopper. Be sure no Metabolic acidosis ¯pH, ¯[HCO3 ]
air bubbles are present. Room air has a high O2 and low CO2 NORMAL ARTERIAL VENOUS -
Metabolic alkalosis pH, [HCO3 ] Any combination of these
content compared to blood and an air bubble or any exposure pH 7.4 7.4
may also occur.
to room air will alter PO2 and PCO2 measurements. Samples PCO2 (mm Hg) 40 45
should go immediately to the lab and be run within 30 Respiratory acidosis ¯pH, PCO2
PO2 (mm Hg) 90-100 40-60 Respiratory alkalosis pH,¯ PCO2
minutes. Samples can be held for 3 hours in an ice bath. Bicarbonate (mEq/L) 24 24
O2 sat (%) 95-100 40-70
Acid Base and Electrolyte Ballance 1
When a primary abnormality occurs in one system, an opposite Metabolic acidosis mixed metabolic acidosis and respiratory acidosis, because of the
compensatory response can occur in the other system. THE BODY - inadequate respiratory compensation.
For each 1 mEq/L in HCO3 PCO2 by 0.7 mm Hg
WILL NEVER OVER-COMPENSATE! If the PCO2 had been 12 mm Hg (lower than what was
Metabolic alkalosis
-
predicted, or a change in the alkaline direction), the patient would
For example: For each 1 mEq/L in HCO3 PCO2 by 0.7 mm Hg have a mixed metabolic acidosis and respiratory alkalosis, since the
A metabolic acidosis will stimulate hyperventilation in the Respiratory acidosis body never over-compensates.
respiratory system. This will ¯PCO2 and hence, ¯ [H+], o Acute
helping to return the pH to normal. For each 1 mm Hg in PCO2
-
HCO3 by 0.15 mEq/L
Causes of metabolic acidosis
A metabolic alkalosis will cause hypoventilation and an in o Chronic -
There are two basic mechanisms for decreased [HCO3 ]:
PCO2. This will cause an in [H+] by shifting the equilibrium - 1. Loss of bicarbonate from the body
in the equation, and help return the pH to normal. For each 1 mm Hg in PCO2 HCO3 by 0.35 mEq/L
Respiratory alkalosis This is called secretional or hyperchloremic metabolic
o Acute acidosis and occurs any time a fluid rich in HCO3 is lost. Increased
In both of these examples, the changes in the respiratory renal reabsorption of chloride with hyperchloridemia is present in
system represent a compensation. Eventually correction will occur -
For each 1 mm Hg in PCO2 HCO3 by 0.25 mEq/L secretional metabolic acidosis in order to maintain electroneutrality.
when the primary cause for the metabolic acidosis or metabolic o Chronic Hypovolemia may also contribute to the hyperchloridemia.
- - Examples of bicarbonate rich fluids that may be lost include:
alkalosis is corrected and renal conservation or elimination of HCO3 For each 1 mm Hg in PCO2 HCO3 by 0.55 mEq/L
returns this parameter to normal. o Intestinal fluid - lost in diarrhea or trapped by GI
Although these formulas haven’t been established for other obstruction
More examples: species, you can use them to approximate a normal body response to o Saliva - especially in ruminants; animals that can't
A respiratory acidosis will stimulate renal excretion of H+ and an acid base imbalance. If the other system has not compensated swallow can lose HCO3 in salivary secretions
resorption of HCO3 – appropriately, a mixed metabolic/respiratory abnormality is present. o Urine - in a form of renal disease called renal
A respiratory alkalosis results in decreased H+ excretion and tubular acidosis, the kidneys are unable to
- Interpretation of Basic Acid Base Abnormalities -
decreased resorption of HCO3 . resorb HCO3 , leading to acidosis
In these cases, the renal response represents compensation. 2. Retention, generation, or ingestion of acid
1. METABOLIC ACIDOSIS This is called titrational metabolic acidosis. In this type
Correction would require removal of the respiratory lesion/pathology
that provoked the abnormality. of metabolic acidosis, the excess organic acid dissociates into H+ and
Example: 8 year old dog with diarrhea and dehydration for 3 days. A . Bicarbonate combines with and removes the H+ leaving the A-
-
An arterial sample for blood gas analysis is obtained. (anion or negative charge) in the body. The more H+ there is to be
Evaluation of Acid/Base Problems
We will look at how one goes about evaluating the four basic titrated/buffered, the more anion or negative charge there is built up.
Patient Normal Direction of Change
acid/base abnormalities and their combinations. Each will be
pH = 7.29 7.4 Acid Examples are:
introduced by the results of a blood gas analysis of a patient with the
PCO2 = 28 mm Hg 40 Alkaline o Lactic acid- produced in shock, grain overload, etc.
particular disorder. Remember that mixed abnormalities can occur!
-
HCO3 = 6 mEq/L 24 Acid o Keto acids- produced in diabetes and starvation
Interpretation, general steps: Step 1: A pH = 7.29 is a change in the acid direction, so we are o Uremic acids- acids such as SO4 and PO4 which are
1. First, determine the direction of the pH change dealing with an acidosis. normally cleared by the kidneys build up in uremia;
a. if pH > 7.4, there is an alkalosis Step 2: The respiratory system ( PCO2 = 28) is shifted in the BUN and creatinine will be increased
b. if pH < 7.4, there is an acidosis - o Exogenous toxins- eg. ethylene glycol, methanol,
2. Second, determine which system, respiratory (PCO2) or alkaline direction, and the metabolic system ( HCO3 = 6) is
shifted in the acid direction. The imbalance is therefore, a paraldehyde, salicylates
-
metabolic (HCO3 ) has shifted in the direction of the pH metabolic acidosis.
change. This determines which system the primary Step 3: Evaluate the respiratory compensatory response. For It’s important to determine if a metabolic acidosis is titrational or
abnormality is in. If both metabolic and respiratory - secretional (or both) because the possible causes are different. The
systems have shifted in the direction of the pH change, every 1 mEq/L decrease in HCO3 , there should be a 0.7 mm anion gap is used to make this differentiation, and to aid in diagnosis
then it is a mixed metabolic and respiratory problem. Hg decrease in PCO2. This should predict the PCO2 within 1- and treatment. Interpretation of the anion gap is based on the fact
3. Next, evaluate the compensatory response of the other 2 mm Hg. that titrational acidoses result in the production of large amounts of
system. The following table has been formulated for use unmeasured negative charges (anions). One mEq of acidic anions
in dogs. Use the “classic” normals given earlier when The predicted PCO2 is 27.4. The patient PCO2 of 28 is neutralizes 1.0 mEq of HCO3 and the anion that's left increases the
using these formulas. therefore an appropriate response and this is a simple metabolic anion gap 1.0 mEq.
acidosis.
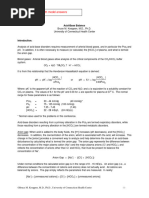
Expected Compensatory Response in Simple Acid-Base Suppose this patient's PCO2 had been 38 mm Hg. In that Organic acid HA ® H + + A -
Disturbances in Dogs case, the patient's PCO2 would be higher (a shift in the acid H ion unmeasured anion
direction) than the predicted PCO2. This patient would then have a
Disturbance Compensation
Acid Base and Electrolyte Ballance 2
This doesn't occur in secretional acidoses. The anion gap is used to - consists of fluid therapy with normal saline solution to
HCO3 = 38.4 24 Alkaline
detect the presence of the unmeasured anions in titrational acidoses. replace fluid volume and chloride and correction of the
The theory is that: Total (+ ) charges = Total (-) charges initiating cause.
Step 1: The pH is higher than normal, so this is an alkalosis.
[Na+] + [K+] + [UC+] = [HCO3-] + [Cl-] + [UA-]
Where [UC+] = unmeasured positive charges (cations) and [UA-] = Step 2: The metabolic system is shifted in the alkaline direction Summary of Metabolic Alkalosis
unmeasured negative charges (anions) and the respiratory system is shifted in the acid direction, -
therefore, this is a metabolic alkalosis. pH , HCO3
ß
Step 3: Evaluate the respiratory compensation. Compensation The PCO2 should increase as part of the compensatory response.
-
([Na+] + [K+] ) - ([HCO3 ] + [Cl-]) = [UA-] - [UC+] should consist of hypoventilation to CO2 and H+. However, History and physical exam are necessary to look for the source of
ß hypoxia can result during the hypoventilation and this can gastric fluid loss (vomiting) or sequestration (abomasal
- limit the ability of the mechanism to provide adequate displacement / impaction).
Anion Gap = ( [Na ] + [K ] ) - ( [HCO3 ] + [Cl ] ) = [UA-] -
+ + -
compensation. Treatment involves replacing fluid volume and Cl-.
[UC+ ]
If the canine compensation formula is used (recognizing that this has
In other words, the difference between the measured cations
not been validated for the cow), there should be a 0.7 mm Hg
-
(Na and K+) and the measured anions (Cl- and HCO3 ) is equal to
+
- - 3. RESPIRATORY ALKALOSIS
increase in PCO2 for each 1 mEq/L increase in HCO3 . The HCO3
the difference between unmeasured anions and unmeasured cations.
The unmeasured cations in the body are constant so any increase in has increased by 14.4 in this patient, so the PCO2 should increase by Example: 12 year old dog with congestive heart failure. An arterial
anion gap is due to unmeasured anions, i.e. organic acids. approximately 10. This cow has increased from a normal venous sample is taken.
The anion gap is normally: value of 45 mm Hg to 55 mm Hg, so compensation is adequate. The Patient Normal Direction of Change
limit of compensation for PCO2 is about 60 mm Hg. If the pCO2 is pH = 7.49 7.4 Alkaline
15-25 in dogs and cats greater than 60 mm Hg, there may be a mixed acid/base imbalance PCO2 = 24.4 40 Alkaline
10-20 in other species with a metabolic alkalosis and a respiratory acidosis. HCO3 = 16.2 24 Acid
PO2 = 82.1
An anion gap higher than the reference range indicates the If the PCO2 is low or normal (no response), a concurrent
presence of unmeasured negative charges (anions) and classifies a respiratory alkalosis exists. Step 1: The pH is elevated, so this is an alkalosis.
metabolic acidosis as titrational. Hyperchloridemia is not observed
Step 2: The respiratory system is shifted in the alkaline direction
with titrational metabolic acidosis unless hemoconcentration is Causes of Metabolic Alkalosis and the metabolic system is shifted in the acid direction,
present, since electroneutrality is maintained by the unmeasured The vast majority of cases of metabolic alkalosis are caused by therefore, this is a respiratory alkalosis.
anions, rather than retention of Cl-. Also, severe hypoproteinemia or loss of HCl from the stomach or abomasum. Loss of HCl is
hypoalbuminemia can decrease the anion gap, making interpretation Step 3: Evaluate the metabolic compensatory response.
-
more difficult and possibly masking any increase by organic acids. associated with an increase in HCO3 , and results in
metabolic alkalosis. This happens in vomiting, abomasal The response to a respiratory abnormality is broken into acute
Summary of Metabolic Acidosis displacement or impaction, and vagal indigestion. (buffers) and chronic (renal) responses. Acute responses can occur
- Hypochloridemia is present in these cases, because of the Cl- lost in minutes, chronic responses may take several days.
pH ¯, HCO3 ¯ or sequestered. Acute: In the acute buffer response, H+ is released from
In the dog, an appropriate respiratory compensation would be a The fact that Cl- is lost along with H+ is important. These intracellular phosphates and proteins and combines with
0.7 mm Hg decrease in PCO2 for every 1 mEq/L decrease in animals are usually hypovolemic because of fluid loss. - -
- HCO3 . This results in a decrease in HCO3 .
HCO3 . If the response is inadequate, a mixed acid-base Hypovolemia leads to renal resorption of Na+ in the Chronic: (>2-3 days) The chronic response represents ¯ renal
disturbance may be occurring. kidney to maintain blood pressure. excretion of H+. The retained H+ further reduces plasma
Calculate the anion gap to differentiate titrational ( AG) from When sodium is resorbed in the kidney, an anion must be -
secretional (normal AG) metabolic acidoses. resorbed or a different cation excreted along with it to HCO3 . This takes several days to occur.
Know causes of titrational and secretional acidoses. maintain electroneutrality. Normally, Cl- is the anion
resorbed, but since these animals are chloride deficient, Formulae:
Treatment of metabolic acidosis involves fluid replacement and
bicarbonate must be resorbed or H+ excreted instead. Either Acute: For every 1 mm Hg decrease in PCO2, HCO3 should
-
HCO3 replacement - decrease 0.25 mEq/L
one of these (HCO3 absorption or H+ excretion) worsens the -
alkalosis. e.g. If PCO2 is ¯ 20, HCO3 should ¯ 5 mEq/L
2. METABOLIC ALKALOSIS
A metabolic alkalosis with an acidic urine is referred to as -
If PCO2 is ¯ 30, HCO3 should ¯ 7.5 mEq/L
Example: 2 year old Jersey cow, recently calved, off feed. A paradoxical aciduria, and is common, for example, in Chronic: For every 1 mm Hg decrease in PCO2, HCO3 should
venous blood sample was taken for analysis. abomasal displacement in ruminants. decrease 0.55 mEq/L
Metabolic alkalosis can also occur from over-administration of In our example, the dog has a PCO2 of 24.4, representing
Patient Normal Direction of change bicarbonate containing fluids, such as lactated Ringer's a decrease of 15.6 mm Hg.
pH = 7.51 7.4 Alkaline solution, use of loop diuretics, such as furosemide, which lead Compensation would be:
PCO2 = 55 45 Acid to hypokalemia, and, rarely, low chloride intake. Treatment -
¯ of ~4 mEq/L ( 0.25 x 15.6 ) HCO3 if acute
Acid Base and Electrolyte Ballance 3
- Step 1: The pH is decreased, so this is an acidosis. PO2 is low unless the patient is on supplemental O2 (sample
or ¯ of ~ 8-9 mEq/L (0.55 x 15.6) HCO3 if chronic
Step 2: The respiratory component is also shifted in the acid arterial blood)
- direction so we are dealing with a respiratory acidosis. Look for cause of decreased gas exchange (e.g. thoracic
Therefore, the HCO3 should be in a range of 15-20 depending Step 3: Evaulate the metabolic compensatory response. radiographs, bronchoscopy).
on how long the process has been going on. The actual HCO3
of 16.2 represents an appropriate compensation. Had the As with respiratory alkalosis, you must determine if the problem is All the discussion thus far has used what some call a
- acute or chronic. “traditional” approach to acid base abnormalities. There are other
HCO3 been < 15, a concurrent metabolic acidosis would be
- ways of discussing and evaluating acid base. You will more than
present. Had the HCO3 been > 20, there would be a Formulae: If the canine formula is used, then the following will likely encounter clinicians of various types that will use these other
concurrent metabolic alkalosis. occur approaches. At that point, you will probably learn a lot more about
Based on the history, you must determine if the situation is - them. Here is a VERY brief summary.
acute or chronic. Acute: For each PCO2 increase of 1 mm Hg, HCO3 should increase
0.15 mEq/L. Nontraditional Approaches to Acid-Base Abnormalities
Causes of Respiratory Alkalosis -
Chronic: For each PCO2 increase of 1 mm Hg, HCO3 should The most common nontraditional approach to acid-base
Respiratory alkalosis is always due to hyperventilation. The increase 0.35 mEq/L. evaluation is Stewart’s quantitative approach.
hyperventilation can be due to: Stewart’s approach states that the pH is determined by 3
Extrathoracic causes. These include fever, pain, heat stroke, In this patient, the PCO2 is increased 40 mm Hg (from 40 to independent variables, including the PCO2, the strong ion
apprehension, and anemia. In these cases there will be a -
80). The HCO3 should go up 6 (to 30) if the situation is acute or 14 difference (SID), which is basically Na+ - Cl-, and total
normal PO2.
(to 38) if the situation is chronic. protein or albumin.
Intrathoracic causes. Pulmonary diseases resulting in
- With Stewart’s approach, a decrease in protein produces alkalosis
ventilation:perfusion abnormalities will result in hypoxia The response in this case (HCO3 = 29) is probably
and an increase in protein produces acidosis. A decrease in
which will stimulate hyperventilation. These pulmonary appropriate if the condition is acute, e.g. the result of anesthesia. If
the SID (such as with Cl- retention) causes an acidosis, and an
diseases may include pneumonia, pulmonary edema, -
the condition was chronic, an HCO3 of 29 would represent a increase in the SID (decrease in Cl-) produces an alkalosis.
pulmonary thromboembolism, pleural effusion, and thoracic
concurrent metabolic acidosis. Changes in PCO2 produce the same results seen with the
masses. They usually result in a ¯ PO2. Congestive heart
failure or cardiac diseases with right to left shunting can also traditional approach, with an increase in PCO2 producing a
Causes of Respiratory Acidosis
result in a respiratory alkalosis. respiratory acidosis, and a decrease in PCO2 causing a
Respiratory acidosis can be caused by anything that decreases
o Therefore, PO2 (using an arterial blood sample) can be used to
gas exchange across alveoli. respiratory alkalosis.
separate intrathoracic ( ¯ PO2) and extrathoracic ( normal
or PO2) causes of alkalosis. Examples include: In summary, acid-base balance in the body involves several
o Treatment of respiratory alkalosis requires treatment of \ the Severe pulmonary disease ( pneumonia, pulmonary edema, complex interactions, and different approaches have been developed
underlying problem; e.g. treat the pneumonia, cardiac emphysema) to aid in the understanding of this balance. For our purposes in this
medications, etc. CNS depression that decreases respiration (CNS disease or course, use the traditional approach to acid-base disorders, but
drugs) recognize that changes in electrolytes or protein can affect acid-base
Summary of Respiratory Alkalosis results and should also be considered.
Severe bloat or abdominal masses that decrease tidal volume due
pH, ¯ PCO2 to pressure on the diaphragm
Determine whether the process is acute or chronic and use the Pleural effusion
appropriate formula to evaluate the metabolic compensatory ELECTROLYTE BALANCE
Neuromuscular disorders
response. -
Use arterial PO2 to distinguish intrathoracic from extrathoracic Serum electrolytes include Na+, K+, Cl-, and HCO3 . In
Basically, anything that causes an intrathoracic respiratory alkalosis this next section, we’ll discuss what clinical situations lead to
causes. will cause a respiratory acidosis when it becomes severe enough that
Evaluate patient's thoracic cavity, emotional state, PCV and Hgb changes of these electrolytes.
CO2 can no longer cross the alveoli.
to determine causes. O2 is usually low in respiratory acidosis ( PO2 determined on arterial Sample Collection
blood) unless the animal is breathing supplemental oxygen, for Serum is the best sample for electrolyte determinations.
4. RESPIRATORY ACIDOSIS example, during anesthesia. Heparinized plasma can also be used when electrolytes need to be
Treatment involves correcting the underlying problem. Bicarbonate evaluated rapidly. Hemolysis and lipemia can interfere with
Example: 2 year old Quarter Horse with severe colic. Arterial blood supplementation is usually not very effective.
taken after induction of anesthesia for laparotomy. electrolyte assays.
Patient Normal Direction of Changes Summary of Respiratory Acidosis
pH = 7.15 7.4 Acid SODIUM
¯ pH, PCO2
pCO2 = 80 40 Acid
Sodium is the major cation of the extracellular fluid (plasma).
Assess whether the problem is acute or chronic and use the It is the major ion that determines plasma osmolality. Control of
HCO3 = 29 24 Alkaline appropriate formula to evaluate compensation. sodium concentration is regulated by:
Acid Base and Electrolyte Ballance 4
Aldosterone, which promotes renal reabsorption of sodium, and Potassium is the major intracellular cation. Potassium levels Dietary K+ deficiency. This is rarely a primary cause of
potassium excretion must be maintained in a narrow range for normal cardiac and hypokalemia, but may contribute to hypokalemia in anorectic
Atrial natriuretic factor, which promotes renal sodium excretion, neuromuscular function to occur. Most potassium is present animals, especially herbivores.
and intracellularly and shifting of K+ in and out of cells is one Hyperadrenocorticism. Leading to excessive urinary loss of K+.
Antidiuretic hormone, which promotes renal conservation of mechanism of maintaining serum K+ levels. Serum K+ is, therefore, Alkalosis. During alkalosis, H+ ions shift outside the cells to
water. not a reliable indicator of total body K+. minimize pH shift. K+ ions move into the cells to maintain
Serum potassium concentration is influenced most by diet, electroneutrality. This can also occur with rapid correction of
Causes of Hypernatremia renal excretion (with aldosterone promoting K+ excretion), and acidosis in patients when K+ moves back into the cells.
Usually the result of dehydration. Must have loss of H2O without intracellular/extracellular shifting. Insulin therapy. Because of total body K+ deficiency,
loss of Na+, i.e. hypotonic water loss. An example of a hypokalemia often follows insulin therapy since insulin
disease in which this can occur is diabetes insipidus. Causes of Hyperkalemia facilitates K+ entry into the cells.
Salt poisoning, i.e. a diet rich in sodium with limited access to Decreased glomerular filtration or urinary obstruction. Most False decreases in [K+] with lipemia or hyperproteinemia. See
water. excess K+ is excreted in the urine. Prerenal, renal, or explanation under hyponatremia.
Primary adipsia (rare) postrenal azotemia are often accompanied by increased [K+].
Hyperadrenocorticism (may cause a slight hypernatremia) Hypoadrenocorticism. Elevated K+ levels are common in CHLORIDE
Addison's disease. Chloride is the major anion of the extracellular fluid.
Causes of Hyponatremia Acidosis. During acidosis, H+ ions shift intracellularly to Typically, it changes along with Na+ to maintain electroneutrality.
Almost always associated with loss of Na rich fluids.
+ minimize pH change. K+ ions move extracellularly to Three major changes in Cl- which are unrelated to Na+ changes
Hypoadrenocorticism (Addison's disease). Na+ is lost in the maintain electroneutrality. Upon correction of the acidosis, are:
urine. Usually K is elevated as well. The Na :K ratio is
+ + + the H+ ions move back out of the cells and K+ ions move back Hypochloridemia in metabolic alkalosis. Cl- is lost with gastric
normally > 26:1. A ratio of < 23: 1 is suggestive of Addison's in. This may occur more in secretional metabolic acidosis or abomasal fluids.
disease. than in titrational metabolic acidosis. Hyperchloridemia in secretional metabolic acidosis. Cl- increases
Diarrhea. Especially in horses, severe diarrhea can result in Na + Tissue necrosis or altered membrane permeability. Intracellular -
[K+] is significantly higher than plasma [K+]. Necrosis of to replace the lost HCO3 and maintains electroneutrality.
loss.
cells allows release of K+ and may lead to hyperkalemia. Hyperchloridemia with K bromide therapy due to interference of
+
Renal disease. Na+ is freely filtered in the glomerulus, and most bromide with Cl- assay.
is normally reabsorbed in the proximal tubules. Na wasting
+ Insulin deficiency. Insulin facilitates K+ entry into cells.
can occur in tubular disease. Clinically, this doesn't usually result in hyperkalemia in
diabetics because renal excretion of K+ usually maintains low BICARBONATE
Dietary salt deficiency.
or normal [K+] in the blood. Because there is a total body K+
Treatment with low Na+ fluids. For example, 5% dextrose in Bicarbonate is the second most prominent anion of the blood.
deficiency, hypokalemia may then follow insulin therapy in
H2O. Changes in bicarbonate were described in the acid/base section of
diabetes mellitus. Insulin (plus glucose) is used clinically to
Diabetes mellitus. Hyperglycemia ® hyperosmolality ® fluid reduce serum [K+] in hyperkalemia due to other causes. these notes.
shifts with Na dilution. This may occur if blood glucose is ³ Hemolysis. The pig, horse, cow and some dog breeds (eg.,
+
500 mg/dl. Akitas) have high concentrations of potassium in their red OSMOLALITY
Third space loss- e.g. displaced abomasums in ruminants. This is blood cells. Osmolality is determined by the number of particles in solution.
associated with loss of H and Cl into a space that is neither Marked thrombocytosis. May cause pseudohyperkalemia when
+ -
It has no relationship to particle size or molecular weight,
the intracellular nor the extracellular fluid compartment. platelets release K+ into the serum. only to the number of particles. Because of this, small
Artifact Parenteral administration of K+. molecules that are present in high concentrations, such as Na+,
Hyperkalemic periodic paralysis in horses. are more significant in determining plasma osmolality and
False decreases in [Na+] occur with lipemia or osmotic pressure than are large molecules present in low
Use of K3EDTA as the anticoagulant. This is artifactual
hyperproteinemia when techniques using diluted samples (flame numbers, such as proteins.
hyperkalemia.
photometer, some ion specific electrodes) are used for [Na+] Na+ is the major determinant of plasma osmolality. Osmotic
determination. Serum consists of an aqueous phase normally about forces control the shifts of water from intracellular to
Causes of Hypokalemia
96%) and non-aqueous phase (about 4%). Na+ is distributed only in extracellular spaces as well as the retention and/or loss of
the aqueous phase. Instruments using diluted samples measure the Excessive gastrointestinal losses. This may include vomiting and
diarrhea. fluid from the body. Since Na+ is the major determinant of
total amount of Na+ present in a total volume of serum rather than osmolality in the body and since water passively follows
the amount in just the aqueous phase. Any process that increases the Excessive urinary losses. This may occur secondary to osmotic
diuresis as in diabetes mellitus, or diuretic therapy. There is a osmotic gradients, control of body water is related to control
nonaqueous phase of serum, such as lipemia or hyperproteinemia, of body [Na+].
will reduce the [Na+] in serum although the [Na+] in the aqueous syndrome in cats in which there is increased urinary K+ loss
in association with chronic metabolic acidosis. The clinical Plasma osmolality can be measured using an osmometer. It can
phase is normal.
signs that result are often characterized by a polymyopathy. also be estimated based on serum concentrations of the most
Also- cats with chronic renal failure don’t seem to regulate numerous osmoles, which are Na+, K+, BUN and glucose.
POTASSIUM
their GI and renal potassium metabolism well. The formula for estimating plasma osmolality is:
o Osmolality (mOsm/kg) =
Acid Base and Electrolyte Ballance 5
2 ( Na+ + K+ ) + ( Glucose ) + ( BUN)
18 2.4
o Glucose and BUN are measured in mg/dl; Na+ and K+ are
measured in mEq/L.
Typically osmolality » 280-310 mOsm/kg. Reference ranges
should be established by each lab.
The osmolal gap is the difference between the actual plasma
osmolality (measured) and thecalculated osmolality.
A normal osmolal gap is < 10 for dogs, < 15 for cattle, and < 7
for horses.
An osmolal gap of >10 in a dog is indicative of an osmotically
active molecule in the plasma other than the factors in the
osmolality equation. Ethylene glycol, lactate, ketones, uremic
acids, salicylates, methanol, and mannitol can all produce an
osmolal gap. Although this is not commonly done, following
the changes in the osmolal gap would be one way of
monitoring elimination of ethylene glycol in a patient being
treated for ethylene glycol toxicity.
Hyperproteinemia and hyperlipidemia can cause decreased serum
H2O content and result in false hyponatremia with an
increased osmolar gap (see discussion of false hyponatremia
in electrolyte section of these notes).
Acid Base and Electrolyte Ballance 6
You might also like
- Traditional Acid-Base Analysis: Kate HopperNo ratings yetTraditional Acid-Base Analysis: Kate Hopper7 pages
- Review Article: Sodium Bicarbonate Therapy in Patients With Metabolic AcidosisNo ratings yetReview Article: Sodium Bicarbonate Therapy in Patients With Metabolic Acidosis14 pages
- Acid-Base (Anesthesia Text) - OpenAnesthesiaNo ratings yetAcid-Base (Anesthesia Text) - OpenAnesthesia12 pages
- How To Interpret Arterial Blood Gas Data?No ratings yetHow To Interpret Arterial Blood Gas Data?7 pages
- Blood Gas Analysis: Respiratory DisordersNo ratings yetBlood Gas Analysis: Respiratory Disorders15 pages
- Acid-Base Principles and Practical Interpretation in Small Animals - WSAVA2005 - VINNo ratings yetAcid-Base Principles and Practical Interpretation in Small Animals - WSAVA2005 - VIN9 pages
- Clinical_Approach_to_Assessing_Acid_Base_Status_Physiological_vsNo ratings yetClinical_Approach_to_Assessing_Acid_Base_Status_Physiological_vs12 pages
- Blood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSINo ratings yetBlood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSI39 pages
- Arterial Blood Gases: Laboratory InsightsNo ratings yetArterial Blood Gases: Laboratory Insights9 pages
- Uia 16 Acid Base Balance and Interpretation of Blood Gas ResultsNo ratings yetUia 16 Acid Base Balance and Interpretation of Blood Gas Results4 pages
- Case 27: What Is The Response of The Kidney To Metabolic Acidosis?No ratings yetCase 27: What Is The Response of The Kidney To Metabolic Acidosis?10 pages
- Understanding Base Excess (BE) : Merits and PitfallsNo ratings yetUnderstanding Base Excess (BE) : Merits and Pitfalls4 pages
- The Stewart Approach - One Clinician's Perspective+++No ratings yetThe Stewart Approach - One Clinician's Perspective+++14 pages
- A Stepwise Approach To Acid Base Disorders in ICU100% (3)A Stepwise Approach To Acid Base Disorders in ICU71 pages
- Parasitic Problems and Their Control in EquinesNo ratings yetParasitic Problems and Their Control in Equines63 pages
- Strangles: Distemper, Infectious Adenitis Strept ThroatNo ratings yetStrangles: Distemper, Infectious Adenitis Strept Throat21 pages
- Prediction of Stroke Using Machine Learning: June 2020No ratings yetPrediction of Stroke Using Machine Learning: June 202010 pages
- Hemostasis, Surgical Bleeding and TransfusionNo ratings yetHemostasis, Surgical Bleeding and Transfusion10 pages
- Human Anatomy and Physiology Chapter 6 Lymphatic System PDF Notes by NoteskartsNo ratings yetHuman Anatomy and Physiology Chapter 6 Lymphatic System PDF Notes by Noteskarts6 pages
- Thyroid Hormones - Analogues and InhibitorsNo ratings yetThyroid Hormones - Analogues and Inhibitors17 pages
- d4 Medical Examiner Report For A Lorry or Bus Driving LicenceNo ratings yetd4 Medical Examiner Report For A Lorry or Bus Driving Licence8 pages
- COAPT A Randomized Trial of Transcatheter Mitral ValveNo ratings yetCOAPT A Randomized Trial of Transcatheter Mitral Valve1 page
- Test Bank For Medical Terminology Simplified: A Programmed Learning Approach by Body System, 5th Edition Barbara A. Gylys Regina M. Masters100% (3)Test Bank For Medical Terminology Simplified: A Programmed Learning Approach by Body System, 5th Edition Barbara A. Gylys Regina M. Masters49 pages
- Drugs Study of Omeprazole, Metoclopramide Etc75% (4)Drugs Study of Omeprazole, Metoclopramide Etc12 pages
- Venous Thrombosis and Embolism Prevention and ManagementNo ratings yetVenous Thrombosis and Embolism Prevention and Management39 pages
- Ecg Stemi: Sequence of Changes in Evolving STEMINo ratings yetEcg Stemi: Sequence of Changes in Evolving STEMI3 pages
- Beck, David E. - Kann, Brian R. - Margolin, David A. - Vargas, H. David - Whitlow, Charles B - Improving Outcomes in Colon and Rectal Surgery (2019, CRC Press - Taylor & Francis Group)100% (2)Beck, David E. - Kann, Brian R. - Margolin, David A. - Vargas, H. David - Whitlow, Charles B - Improving Outcomes in Colon and Rectal Surgery (2019, CRC Press - Taylor & Francis Group)441 pages
- Arterial Blood Gas Analysis - making it easyFrom EverandArterial Blood Gas Analysis - making it easy
- Review Article: Sodium Bicarbonate Therapy in Patients With Metabolic AcidosisReview Article: Sodium Bicarbonate Therapy in Patients With Metabolic Acidosis
- Acid-Base Principles and Practical Interpretation in Small Animals - WSAVA2005 - VINAcid-Base Principles and Practical Interpretation in Small Animals - WSAVA2005 - VIN
- Clinical_Approach_to_Assessing_Acid_Base_Status_Physiological_vsClinical_Approach_to_Assessing_Acid_Base_Status_Physiological_vs
- Blood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIBlood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSI
- Uia 16 Acid Base Balance and Interpretation of Blood Gas ResultsUia 16 Acid Base Balance and Interpretation of Blood Gas Results
- Case 27: What Is The Response of The Kidney To Metabolic Acidosis?Case 27: What Is The Response of The Kidney To Metabolic Acidosis?
- Understanding Base Excess (BE) : Merits and PitfallsUnderstanding Base Excess (BE) : Merits and Pitfalls
- The Stewart Approach - One Clinician's Perspective+++The Stewart Approach - One Clinician's Perspective+++
- Strangles: Distemper, Infectious Adenitis Strept ThroatStrangles: Distemper, Infectious Adenitis Strept Throat
- Prediction of Stroke Using Machine Learning: June 2020Prediction of Stroke Using Machine Learning: June 2020
- Human Anatomy and Physiology Chapter 6 Lymphatic System PDF Notes by NoteskartsHuman Anatomy and Physiology Chapter 6 Lymphatic System PDF Notes by Noteskarts
- d4 Medical Examiner Report For A Lorry or Bus Driving Licenced4 Medical Examiner Report For A Lorry or Bus Driving Licence
- COAPT A Randomized Trial of Transcatheter Mitral ValveCOAPT A Randomized Trial of Transcatheter Mitral Valve
- Test Bank For Medical Terminology Simplified: A Programmed Learning Approach by Body System, 5th Edition Barbara A. Gylys Regina M. MastersTest Bank For Medical Terminology Simplified: A Programmed Learning Approach by Body System, 5th Edition Barbara A. Gylys Regina M. Masters
- Venous Thrombosis and Embolism Prevention and ManagementVenous Thrombosis and Embolism Prevention and Management
- Beck, David E. - Kann, Brian R. - Margolin, David A. - Vargas, H. David - Whitlow, Charles B - Improving Outcomes in Colon and Rectal Surgery (2019, CRC Press - Taylor & Francis Group)Beck, David E. - Kann, Brian R. - Margolin, David A. - Vargas, H. David - Whitlow, Charles B - Improving Outcomes in Colon and Rectal Surgery (2019, CRC Press - Taylor & Francis Group)