HIE and CVS
HIE and CVS
Uploaded by
akshayajainaCopyright:
Available Formats
HIE and CVS
HIE and CVS
Uploaded by
akshayajainaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
HIE and CVS
HIE and CVS
Uploaded by
akshayajainaCopyright:
Available Formats
THE JOURNAL OF PEDIATRICS • www.jpeds.
com MEDICAL
PROGRESS
Hypoxic-Ischemic Encephalopathy and Therapeutic Hypothermia:
The Hemodynamic Perspective
Regan E. Giesinger, MD, FRCPC1,2, Liane J. Bailey, BScH3, Poorva Deshpande, MBBS, MRCPCH1,2, and
Patrick J. McNamara, MB, BCh, BAO, DCH, MSc, MRCP, MRCPCH1,2,4
H
ypoxic-ischemic encephalopathy (HIE) is a severe to intervention may decrease the effectiveness of neuroprotective
central nervous system injury in neonates secondary strategies by compromising vital organ perfusion and
to perinatal asphyxia. It may cause devastating life- metabolism.
long neurocognitive impairments including cerebral palsy. The
introduction of therapeutic hypothermia (TH) as standard
therapy for neonates >36 weeks gestational age with HIE has Biophysiologic Effects of Asphyxia
improved patient outcomes and is supported by evidence from
both animal studies and large-scale clinical trials in humans. Direct Cardiovascular Effects of Asphyxia
TH has been shown to produce clinically important improve- The cardiovascular consequences of a hypoxic-ischemic insult
ments in both neonatal mortality (number needed to treat = 11) are broad and complex. Both the primary insult and ongoing
and neurodevelopmental impairment in survivors (number central nervous system redistribution of blood flow lead to
needed to treat = 8) in patients with moderate or severe reduced myocardial perfusion and resultant papillary muscle
encephalopathy.1 Although this intervention is the standard and subendocardial tissue ischemia.4 The neonatal heart is
of care in many institutions, the rates of death or uniquely vulnerable to ischemic injury because of relative im-
neurodevelopmental impairment are approximately 45%- maturity of transverse tubular architecture and lack of devel-
55% despite optimal application of TH1; reasons for this opment of the excitation-contraction coupling of the
disparity remain elusive. The relative contribution of hemo- cardiomyocyte.5 In addition, hypoxia upregulates a variety of
dynamic instability or treatment for it to the injurious process molecular pathways that lead to decreased myocardial
remains poorly understood; most clinicians “feel” a compul- contractility.6 Transient myocardial ischemia, which may or may
sion to treat presumed low blood pressure or low cardiac output not be symptomatic, occurs in one-third of asphyxiated neo-
based on traditional viewpoints. Multiorgan dysfunction is nates and represents one of the most common causes of peri-
common2 and cardiovascular dysfunction, defined as either evi- natal myocardial infarction.7-9 Birth asphyxia or associated
dence of transient myocardial ischemia or hypotension re- conditions, such as meconium aspiration syndrome, may limit
quiring an inotrope >24 hours, is noted in 62% of neonates the normal decline in pulmonary vascular resistance after birth
with a diagnosis of HIE.2 leading to acute pulmonary hypertension. The clinical and
The reported incidence of hemodynamic instability in pub- physiological consequences include low pulmonary blood flow
lished clinical trials ranges from 33% to 77% in patients re- and/or right heart dysfunction because of high right ventricu-
ceiving TH and from 25% to 83% in controls3 (Table I; available lar afterload leading to systemic hypotension/low cardiac output
at www.jpeds.com). Though there has been no consistent link state. TH further induces pulmonary vasoconstriction,10 which
between the degree of hemodynamic instability and may aggravate acute pulmonary hypertension necessitating an
neurodevelopmental outcome, the physiology is often complex, escalation of treatment; the impact of such deterioration and
which presents a window of opportunity to individualize treatments for it on brain injury remain unknown.
therapy with a goal of improving outcomes.
The current therapeutic approach to hemodynamic care Interaction between the Cardiovascular System
focuses on improving arbitrary mean arterial pressure thresh- and Central Nervous System Injury
olds and fails to consider the severity of the asphyxial injury, Hypoxic-ischemic injury represents a complex biological dis-
the complexity of the hemodynamic derangement, or the turbance, which may lead to secondary energy failure and cell
impact of both TH and rewarming. In this review, we ap- death by both necrosis and/or apoptosis (Figure 1).6,7,11 Whether
praise the clinical and physiological impact of HIE and TH on there is a direct link between cerebral ischemia and cardiac dys-
neonatal hemodynamics and myocardial performance. It is function in HIE is not yet clear. Stroke victims are known to
plausible that ongoing hemodynamic instability, related either
to the primary insult or the effects of TH, and the approach
From the 1Division of Neonatology, The Hospital for Sick Children, Toronto, Ontario,
Canada; 2Department of Pediatrics, University of Toronto, Toronto, Ontario, Canada;
3
Institute of Medical Science; and 4Department of Physiology, University of Toronto,
HIE Hypoxic-ischemic encephalopathy Toronto, Ontario, Canada
iNO Inhaled nitric oxide The authors declare no conflicts of interest.
MRI Magnetic resonance imaging
TH Therapeutic hypothermia 0022-3476/$ - see front matter. © 2016 Elsevier Inc. All rights reserved.
http://dx.doi.org10.1016/j.jpeds.2016.09.009
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
THE JOURNAL OF PEDIATRICS • www.jpeds.com Volume ■■
Figure 1. Theoretical model of concurrent circulatory and neuronal changes after a hypoxic ischemic injury.11-15 Cells may enter
the latent phase at different times because both primary and secondary energy failure may coexist. CBF, cerebral blood flow.
experience electrocardiographic abnormalities and cardiovas- of the latent period varies, and hemodynamic instability after
cular disturbances, similar to HIE, which may lead to death.12 the initial insult may contribute to ongoing injury beyond the
In a rat model, cerebral ischemia directly causes myocardial 6- hour therapeutic window (Figure 1). The duration of po-
dysfunction by disrupting calcium homeostasis.16 This pro- tential exposure to ongoing injury likely relates to the nature
vides biological plausibility for a comparable association in and severity of the initial insult, and the aggressiveness of re-
human neonates. suscitation; therefore, injury may occur over a period of minutes
to hours. Early recognition of low systemic blood flow may
Effects of Asphyxia on Cerebral Blood Flow play a role; however, it is unclear whether cardiovascular therapy
Asphyxia is associated with a variable degree of vasomotor pa- itself may impact the brain’s ability to autoregulate as has been
ralysis, which if moderate or severe, may be associated with suggested in some preterm studies. The relative contribution
impaired autoregulation. This is supported by evidence that of reperfusion to the injurious process is likely to relate to the
hypoperfusion is followed by hyperperfusion over a predict- specific agent used, dosage used, and route of administra-
able time course. The magnitude of this elevation in cerebral tion; rapid augmentation of inotropic agents or potent vaso-
blood flow is associated with the risk of neurocognitive pressors may cause dramatic reperfusion over a period of
impairment17; specifically, the most severely affected infants minutes to hours.24 Current guidelines for initiation of TH are
develop high cerebral blood flow by 12-24 hours of age.18 It based on evidence from animal experimental models where
remains unclear, however, whether this association is a mani- the insult was timed, and on both human and animal studies
festation of the severity of the underlying insult or whether where central nervous system damage occurs during the sec-
reperfusion injury contributes to worse outcome. ondary energy failure stage after a 6- to 15-hour latent period.
The initial injury varies in severity, duration, and timing and It is unclear whether there are groups of neonates who may
has been classically grouped into discrete categories (Table II; benefit from modification of established guidelines for TH or
available at www.jpeds.com)19,20; in reality, neonates with HIE, if tighter control of hemodynamics and cerebral blood flow
particularly the moderate group, represent a heterogeneous may contribute to improved outcomes.
group with variable and overlapping clinical and radiologic
phenotypes.21 At a cellular level in fetal sheep, partial pro- Cardiovascular Impact of TH
longed asphyxia produces cortical hyperexcitability and sen- Though the mechanisms of hypothermic neuroprotection are
sitization to neuronal injury, implying an escalating risk of acute fairly well understood,13,14,25 the effects of TH on other organ
or chronic injury.22 It is biologically plausible that unregu- systems are relatively unknown. Human and animal models
lated changes in cerebral blood flow may have a role in suggest a cardioprotective effect similar to its effect in the central
modulating the severity of injury following the initial insult. nervous system; troponin I levels are reduced in newborn piglets
In near-term fetal sheep, cooling initiated after the start of the and human neonates when TH is used.26 Liu et al26 found that
secondary energy failure stage is not effective.23 In clinical prac- immediate initiation of TH resulted in a 50% reduction in
tice, the exact timing of injury is rarely known, the duration ischemic heart lesions compared with normothermic piglet
2 Giesinger et al
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
■■ 2016 MEDICAL PROGRESS
Figure 2. Interrelationship between contributors to ischemic injury resulting from initial insult, TH, and reperfusion injury on
rewarming.2,28,30,32-34 Both ischemia and reperfusion injury may contribute to the degree of brain injury via modification of car-
diovascular factors. Resumption of cellular activity after transient suppression is a putative source of potentially damaging oxi-
dative radicals.25 HR, heart rate; LV, left ventricle; PBF, pulmonary blood flow; PVR, pulmonary vascular resistance; RV, right
ventricle.
controls. Sinus bradycardia, however, is a well-established as- nates with a more severe or prolonged hypoxia are at greater
sociation of TH. It occurs because of slowed diastolic repo- risk of impaired transition eventually leading to persistent pul-
larization in the sino-atrial node and diminished influence of monary hypertension of the newborn. Specifically, reduced pul-
the sympathetic autonomic nervous system on heart rate.5 In monary blood flow leads to lower preductal cardiac output
controlled hypothermia for out-of-hospital patients with cardiac which, combined with systemic hypoxemia, may further
arrest, resting bradycardia is associated with a significant re- magnify the ischemic insult.31 On the other hand, the use of
duction in mortality and improved neurologic outcome.27 The rapidly acting pulmonary vasodilators, such as inhaled nitric
mechanism behind this association is unclear, likely multifac- oxide (iNO), leads to increased pulmonary venous return and
torial, and may reflect both cause and effect. Relative brady- augmentation of preductal cardiac output, which may con-
cardia may result in an overall reduction in myocardial substrate tribute to reperfusion injury (Figure 2). During rewarming,
requirement and, therefore, may be protective against ongoing these changes are likely to be further amplified. Concurrent
ischemic stress, whereas the use of chronotropic cardiovascu- exposure to high concentrations of oxygen35 and exogenous
lar treatments may increase metabolic requirements and the nitric oxide36 promotes the production of reactive oxygen
risk of cell death. Alternatively, normal heart rate despite low species, which may cause further injury to the brain.
temperature may reflect subclinical systemic hypoperfusion and The impact of abnormal hemodynamics on cerebral blood
may contribute to ongoing brain injury (Figure 1). The re- flow is relevant to short-term clinical outcomes. In 24 neo-
duction in heart rate after initiation of TH leads to a 60%- nates, normal brain MRI was associated with lower cerebral
70% decrease in left ventricular output compared with blood flow, which further declined in those undergoing TH
normothermic controls.28 These changes are generally well tol- compared with neonates with poor radiologic outcome who
erated, and although cardiac output is lower, it is likely to meet had a higher baseline and progressive rise in cerebral blood
the metabolic needs of the asphyxiated newborn, particu- flow despite TH.17 In addition, neonates with abnormal brain
larly in the context of TH where metabolic activity is further MRI demonstrate significant redistribution of left ventricu-
reduced. TH alone is not associated with an increased risk of lar output toward the central nervous system. This is evi-
hypotension, 1 and in the absence of cardiovascular denced by a 57% reduction in left ventricular output with
comorbidities, most neonates have normal or slightly in- preserved superior vena cava flow during TH in asphyxiated
creased blood pressure related to hypothermia induced vaso- neonates with abnormal day 3-4 MRI compared with healthy
constriction and normal myocardial performance.29 term controls studied at a comparable age. Neonates with
Severity of brain injury may be associated with dysregulation normal postrewarming MRI have a proportional reduction in
of vascular tone in the pulmonary vascular bed. Neonates with both left ventricular output and superior vena cava flow during
concurrent pulmonary hypertension and HIE are more likely TH.28 It is not known whether this redistribution reflects brain-
to have an abnormal brain magnetic resonance imaging (MRI) sparing physiological adaptation, or whether it is pathologic
despite TH.30 This may reflect greater disease severity as neo- and represents impaired cerebral autoregulation. Low left
Hypoxic-Ischemic Encephalopathy and Therapeutic Hypothermia: The Hemodynamic Perspective 3
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
THE JOURNAL OF PEDIATRICS • www.jpeds.com Volume ■■
ventricular output alone, however, is not associated with a
Table III. Confounders of assessment of systemic he-
greater risk of ischemic MRI changes.30 Further studies are re-
modynamics in patients because of HIE* and/or TH†39
quired to determine clinical relevance of this observation.
Hyperperfusion and associated hyperoxia are putative con- Variables Change Pathophysiology
tributory factors to secondary injury.18 Identification of the ideal Heart rate Sinus bradycardia ↓ repolarization at SA node†
cerebral blood flow to optimize substrate delivery and mini- Blood pressure ↑ DAP Systemic vasoconstriction†
↓ SAP ↓ cardiac output†
mize the risk of reperfusion injury may yield a potential target Color Pallor ↓ skin perfusion†
of therapy. No clinical intervention aimed at matching cere- Capillary refill time Prolongation ↓ skin perfusion†
bral demand with supply is presently available; the ideal strat- Urinary output Oliguria or anuria Acute renal injury*
Blood gas Metabolic acidosis Residual perinatal acidosis*
egy should take into consideration the theoretical hazards of Lactate Lactic acidosis Lactate washout after initial
isolated hyper- or hypoperfusion or cycling between both. The insult*, sequestering†
optimum ranges for arterial pressure and cardiac output, which DAP, diastolic arterial pressure; SA, sinoatrial; SAP, systolic arterial pressure.
minimize harmful fluxes in cerebral perfusion, remain uncer- *HIE.
tain and warrant prospective scientific investigation. In †TH.
addition, none of the infants in these studies were followed
long-term; therefore, the relationship between cerebral blood ficult because of the confounding effects of temperature
flow and neurodevelopmental impairment remains an area for (Table III). First, it is the norm for neonates undergoing TH
study. to have resting bradycardia32; normal heart rate may be falsely
reassuring. Laboratory markers, such as metabolic acidosis and
The Effects of Rewarming elevated lactate,40 may reflect the primary hypoxic insult, in-
The physiological consequences of rewarming are likely to in- dependent of cardiovascular status, and may persist for hours
fluence both treatment and clinical outcomes, although there to days after the initial injury, or may relate to a low cardiac
is little published evidence (Figure 2). Known changes include output state.41 A high index of suspicion should be main-
augmentation of cardiac output and systolic blood pressure tained for circulatory inadequacy, and clinical variables should
with a concurrent decrease in systemic vascular resistance and be interpreted cautiously in the context of multiorgan
diastolic blood pressure; the net consequence is overall reduc- dysfunction.
tion of mean blood pressure by approximately 8 mm Hg.32 The Arterial pressure thresholds are commonly used to ap-
pattern of redistribution of cardiac output to the brain, seen praise cardiovascular health but may be difficult to interpret.
during the cooling phase in infants with adverse outcome, Observational studies in healthy, term neonates attempt to as-
remains consistent during rewarming.28 These physiologic certain the reference ranges for the different variables repre-
changes may have implications for neonates requiring cardio- sented by neonatal arterial pressure. The bulk of neonates have
vascular support, particularly if there is concomitant dose es- been studied in small populations via noninvasive upper-
calation. In addition, changes in temperature affect volume of limb measurement on day 1-242,43 or beyond,44,45 with limited
distribution, metabolism, and clearance of drugs.5,37 Drugs with data in the transitional period.46 Arterial pressure is influ-
a large volume of distribution are mobilized from seques- enced by gestational and chronologic age47,48; some sources
tered tissues and may have an exaggerated effect during suggest differences related to birth weight48 and sex.46 Based
rewarming. on limited data, day 1 median (fifth per centile) values for sys-
In a cohort of 160 asphyxiated neonates, of whom 9% de- tolic, diastolic, and mean arterial pressure are 65 mm Hg
veloped intraventricular hemorrhage, hemorrhage at the time (55 mm Hg), 45 mm Hg (30 mm Hg), and 48 mm Hg (40 mm
of rewarming was associated with a greater degree of hemo- Hg), respectively.42 High quality, large, prospective cohort studies
dynamic instability.38 Therefore, it is plausible that rewarm- that take into consideration sex, racial, and geographic vari-
ing represents a particularly vulnerable period for the central ability, as well as gestation and size are required. Multiple time
nervous system; it is important to avoid large fluctuations in point measurements over the first 24 hours are required to take
cerebral blood flow during this period. Active adjustment of variation in transition into account. When assessing the clini-
cardiovascular medications throughout the warming period cal relevance of systemic hypotension, it is important to con-
may be necessary to avoid iatrogenic hypertension and exces- sider the components of systolic, diastolic, and mean separately.
sive unregulated cerebral blood flow. Neonates require careful An adequate diastolic arterial pressure is generally main-
monitoring during rewarming; for those neonates requiring tained in neonates receiving TH by hypothermia induced pe-
significant support, more gradual rewarming may have theo- ripheral vasoconstriction.32 In contrast, systolic arterial pressure
retical benefit in achieving a more controlled change in he- is usually in the low normal range but is likely to be suffi-
modynamics. Rewarming hemodynamics, however, requires cient to maintain adequate organ perfusion.32 Dramatic in-
further study. creases in systolic arterial pressure are theoretically harmful
by increasing the risk of reperfusion hemorrhage; cautious use
Clinical Implications of HIE/TH of pharmacologic support in otherwise stable neonates is there-
fore recommended. Over reliance on mean arterial pressure,49
Clinical assessment of systemic and central nervous system he- however, may also result in late identification of major drops
modynamics in neonates with asphyxia during TH may be dif- in systolic arterial pressure.
4 Giesinger et al
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
■■ 2016 MEDICAL PROGRESS
Table V. Echocardiography findings, pathophysiology, and suggested therapy in neonates with HIE and hemodynamic
instability39
Clinical presentation Echocardiography findings Management principles Suggested management
Low SAP, normal LV/RV systolic dysfunction (+) Inotropy 1st line: dobutamine
oxygenation 2nd line: epinephrine
- Hydrocortisone (if refractory)
Low SAP, impaired PPHN Pulmonary vasodilation and 1st line: iNO, optimum ventilation
oxygenation ↑SBF 2nd line: vasopressin or norepinephrine
- PGE1 (if restrictive DA)
- Hydrocortisone (if refractory)
LV dysfunction + PPHN (+) inotropy, maintain R 1st line: dobutamine, PGE1 (if
→ L ductal shunt to support restrictive DA)
SBF 2nd line: epinephrine (caution if severe oxygenation failure)
- Hydrocortisone (if refractory)
RV dysfunction + PPHN (+) Inotropy, reduce RV 1st line: dobutamine, iNO
afterload, maintain adequate 2nd line: PGE1 (if restrictive DA) 3rd line: vasopressin or norepinephrine
RV preload - Hydrocortisone (if refractory)
PGE1, prostaglandin E1; SBF, systemic blood flow.
Electrocardiogram and cardiac enzymes are widely used to of the mitral valve leaflet.9 The assessment of right ventricu-
identify myocardial ischemia in adult patients.50 Electrographic lar function was previously limited to subjective assessment;
changes (Table IV; available at www.jpeds.com)51 and marked however, this method has been shown to be inaccurate.56 Recent
cardiac enzyme increase51,52 also have been associated with tran- studies of healthy newborn infants have shown that calcula-
sient myocardial ischemia in neonates with HIE. The sensi- tion of right ventricular fractional area change, the displace-
tivity and specificity of the electrocardiogram for the detection ment of the tricuspid annulus (tricuspid annular plane systolic
of transient myocardial ischemia are not known, though as- excursion), or use of deformation/tissue Doppler methods are
phyxiated neonates more frequently demonstrate abnormali- feasible for evaluation of right ventricular systolic performance.57
ties of the ST segment and Q waves than healthy controls.53 Left and right ventricular output may be calculated as surro-
Alterations in the amplitude and axis of the T wave alone may gate markers of systolic performance. Where available, tar-
be associated with ischemia after 24 hours of life.54 Further study geted neonatal echocardiography offers an advantage in the
is required to define the prognostic value of the electrocar- ability to perform longitudinal assessments and assess treat-
diogram; if early ischemic changes can be reliably detected, the ment response; with increasing training of neonatologists in
electrocardiogram may aid in identification of neonates who the skill, focused assessment will be more widely available.
may benefit from echocardiography. Creatine kinase MB Novel technologies may allow the assessment of the direct
isozyme is significantly elevated in neonates with moderate to impact of cardiovascular change on brain health. Near-
severe encephalopathy and begins to rise within 4-8 hours of infrared spectroscopy is a bedside tool that indirectly evalu-
injury.9 Furthermore, it has been suggested that cardiac tro- ates cerebral blood flow by measuring real-time regional mixed
ponin I level at 24 hours of age, often not measured as part venous saturation (rScO2), reflecting the oxygen supply/
of routine clinical practice, is a useful prognostic marker of demand ratio. There is some evidence that it could be used
neurologic outcome 18-22 months in both cooled and to predict adverse outcome in the setting of HIE/TH58 and has
noncooled infants.55 been used to assess cerebral autoregulation.59 These studies have
Targeted neonatal echocardiography is a bedside tool, used limitations including small sample sizes and the lack of cor-
to assess cardiovascular health and refine therapeutic inter- relation with a clinical gold standard method. Longitudinal
ventions in this high-risk population (Table V). Assessment studies of combined targeted neonatal echocardiography and
by an experienced operator may enhance the precision of di- near infrared spectroscopy may allow further delineation of
agnosis and clinical appropriateness of therapeutic interven- abnormal physiology and the impact of treatment. Heart rate
tions by delineating actual pathophysiology of hemodynamic variability is a well-validated surrogate of fetal well-being in
instability, rather than relying on clinical estimation. In neo- obstetrical literature; specifically, reduced beat-to-beat vari-
nates who are sick and have HIE, assessment by pediatric car- ability and superimposed decelerations are associated with acute
diology may be beneficial. A high index of suspicion is fetal asphyxia.60 Recent literature has examined the predic-
important, particularly in infants of mothers with diabetes, for tive role of heart rate variability in staging of HIE and outcome
associated congenital heart disease or hypertrophic obstruc- prognostication. Preliminary data suggests that lower heart rate
tive cardiomyopathy. In the absence of targeted neonatal variability in the first 24 hours of life is associated with more
echocardiography, echocardiography by pediatric cardiology severe HIE as measured by electroencephalogram and MRI.60
may provide insight into hemodynamics, depending on local Heart rate variability is, however, ineffective for predicting
practice. Left ventricular systolic function may be assessed using seizures,61 and it remains to be seen whether this modality will
conventional methods (fractional shortening or ejection frac- provide additional or earlier information than established
tion), or tissue Doppler imaging of the anterior/septal walls methods.
Hypoxic-Ischemic Encephalopathy and Therapeutic Hypothermia: The Hemodynamic Perspective 5
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
THE JOURNAL OF PEDIATRICS • www.jpeds.com Volume ■■
Approach to Cardiovascular Care in HIE/TH hypertension,65 and it has been shown to improve systemic he-
modynamics in animal models of asphyxia66,67; its effects in neo-
The approach to cardiovascular care should consider actual nates with HIE, particularly those with left ventricular
pathophysiology, phase of intervention (eg, during TH or re- dysfunction, remain unknown. Of note, the administration of
warming), and impact of concomitant treatments.39 Most neo- milrinone to neonates undergoing TH for HIE is not recom-
nates with isolated transient myocardial ischemia are mended as drug clearance is lower, which may lead to toxic
asymptomatic and improve over time. Given the association drug levels and extreme hypotension because of potent sys-
between increased cerebral blood flow and poor outcome, ag- temic vasodilation.63 There is limited evidence for the use of
gressive volume resuscitation should be avoided except when norepinephrine, an endogenous systemic vasoconstrictor; it is
there is direct evidence of acute hypovolemia. Blood transfu- a potent a agonist with some activity at the b1 receptor. Both
sion for anemia should be considered in pulmonary hyper- animal data68,69 and small trials in human neonates70 suggest
tension to optimize oxygen carrying capacity. Myocardial that norepinephrine may have some pulmonary vasodilator
ischemia may affect either ventricle or both. Left ventricular effects; b1 activity provides some positive inotropy. Adrenal
dysfunction results in reduced stroke volume and low cardiac insufficiency may occur independently or in combination with
output; right ventricular dysfunction may lead to both hy- other causes of hypotension, presenting with refractory hy-
poxemia and systemic hypotension via reduced pulmonary potension despite catecholamine therapy and potentially as-
blood flow, reduced left ventricular preload, and, therefore, low sociated with hyponatremia and hypoglycemia. Hydrocortisone
left ventricular output. Ventricular dysfunction may mani- is indicated in refractory hypotension, especially if adrenal injury
fest as systolic or severe hypotension with mild or moderate is suspected.
hypoxemia. Optimal thresholds for intervention are poorly Although the neurologic benefits of TH are clear, exposure
defined; clinicians need to weigh the impact of cardiovascu- to lower core body temperature increases the degree of pul-
lar treatments for impaired myocardial function and low cardiac monary vasoconstriction.10 Though there was no statistically
output against the consequences of reperfusion injury. significant increase in clinically detectable pulmonary hyper-
Dobutamine is the most appropriate first line agent for iso- tension identified in randomized controlled trials, the trials were
lated hypotension, particularly in neonates with low systolic not powered to detect differences in illness severity and from
blood pressure and evidence of end organ hypoperfusion, to some trials (eg, Infant Cooling Evaluation, Neo.nEURO.network
increase stroke volume and cardiac output (Table V). It acts Trial) the most hemodynamically unstable infants were
through a1 and b1 receptors in the myocardium to increase excluded71,72 (Table I). In a subpopulation with preexisting pul-
in cardiac contractility and heart rate. The peripheral effects monary hypertension, TH may further impair oxygenation73;
include both vasoconstriction and vasodilation resulting in a judicious increases in target temperature may improve
net neutral effect.62 oxygenation.74 The approach to management in neonates with
In the setting of high afterload because of persistent pul- moderate hypoxemia should focus on strategies to maximize
monary hypertension, any degree of right ventricular dys- pulmonary vasodilation, in an effort to allow continuation of
function may be poorly tolerated. Even with normal right TH. It has been our anecdotal clinical experience that in pa-
ventricular function, pulmonary hypertension may lead to low tients where pulmonary vasodilator treatments fails, modifi-
pulmonary blood flow, impaired oxygenation, and low cardiac cations of target temperature by small increments (0.5-1 degree)
output. In the setting of pulmonary hypertension and HIE, may improve oxygenation; rarely, TH may need to be discon-
conventional therapies including sedation, muscle relax- tinued. Although there may be advantages to attaining target
ation, and ventilation are indicated. Though a poor response temperature as early as is feasible, it is important to remem-
is seen in 40% of neonates,63 iNO remains the first line pul- ber that TH is a postresuscitation intervention; hence, medical
monary vasodilator. In neonates without concurrent pulmo- stabilization of oxygenation failure in the immediate period
nary parenchymal disease (eg, meconium aspiration syndrome), after birth should precede the initiation of TH.
care must be taken to avoid excess mean airway pressure as Moderate to severe left ventricular systolic dysfunction may
this can further impair pulmonary venous return (Table V). lead to pulmonary venous hypertension because of diastolic
For neonates with systemic hypotension and pulmonary hy- impairment. This manifests clinically as respiratory insuffi-
pertension, intravenous infusion of dobutamine is an appro- ciency and hypoxemia, which may mimic persistent pulmo-
priate choice as it will improve cardiac output and may offer nary hypertension of the newborn.
some improvement to pulmonary blood flow. Vasopressin is Diagnostic clues may include pulmonary edema on chest
a drug with dichotomous properties. In vascular smooth muscle radiography or left to right atrial shunting in the presence of
such as the skin, skeletal muscle, and splanchnic circulation, a right to left ductal shunt in the setting of left ventricular sys-
it produces potent vasoconstriction. In the pulmonary vas- tolic dysfunction on echocardiography.75 Neonates with severe
culature, vasopressin activates endothelial receptors, which result left ventricular dysfunction may have critically low left ven-
in stimulation of the nitric oxide pathway and vasodilation of tricular output and require the support of agents with inotropy,
select vessels.64 Vasopressin may be physiologically advanta- especially as hypothermia induced vasoconstriction may cause
geous in neonates with systemic hypotension and oxygen- left ventricular wall stress and exacerbate dysfunction 76
ation failure where there is unrestrictive right-left flow. There (Table V). The clinical picture may functionally mimic criti-
is evidence of benefit in neonates with pulmonary cal aortic stenosis requiring intravenous prostaglandin infu-
6 Giesinger et al
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
■■ 2016 MEDICAL PROGRESS
sion to maintain ductal patency and augment postductal cardiac 8. Martin-Ancel A, Garcia-Alix A, Gaya F, Cabanas F, Burgueros M, Quero
output. Therapies with pulmonary vasodilator effects (eg, J. Multiple organ involvement in perinatal asphyxia. J Pediatr 1995;127:786-
93.
oxygen, iNO) should be used with caution, as they either may 9. Armstrong K, Franklin O, Sweetman D, Molloy EJ. Cardiovascular dys-
be of no benefit or may precipitate cardiogenic shock. Strat- function in infants with neonatal encephalopathy. Arch Dis Child
egies to increase pulmonary vascular resistance (eg, permis- 2012;97:372-5.
sive hypercapnia, lower oxygen saturation targets) and promote 10. Benumof JL, Wahrenbrock EA. Dependency of hypoxic pulmonary va-
right-left shunt are required to augment systemic blood flow. soconstriction on temperature. J Appl Physiol Respir Environ Exerc Physiol
1977;42:56-8.
In severe cases, retrograde flow in the aortic arch may augment 11. Vannucci RC, Towfighi J, Vannucci SJ. Secondary energy failure after ce-
cerebral perfusion. Neonates with severe right ventricular sys- rebral hypoxia-ischemia in the immature rat. J Cereb Blood Flow Metab
tolic dysfunction may benefit from afterload reduction with 2004;24:1090-7.
pulmonary vasodilator therapy. In addition, as the pulmo- 12. Dogan A, Tunc E, Ozturk M, Kerman M, Akhan G. Electrocardio-
nary circulation becomes pressure passive, maintaining graphic changes in patients with ischaemic stroke and their prognostic
importance. Int J Clin Pract 2004;58:436-40.
adequate right ventricular preload is essential (Table V). In 13. Wassink G, Gunn ER, Drury PP, Bennet L, Gunn AJ. The mechanisms
some centers, targeted neonatal echocardiography may provide and treatment of asphyxial encephalopathy. Front Neurosci 2014;8:40.
pathophysiologic information, which may enhance the care of 14. Gunn AJ, Gunn TR, de Haan HH, Williams CE, Gluckman PD. Dra-
neonates with severe or refractory hypotension and/or matic neuronal rescue with prolonged selective head cooling after isch-
hypoxemia. emia in fetal lambs. J Clin Invest 1997;99:248-56.
15. Bhalala US, Koehler RC, Kannan S. Neuroinflammation and neuroimmune
dysregulation after acute hypoxic-ischemic injury of developing brain. Front
Conclusions Pediatr 2014;2:144.
16. Sun L, Ai J, Wang N, Zhang R, Li J, Zhang T, et al. Cerebral ischemia elicits
aberration in myocardium contractile function and intracellular calcium
Neonates with asphyxia represent a vulnerable population. Al- handling. Cell Physiol Biochem 2010;26:421-30.
though TH has transformed the care of this population and 17. Kumagai T, Higuchi R, Higa A, Tsuno Y, Hiramatsu C, Sugimoto T, et al.
led to improved neurodevelopmental outcomes, refinement of Correlation between echocardiographic superior vena cava flow and short-
cardiovascular care may provide additional benefit. Cur- term outcome in infants with asphyxia. Early Hum Dev 2013;89:307-10.
18. Ilves P, Lintrop M, Metsvaht T, Vaher U, Talvik T. Cerebral blood-flow
rently, the relationship between altered hemodynamics and
velocities in predicting outcome of asphyxiated newborn infants. Acta
brain health remains poorly understood. A comprehensive un- Paediatr 2004;93:523-8.
derstanding of the physiological mechanisms of disease and 19. Shah PS, Perlman M. Time courses of intrapartum asphyxia: neonatal char-
therapy and real-time bedside assessment tools, such as tar- acteristics and outcomes. Am J Perinatol 2009;26:39-44.
geted neonatal echocardiography, may be invaluable aids to 20. Pasternak JF, Gorey MT. The syndrome of acute near-total intrauterine
asphyxia in the term infant. Pediatr Neurol 1998;18:391-8.
decision-making. Individualization of therapy may present an
21. Shankaran S, McDonald SA, Laptook AR, Hintz SR, Barnes PD, Das A,
opportunity for improved outcomes. ■ et al. Neonatal magnetic resonance imaging pattern of brain injury as a
biomarker of childhood outcomes following a trial of hypothermia for
Submitted for publication May 5, 2016; last revision received Jul 13, 2016; neonatal hypoxic-ischemic encephalopathy. J Pediatr 2015;167:987-93, e3.
accepted Sep 7, 2016 22. Mallard EC, Williams CE, Gunn AJ, Gunning MI, Gluckman PD. Fre-
Reprint requests: Patrick J. McNamara MB, MSC, Division of Neonatology, quent episodes of brief ischemia sensitize the fetal sheep brain to neu-
The Hospital for Sick Children, 555 University Ave, Toronto, Ontario, Canada ronal loss and induce striatal injury. Pediatr Res 1993;33:61-5.
M5G 1X8. E-mail: patrick.mcnamara@sickkids.ca 23. Gunn AJ, Bennet L, Gunning MI, Gluckman PD, Gunn TR. Cerebral hy-
pothermia is not neuroprotective when started after postischemic sei-
zures in fetal sheep. Pediatr Res 1999;46:274-80.
References 24. Munro MJ, Walker AM, Barfield CP. Hypotensive extremely low birth
weight infants have reduced cerebral blood flow. Pediatrics 2004;114:1591-
1. Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. 6.
Cooling for newborns with hypoxic ischaemic encephalopathy. Co- 25. Thoresen M, Satas S, Puka-Sundvall M, Whitelaw A, Hallstrom A, Loberg
chrane Database Syst Rev 2013;1:CD003311. EM, et al. Post-hypoxic hypothermia reduces cerebrocortical release of
2. Shah P, Riphagen S, Beyene J, Perlman M. Multiorgan dysfunction in NO and excitotoxins. Neuroreport 1997;8:3359-62.
infants with post-asphyxial hypoxic-ischaemic encephalopathy. Arch Dis 26. Liu X, Tooley J, Loberg EM, Suleiman MS, Thoresen M. Immediate hy-
Child Fetal Neonatal Ed 2004;89:F152-5. pothermia reduces cardiac troponin I after hypoxic- ischemic encepha-
3. Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, lopathy in newborn pigs. Pediatr Res 2011;70:352-6.
et al. Moderate hypothermia to treat perinatal asphyxial encephalopa- 27. Thomsen JH, Nielsen N, Hassager C, Wanscher M, Pehrson S, Kober L,
thy. N Engl J Med 2009;361:1349-58. et al. Bradycardia during targeted temperature management: an early
4. Kanik E, Ozer EA, Bakiler AR, Aydinlioglu H, Dorak C, Dogrusoz B, et al. marker of lower mortality and favorable neurologic outcome in coma-
Assessment of myocardial dysfunction in neonates with hypoxic- tose out-of-hospital cardiac arrest patients. Crit Care Med 2016;44:308-
ischemic encephalopathy: is it a significant predictor of mortality? J Matern 18.
Fetal Neonatal Med 2009;22:239-42. 28. Hochwald O, Jabr M, Osiovich H, Miller SP, McNamara PJ, Lavoie PM.
5. Wood T, Thoresen M. Physiological responses to hypothermia. Semin Fetal Preferential cephalic redistribution of left ventricular cardiac output during
Neonatal Med 2014;20:87-96. therapeutic hypothermia for perinatal hypoxic-ischemic encephalopa-
6. Calbet JA, Robach P, Lundby C. The exercising heart at altitude. Cell Mol thy. J Pediatr 2014;164:999-1004, e1.
Life Sci 2009;66:3601-13. 29. Nestaas E, Skranes JH, Stoylen A, Brunvand L, Fugelseth D. The myo-
7. Dattilo G, Tulino V, Tulino D, Lamari A, Falanga G, Marte F, et al. cardial function during and after whole-body therapeutic hypothermia
Perinatal asphyxia and cardiac abnormalities. Int J Cardiol 2011;147:e39- for hypoxic-ischemic encephalopathy, a cohort study. Early Hum Dev
40. 2014;90:247-52.
Hypoxic-Ischemic Encephalopathy and Therapeutic Hypothermia: The Hemodynamic Perspective 7
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
THE JOURNAL OF PEDIATRICS • www.jpeds.com Volume ■■
30. More K, Sakhuja P, Ting J, Seth J, Lapointe A, Jain A, et al. Cardiovas- diographic, echocardiographic and enzymatic correlations. Eur J Pediatr
cular Performance during Whole Body Hypothermia And After Active Re- 1999;158:742-7.
warming and MRI Patterns of Brain Injury. E:PAS2014:#4107.193. 52. Agrawal J, Shah GS, Poudel P, Baral N, Agrawal A, Mishra OP. Electro-
31. Jain A, McNamara P. Persistent pulmonary hypertension of the newborn: cardiographic and enzymatic correlations with outcome in neonates with
physiology, hemodynamic assessment and novel therapies. Semin Fetal hypoxic-ischemic encephalopathy. Ital J Pediatr 2012;38:33.
Neonatal Med 2015;20:262-71. 53. Jedeikin R, Primhak A, Shennan AT, Swyer PR, Rowe RD. Serial electro-
32. Zanelli S, Buck M, Fairchild K. Physiologic and pharmacologic consid- cardiographic changes in healthy and stressed neonates. Arch Dis Child
erations for hypothermia therapy in neonates. J Perinatol 2011;31:377- 1983;58:605-11.
86. 54. Primhak RA, Jedeikin R, Ellis G, Makela SK, Gillan JE, Swyer PR, et al.
33. Banagale RC, Donn SM. Asphyxia neonatorum. J Fam Pract 1986;22:539- Myocardial ischaemia in asphyxia neonatorum. Electrocardiographic, en-
46. zymatic and histological correlations. Acta Paediatr Scand 1985;74:595-
34. Coughtrey H, Jeffery HE, Henderson-Smart DJ, Storey B, Poulos V. Pos- 600.
sible causes linking asphyxia, thick meconium and respiratory distress. 55. Liu X, Chakkarapani E, Stone J, Thoresen M. Effect of cardiac compres-
Aust N Z J Obstet Gynaecol 1991;31:97-102. sions and hypothermia treatment on cardiac troponin I in newborns with
35. Firth ALYJ. Bringing down the ROS: a new therapeutic approach for PPHN. perinatal asphyxia. Resuscitation 2013;84:1562-7.
Am J Physiol Lung Cell Mol Physiol 2008;295:L976-8. 56. Ling LF, Obuchowski NA, Rodriguez L, Popovic Z, Kwon D, Marwick TH.
36. Pacher PBJ, Liaudet L. Nitric oxide and peroxynitrite in health and disease. Accuracy and interobserver concordance of echocardiographic assess-
Physiol Rev 2007;87:315-424. ment of right ventricular size and systolic function: a quality control ex-
37. de Haan TR, Bijleveld YA, van der Lee JH, Groenendaal F, van den Broek ercise. J Am Soc Echocardiogr 2012;25:709-13.
MPH, Rademaker CMA, et al. Pharmacokinetics and pharmacodynam- 57. Jain A, Mohamed A, El-Khuffash A, Connelly KA, Dallaire F, Jankov RP,
ics of medication in asphyxiated newborns during controlled hypother- et al. A comprehensive echocardiographic protocol for assessing neona-
mia. The PharmaCool multicenter study. BMC Pediatr 2012;12:45. tal right ventricular dimensions and function in the transitional period:
38. Al Yazidi G, Boudes E, Tan X, Saint-Martin C, Shevell M, Wintermark normative data and z scores. J Am Soc Echocardiogr 2014;27:1293-
P. Intraventricular hemorrhage in asphyxiated newborns treated with hy- 304.
pothermia: a look into incidence, timing and risk factors. BMC Pediatr 58. Shellhaas RA, Kushwaha JS, Plegue MA, Selewski DT, Barks JD. An evalu-
2015;15:106. ation of cerebral and systemic predictors of 18- month outcomes for
39. Giesinger RE, McNamara PJ. Hemodynamic instability in the critically neonates with hypoxic ischemic encephalopathy. J Child Neurol
ill neonate: an approach to cardiovascular support based on disease patho- 2015;30:1526-31.
physiology. Semin Perinatol 2016;40:174-88. 59. Massaro AN, Govindan RB, Vezina G, Chang T, Andescavage NN, Wang
40. Beken S, Aydin B, Dilli D, Erol S, Zenciroglu A, Okumus N. Can bio- Y, et al. Impaired cerebral autoregulation and brain injury in newborns
chemical markers predict the severity of hypoxic- ischemic encephalopa- with hypoxic-ischemic encephalopathy treated with hypothermia. J
thy? Turk J Pediatr 2014;56:62-8. Neurophysiol 2015;114:818-24.
41. Al Balushi A, Guilbault MP, Wintermark P. Secondary increase of lactate 60. Vergales BD, Zanelli SA, Matsumoto JA, Goodkin HP, Lake DE, Moorman
levels in asphyxiated newborns during hypothermia treatment: reflect of JR, et al. Depressed heart rate variability is associated with abnormal EEG,
suboptimal hemodynamics (a case series and review of the literature). MRI, and death in neonates with hypoxic ischemic encephalopathy. Am
AJP Rep 2016;6:e48-58. J Perinatol 2014;31:855-62.
42. Kent AL, Kecskes Z, Shadbolt B, Falk MC. Normative blood pressure data 61. Massaro AN, Govindan RB, Al-Shargabi T, Andescavage NN, Metzler M,
in the early neonatal period. Pediatr Nephrol 2007;22:1335-41. Chang T, et al. Heart rate variability in encephalopathic newborns during
43. Nwokoye IC, Uleanya ND, Ibeziako NS, Ikefuna AN, Eze JC, Ibe JC. Blood and after therapeutic hypothermia. J Perinatol 2014;34:836-41.
pressure values in healthy term newborns at a tertiary health facility in 62. Ruffolo RR Jr. The pharmacology of dobutamine. Am J Med Sci
Enugu, Nigeria. Niger J Clin Pract 2015;18:584-8. 1987;294:244-8.
44. Satoh M, Inoue R, Tada H, Hosaka M, Metoki H, Asayama K, et al. Ref- 63. McNamara PJ, Shivananda SP, Sahni M, Freeman D, Taddio A. Pharma-
erence values and associated factors for Japanese newborns’ blood pres- cology of milrinone in neonates with persistent pulmonary hyperten-
sure and pulse rate: the babies’ and their parents’ longitudinal observation sion of the newborn and suboptimal response to inhaled nitric oxide.
in Suzuki Memorial Hospital on intrauterine period (BOSHI) study. J Pediatr Crit Care Med 2013;14:74-84.
Hypertens 2016;34:1578-85. 64. Holmes CL, Patel BM, Russell JA, Walley KR. Physiology of vasopressin
45. Samanta M, Mondal R, Ray S, Sabui T, Hazra A, Kundu C, et al. Nor- relevant to management of septic shock. Chest 2001;120:989-1002.
mative blood pressure data for Indian neonates. Indian Pediatr 2015;52:669- 65. Mohamed A, Nasef N, Shah V, McNamara PJ. Vasopressin as a rescue
73. therapy for refractory pulmonary hypertension in neonates: case series.
46. Salihoglu O, Can E, Beskardes A, Koc BS, Tan I, Can G, et al. Delivery Pediatr Crit Care Med 2014;15:148-54.
room blood pressure percentiles of healthy, singleton, liveborn neo- 66. Cheung DC, Gill RS, Liu JQ, Manouchehri N, Sergi C, Bigam D, et al.
nates. Pediatr Int 2012;54:182-9. Vasopressin improves systemic hemodynamics without compromising mes-
47. Pejovic B, Peco-Antic A, Marinkovic-Eric J. Blood pressure in non- enteric perfusion in the resuscitation of asphyxiated newborn piglets: a
critically ill preterm and full-term neonates. Pediatr Nephrol 2007;22:249- dose-response study. Intensive Care Med 2012;38:491-8.
57. 67. Pelletier JS, LaBossiere J, Dicken B, Gill RS, Sergi C, Tahbaz N, et al. Low-
48. Sadoh WE, Ibhanesebhor SE. Oscillometric blood pressure reference values dose vasopressin improves cardiac function in newborn piglets with acute
of African full-term neonates in their first days postpartum. Cardiovasc hypoxia-reoxygenation. Shock 2013;40:320-6.
J Afr 2009;20:344-7. 68. Hirsch LJ, Rooney MW, Wat SS, Kleinmann B, Mathru M. Norepineph-
49. Dempsey EM, Barrington KJ. Diagnostic criteria and therapeutic inter- rine and phenylephrine effects on right ventricular function in experi-
ventions for the hypotensive very low birth weight infant. J Perinatol mental canine pulmonary embolism. Chest 1991;100:796-801.
2006;26:677-81. 69. Cutaia M, Friedrich P. Hypoxia-induced alterations of norepinephrine
50. O’Connor RE, Al Ali AS, Brady WJ, Ghaemmaghami CA, Menon V, vascular reactivity in isolated perfused cat lung. J Appl Physiol 1987;63:982-
Welsford M, et al. Part 9: acute coronary syndromes: 2015 American Heart 7.
Association Guidelines update for cardiopulmonary resuscitation and emer- 70. Tourneux P, Rakza T, Bouissou A, Krim G, Storme L. Pulmonary circu-
gency cardiovascular care. Circulation 2015;132(18 Suppl 2):S483- latory effects of norepinephrine in newborn infants with persistent pul-
500. monary hypertension. J Pediatr 2008;153:345-9.
51. Barberi I, Calabro MP, Cordaro S, Gitto E, Sottile A, Prudente D, et al. 71. Jacobs SE, Morley CJ, Inder TE, Stewart MJ, Smith KR, McNamara PJ,
Myocardial ischaemia in neonates with perinatal asphyxia. Electrocar- et al. Whole-body hypothermia for term and near- term newborns with
8 Giesinger et al
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
■■ 2016 MEDICAL PROGRESS
hypoxic-ischemic encephalopathy: a randomized controlled trial. Arch 78. Shankaran S, Laptook A, Ehrenkranz R, Tyson J, McDonald S, Donovan
Pediatr Adolesc Med 2011;165:692-700. E, et al. Whole-body hypothermia for Neonates with hypoxic-ischemic
72. Simbruner G, Mittal RA, Rohlmann F, Muche R. Systemic hypothermia encephalopathy. N Engl J Med 2005;353:1574-84.
after neonatal encephalopathy: outcomes of neo.nEURO.network RCT. 79. Lin ZL, Yu HM, Lin J, Chen SQ, Liang ZQ, Zhang ZY. Mild hypother-
Pediatrics 2010;126:e771-8. mia via selective head cooling as neuroprotective therapy in term neo-
73. Thoresen M, Whitelaw A. Cardiovascular changes during mild therapeu- nates with perinatal asphyxia: an experience from a single neonatal intensive
tic hypothermia and rewarming in infants with hypoxic-ischemic en- care unit. J Perinatol 2006;26:180-4.
cephalopathy. Pediatrics 2000;106(1 Pt 1):92-9. 80. Gluckman P, Wyatt JS, Azzopardi D, Ballard R, et al. Selective head cooling
74. Gunn AJ, Gluckman PD, Gunn TR. Selective head cooling in newborn with mild systemic hypothermia after neonatal encephalopathy: a
infants after perinatal asphyxia: a safety study. Pediatrics 1998;102(4 Pt multicentre randomized trial. Lancet 2005;365:633-70.
1):885-92. 81. Akisu M, Huseyinov A, Yalaz M, Cetin H, Kultursay N. Selective head
75. Gien J, Kinsella JP. Management of pulmonary hypertension in infants cooling with hypothermia suppresses the generation of platelet-activating
with congenital diaphragmatic hernia. J Perinatol 2016;36(Suppl 2):S28- factor in cerebrospinal fluid of newborn infants with perinatal as-
31. phyxia. Prostaglandins Leukot Essent Fatty Acids 2003;69:45-50.
76. Barlow AJ, Ward C, Webber SA, Sinclair BG, Potts JE, Sandor GG. Myo- 82. Shankaran S, Laptook A, Wright LL, Ehrenkranz RA, Donovan EF, Fanaroff
cardial contractility in premature neonates with and without patent ductus AA, et al. Whole-body hypothermia for neonatal encephalopathy: animal
arteriosus. Pediatr Cardiol 2004;25:102-7. observations as a basis for a randomized, controlled pilot study in term
77. Zhou W, Cheng G, Shao X, Liu X, Shan R, Zhuang D, et al. Selective head infants. Pediatrics 2002;110:377-85.
cooling with mild systemic hypothermia after neonatal hypoxic isch- 83. Eicher DJ, Wagner CL, Katikaneni LP, Hulsey TC, Bass WT, Kaufman DA,
emic encephalopathy: a multicentre randomized controlled trial in China. et al. Moderate hypothermia in neonatal encephalopathy: safety out-
J Pediatr 2010;157:367-72. comes. Pediatr Neurol 2005;32:18-24.
Hypoxic-Ischemic Encephalopathy and Therapeutic Hypothermia: The Hemodynamic Perspective 9
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
THE JOURNAL OF PEDIATRICS • www.jpeds.com Volume ■■
Table I. Summary of enrollment criteria for randomized controlled trials of TH for HIE
Hemodynamic variables
Trials Inclusion Exclusion (definition) Outcome variables
Authors Year
TOBY3 2009 • ≥36 wk • ≥6 h of age • Hypotension (MAP < 40 mm • Composite outcome‡:
Whole body TH • Apgar ≤5 at 10 min • Major anomalies Hg) 77% TH vs 83% 45% TH vs 53%
• Resuscitation at 10 min • Surgical disorder control (NS) control (NS)
• Acidosis* cord or <60 min • PPHN (not defined) 10% TH vs
• Encephalopathy† or abnormal aEEG 6% control (NS)
neoEURO72 2010 • ≥36 wk • ≥5.5 h of age • Hypotension (MAP < 40 mm • Composite outcome‡:
Whole body TH • Apgar ≤5 at 10 min • High dose anticonvulsants Hg) 53% TH vs 44% 51% TH vs 83%
• Resuscitation at 10 min • IUGR (<1.8 kg) control (NS) control (P = .001)
• Acidosis* cord or <60 min • Major anomalies • PPHN (need for iNO) 7% TH, • Died during intervention
• Encephalopathy† or abnormal aEEG • Deemed in “extremis” by 16% control (NS) period 8% TH vs 13
neonatologist control (NS)
ICE71 2011 • ≥35 wk • ≥6 h of age • Hypotension (treated with • Composite outcome‡:
Whole body TH • Apgar ≤5 at 10 min • IUGR (<2 kg) inotropes) 46% TH vs 47% 51% TH vs 66%
• Mechanical ventilation at 10 min • Major anomalies control (NS) control (P = .03)
• Acidosis cord or <60 min (pH < 7.0, BD >12) • Active bleeding • PPHN (FiO2 1.0) excluded • Died: 25% TH vs 39%
• Encephalopathy† • FiO2 >80% control (P = .04)
• Refractory hypotension
• Unresponsive acidosis
Zhou et al77 2010 • ≥37 wk • ≥6 h of age • Hypotension (refractory • Composite outcome‡:
Selective head TH + • Apgar ≤3 at 1, ≤5 at 5 • Weight <2.5 kg MAP <40 mm Hg) 33% TH vs 49%
mild systemic TH • Resuscitation at 5 min • Major abnormalities frequency not reported; control (P = .01)
• Acidosis* • Clinical chorioamnionitis difference reported as NS
• Encephalopathy† • Other cause of encephalopathy
• Hb < 120
NICHD78 2005 • ≥36 wk • ≥6 h of age • Hypotension (need for • Composite outcome‡:
Total body cooling • Apgar ≤5 at 10 min • Major anomalies inotropes) 33% TH vs 25% 44% TH vs 62%
• Ventilation at 10 min • IUGR (<1.8 kg) control (NS) control (P = .01)
• Acidosis* (or pH 7.01-7.15 & BD 10- • Moribund • PPHN (not defined) 25% TH vs • Died: 24% TH vs 37%
15.9 + sentinel event) 22% control (NS) control (NS)
• Encephalopathy†
Lin et al79 2006 • ≥ 37 wk • Major anomalies • Hypotension (not defined) • Primary end point of
Selective head TH • Apgar ≤5 at 5 min • Severe PH (not defined) maintained with dopamine improved d 5-7 CT
• Acidosis on first ABG (pH <7.1 or BD >15) • PPHN not reported findings (P < .01)
• Encephalopathy† • Neonatal Behavioral
Neurologic assessment
d 7-10 (P < .01)
Gunn et al74 1998 • ≥37 wk • Major anomalies • Hypotension (MAP < 40 mm
Whole body TH • Acidosis (UA pH ≤ 7.09) • Metabolic diseases Hg) 0% TH vs 0% control
• Apgar ≤6 at 5 min • PPHN (needing iNO) 50%
• Encephalopathy† “minimal TH” vs 0% “mild
TH” vs 20% control
CoolCap80 2005 • ≥36 wk • ≥5.5 h of age • Hypotension (MAP < 40 mm • Composite outcome‡:
Selective head TH + • Apgar ≤5 at 10 min • Prophylactic anticonvulsants Hg) 55% TH vs 52% 55% TH vs 66%
mild systemic TH • Resuscitation at 10 min • Major anomalies control (NS) control (P = .01)
• Acidosis* cord or <60 min • Intracranial hemorrhage • PPHN not reported • Died: 33% TH vs 38%
• Encephalopathy† • IUGR (1.8 kg) • Respiratory distress (need for control (P = .05)
• Illness acuity deemed too high ventilation, CPAP or ECMO)
(neonatologist) 84% TH vs 78% control
Akisu et al81 2003 • ≥37 wk • ≥6 h of age • Hypotension (MAP < 45 mm • Primary outcome: CSF
Selective head TH + • Apgar ≤5 at 5 min • Metabolic disorders Hg) 0% TH vs 0% control platelet-activating
mild systemic TH • Acidosis cord or first ABG (pH <7.1 or BD >10) • Congenital or chromosomal (NS) factor.
• Encephalopathy† disorders • PPHN not reported
• Congenital infection
• Transitory drug depression
Shankaran et al82 2002 • ≥36 wk • ≥6 h of age • Hypotension (need for • Died: 22% TH vs 30%
Whole body TH • Apgar ≤5 at 10 min • Chromosomal/ congenital vasopressor) 56% TH vs control
• Ventilation at 10 min anomaly 30% control • Abnormal MRI 33% TH vs
• Acidosis* cord or <60 min (or pH 7.01-7.15 or • Severe IUGR ( < 1.8 kg) • PPHN (not defined) 33% TH vs 30% control
BD 10-15.9 + sentinel event) • Unlikely to survive 20% control
• Encephalopathy† • Neonatologist deemed
inappropriate to consent
Eicher et al83 2005 • ≥35 wk and 2000g • ≥6 h of age • Hypotension (d on inotropes) 5 • Neurologic outcomes not
Whole body TH • Encephalopathy† • Clinical sepsis, chorioamnionitis TH vs 2 control (P = .02) reported.
• Plus 2 of: • IUGR (<10th percentile) • PPHN (not defined) 29% TH vs
• Apgar ≤5 at 10 min • Congenital anomalies 16% control (NS)
• Resuscitation at 10 min • PPHN requiring iNO 16% TH
• Acidosis cord ≤7.0 or BD ≥13 (first pH <7.1) vs 3% control (P = .01)
• Fetal bradycardia, postnatal hypoxemia, or
hypotension
ABG, arterial blood gas; aEEG, amplitude integrated electroencephalogram; BD, base deficit; CPAP, continuous positive airway pressure; CSF, cerebrospinal fluid; ECMO, extracorporeal membrane oxygenation;
FiO2, fraction of inspired oxygen; IUGR, intrauterine growth restriction; ICE, Infant Cooling Evaluation; MAP, mean arterial pressure; NS, normal saline; PPHN, persistent pulmonary hypertension of the newborn;
UA, umbilical artery.
*Acidosis: pH <7 and/or base deficit >16 mmol/L unless otherwise specified.
†Encephalopathy: Moderate or severe on the basis of Sarnat Score.
‡Composite outcome: Death or severe neurodevelopmental impairment.
9.e1 Giesinger et al
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
■■ 2016 MEDICAL PROGRESS
Table II. Comparison of types of asphyxial injury and their characteristics19,20
Acute near-total asphyxia Partial prolonged asphyxia
Type of injury Single catastrophic event Repeated moderate exposure
Pattern of injury Subcortical nuclei in the thalamus and brainstem Cerebral white matter and non-CNS organs
Pathophysiology Acute damage to areas with highest metabolic requirements Gradual redistribution of blood to deep brain structures at the expense of other areas
CNS, central nervous system.
Table IV. Electrocardiogram grading of transient myo-
cardial ischemia51
Grade Severity Electrocardiogram finding
I Equivocal Flat or inverted T wave in 1 lead only
II Suggestive Flat or inverted T wave in several leads + abnormal Q
wave in any lead
III Moderate Flat or inverted T wave in several leads or bundle branch
block + abnormal Q + abnormal ST segments
IV Severe Classic segmental infarction pattern with abnormal Q
waves + markedly elevated ST segments
Hypoxic-Ischemic Encephalopathy and Therapeutic Hypothermia: The Hemodynamic Perspective 9.e2
FLA 5.4.0 DTD ■ YMPD8660_proof ■ October 11, 2016
You might also like
- Intracerebral Haemorrhage: Disease PrimersDocument18 pagesIntracerebral Haemorrhage: Disease PrimersMarlon VillanuevaNo ratings yet
- Cerebral Herniation Syndromes and Intracranial HypertensionFrom EverandCerebral Herniation Syndromes and Intracranial HypertensionMatthew KoenigNo ratings yet
- Encephalopaty Hipertensi Pmed JurnalDocument7 pagesEncephalopaty Hipertensi Pmed JurnalekaNo ratings yet
- Fetal and Neonatal Effects of N Acetylcysteine When Used - 2016 - The Journal oDocument16 pagesFetal and Neonatal Effects of N Acetylcysteine When Used - 2016 - The Journal oNiluh SukreniNo ratings yet
- The Intensivist's Perspective of Shock, Volume Management, and Hemodynamic MonitoringDocument16 pagesThe Intensivist's Perspective of Shock, Volume Management, and Hemodynamic MonitoringKarem YoHalyNo ratings yet
- Hypothermia-Ischemia Final Draft E-PortfolioDocument11 pagesHypothermia-Ischemia Final Draft E-Portfolioapi-317145308No ratings yet
- Captura de pantalla 2024-10-28 a la(s) 12.51.27 p.m.Document18 pagesCaptura de pantalla 2024-10-28 a la(s) 12.51.27 p.m.johegoj721No ratings yet
- Stroke PreventionDocument8 pagesStroke PreventionjaanhoneyNo ratings yet
- Fneur 10 00138 PDFDocument13 pagesFneur 10 00138 PDFnicNo ratings yet
- hipoglikemi dan strok hemoragicDocument7 pageshipoglikemi dan strok hemoragicSpongebob zzNo ratings yet
- Initial Diagnosis and Management of Acutely Elevated Intracranial PressureDocument8 pagesInitial Diagnosis and Management of Acutely Elevated Intracranial PressureGlessin MurilloNo ratings yet
- Posterior Reversible Encephalopathy Syndrome: A Review: Jai Shankar, DM, MSC, Jillian Banfield, PHDDocument7 pagesPosterior Reversible Encephalopathy Syndrome: A Review: Jai Shankar, DM, MSC, Jillian Banfield, PHDkidNo ratings yet
- Therapeutic Hypothermia in Children After Cardiac Arrest: Eview RticleDocument8 pagesTherapeutic Hypothermia in Children After Cardiac Arrest: Eview RticleIRINA SULEY TIRADO PEREZNo ratings yet
- Improving Outcome post-arrest-ILCOR statement-Perkins-Resuscitation-2024Document23 pagesImproving Outcome post-arrest-ILCOR statement-Perkins-Resuscitation-2024mcoghill3No ratings yet
- Wa0004.Document17 pagesWa0004.nhunhuochachNo ratings yet
- Ischemic Cerebral Stroke Case Report, Complications and Associated FactorsDocument5 pagesIschemic Cerebral Stroke Case Report, Complications and Associated Factorsfaradilla wiyandaNo ratings yet
- Biruh T Workeneh Hyponatremia Demystified IntegratingDocument17 pagesBiruh T Workeneh Hyponatremia Demystified IntegratingsaqqarazoserNo ratings yet
- Pi Is 1059131118301596Document6 pagesPi Is 1059131118301596juan.gomez5152No ratings yet
- Pediatric Neuroanesthesia: Sulpicio G. Soriano, MD, Elizabeth A. Eldredge, MD, Mark A. Rockoff, MDDocument16 pagesPediatric Neuroanesthesia: Sulpicio G. Soriano, MD, Elizabeth A. Eldredge, MD, Mark A. Rockoff, MDbuddy9568No ratings yet
- Aching Er 2017Document10 pagesAching Er 2017Anonymous Us5v7C6QhNo ratings yet
- Prolonged Paroxysmal Sympathetic Storming Associated With Spontaneous Subarachnoid HemorrhageDocument5 pagesProlonged Paroxysmal Sympathetic Storming Associated With Spontaneous Subarachnoid Hemorrhageiri_balNo ratings yet
- Perioperative Management of Thyroid DysfunctionDocument5 pagesPerioperative Management of Thyroid DysfunctionAnonymous ORleRrNo ratings yet
- MELAS Case ReportDocument12 pagesMELAS Case ReportIRENA GENINo ratings yet
- Fisiopatología EstatusDocument14 pagesFisiopatología EstatusDaniel LeivaNo ratings yet
- Shock Management in Children: Nora SoviraDocument6 pagesShock Management in Children: Nora Soviraminerva-larasatiNo ratings yet
- 2 PBDocument11 pages2 PBAttilio Del RossoNo ratings yet
- Drug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansDocument0 pagesDrug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansRajihah JihahNo ratings yet
- POTS Current Concepts Trends in CVMDocument5 pagesPOTS Current Concepts Trends in CVMmperlethNo ratings yet
- Mechanisms, Clinical Implications, and Treatment of Intradialytic HypotensionDocument7 pagesMechanisms, Clinical Implications, and Treatment of Intradialytic Hypotensionhemer hadyn calderon alvitesNo ratings yet
- 2 PBDocument13 pages2 PBsofia95yNo ratings yet
- "Triple H" Therapy For Aneurysmal Subarachnoid Haemorrhage: Real Therapy or Chasing Numbers?Document0 pages"Triple H" Therapy For Aneurysmal Subarachnoid Haemorrhage: Real Therapy or Chasing Numbers?ganpur01No ratings yet
- Nihms687466 PDFDocument14 pagesNihms687466 PDFyoiiiNo ratings yet
- Olavarria2016 PDFDocument5 pagesOlavarria2016 PDFNurul AzmiyahNo ratings yet
- Cerebro NeonatalDocument8 pagesCerebro NeonatalRodri EspinNo ratings yet
- Neurologic Aspects of Cardiac Emergencies - 2014 - Critical Care ClinicsDocument28 pagesNeurologic Aspects of Cardiac Emergencies - 2014 - Critical Care ClinicsDani Tames PedrazasNo ratings yet
- Hyponatremia in The Neurocritical Care PatientDocument10 pagesHyponatremia in The Neurocritical Care PatientAli JENDOUBINo ratings yet
- 1013 Vasoactive Agents in ShockDocument20 pages1013 Vasoactive Agents in Shockzeldaoftime67% (3)
- JurnalDocument9 pagesJurnalRifqi FathendraNo ratings yet
- Aminas NeonatosDocument19 pagesAminas NeonatosLobikark MXNo ratings yet
- Journal Homepage: - : IntroductionDocument12 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- HSA Aneurism+â-Ítica ICM 2014Document4 pagesHSA Aneurism+â-Ítica ICM 2014Ellys Macías PeraltaNo ratings yet
- Atow 464 00Document10 pagesAtow 464 00Mauricio P�rez Mac�asNo ratings yet
- Manzanares 2015Document10 pagesManzanares 2015Caro ReaNo ratings yet
- Critical Care Management of Potential Donors Clin Transplant 2009Document8 pagesCritical Care Management of Potential Donors Clin Transplant 2009Marisol Gallego DuqueNo ratings yet
- Turan 2014Document17 pagesTuran 2014zixzaxoffNo ratings yet
- Optimal PH Strategy For Hypothermic Circulatory Ar PDFDocument2 pagesOptimal PH Strategy For Hypothermic Circulatory Ar PDFKhairunnisa FitriNo ratings yet
- The Ductus Arteriosus A Refined ApproachDocument9 pagesThe Ductus Arteriosus A Refined ApproachHelenaFalconeNo ratings yet
- 2020 Birth Asphyxia - StatPearls - NCBI Bookshelf Jurnal 2Document4 pages2020 Birth Asphyxia - StatPearls - NCBI Bookshelf Jurnal 2Chiki CacaNo ratings yet
- AvocadoDocument16 pagesAvocadoKahinyaNo ratings yet
- Pi Is 0140673605601146Document1 pagePi Is 0140673605601146Novita Dewi LestariNo ratings yet
- Complications of Brain Tumors and Their TreatmentDocument18 pagesComplications of Brain Tumors and Their TreatmentBenedictus Yudha BaskaraNo ratings yet
- Antihypertensive Treatment and Cognitive Function: Another Tempest in A P Pot?Document3 pagesAntihypertensive Treatment and Cognitive Function: Another Tempest in A P Pot?Rifka NabilaNo ratings yet
- Diagnosis and Management of Subarachnoid HemorrhageDocument25 pagesDiagnosis and Management of Subarachnoid HemorrhageMisael ClintonNo ratings yet
- Study of Metabolic Syndrome and Diabetes Mellitus Among Ischemic Stroke Patients in A Tertiary Hospital, Northern KarnatakaDocument7 pagesStudy of Metabolic Syndrome and Diabetes Mellitus Among Ischemic Stroke Patients in A Tertiary Hospital, Northern KarnatakaIJAR JOURNALNo ratings yet
- Intradialitic HypotensionDocument7 pagesIntradialitic HypotensionanitaNo ratings yet
- HIEareviewforthe Clinician JAMA2015Document8 pagesHIEareviewforthe Clinician JAMA2015van anh nguyen huynhNo ratings yet
- BMJ 40 74 2Document8 pagesBMJ 40 74 2Enrique GómezNo ratings yet
- 2016 - CM Difficulties in The Diagnosis and Management ofDocument6 pages2016 - CM Difficulties in The Diagnosis and Management ofmihaelamocanNo ratings yet
- Articolo Sodio 6Document9 pagesArticolo Sodio 6Francesca BertaccaNo ratings yet
- Secondary HypertensionFrom EverandSecondary HypertensionAlberto MorgantiNo ratings yet
- Plagiarism Turnitin - Docx-2Document13 pagesPlagiarism Turnitin - Docx-2akshayajainaNo ratings yet
- Culture Data Upto July 16Document7 pagesCulture Data Upto July 16akshayajainaNo ratings yet
- Delivery Room Management of Asphyxiated Term and Near Term InfantsDocument13 pagesDelivery Room Management of Asphyxiated Term and Near Term InfantsakshayajainaNo ratings yet
- Approach To Conjunctivitis in NeonatesDocument8 pagesApproach To Conjunctivitis in NeonatesakshayajainaNo ratings yet
- Clinical Characteristics, Diagnosis, and Management Outcome of SurfactantDocument7 pagesClinical Characteristics, Diagnosis, and Management Outcome of SurfactantakshayajainaNo ratings yet
- JNB 2 142Document6 pagesJNB 2 142akshayajainaNo ratings yet
- Mercuri 2017Document13 pagesMercuri 2017akshayajainaNo ratings yet
- Finkel 2017Document11 pagesFinkel 2017akshayajainaNo ratings yet
- Cyanotic Spells UHL Childrens Hospital GuidelineDocument6 pagesCyanotic Spells UHL Childrens Hospital GuidelineakshayajainaNo ratings yet
- Ogino and Wilson 2004Document16 pagesOgino and Wilson 2004akshayajainaNo ratings yet
- The Systemic Review of CV Junction TuberculosisDocument8 pagesThe Systemic Review of CV Junction TuberculosisakshayajainaNo ratings yet
- Maas 2007Document4 pagesMaas 2007akshayajainaNo ratings yet
- Ontimmunol09 01837Document17 pagesOntimmunol09 01837akshayajainaNo ratings yet
- Rev 00138Document11 pagesRev 00138akshayajainaNo ratings yet
- Hyperleukocytosis: Emergency Management: The Indian Journal of Pediatrics November 2012Document6 pagesHyperleukocytosis: Emergency Management: The Indian Journal of Pediatrics November 2012akshayajainaNo ratings yet
- Nursing Care PlanDocument22 pagesNursing Care Planaln00550% (2)
- Fluid Therapy in Emergency DepartmentDocument5 pagesFluid Therapy in Emergency DepartmentAnnisa Fitri AnggrainiNo ratings yet
- Physiological Modeling - Final Project (Circulatory System)Document18 pagesPhysiological Modeling - Final Project (Circulatory System)Joshua DamianNo ratings yet
- Cardiac Physiology NotesDocument11 pagesCardiac Physiology Notespunter11100% (1)
- NCP For CHDDocument2 pagesNCP For CHDMonica Rivera100% (1)
- NSG 117 PerfusionDocument55 pagesNSG 117 PerfusionAnonymous UJEyEsNo ratings yet
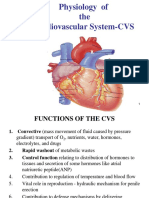
- Physiology of The Cardiovascular System-CVSDocument56 pagesPhysiology of The Cardiovascular System-CVSAmanuel Maru50% (2)
- Cardiac OutputDocument30 pagesCardiac OutputGanesh VignaniNo ratings yet
- Heart Failure Nursing Care Plans - 15 Nursing Diagnosis - NurseslabsDocument13 pagesHeart Failure Nursing Care Plans - 15 Nursing Diagnosis - NurseslabsJOSHUA DICHOSONo ratings yet
- Acute Decompensated Heart FailureDocument43 pagesAcute Decompensated Heart FailureZit HibaNo ratings yet
- NCP Decreased Cardiac OutputDocument2 pagesNCP Decreased Cardiac OutputYamete KudasaiNo ratings yet
- Decreased Cardiac OutputDocument5 pagesDecreased Cardiac Outputshuang81No ratings yet
- TAPSE AgainDocument8 pagesTAPSE Againomotola ajayiNo ratings yet
- HDO Leaflet PTDocument12 pagesHDO Leaflet PTErickson Fabian CastilloNo ratings yet
- 1ST Proff MBBS Papers (2021-11)Document66 pages1ST Proff MBBS Papers (2021-11)drbishalchowdhury13No ratings yet
- How I Personalize Fluid Therapy in Septic Shock?: Review Open AccessDocument11 pagesHow I Personalize Fluid Therapy in Septic Shock?: Review Open AccessGian CarloNo ratings yet
- Obat-Obat KardiovaskulerDocument50 pagesObat-Obat KardiovaskulerMuhammad IqbalNo ratings yet
- Decreased Cardiac Output NCPDocument2 pagesDecreased Cardiac Output NCPbaba69baba100% (1)
- Dopamine Drug StudyDocument3 pagesDopamine Drug StudyNicole Soo78% (9)
- Chap+12+CO, VRegul+Fall11 1Document17 pagesChap+12+CO, VRegul+Fall11 1Drbee100% (1)
- Cardiogenic Shock NCLEX Review QuizDocument6 pagesCardiogenic Shock NCLEX Review QuizRegie Marie EvangelistaNo ratings yet
- Archer Critical Care ConceptDocument21 pagesArcher Critical Care ConceptJoanna Ephraim CruzNo ratings yet
- MANUAL DE SERVICIO - C70 COMENDocument86 pagesMANUAL DE SERVICIO - C70 COMENhealthasuntosNo ratings yet
- 4conference mv2 HKR PDFDocument87 pages4conference mv2 HKR PDFekafithraNo ratings yet
- ACSM Certkiller 040-444 v2017-11-28 by Hammond 190qDocument78 pagesACSM Certkiller 040-444 v2017-11-28 by Hammond 190qSwisskelly1100% (1)
- MS Cardiac SurgeryDocument99 pagesMS Cardiac SurgeryFazeela Naveen100% (1)
- The Eight Vital Signs of Patient MonitoringDocument6 pagesThe Eight Vital Signs of Patient MonitoringmelianyyessicaNo ratings yet
- Circulation SEQs With KeysDocument15 pagesCirculation SEQs With KeysMudassar Roomi100% (1)
- Approach To Shock and Hypotension in NeonatesDocument6 pagesApproach To Shock and Hypotension in NeonatesReshmiNo ratings yet
- Devices Used in ICU: Critical Care NursingDocument95 pagesDevices Used in ICU: Critical Care NursinghendranatjNo ratings yet