Professional Documents
Culture Documents
Unrecognized Diabetes Among Hospitalized Patients: Nal Article
Unrecognized Diabetes Among Hospitalized Patients: Nal Article
Uploaded by
amandaribeirouOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Unrecognized Diabetes Among Hospitalized Patients: Nal Article
Unrecognized Diabetes Among Hospitalized Patients: Nal Article
Uploaded by
amandaribeirouCopyright:
Available Formats
E p i d e m i o I o g y / H e a 11 h Se r v i ce s/ P sy ch o so cia I R e s e a r c h
N A L A R T I C L E
Unrecognized Diabetes Among
Hospitalized Patients
CLARESA S. LEVETAN, MD MARY KASS, MD pital. Those patients in whom diabetes was
MAUREEN PASSARO, MD ROBERT E. RATNER, MD the primary reason for their hospital admis-
KATHLEEN JABLONSKI, PHD sion were excluded from further analysis.
Medical records of hyperglycemic patients
without a diagnosis of diabetes at the time
of admission were further reviewed.
A checklist was developed for the pur-
OBJECTIVE — To evaluate the hospital care rendered to hyperglycemic individuals who did poses of data collection. Frequency tables
not have a diagnosis of diabetes before admission. were run on demographic and outcomes
data, and percentages were calculated
Downloaded from http://diabetesjournals.org/care/article-pdf/21/2/246/585515/21-2-246.pdf by guest on 07 June 2024
RESEARCH DESIGN A N D M E T H O D S — A total of 1,034 consecutively hospitalized based on the following information:
adult patients at a 750-bed inner-city teaching hospital were evaluated. Patients with one or
more plasma glucose values >200 mg/dl were identified by the laboratory data system on a daily
basis. Patients without a diagnosis of diabetes at the time of admission were evaluated to deter- 1. Presence of diabetes in the medical
mine if and how physicians addressed the hyperglycemia, whether a new diagnosis of diabetes problem list or included in the initial
was made during admission, and whether follow-up was planned to address the hyperglycemia. history by the admitting physician.
2. Presence of more than one glucose
RESULTS — After excluding patients who were admitted for a primary diagnosis of diabetes, value >200 mg/dl.
37.5% of all hyperglycemic medical patients and 33% of hyperglycemic surgical patients were 3. Value of the peak glucose.
without a diagnosis of diabetes at the time of admission. These patients had a mean peak glucose 4. Documentation in the daily progress
of 299 mg/dl, and 66% had two or more elevated values during their hospitalization. Fifty-four notes of diabetes as a possible diagnosis.
percent received insulin therapy, and 59% received bedside glucose monitoring, yet 66% of daily 5. Documentation of hyperglycemia in
patient progress notes failed to comment on the presence of hyperglycemia or diabetes. Diabetes
the daily progress notes.
was documented in only three patients (7.3%) as a possible diagnosis in the daily progress notes.
6. Orders for medical therapy for the
CONCLUSIONS — Despite marked hyperglycemia, most medical records made no reference treatment of hyperglycemia.
to the possibility of unrecognized diabetes. Given the average delay of a decade between the 7. Orders for bedside glucose monitoring.
onset and diagnosis of type 2 diabetes, further evaluation of hyperglycemic hospitalized patients 8. Documentation of hyperglycemia in
may present an important opportunity for earlier detection and the initiation of therapy the discharge summary.
9. Documentation of follow-up plans for
further diabetes work-up or therapy in
thefinalprogress note or the discharge
H
alf of the 16 million Americans with and to determine whether such patients are
diabetes are imdiagnosed (1-3). The summary.
appropriately evaluated and treated.
diagnosis of diabetes is frequently not
considered until another medical problem RESEARCH DESIGN AND RESULTS— Of the 1,034 hospitalized
occurs and hyperglycemia is found inci- METHODS — We prospectively evalu- adult patients, 130 (12.6%) had one or
dentally. As a result, the diagnosis of type 2 ated all 1,034 consecutively hospitalized more documented plasma glucose values
diabetes is estimated to be delayed by an adult patients during a single week at an >200 mg/dl. Fifteen patients (11.5%) had
average of 10 years after the actual onset of inner-city tertiary-care teaching hospital diabetes documented as the principal rea-
the disease (4,5). with a capacity of 750 beds. Patients with son for hospital admission and were
Despite the fact that more than 4 mil- one or more plasma glucose values >200 excluded from further study; the other 115
lion Americans with a known diagnosis of mg/dl were identified by the laboratory with hyperglycemia served as the study
diabetes are hospitalized annually in this data system on a daily basis. In addition to population for further analysis. Those with
country, little is known about the preva- the glucose value, the following data were preexisting diabetes plus those recognized
lence of hyperglycemia within the hospi- obtained: name, medical record number, as having new-onset diabetes at the time of
talized population who do not have a medical service, patient age, and sex. admission constituted 64% (74/115) of the
diagnosis of diabetes before admission (6). The medical records of these patients hyperglycemic population (Fig. 1).
We set forth to evaluate the hospital care were evaluated after their discharge to deter- Table 1 describes the distribution of
rendered to these hyperglycemic individu- mine if diabetes was a diagnosis that was hyperglycemic patients by medical service.
als without a prior diagnosis of diabetes present at the time of admission to the hos- Thirty-six percent (41/115) of patients were
previously unrecognized as having a disorder
of glucose metabolism. Of the 41 patients
From the Medlantic Research Institute (C.S.L., M.P, K.J., R.E.R.) and the Washington Hospital Center (M.K.), with hyperglycemia in whom there was no
Washington, DC.
Address correspondence and reprint requests to Dr. Claresa Levetan, Medlantic Research Institute, 650
documentation of diabetes existing before
Pennsylvania Ave., SE, Suite 50, Washington, DC 20003. hospital admission, 23 (56.1%) were men
Received for publication 21 May 1997 and accepted in revised form 21 October 1997. and 18 (43.9%) were women (Table 2). Of
246 DIABETES CARE, VOLUME 21, NUMBER 2, FEBRUARY 1998
Levetan and Associates
C O N C L U S I O N S — W e found that
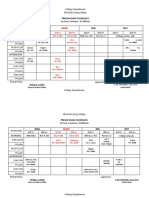
1034 one-third of all hyperglycemic patients on
Hospitalized both the medical and surgical services had
Patients no prior history of diabetes. Sixty-six per-
cent of these hyperglycemic individuals
had two or more elevated glucose values.
Despite therapeutic intervention with
insulin in more than half of our patients,
there was almost never documentation
130(13%) regarding the hyperglycemia and rarely was
Laboratory Documented diabetes a diagnostic consideration.
Glucose > 200 mg/dl
We believe that physicians assumed
that the hyperglycemia was a transient find-
ing that resulted from the stress of acute ill-
ness rather than considering the diagnosis
15(11.5%) 115(88.5%) of unrecognized diabetes. Given the pro-
Diabetes as
Downloaded from http://diabetesjournals.org/care/article-pdf/21/2/246/585515/21-2-246.pdf by guest on 07 June 2024
Diabetes as found delay in the diagnosis of type 2 dia-
Primary Secondary betes nationwide, we believe that it is a
Diagnosis Diagnosis common occurrence for physicians to over-
look hyperglycemia, and our findings are,
therefore, not unique to this institution or
geographic region (4,5).
There are no unique diagnostic criteria
41 (35.7%) or recommendations for making a defini-
Diabetes present Diabetes not present tive diagnosis of diabetes in the stressed
on admission on admission state. All of the patients identified had glu-
cose values >200 mg/dl and met the labo-
ratory criteria for diabetes established by
the National Diabetes Data Group, the
World Health Organization, and the Amer-
Chart review of ican Diabetes Association (7-11).
Patients with Potentially Despite the well-defined pathophysiol-
Unrecognized Diabetes ogy of intercurrent illness and surgery on
serum glucose, stress hyperglycemia has
Figure 1—Schematic ojhospitalized patients evaluated for hyperglycemia. eluded consistent documentation (12-27).
Although impaired carbohydrate metabo-
lism resulting in hyperglycemia is seen in
the 41 patients, 27 (65.9%) had two or more insulin coverage for their elevated glucose patients both with and without diabetes,
documented glucose values >200 mg/dl values, of which two patients (5%) were studies have also demonstrated that stress
with a mean peak glucose of 299 mg/dl with subsequently placed on definitive diabetes can also result in diminished glucose values,
a range of 202-503 mg/dl. The mean age therapy during admission (Table 3). Two and patients not given sufficient exogenous
among these patients was 61 years. patients (4.9%) received bedside glucose glucose can develop hypoglyeemia and
There was no physician documenta- monitoring but no insulin coverage, and ketosis in times of stress (9-27). Stress
tion that hyperglycemia or diabetes was seventeen patients (41.5%) had no medical hyperglycemia should theoretically result
present in 27 (65.9%) of the 41 records orders reflecting the recognition or treat- in higher glycemic excursions in diabetic
(Fig. 2). Eleven records (26.8%) did not use ment of hyperglycemia. individuals than in nondiabetic individuals
the word diabetes, but described "hyper-
glycemia" or an "increased finger stick glu-
cose" value. Only three records (7.3%) Table 1—The distribution of hyperglycemic patients by medical service
mentioned diabetes as a diagnostic possi-
bility. Other than the three records in which
diabetes was considered, none of the daily Diabetes Diabetes Unrecognised
Glucose recognized unrecognized at admission
progress notes or discharge summaries dis-
Service >200 mg/dl before or at admission at admission
cussed plans for the further evaluation or
specific management of hyperglycemia after n 115 74 41 —
hospital discharge. Medicine 66 40 25 37.5
Although 66% of the medical records Surgery 48 32 16 33
did not mention diabetes or hyperglycemia, Gynecology 2 1 1 50
22 (54%) of the 41 patients received both Podiatry 1 1 0 0
bedside glucose monitoring and regular Data are n or %.
DIABETES CARE, VOLUME 21, NUMBER 2, FEBRUARY 1998 247
Unrecognized diabetes in hospitalized patients
Table 2—Characteristics of hyperglycemic tality rates were seen during the 3-year fol- Table 3—Therapeutic intervention for
patients without a prior diagnosis of diabetes low-up period for patients in whom intra- patients with hyperglycemia and without a
venous insulin, followed by multiple daily prior history of diabetes
injections, was initiated in the hospital and
Sex (%) (M/F) 56.1/43.9
continued as an outpatient (29-31).
Age (years) 61±18(27-92) Intervention Percentage
Although dozens of medications have
Mean peak glucose (mg/dl) 299 (202-503)
been described as inducing diabetes, there Received insulin treatment and 53.6
Patients with two or 65.9
has been little documented about the bedside glucose monitoring
more glucose values
glycemic status of patients before the initi- Received bedside monitoring 4.9
>200 mg/dl (%) without insulin treatment
ation of the offending drugs. Cortico-
steroids have been evaluated as a means of No medical orders 41.5
unmasking impaired glucose tolerance, but for hyperglycemia
among normal controls, only 3% had a
because of a relative or absolute deficiency positive glucose tolerance test when pre-
of endogenous insulin. treated with corticosteroids (32). Studies of
corticosteroid-treated individuals have
Downloaded from http://diabetesjournals.org/care/article-pdf/21/2/246/585515/21-2-246.pdf by guest on 07 June 2024
Husband et al. (28) followed a group of budget (37). Delays in the diagnosis of dia-
hospitalized patients with acute myocardial found that <20% of steroid-treated indi- betes carry with it substantialfinancialand
infarction with newly recognized hyper- viduals develop diabetes (33,34). health ramifications. Further study is
glycemia. Two months after hospital dis- It is critical that diabetes be diagnosed as needed to define differences between the
charge, patients were evaluated with early as possible, since diabetic complica- hospitalized patient population with tran-
glucose tolerance testing with findings that tions frequently occur before the diagnosis sient stress-induced hyperglycemia and
an admission glucose value of ^ 180 mg/dl of type 2 diabetes. More than 20% of the those with unrecognized diabetes.
predicted undiagnosed diabetes rather than individuals with diabetes have retinopathy at We believe that the failure to consider
stress hyperglycemia (28). Although stress the time of diagnosis, and it is often their the possibility of diabetes represents a
can account for hyperglycemia, our patient retinopathy eye findings that lead to the missed window of opportunity for making
population had glucose values in a range subsequent diagnosis of diabetes (4,5). The an earlier diagnosis and for initiating inter-
that warrants the consideration for a diag- prevalence of unrecognized diabetes remains ventions that may delay the devastating
nosis of diabetes rather than the assump- extremely high. By 65 years of age, 18.7% of complications of this disease. We recom-
tion of stress hyperglycemia. the population has diabetes, yet half remain mend that physicians assume that hypergly-
The Diabetes Insulin-Glucose in Acute undiagnosed (35). Regardless of the etiology, cemia is diabetes until they prove otherwise.
Myocardial Infarction (DIGAMI) series persistent hyperglycemia leads to the accel-
underscores the importance of aggressive eration of both microvascular and macrovas-
early intervention in the management of cular disease (36). References
hyperglycemic patients who have been In the U.S., expenditures resulting 1. U.S. Department of Health and Human Ser-
vices: Diabetes in the United States: A Strategy
admitted with suspected myocardial infarc- from the morbidity of patients with dia- for Prevention 1993. U.S. Department of
tion, including those without a previous betes exceed $100 billion per year and Health and Human Services, Public Health
history of diabetes. Significantly lower mor- account for 15% of the entire health care Service, Centers for Disease Control and
Prevention, National Center for Chronic
Disease Prevention and Health Promotion,
Division of Diabetes Translation, 1993
27% 2. Harris MI, Hadden WC, Knowler WC,
Bennett PH: Prevalence of diabetes and
impaired glucose tolerance and plasma glu-
cose levels in the U.S. population aged
20-74 yr. Diabetes 36:523-534, 1987
3. Harris MI: Undiagnosed NIDDM: clinical
and public health issues. Diabetes Care
16:642-652, 1993
4. Harris MI: Classification, diagnostic criteria,
and screening for diabetes. In Diabetes in
America. 2nd ed. Harris MI, Cowie CC,
Stern MR Boyko EJ, Reiber GE, Bennett PH,
66% Eds. Washington, DC, U.S. Govt. Printing
Office, 1995, p. 15-35 (NIH publ. no. 95-
1468)
5. Harris MI, Klein R, Welbom TA, Knuiman
• No mention of diabetes or hyperglycemia MW: Onset of NIDDM occurs at least 4 to
7 years before clinical diagnosis. Diabetes
D Diabetes mentioned
Care 15:815-819, 1992
ID Hyperglycemia mentioned 6. U.S. National Center for Health Statistics:
1995 National Hospital Discharge Survey
Figure 2—Documentation of diabetes or hyperglycemia in the physicians' daily progress notes. (Public Use Data Tapes). U.S. Department
248 DIABETES CARE, VOLUME 21, NUMBER 2, FEBRUARY 1998
Levetan and Associates
of Health and Human Services, Washing- sult Clin Psychol 55:529-533,1987 29. Malmberg K, Ryden I, Iiamsten A, Herlitz J,
ton, DC, 1995 18. Chase HP, Jackson GG: Stress and sugar con- Walatdenstrom A, Wedel H: Effect of insulin
7. Lustman PJ, Gavard JA: Psychosocial trol in children with insulin-dependent dia- treatment on cause-specific one-year mor-
aspects of diabetes adult populations. In betes mellitus. J Pediatr 98:1011-1013,1981 tality and morbidity in diabetic patients with
Diabetes in America. 2nd ed. Harris MI, 19. Hanson CL, Pichert JW: Perceived stress acute myocardial infarction: DIGAMI Study
Cowie CC, Stem MP, Boyko EJ, Reiber GE, and diabetes control in adolescents. Health Group, Diabetes Insulin-Glucose in Acute
Bennett PH, Eds. Washington, DC, U.S. Psychol 5:439-452, 1986 Myocardial Infarction. Eur Heart J 17:
Govt. Printing Office, 1995, p. 507-517 20. Vandenbergh RL, Sussman KE, Titus CC: 1337-1344,1996
(NIHpubl.no. 95-1468) Effects of hypnotically induced acute emo- 30. Malmberg K for the DIGAMI Study Group:
8. World Health Organization: Diabetes Melli- tional stress on carbohydrate-lipid metabo- Prospective randomized study of intensive
tus: Report oja WHO Study Group. Geneva, lism in patients with diabetes mellitus. insulin treatment on long-term survival after
World Health Org., 1985, p. 1-113 (Tech. Psychosom Med 28:382-390, 1966 acute myocardial infarction in patients with
Rep. Ser.,no. 727) 21. Vandenbergh RL, Sussman KE, Vaughan diabetes mellitus. BMJ 314:1512-1515,
9. World Health Organization: Report of the GD: Effects of combined physical-anticipa- 1997
Expert Committee on Diabetes. Geneva, tory stress on carbohydrate-lipid metabo- 31. Malmberg K, Ryden L, Efendic S, Herlitz J,
World Health Org., 1985 (Tech. Rep. Ser, lism in patients with diabetes mellitus. Nicol P, Waldenstrom A, Wedel H, Welin L:
no. 646) Psychosomatxcs 8:16-19,1967 Randomized trail of insulin-glucose infu-
Downloaded from http://diabetesjournals.org/care/article-pdf/21/2/246/585515/21-2-246.pdf by guest on 07 June 2024
10. National Diabetes Data Group: Classifica- 22. Greydanus DE, Hofmann AD: Psychological sion followed by subcutaneous insulin
tion and diagnosis of diabetes mellitus and factors in diabetes mellitus: a review of the treatment in diabetic patients with acute
other categories of glucose intolerance. Dia- literature with emphasis on adolescence. myocardial infarction (DIGAMI Study):
betes 28:1039-1057, 1979 AmJDis Child 133:1061-1088, 1979 effects on mortality at 1 year. J Am Coll Car-
11. The Expert Committee on the Diagnosis 23. Delamater AM, BubbJ, Kurtz SM, KuntzeJ, diol 26:57-64, 1995
and Classification of Diabetes Mellitus: Smith JA, White NH, Santiago JV: Physio- 32. Fajans SS, Conn JW: An approach to the
Report of the Expert Committee on the logic responses to acute psychological stress prediction of diabetes mellitus by modifi-
Diagnosis and Classification of Diabetes Mel- in adolescents with type I diabetes mellitus. cation of the glucose tolerance test with
litus. Diabetes Care 20:1183-1197,1997 JPediatrPsychol 13:69-86, 1988 cortisone. Diabetes 3:296-304, 1954
12. Gavin LA: Management of diabetes mellitus 24. Gilbert BO, Johnson SB, SilversteinJ, Mal- 33. Weisz A, Ratner R: Factors in renal trans-
during surgery. West] Med 151:525-529, one J: Psychological and physiological plant-induced diabetes mellitus (Abstract).
1989 responses to acute laboratory stressors in Diabetes 35:72A, 1986
13. Gavin LA: Perioperative management of insulin-dependent diabetes mellitus ado- 34. Landy HJ, Isada NB, McGinnis J, Ratner R,
the diabetic patient. Endocrinol Metab Clin lescents and non-diabetic controls. ] Pediatr Grossman JH: The effect of chronic steroid
North Am 21:457-475, 1992 Psychol 14:577-591, 1989 therapy on glucose tolerance in pregnancy.
14. Hirsch IB, McGill JB: Role of insulin man- 25. Kemmer FW, Bisping R, Steingruber HJ, AmJObstetGynecol 159:612-615, 1988
agement of surgical patients with diabetes Baar H, Hardtmann F, Schlaghecke R, Berger 35. Harris MI, Hadden WC, Knowler WC,
mellitus. Diabetes Care 13:980-991, 1990 M: Psychological stress and metabolic con- Bennett PH: Prevalence of diabetes and
15. Hirsch IB, Paauw DS, Brunzell J: Inpatient trol in patients with type I diabetes mellitus. impaired glucose tolerance and plasma glu-
management of adults with diabetes. Dia- NEnglJ Med 314:1078-1084, 1986 cose levels in the U.S. population aged
betes Care 18:870-878, 1995 26. Goetsch VL, Wiebe DJ, Vetum LG, Van 20-74 yr. Diabetes 36:523-534, 1987
16. Gonder-Frederick LA, Carter WR, Cox DJ, Dorsten B: Stress and blood glucose in type 36. Haffner SM, Stem MP, Hazuda HP, Mitchell
Clarke WL: Environmental stress and blood II diabetes mellitus. Behav Res Ther BD, Patterson JK: Cardiovascular risk fac-
glucose change in insulin-dependent dia- 28:531-537, 1990 tors in confirmed prediabetic individuals:
betes mellitus. Health Psychol 9:503-515, 27. Fletcher J, Langman MJS, Kellock RK: does the clock for coronary heart disease
1990 Effect of surgery on blood-sugar levels in start ticking before the onset of clinical dia-
17. Hanson CL, Henggeler SW Burghen GA: diabetes mellitus. Lancet ii:52-55, 1965 betes? JAMA 263:2892-2898, 1990
Social competence and parental support as 28. Husband DJ, Alberti KG, Julian DG: Stress 37. Rubin RJ, Altman WM, Mendelson DN:
mediators of the link between stress and hypergycaemia during acute myocardial Health care expenditures for people with
metabolic control in adolescents with infarction: an indicator of pre-existing dia- diabetes mellitus, 1992. J Clin Endocrinol
insulin-dependent diabetes mellitus. J Con- betes? Lancet ii:179-181,1983 Metab 78:809A-809E 1994
DIABETES CARE, VOLUME 21, NUMBER 2, FEBRUARY 1998 249
You might also like
- Speech & Language Therapy in Practice, Summer 2011Document36 pagesSpeech & Language Therapy in Practice, Summer 2011Speech & Language Therapy in Practice100% (1)
- Management of Diabetes and Hyperglycemia in Hospitals: S C S S. B, M F. M, A A, E P. S, R G. S, I B. H, D H W CDocument39 pagesManagement of Diabetes and Hyperglycemia in Hospitals: S C S S. B, M F. M, A A, E P. S, R G. S, I B. H, D H W CMarshell TendeanNo ratings yet
- Clinical Characteristics of Hyperglycemic Crises in Patients Without A History of DiabetesDocument6 pagesClinical Characteristics of Hyperglycemic Crises in Patients Without A History of DiabetesDewanggaWahyuPrajaNo ratings yet
- DM en UciDocument12 pagesDM en UciJuan Camilo MateusNo ratings yet
- Insulin Management in HospitalDocument8 pagesInsulin Management in HospitalHannahNo ratings yet
- Inpatient ReadmissionsDocument6 pagesInpatient ReadmissionsoanadubNo ratings yet
- The Diabetes Education Study A Controlled Trial ofDocument10 pagesThe Diabetes Education Study A Controlled Trial ofJefferson AvilaNo ratings yet
- Canadian Journal of Diabetes: 2018 Clinical Practice GuidelinesDocument9 pagesCanadian Journal of Diabetes: 2018 Clinical Practice Guidelinesamar singhNo ratings yet
- Clinical Course of Diabetic Ketoacidosis in Hypertriglyceridemic Pancreatitis Pancreas 2015Document4 pagesClinical Course of Diabetic Ketoacidosis in Hypertriglyceridemic Pancreatitis Pancreas 2015América FloresNo ratings yet
- Identification of Two Novel Subgroups in Patients With Diabetes Mellitus and Their Association With Clinical Outcomes - A Two Step Cluster AnalysisDocument13 pagesIdentification of Two Novel Subgroups in Patients With Diabetes Mellitus and Their Association With Clinical Outcomes - A Two Step Cluster AnalysisLeidy Nayerli Garcia RodriguezNo ratings yet
- Stress Hyperglycaemia: SeminarDocument10 pagesStress Hyperglycaemia: SeminarPauPatiñoNo ratings yet
- Original Article: Nancy J. Wei, MD, MMSC David M. Nathan, MD Deborah J. Wexler, MD, MSCDocument8 pagesOriginal Article: Nancy J. Wei, MD, MMSC David M. Nathan, MD Deborah J. Wexler, MD, MSCAnggie AnggriyanaNo ratings yet
- Endoscopic Intervention and Cholecystectomy in Pregnant Women With Acute Biliary Pancreatitis Decreases Early ReadmissionsDocument19 pagesEndoscopic Intervention and Cholecystectomy in Pregnant Women With Acute Biliary Pancreatitis Decreases Early ReadmissionsCarlos Altez FernandezNo ratings yet
- Ijcmr 3211 v1 PDFDocument5 pagesIjcmr 3211 v1 PDFAtul DwivediNo ratings yet
- EndocrinoDocument15 pagesEndocrinoMichelle ElizaldeNo ratings yet
- 2015 Updates On The Management of Diabetes in Dialysis PatientsDocument22 pages2015 Updates On The Management of Diabetes in Dialysis Patientsguanyulin01No ratings yet
- Diabetes Case Report 3Document6 pagesDiabetes Case Report 3Astha TimothyNo ratings yet
- Decition Makin ElderlyDocument15 pagesDecition Makin ElderlyDANNo ratings yet
- Carter 2020Document6 pagesCarter 2020oanadubNo ratings yet
- Indikasi Insulin InfusionDocument7 pagesIndikasi Insulin InfusionnikeNo ratings yet
- Hypoglycemia After Gastric Bypass Surgery. Current Concepts and Controversies 2018Document12 pagesHypoglycemia After Gastric Bypass Surgery. Current Concepts and Controversies 2018Rio RomaNo ratings yet
- Wang2015 1 PDFDocument10 pagesWang2015 1 PDFAdriani HartantoNo ratings yet
- Documented Lifestyle Education Among Young Adults With Incident HypertensionDocument9 pagesDocumented Lifestyle Education Among Young Adults With Incident HypertensionPanji Tutut AnggraeniNo ratings yet
- Factores Asociados A La Adherencia Al Autocontrol de La GlucemiaDocument8 pagesFactores Asociados A La Adherencia Al Autocontrol de La GlucemiaLeidy Milena Hernandez BarraganNo ratings yet
- Clozapina y Su Relacion Con El Sindrome MetabolicoDocument7 pagesClozapina y Su Relacion Con El Sindrome MetabolicoHéctor GuzmánNo ratings yet
- Assessment of Knowledge of Diabetes Among Diabetic and Non-Diabetic IndividualsDocument5 pagesAssessment of Knowledge of Diabetes Among Diabetic and Non-Diabetic IndividualsCharlosNo ratings yet
- Complicaciones y Mortalidad en Pacientes Con Ezq y DBTDocument11 pagesComplicaciones y Mortalidad en Pacientes Con Ezq y DBTDanitza YhovannaNo ratings yet
- J Clin Endocrinol Metab. 2012 97 16 38Document23 pagesJ Clin Endocrinol Metab. 2012 97 16 38rizwan234No ratings yet
- Original Research Article: Vitan Patel, Minal Shastri, Nisha Gaur, Prutha Jinwala, Abhishek Y. KadamDocument5 pagesOriginal Research Article: Vitan Patel, Minal Shastri, Nisha Gaur, Prutha Jinwala, Abhishek Y. KadamTam LyNo ratings yet
- Dysglycemiaandglucose Controlduringsepsis: Mark P. Plummer,, Adam M. DeaneDocument11 pagesDysglycemiaandglucose Controlduringsepsis: Mark P. Plummer,, Adam M. DeanePaul GuijarroNo ratings yet
- 1408 FullDocument7 pages1408 FullFrancisca Collao FNo ratings yet
- 1 s2.0 S1877593409000691 MainDocument5 pages1 s2.0 S1877593409000691 MainDerison MarsinovaNo ratings yet
- Disgkicemias 3Document7 pagesDisgkicemias 3Paul GuijarroNo ratings yet
- Impact of A Nurse Short Message Service Intervention For Patients With DiabetesDocument6 pagesImpact of A Nurse Short Message Service Intervention For Patients With DiabetesFatima Akbar.No ratings yet
- Ni Hms 494378Document27 pagesNi Hms 494378Uswatun HasanahNo ratings yet
- Jurnal AKIDocument7 pagesJurnal AKIAnonymous Vz9teLNo ratings yet
- Dia Care-2014-Dall-3172-9Document8 pagesDia Care-2014-Dall-3172-9jcc3417No ratings yet
- Prevalence, Risk Factors, Adherence and Non Adherence in Patient With Chronic Kidney Disease: A Prospective StudyDocument7 pagesPrevalence, Risk Factors, Adherence and Non Adherence in Patient With Chronic Kidney Disease: A Prospective StudyRanitaRahmaniarNo ratings yet
- Management of Hyperglycemia and Enteral Nutrition in The Hospitalized PatientDocument8 pagesManagement of Hyperglycemia and Enteral Nutrition in The Hospitalized Patienthenry hernandezNo ratings yet
- Medicine: Allopurinol Use and Type 2 Diabetes Incidence Among Patients With GoutDocument7 pagesMedicine: Allopurinol Use and Type 2 Diabetes Incidence Among Patients With GoutGrady CoolNo ratings yet
- Correlates of Quality of Life in Older Adults With DiabetesDocument5 pagesCorrelates of Quality of Life in Older Adults With DiabetesGibran IlhamNo ratings yet
- Weight-Based, Insulin Dose - Related Hypoglycemia in Hospitalized Patients With DiabetesDocument6 pagesWeight-Based, Insulin Dose - Related Hypoglycemia in Hospitalized Patients With DiabetesPuri PuriNo ratings yet
- Ables 2016Document8 pagesAbles 2016oanadubNo ratings yet
- Weight-Based, Insulin Dose - Related Hypoglycemia in Hospitalized Patients With DiabetesDocument6 pagesWeight-Based, Insulin Dose - Related Hypoglycemia in Hospitalized Patients With DiabetesPuri PuriNo ratings yet
- Congestive Heart Failure in Type 2 Diabetes: Prevalence, Incidence, and Risk FactorsDocument6 pagesCongestive Heart Failure in Type 2 Diabetes: Prevalence, Incidence, and Risk FactorsFini Riski Aulia SagalaNo ratings yet
- Artikel Pubmed 3Document6 pagesArtikel Pubmed 3Sofa AmaliaNo ratings yet
- FREQUENCY - OF - NEPHROPATHY - AND - ITS - RELATION - TO - METAB (Diskusi)Document5 pagesFREQUENCY - OF - NEPHROPATHY - AND - ITS - RELATION - TO - METAB (Diskusi)lusiyanaNo ratings yet
- Tests of Glycemia in Diabetes: D E. G, R R. L, R A. L, J I. M, D N, C M. P, D B. SDocument13 pagesTests of Glycemia in Diabetes: D E. G, R R. L, R A. L, J I. M, D N, C M. P, D B. Sfebriyani dyahNo ratings yet
- Go 2006Document12 pagesGo 2006my accountNo ratings yet
- Factors Predicting Malnutrition in Hemodialysis Patients: A Cross-Sectional StudyDocument10 pagesFactors Predicting Malnutrition in Hemodialysis Patients: A Cross-Sectional StudyMarco TolentinoNo ratings yet
- Desantis 2006Document15 pagesDesantis 2006Hoàng ThôngNo ratings yet
- Winter Gerst 2006Document9 pagesWinter Gerst 2006Dr XNo ratings yet
- 2699 PDFDocument4 pages2699 PDFSeptya widhiafniNo ratings yet
- 0717 6163 RMC 149 02 0210Document7 pages0717 6163 RMC 149 02 0210Anthony PonceNo ratings yet
- International Journal Insulin DosingDocument12 pagesInternational Journal Insulin DosingMutia Ramadini91No ratings yet
- Icu 2011Document2 pagesIcu 2011Mica PascualNo ratings yet
- Nihms 79056Document14 pagesNihms 79056angsokasatuNo ratings yet
- Hamsini SreeramDocument33 pagesHamsini SreeramkalyanpavuralaNo ratings yet
- Fasting With Diabetes: A Prospective Observational StudyDocument6 pagesFasting With Diabetes: A Prospective Observational StudyRiyan AdriyanNo ratings yet
- Diabetes Mellitus: Is Type Surgical Disease?Document10 pagesDiabetes Mellitus: Is Type Surgical Disease?Mateo TamayoNo ratings yet
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionFrom EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionNo ratings yet
- Toshbro ArticleDocument4 pagesToshbro ArticleKedar DeshpandeNo ratings yet
- Introducing Yourself: Meet Joe and Ana, Look How They Introduce ThemselvesDocument3 pagesIntroducing Yourself: Meet Joe and Ana, Look How They Introduce Themselvesedwin aguileraNo ratings yet
- Water Treatment For Hemodialysis: Review ArticleDocument8 pagesWater Treatment For Hemodialysis: Review ArticleAmmar YasserNo ratings yet
- Electronics Basic Questions ObjectiveDocument82 pagesElectronics Basic Questions ObjectiveKrishan Gupta100% (3)
- Providing Steam InhalationDocument2 pagesProviding Steam InhalationJee MirasNo ratings yet
- Hero Motocorp Hero MotocorpDocument3 pagesHero Motocorp Hero Motocorpthakur_pradeep85No ratings yet
- Prelim Exam Schedule SY 21 22Document4 pagesPrelim Exam Schedule SY 21 22Joseph Patrick OcapanNo ratings yet
- DSE8003 MKII Data SheetDocument2 pagesDSE8003 MKII Data SheetYacine DaliNo ratings yet
- Low Glycemic Index GuideDocument24 pagesLow Glycemic Index GuideBinibining Kris100% (1)
- NLT R 83116567550Document2 pagesNLT R 83116567550Di bintMuhyiddinNo ratings yet
- Elasticity and Creep in Concrete PrintDocument57 pagesElasticity and Creep in Concrete PrintaezenkwuNo ratings yet
- 8x3 8x4 8x5 AND 8X6: Moist Chocolate CakeDocument3 pages8x3 8x4 8x5 AND 8X6: Moist Chocolate CakeJan Alleana Mayo FernandezNo ratings yet
- Astm D6648-08Document14 pagesAstm D6648-08ROBERTO MIRANDANo ratings yet
- U17 - MTH205 - Final ExamDocument11 pagesU17 - MTH205 - Final ExamMohammed AlawnahNo ratings yet
- DKA Canadian ProtocolDocument2 pagesDKA Canadian Protocolplay_wright2084No ratings yet
- Effects of PycnogenolDocument9 pagesEffects of PycnogenolZac IngNo ratings yet
- Disassembly Monito 201342494933Document5 pagesDisassembly Monito 201342494933K.O.D.No ratings yet
- Nutritional CounsellingDocument7 pagesNutritional CounsellingshilpasheetalNo ratings yet
- Perubahan Nomenclature Field Jambi1Document1 pagePerubahan Nomenclature Field Jambi1Budi SukendroNo ratings yet
- Plumbing Ventilation and TrapsDocument5 pagesPlumbing Ventilation and TrapscessNo ratings yet
- PAP Design BasisDocument17 pagesPAP Design BasisBiju JosephNo ratings yet
- Empowering Social WorkDocument257 pagesEmpowering Social WorkKhizra ChNo ratings yet
- Coperion18 DataDocument4 pagesCoperion18 DataSalem GarrabNo ratings yet
- Medical Questionnaire: To Be Filled by Attending PhysicianDocument3 pagesMedical Questionnaire: To Be Filled by Attending PhysiciansusomNo ratings yet
- Homoeopathic PosologyDocument56 pagesHomoeopathic Posologysubhro kanti dutta100% (1)
- 160 48-RP6Document32 pages160 48-RP6Alexander Ruiz PerezNo ratings yet
- EMT-SOP-004 - Design ValidationDocument6 pagesEMT-SOP-004 - Design ValidationJaveria NazNo ratings yet
- Operating and Maintenance Manual Stack Economizers CRE-CCE-C2XDocument50 pagesOperating and Maintenance Manual Stack Economizers CRE-CCE-C2Xomar.moradi3707No ratings yet
- Zurich Support Services: C M Y KDocument8 pagesZurich Support Services: C M Y KAnastasis StagkasNo ratings yet