0%(1)0% found this document useful (1 vote)
3K viewsGENERAL LINE of Treatment UREA AMMONIA SALT - poISONING
GENERAL LINE of Treatment UREA AMMONIA SALT - poISONING
Uploaded by
SunilThis document provides guidance on the general principles and lines of treatment for poisoning cases. It outlines that the main goals of treatment are to prevent further absorption of toxins, counteract their effects, enhance detoxification and elimination. The key methods discussed are:
1. Removal of toxins from the stomach through gastric lavage or induced vomiting if ingestion was recent.
2. Hastening passage through the bowels using cathartics or laxatives to flush toxins through.
3. Neutralizing or binding toxins still in the gastrointestinal tract using adsorbents like activated charcoal or specific antidotes when available.
Supportive measures like fluid therapy, respiratory
Copyright:
© All Rights Reserved
GENERAL LINE of Treatment UREA AMMONIA SALT - poISONING
GENERAL LINE of Treatment UREA AMMONIA SALT - poISONING
Uploaded by
Sunil0%(1)0% found this document useful (1 vote)
3K views49 pagesThis document provides guidance on the general principles and lines of treatment for poisoning cases. It outlines that the main goals of treatment are to prevent further absorption of toxins, counteract their effects, enhance detoxification and elimination. The key methods discussed are:
1. Removal of toxins from the stomach through gastric lavage or induced vomiting if ingestion was recent.
2. Hastening passage through the bowels using cathartics or laxatives to flush toxins through.
3. Neutralizing or binding toxins still in the gastrointestinal tract using adsorbents like activated charcoal or specific antidotes when available.
Supportive measures like fluid therapy, respiratory
Original Description:
GENERAL LINE Of treatment UREA AMMONIA SALT.poISONING
Original Title
GENERAL LINE Of treatment UREA AMMONIA SALT.poISONING
Copyright
© © All Rights Reserved
Share this document
Did you find this document useful?
Is this content inappropriate?
This document provides guidance on the general principles and lines of treatment for poisoning cases. It outlines that the main goals of treatment are to prevent further absorption of toxins, counteract their effects, enhance detoxification and elimination. The key methods discussed are:
1. Removal of toxins from the stomach through gastric lavage or induced vomiting if ingestion was recent.
2. Hastening passage through the bowels using cathartics or laxatives to flush toxins through.
3. Neutralizing or binding toxins still in the gastrointestinal tract using adsorbents like activated charcoal or specific antidotes when available.
Supportive measures like fluid therapy, respiratory
Copyright:
© All Rights Reserved
0%(1)0% found this document useful (1 vote)
3K views49 pagesGENERAL LINE of Treatment UREA AMMONIA SALT - poISONING
GENERAL LINE of Treatment UREA AMMONIA SALT - poISONING
Uploaded by
SunilThis document provides guidance on the general principles and lines of treatment for poisoning cases. It outlines that the main goals of treatment are to prevent further absorption of toxins, counteract their effects, enhance detoxification and elimination. The key methods discussed are:
1. Removal of toxins from the stomach through gastric lavage or induced vomiting if ingestion was recent.
2. Hastening passage through the bowels using cathartics or laxatives to flush toxins through.
3. Neutralizing or binding toxins still in the gastrointestinal tract using adsorbents like activated charcoal or specific antidotes when available.
Supportive measures like fluid therapy, respiratory
Copyright:
© All Rights Reserved
You are on page 1of 49
At a glance
Powered by AI
The key takeaways are that poisoning is always an emergency and needs to be managed immediately. Supportive care to maintain vital functions like respiration and circulation is important until specific treatment can be given. ABC (Airway, Breathing, Circulation) is important.
The general principles of treatment of poisoning include managing the emergency phases first to improve the animal's condition through supportive care. Prompt removal or neutralization of the poison while maintaining vital body functions is important until slow-acting specific treatment can be given.
Methods to remove poison from the stomach include gastric lavage and in ruminants, manual gastric emptying after emergency gastrotomy/ruminotomy. Gastric lavage should be done soon after ingestion and is indicated in small animals like dogs within 2-4 hours of ingestion.
TOXICOLOGY:
GENERAL LINE OF TREATMENT
OF POISONING
GENERAL PRINCIPLES OF TREATMENT OF POISONING
Poisoning is always an emergency and need to be managed
immediately with appropriate measures using specific antidotes
whenever available.
However, in majority of poisoning cases treatment with an
antidote is not possible due to lack of confirmative diagnosis. In
acute poisonings, first of all truly emergency phases should be
managed to improve condition of the animal by providing
appropriate supportive care to ensure its survival.
For this, focus on prompt removal or the neutralization of poison
whilst maintaining vital functions of the body by restoring
respiration by giving artificial respiration and or drugs acting on
cardiovascular system, CNS stimulants or depressants, emetics
etc. depending on the clinical state of the patient/animal until
slow acting and specific treatment is instituted.
ABC- Airway, Breathing and Circulation
In order to treat the poisoning cases effectively, a
clear understanding of some of the basic principles
of toxicokinetics, toxicodynamics and specific
therapeutic goals is essential
e.g. absorption of the toxic substances be minimised
antagonize the effects of absorbed toxicants
metabolic biotransformation of poison with reduced
toxicity be enhanced
while biotransformation into toxic substances be
inhibited/reduced
elimination from the body be enhanced.
These goals can be achieved generally by -general
Line of treatment of poisoning.
General Line of treatment of poisoning
Gastrointestinal tract is an important site
where from maximum absorption of toxicants
takes place.
Thus, prevention of gastrointestinal
absorption is an important aspect in initial
treatment of acute poisoning. It can be
achieved by:
Removal of the poison from the stomach;
Hastening the passage through bowel;
Neutralization of the poison within the
gastrointestinal tract.
REMOVAL OF THE POISON FROM THE STOMACH:
(i) Gastric lavage:
It should be done as soon as possible after ingestion and its efficacy
decreases with the passage of time.
It is a rapid way of removing the poisons alongwith stomach contacts.
However, its should not be attempted in unconscious or convulsing
animals or in cases of ingestion of caustic substances or petroleum
distillate hydrocarbons.
It is useful only in small animals and is extensively used in dogs if
ingestion has taken place in preceding 2-4 hours.
It is indicated on the anaesthetized animals with endotracheal
intubation
For the purpose, an isotonic sodium chloride solution (occasionally
sodium bicarbonate) occasionally @ 10 ml/ kg is indicated.
Repeat the procedure until the washout stomach fluid is clear.
However, in ruminants, manual gastric emptying after emergency
gastrotomy/ruminotomy is the only satisfactory method of removing
the rumen e.g. plant poisoning or for indigestible materials such as
plastic, polyurethane foam
ii) Emetics:
In dogs, cats and swines, vomition may be induced to empty the stomach.
Emetics may be used if ingestion has taken place within the preceding 2-3
hours.
But vomition should not be induced if there are seizures (unless
controlled) or the animal is in comatose state or there is severe respiratory
distress or has ingested caustic substances (strong acid, alkali or cationic
detergent) or petroleum distillate (gasoline, kerosene, paint thinner etc.)
Emesis may be induced chemically by making used of hypertonic solutions
of copper sulfate or sodium chloride, but not reliable
Drugs like ipecac or apomorphine hydrochloride are used to induce
vomition.
However, there is a greater risk of aspiration pneumonitis due to
aspiration of gastric contents into the trachea and lungs.
a) Apomorphine hydrochloride is administered to dogs at the dose rate of
0.04- 0.07 mg/kg by I/V, I/M or S/C or subconjunctival routes.
contraindicated in the presence of existing central depression. Do not
give emetics to large animals. Apomorphine is contraindicated in cats and
pigs.
b) Xylazine is used in dogs and cats. Emesis is produced within
10-20 min. Emesis in cats is more consistent compared to
dogs. Dose for cats is I mg/kg by IM route. However, slightly
higher dose is recommended for dogs.
(c) Syrup of ipecac (10%) is administered orally; 10-20 ml (1-2
ml/kg) for dogs and 2-5 ml (3.3 ml /kg) for cats. Emesis is
produced within 20-30 minutes.
If none of these drugs are available, common salt (sodium
chloride) 1-3 teaspoons in warm water or hydrogen peroxide
(3% solution) 1 ml/kg may be administered orally. However,
copper sulfate should not be used as it is an irritant and may
hasten the absorption of poisons from the stomach.
HASTENING THE PASSAGE THROUGH BOWEL
i) Cathartics
may be of some value particularly if some slow acting poison is
involved.
Oily ones- no longer recommended in the management of orally
ingested poisons as these may produce dehydration, hypernatremia,
hypermagnesemia, hyperkalemia and hyperphosphatemia.
Irritant purgatives or oil-based purgatives should never be used as
these promote absorption of poison.
However saline purgatives such as sodium sulphate, magnesium
sulphate or magnesium citrate may be used either orally or as
enema.
Dose of sodium sulphate for dogs and cats is 1.0 g/kg (2-25 g) while
100-200 gm for large animals. Orally liquid paraffin is also
recommended for inducing evacuation of the bowel.
Doses for dogs are 5-15 ml, adult cattle and horses 0.5-2.0 litres,
ii) Urinary excretion of poisons may be hastened by increasing
the flow of urine (diuresis).
a). Increase glomerular filtration: Use of potent diuretics is
contraindicated. Administer 10% glucose or 10% mannitol or
sterile saline solution by slow IV infusion.
Large animals: 1-2 ml/kg/24 h;Small animals: 1-2 ml/kg/24 h
b). Reduce tubular reabsorption:
Changing pH of the urine by
Urinary Acidifiers (ammonium chloride, ascorbic acid, sodium
acid phosphate) or Alkalizers (sodium bicarbonate, sodium
acetate, sodium citrate) in an attempt to ionize the offending
toxic substance will promote diuresis and urinary excretion of
poisons-weak bases and weak acids, respectively
(c) Dialysis: Haemo-or peritoneal dialysis
NEUTRALIZATION OF THE POISON WITHIN THE GASTROINTESTINAL TRACT
1) Specific antidotal treatment of poisoning is highly desirable and most
effective.
An antidote may be defined as a specific remedy used for countering the
action of a particular poison
Very few antidotes are available for a limited number of toxicants. Thus,
these are being employed rather rare under such circumstances.
Depending on the mechanism of action, the antidotes may be classified as
Competitive antagonism: e.g. nalorphine for morphine poisoning.
Non-competitive antagonism: e.g. atropine for carbamate poisoning.
Chemical neutralization: e.g. sodium nitrite and sodium thiosulfate for
cyanide poisoning.
Metabolic inhibition: e.g. ethanol for methanol poisoning.
Oxidative reduction: e.g. methylene blue for nitrite poisoning.
Chelation: e.g. dimercaprol (BAL) for arsenic, CaEDTA for lead,
deferoxamine for iron poisoning etc
2) Use of adsorbing agents like activated charcoal
or neutralizing agents like acids, alkalies, chelating agents e.g.
dimercaprol (British antilewisite, BAL), calcium EDTA or tannic acid,
magnesium oxide, aluminium hydroxide gel etc. is recommended
for various poisons,.
Activated vegetable charcoal
is inert, non-absorbale, odourless and tasteless and binds or
adsorbs organic material to form stable complex (es) which is not
absorbed, currently, it is the single most effective and useful agent
employed for prevention of absorption of ingested poisons.
dose rate of 250-500 g in large animals and 5-50 gm in small
animals, preferably as a suspension in water several minutes to 24
hrs after ingestion and before emetics, if possible.
An important ingredient of the universal antidote in combination
with kaolin, tannic acid and magnesium oxide. The universal
antidote contains vegetable charcoal 10 g, magnesium oxide 5g,
kaolin 5 g, tannic acid 5 g and water added upto 200 ml.
TOXICITY OF
Non Metals:
Ammonia/urea, acids, alkalies, sulphur, phosphorous, salt, Fluorosis,
Nitrate/nitrite etc
Metals: As, Bi, Hg, Pb,Cu,Se etc
Plants:
Cyanogenetic Glycosides, Alkaloid, NO3 rich etc Ricinus communis (Castor);
Lantana camera (Lantana), photosensitization
Drugs:
NSAIDS, Antibiotics- aminoglycosides, tetracyclines, fluoroquinolone, feed
additives , vitamins etc
Insecticides, herbicides, weedicide, agrochemicals etc
Mycotoxins, bacterial toxins
Venoms/Bites/Stings Zootoxins : snake, scorpion, wasp, spider etc
Radiation hazards, environmental pollutants
UREA AND AMMONIA TOXICITY
Urea is used as a fertilizer on crop and pasture fields
a cheap source of non-proteinous nitrogen (NPN) in ruminants
ration
better tolerated when mixed with sufficient amounts of other
feeds. About 1-2 per cent of total ration (dry weight basis)-SAFER,
but larger amounts are likely to produce poisoning.
Ruminal microflora possesses urease activity which hydrolyse urea
into ammonia and water.
Ammonia is assimilated for amino acids and microbial protein
synthesis.
Therefore, dietary requirement of proteins is decreased IF NPN
source is added to the ration of ruminants.
For proper utilization of ammonia (NH3)' within certain limits,
readily and sufficiently available soluble carbohydrates in the form
of starch and glucose are essential.
However, production of ammonia beyond handling capacity of
liver results in urea poisoning.
Ruminants/ Animals should be accustomed to urea feeding by
gradually increasing its level in the ration/feed
Tolerance and adaptation to urea feeding is lost rapidly. If the
animals receive no urea for three days, they become
susceptible to urea poisoning.
Higher Susceptibility Factors : starvation and low protein
diet., insufficient availability of soluble carbohydrate sources
in the feed/diet, adaptation of the animals, abrupt change in
the diet, lack of water, ruminal pH (alkaline pH- predispose for
toxicity)
Food/ rations based on concentrates reduce severity of
intoxication
Simultaneous feeding of soyabean meal potentiates urea
toxicity due to liberation of excess of ammonia as soyabean
meal contains urease enzyme..
Ruminants are most sensitive speciessusceptible to ammonia
poisoning
Higher capacity of ruminants than non-ruminants to handle
absorbed ammonia as the former have a greater hepatic urea
synthesizing ability or a high glutamine synthetase activity in
the spleen, liver and brain.
Equines appear to be tolerant to relatively large.doses of urea
where its hydrolysis takes place in the caecum.
Pigs are quite resistant to even very large doses of urea.
Oral LDso value of urea in cattle and sheep is 1.0-1.5 glkg and
horse is 4.0 glkg while toxic dose in cattle and sheep is 0.3 -
0.5 glkg
Sources of Urea poisoning
Accidental ingestion of solid or liquid form of
urea due to improper storage or spilage
Feeding of large quantities of NPN urea-
mollases feeds to unaccustomed animals
Improperly mixed feed- excess urea in ration
etc.
Mechanism of toxicity:
Hydrolysis of urea occurs in the rumen.
The rate of ammonia production depends primarily on the amount
of ration ingested, the amount of urease present in the ruminal
contents or the diet and pH of the ruminal contents.
Toxicity of urea is due to ammonia absorbed from the stomach
/rumen which depends on ruminal pH.
Urea + water > CO
2
+ NH
3
At rumen pH of < 6.2, majority of the released ammonia is in the
form of ammonium ions (NH4) which are highly water soluble and
absorbed poorly i.e. low pH favours production of NH4
If absorption of ammonia into blood is up to certain limits, body
detoxifies ammonia as absorbed ammonia is normally incorporated
into the urea cycle and excreted as urea in urine
Conversion of ammonia (NH3) to urea occurs in the liver.
Ruminants have a higher capacity to handle absorbed NH3 than
the non-ruminants- greater hepatic urea - synthesizing ability
When concentration of NH3 in rumen exceeds 80 mgldl, NH3
appears in the peripheral blood and high NH3 concentrations are
built up in blood stream and thus NH3 accumulates in tissue cells.
When blood NH3 nitrogen reaches 0.80 - 1.30 mg/dl, clinical signs
of poisoning become apparent.
Ammonia inhibits the citric acid cycle, exact mechanism -not
known.
Saturation of glutamine-synthesizing system causes a backing up
in the citric acid cycle and decrease in its. Intermediates.
As a result there is decrease in energy production and cellular
respiration and thus cells begin to malfunction.
CNS is the first to 'be affected as it has a large requirement for
energy
Impairment of TCA cycle results in cellular energy and respiration
deficits and ultrastructural degenerative changes.
An increase in anaerobic glycolysis, blood glucose and blood lactate.
Liver dysfunction increases susceptibility to poisoning
Clinical signs:
Onset- fast or delayed- on the production of ammonia in the
rumen and its absorption into the blood stream
But signs are most acute in nature and death generally occurs
within half to four hours of ingestion.
Characteristic signs :
weakness, initial restlessness, salivation, prominent frothing
at the mouth and nose, grinding of teeth, abdominal
pain(Colic), bradycardia, marked jugular pulse dyspnoea,
bloat, forced rapid breathing, pulse and respiration
progressIvely become weak and slow.
Later severe groaning, shivering, twitching of eye lids, lips,
taiL, ataxia, terminal toniC convulsions and death, generally
when the blood ammonia concentration are> 5 mgldl.
Animals appear rigid rather than depressed between the
convulsions.
Post -mortem lesions:
No characteristic post-mortem lesions are present in urea
poisoning
Strong odour of ammonia in the rumen.
Generalized haemorrhages, congestion and vascular injuries.
Hydrothorax and hydropericardium.
Haemorrhagic enteritis with oedema and ulceration of
intestinal mucous membrane.
Liver is enlarged, pale and friable., Fatty degenerations of
liver and kidneys
Haemorrhagic degenerative changes in brain.
Pulmonary oedema and acute catarrhal bronchitis,
peribronchial and intraalveolar haemorrhages.
Diagnosis:
History of access to urea.
Clinical signs.
Post mortem lesions.
Laboratory investigations indicating high ruminal
fluid and blood ammonia concentrations,
rumina I pH of more than 7.5 and increase in blood
urea nitrogen.
Feed analysis for urea, ammonium salts etc.
Stomach / ruminal contents for urea or ammonical
fertilization.
Differential diagnosis:
(i) Arsenic poisoning.
(ii) Strong caustics poisoning.
(iii) Lead poisoning.
(iv) Organochlorine pesticides.
(v) Organophosphates toxicity.
(vi) Nitrate and cyanide poisoning.
(vii) Encephaletic disease, enterotoxaemia, brain
engorgement.
TREATMENT:
No specific antidote for urea poisoning and generally the
treatment is ineffective.
Aimed at reducing the concentration of ammonia in the blood
either by reducing the production of ammonia and hastening
the conversion of ammonia to urea.
Weak acids, generally vinegar or 5% acetic acid in sufficient
quantity of cold water is administered.
for sheep is 0.5-1.0 litre and cattle are 4.0 liters.
It not only dilutes the ruminal contents but also reduces the
production of ammonia by lowering pH of the rumen and
slowing the rate of hydrolysis of urea by reducing urease
activity and also promotes diuresis.
Excessive gas accumulated in the rumen is removed by trocar
and canula.
stomach tube or ruminotomy.
CORROSIVES TOXICITY/ POISONING
ACIDS AND ALKALIES
Definition of Corrosive
A corrosive poison is one that causes tissue injury by a
chemical reaction
Most commonly:
Strong acids & alkalis
Concentrated weak acids & alkalis
Oxidizers (with neutral pH)
Alkylating agents
Dehydrating agents
Halogens & organic halides
Other organic chemicals (phenol)
Common Agents
Acids:
automobile batteries, gun barrel cleaning fluid and swimming pool cleaning
agents.
Car battery fluid : H
2
SO
4
toilet bowl cleanersDe-scalers: HCl
Metal cleaners: HNO
3
Rust removers: HF
Disinfectants: Phenol
Alkali: More Dangerous than acids
Alkaline (NaOH, KOH,Na2CO3,
NH4OH,KMnO4) products
drain cleaners, washing products, liquid
cleansers and toilet bowl products
Household cleaners: Ammonia-
based
Disinfectants; Bleach (hypochlorite)
Drain cleaners; NaOH
Factors Determining Corrosiveness
Solid particulate: deep local burns
Liquids; diffuse/ circumferential
Food may buffer
Pyloric spasm from acid
J transit time
Titrable acid/alkali reserve (TAR)
(amount needed to normalize pH
of corrosive)
Mechanism of Injury
Aci
d
Coagulation
(desiccate / denature protein)
Eschar formed
Delayed eschar loss (> 3 days):
perforation / bleeding
Fibrosis & cicatrization is subsequently seen
Alkali
Liquefaction
(saponify fat / solubilize protein)
Collagen swelling
Small vessel thrombosis
Heat
CORROSIVES
On dermal and ocular exposure:
serious burns, extremely painful, corneal/conjuctival
necrosis, perforation and opacity which may not be evident
immediately.
On ingestion
corrosive burns of mucosal membranes appear firstly as
milky white or grey,
which later turns to wrinkled black.
Animal may vocalize or depressed; manifest pain by panting
inability to swallow. Haematemesis
abdominal pain, polydypsia, respiratory distress, shock, secondary
pneumonia from aspiration of vapours
gastrointestinal bleeding, perforation and fistula are the other
signs observed depending on the severity.
Clinical Approach
Identify immediate life threats
Mortality ~10-15% reported in hospitalized patients
Mainly due to:
Airway injury:
Mucosal edema obstruction
Inhalation ALI / ARDS
Gastro-esophageal injury:
Perforation sepsis
Haemorrhage
Treatment
Oral dilution with egg white , milk or water
Skin and eyes thourghly flushed with copious water and
sterile saline respectively
Therapy for shock: IV fluids, steroids within 48 hours,
which reduce the fibroblastic activity and inflammation,
reduce the stricture from circumferential alkaline burns.
Analgesics and antibiotics prophylactically in animals
with perforations.
Contraindications: 1. Attempts to neutralize burns
chemically, as exothermic reactions produce elevated
local heat and thermal burns.. 2. Gastric lavage and
induction of emesis 3. Charcoal is ineffective in binding to
caustics
Decontamination- X?
Almost any attempt to gastric emptying / dilution
is CONTRAINDICATED in corrosive poisoning
NO emetics (ipecac): injury & perforation risk
NO Nasogastric (NG) tube: Esophageal perf. ; aspiration
NO Activated charcoal; No adsorption / interferes
NG tube aspiration may be considered early
(<90 minutes) in large volume ingestions
Dilution & Neutralization?
Dilution of ingestants by NasoGastric Tube
lavage generates heat & increases risk of
aspiration
No proven benefit
Attempts at neutralization have similar
effects
Small volume dilution with water may be
rarely considered early (<30 minutes) with
particulate agents
DISINFECTANTS
QACs, phenol, pine oil, bleaches, alcohols; are more toxic than
soaps and detergent compounds
Phenols
Highly reactive and corrosive contact poisons; denatures
and precipitates cellular proteins of all contacting cells.
Nephrotoxic, hepatotoxic and neurotoxic; rapidly absorbed
through ingestion, inhalation or skin.
Cats are highly sensitive to phenolic compounds. S
Sources of phenolic compounds include flooring materials,
coal tar, creosote, tar paper.
Dermal exposure : in intense pain, areas of coagulative necrosis;
treated by glycerol, polyethylene glycol washing, thorough
rinsing with water , dressings soaked in 0.5% soda bica.
Ocular exposure : corrosive burns of mouth, oropharynx,
oesophagus. vomition, salivation, hyperactivity, ataxia, panting,
weakness, tremor, coma, seizures, methhaemoglobinaemia,
respiratory alkalosis, severe liver and kidney damage.
Treatment :
Demulcents-milk, egg white, gastric lavage
Emesis(contraindicated if severe damage)
Activated charcoal, saline cathartic,
1% methylene blue, 4mg/kg;IV; ascorbic acid
20mg/kg,PO; N-acetyl cysteine 140mg/kgIV,
70mg/kg PO. q,id for 3 days.
Ocular exposure is treated by sterile saline
wash.
Bleaches
sodium hypochlorite. Calcium hypochlorite and
trichloroisocyanuric acid in industrial strength bleaching
solutions ,swimming pool chlorine products and
chlorine laundry bleaches.
Non chlorine bleach preparations or colorfast bleaches
contain sodium peroxide, sodium perborate or
enzymatic detergents.
Toxicity is of lower degree
Irritation of oropharynx, salivation, vomition and
abdominal pain. Bleaching of hairs, pulmonary
irritation- coughing , dyspnoea and retching on
inhalation
Nonchlorine bleach products, (sodium perborate,
sodium peroxide) are alkaline and severe gastric
irritatants causing renal damage and CNS excitation.
Treatment
Milk and water orally
Washing with soap and rinsing with abundant
water/sterile saline on dermal/ocular exposure.
Induction of emesis and orogastric lavage is
contraindicated to avoid the risk of causing
further oesophageal irritation.
Milk of magnesia (2-3ml/kg) can be administered
symptomatically
Boric acid
ingredient in ant and roach killers
Vomition(blue-green vomitus), renal damage, CNS
excitation and depression.
Gastric decontamination with emesis induction
Gastroprotectants ( activated charcoal is
ineffective)
Cathartics, IVfluid therapy and antiemetics
COMMON SALT (SODIUM CHLORIDE) TOXICITY
An essential nutrient and added to the feed and ration of
animals but it is the quantity consumed which makes it
toxic.
Excessive ingestion of sodium chloride causes toxicity
and the condition is also termed as water deprivation
syndrome.
All species of animals including human beings and
poultry are poisoned but poultry and pigs are most
susceptible to salt poisoning.
In poultry- young chicks are most susceptible due to
indiscriminate feeding behaviour, poor sense of taste,
low plasma proteins in chicks and decreased glomerular
filtration area in the kidneys of chicks compared to
mammals.
Sources of poisoning:
Feeds containing high quantities of common Salt
Accidental over ingestion of common salt or excessive licking of salt
licks kept on the premises particularly when the animals have been
on restricted salt supply
After a period of salt deprivation for quite some time then the
animals may develop cravmg for salt or salt hunger
Excessive consumption of salty meat or meat flavoured brines by
carnivores, swill feeding to pigs (residues from bakeries, brine from
butcher's shop, salt whey from cheese factories ) or salted fish
waste, oil fields as salt water is an effluent from oil production.
Change from low salt ration to high salt ration, low vitamin E and
sulphur containing aminoacids.
Overdosing of animals with sodium sulphate or some other sodium
salts also results in salt poisoning.
However, - over-consumption of salt can be tolerated by the
animals if sufficient quantity of water is made available to the
animals immediately after ingestion 0fsalt.
Mechanism of toxicity:
Sodium ions and water balance are mainly disturbed.
Excess of sodium ions in gastrointestinal tract cause mild irritation and
secretion of water into the lumen of intestine and thus diarrhoea further
resulting into dehydration.
Absorption of Na
+
results in hypertonicity of blood and hypernatremia,
shrinkage of kidney tubules, deposition of sodium crystals in the tubules,
anuria and uremia etc. following transient polyuria due to initial excretion
of Na+ in the urine.
Decreased ability of sodium pumps to remove Na+ from the cells set up
an osmotic gradient.
Excess of Na+ in blood stream (extracellular hyperosmolarity) results in
shrinkage of capillary vascular endothelial cells in the brain and
meninges which in turn stimulate the capillary permeability and escape
of water from blood to interstitial spaces (intracellular dehydration) and
development of brain or cerebral oedema.
Cerebral oedema in pigs is also associated with the accumulation of
eosinophils in the brain tissue. As a result of cerebral oedema, there is
increased cerebrospinal fluid pressure and reduced blood flow to the
brain and thus hypoxia.
Clinical signs:
General signs- anorexia, excessive thirst, salivation, initially
diarrhoea followed by constipation, polyuria followed by anuria,
(Vomiting in dogs, )
Nasal discharge and weak pulse.
Body temperature is normal but ear and skin are cold.
Rigidity of muscles, hyper-irritability, blindness, stumbling,
walking backwards or in circles, pedalling of limbs, recurrent
convulsive seizures, recumbency, coma and death -hrs to days.
profuse watery diarrhoea with colic in ruminants, diarrhoea
with colic, mucus in faeces,
knuckling of fetlocks, dehydration and prostration in lactating
animals
Pruritis, ataxia, dog sitting posture, blindness, convulsions,
comatose and paddling in pigs
Intense thirst, respiratory distress, fluid discharge from beak,
weakness, wet faeces and limb paralysis in poultry .
Post mortem lesions:
Congestion and inflammation of gastrointestinal tract.
Faeces are fluidy and dark or dry.
Hydropericardium
Severe acute inflammation of gastric and intestinal lining
Oedema of tissues and body cavities.
Renal congestion.
Oedema of the cerebral cortex (polioencephalomalacia in cattle,
eosinophilic Meningoencephalitis in pigs).
Microscopically : large number of eosinophils in the distended
perivascular space and meninges are almost pathognomonic hl pigs but
not in poultry.
Other changes are degeneration of neurons and slight general gliosis,
vacuolization, disruption of the area between cortex and white matter.
Polultry:
Congestion of liver in chicks, hyperaemia of the organs and deposits of
uric acid in kidneys. ureters and droppings in mature birds.
Diagnosis:
History of salt ingestion.
Clinical signs of poisoning including excessive thirst.
Post-mortem lesions.
Species involved.
Circumstantial evidences of relatively restricted water or salt
supply.
Laboratory investigations indicating plasma sodium levels of
exceeding 150 mEq/L in live animals and CSF sodium level
of> 145 mEq/L and brain sodium > 1800 ppm in dead
animals.
Differential diagnosis:
Chlorinated hydrocarbons(OCC) toxicity: ( no thirst
and hyperthermia.)
organophosphate compounds (OPC)- hypothermia.
Drugs or plants causing central symptoms of
stimulation.
Lead or other metals toxicity where gastric
symptoms are more severe.
Injury to CNS., Pseudorabies, Encephalitis
Treatment:
No specific antidote is available.
Remove the toxic feed/ or water.
Salt free fresh water be made available, however, initially
access of the animal to Water should be restricted as
large intake of water will kill the animal by aggravating
cerebral oedema.
Small quantities of water frequently
Isotonic or hypotonic salt solution intraperitoneally daily for 2-
3 days.
Gastrointestinal tract sedatives.
Sedatives to counter the CNS stimulation.
FLUORINE TOXICITY
You might also like
- Australian Medicines Handbook Pty LTDDocument23 pagesAustralian Medicines Handbook Pty LTDCleonSciaxeNo ratings yet
- Classification and Dosage of Antimicrobial Agents in Veterinary MedicineDocument24 pagesClassification and Dosage of Antimicrobial Agents in Veterinary MedicineSunil0% (1)
- Nitric Oxide Pharmacology .Document130 pagesNitric Oxide Pharmacology .SunilNo ratings yet
- Restraining of ReptilesDocument85 pagesRestraining of ReptilesSunil100% (1)
- UOP Oleflex Process For Propylene Production: PetrochemicalDocument2 pagesUOP Oleflex Process For Propylene Production: PetrochemicalWong Yee Sun50% (2)
- Drugs Acting On Gastrointestinal SystemDocument41 pagesDrugs Acting On Gastrointestinal SystemDivya JoyNo ratings yet
- Drugs Affecting Calcium BalanceDocument63 pagesDrugs Affecting Calcium BalanceRd Chandane100% (1)
- Chemical Nature of Natural Drugs: Unit 8Document48 pagesChemical Nature of Natural Drugs: Unit 8Preeti VermaNo ratings yet
- Chemotherapy For Protozoal InfectionsDocument32 pagesChemotherapy For Protozoal InfectionsJia YingNo ratings yet
- Tandard Perating Rocedure: RotarodDocument2 pagesTandard Perating Rocedure: RotarodRohan PalNo ratings yet
- Hematinics: Dr. Monalisa Mondal Demonstrator Department of PharmacologyDocument28 pagesHematinics: Dr. Monalisa Mondal Demonstrator Department of PharmacologyShirsh JauriharNo ratings yet
- Practical 1-Far 161-FinishDocument10 pagesPractical 1-Far 161-FinishZulkifli Khairuddin100% (1)
- Antiadrenergic DrugsDocument19 pagesAntiadrenergic DrugsshivanshpandeNo ratings yet
- Bioassay of Histamine by Using Isolated Chicken Ileum: Correspondence For Author Rakesh B. DaudeDocument5 pagesBioassay of Histamine by Using Isolated Chicken Ileum: Correspondence For Author Rakesh B. DaudeCelsia NestiNo ratings yet
- Drugs Acting On Digestive System of AnimalsDocument11 pagesDrugs Acting On Digestive System of AnimalsSunil100% (4)
- Glucose (Mono Reagent) (GOD/POD Method) : For in Vitro Diagnostic Use OnlyDocument2 pagesGlucose (Mono Reagent) (GOD/POD Method) : For in Vitro Diagnostic Use OnlySourav MondalNo ratings yet
- GIT DrugsDocument57 pagesGIT Drugssalva sambaaNo ratings yet
- Pharmacology of The GITDocument31 pagesPharmacology of The GITmarviecute22No ratings yet
- Pharmacology Renal DiureticsDocument24 pagesPharmacology Renal Diureticskpsuan100% (1)
- Introduction of PharmacotherapyDocument51 pagesIntroduction of PharmacotherapyJeffrey RamosNo ratings yet
- general systemic states د.عزيزةDocument75 pagesgeneral systemic states د.عزيزةAhmed Hamdy NaDa100% (2)
- Screening Methods - Analgesic DrugsDocument28 pagesScreening Methods - Analgesic DrugsKeerthi Sagar100% (1)
- Unit 8 Drugs Acting On The Endocrine SystemDocument26 pagesUnit 8 Drugs Acting On The Endocrine SystemTherese Margarette SantiagoNo ratings yet
- Mouse Handling Techniques PacketDocument24 pagesMouse Handling Techniques PacketLovely Ann AyapanaNo ratings yet
- Drug Induced Hepatitis: Dr.M.Sharmila Assistant Professor M7 (Prof CR Unit) Institute of Internal MedicineDocument21 pagesDrug Induced Hepatitis: Dr.M.Sharmila Assistant Professor M7 (Prof CR Unit) Institute of Internal MedicineAtakan Yeşil100% (1)
- Veterinary Pharmacology Toxicology PDFDocument11 pagesVeterinary Pharmacology Toxicology PDFSandeep Kumar Chaudhary55% (11)
- Screening ShortDocument30 pagesScreening Shortjignesh100% (1)
- Top Drugs: 1. ACETAMINOPHEN (Tylenol)Document12 pagesTop Drugs: 1. ACETAMINOPHEN (Tylenol)epingNo ratings yet
- Cytotoxic Drugs: Pharm. Dr. Ezekiel EfeobhokhanDocument24 pagesCytotoxic Drugs: Pharm. Dr. Ezekiel EfeobhokhanjonaNo ratings yet
- 01 Introduction To Clinical Toxicology (1) - 5Document295 pages01 Introduction To Clinical Toxicology (1) - 5Lyadelou FortuNo ratings yet
- MetronidazoleDocument16 pagesMetronidazoleAnshul Arora100% (2)
- Experimental Pharmacology (PDFDrive)Document168 pagesExperimental Pharmacology (PDFDrive)Priya MohiteNo ratings yet
- Ward RoundDocument2 pagesWard RoundAnonymous whcvnPBeQNo ratings yet
- Animal Used For Experimental PharmacologyDocument3 pagesAnimal Used For Experimental PharmacologyAishwarya PatilNo ratings yet
- Hand Eczema - PPT 59 CKDocument23 pagesHand Eczema - PPT 59 CKGrm MotorsNo ratings yet
- Review Notes For Diabetes MellitusDocument8 pagesReview Notes For Diabetes MellitusEditha LucasNo ratings yet
- Principles of PharmacologyDocument9 pagesPrinciples of Pharmacologybencleese100% (1)
- Anti-Viral Drugs AltDocument42 pagesAnti-Viral Drugs AltSidraNo ratings yet
- CPCSEA GuidelinesDocument27 pagesCPCSEA GuidelinesArchana VanjariNo ratings yet
- ChronopharmacologyDocument5 pagesChronopharmacologyDRx Ijajul HussainNo ratings yet
- Anti LeproticDocument9 pagesAnti LeproticMeenakshi shARMANo ratings yet
- SulfonamidesDocument14 pagesSulfonamidescamzyyy30No ratings yet
- Pharmacology of Thyroid Hormones and Anti Thyroid Drugs For Second Year Medicine StudentsDocument48 pagesPharmacology of Thyroid Hormones and Anti Thyroid Drugs For Second Year Medicine StudentsAmanuel MaruNo ratings yet
- I. Practicals: Practical Exam Pattern For Ii Mbbs Pharmacology Cbme Batch (2019)Document2 pagesI. Practicals: Practical Exam Pattern For Ii Mbbs Pharmacology Cbme Batch (2019)santhoshNo ratings yet
- Screening MethodsDocument1 pageScreening MethodsManoj chalageriNo ratings yet
- Pharmaco DynamicsDocument7 pagesPharmaco DynamicsDavid NicholasNo ratings yet
- Orientation To Pharmacy-2011Document51 pagesOrientation To Pharmacy-2011khairi_mustafa1704No ratings yet
- ZOOTOXINSDocument72 pagesZOOTOXINSSunil86% (7)
- Organophosphate PoisoningDocument40 pagesOrganophosphate PoisoningMadhu Sudhan PandeyaNo ratings yet
- Antihelminths: DR Japhet Mangoyi Department of Clinical PharmacologyDocument15 pagesAntihelminths: DR Japhet Mangoyi Department of Clinical PharmacologyMitchelle SaurambaNo ratings yet
- Pharmacotherapy of Myocardial InfaractionDocument69 pagesPharmacotherapy of Myocardial InfaractionNikhil KamdiNo ratings yet
- Polioencephalomalacia in GoatsDocument20 pagesPolioencephalomalacia in GoatsUmesh GopalanNo ratings yet
- Pharmacology Practical Manual - Student Copy2Document11 pagesPharmacology Practical Manual - Student Copy2NareshNo ratings yet
- Biomed LDH 51Document2 pagesBiomed LDH 51D Mero LabNo ratings yet
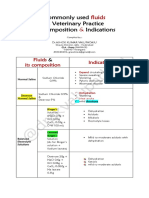
- Common IV Fluids at Composition & IndicationsDocument2 pagesCommon IV Fluids at Composition & IndicationsNilesh SuryawanshiNo ratings yet
- Pharmacology Lecture - 15 Inotropic DrugsDocument3 pagesPharmacology Lecture - 15 Inotropic DrugsChris Queiklin100% (1)
- Pharmacology of The GIT System: CIC Ragasa, RN-MDDocument70 pagesPharmacology of The GIT System: CIC Ragasa, RN-MDCarmencita Ileen Ragasa - AhmedNo ratings yet
- HOMEOPATHY TREATMENT OF VARIOUS DISEASES OF POULTRY (BROILERS & LAYERS) - Pashudhan PrahareeDocument1 pageHOMEOPATHY TREATMENT OF VARIOUS DISEASES OF POULTRY (BROILERS & LAYERS) - Pashudhan PrahareeAashish SatyamNo ratings yet
- Health Promotion and Education in School - VL PDFDocument28 pagesHealth Promotion and Education in School - VL PDFAshu AmmuNo ratings yet
- Anti Hypertensive DrugsDocument3 pagesAnti Hypertensive DrugsMu'allim HawaryNo ratings yet
- 71134lecture 6Document27 pages71134lecture 6azizNo ratings yet
- Fluorosis Phosphorous Nitrate Toxicity in AnimalsDocument55 pagesFluorosis Phosphorous Nitrate Toxicity in AnimalsSunilNo ratings yet
- Mycotoxins in Animal HealthDocument103 pagesMycotoxins in Animal HealthSunil100% (3)
- VPT MCQ ForDocument10 pagesVPT MCQ ForSunilNo ratings yet
- Carbon Monoxide PoisoningDocument22 pagesCarbon Monoxide PoisoningSunilNo ratings yet
- Antiseptics and Disinfectants For Veterinary ClinicsDocument3 pagesAntiseptics and Disinfectants For Veterinary ClinicsSunil100% (5)
- Drugs in ReptilesDocument71 pagesDrugs in ReptilesSunil100% (1)
- Endocrine Vety PharmaDocument16 pagesEndocrine Vety PharmaSunilNo ratings yet
- VCI MSVE 2008 RegulationsDocument136 pagesVCI MSVE 2008 RegulationsSunil50% (2)
- Classification of AmphibiansDocument22 pagesClassification of AmphibiansSunilNo ratings yet
- Toxicological Investigation and Its Significance in Animal Health DiagnosisDocument8 pagesToxicological Investigation and Its Significance in Animal Health DiagnosisSunil100% (1)
- Drugs Acting On Respiratory System of AnimalsDocument8 pagesDrugs Acting On Respiratory System of AnimalsSunil100% (4)
- Site of Action of Drugs Acting On Adrenergic Neurohumoral Transmission PDFDocument1 pageSite of Action of Drugs Acting On Adrenergic Neurohumoral Transmission PDFSunilNo ratings yet
- Drugs Acting On Digestive System of AnimalsDocument11 pagesDrugs Acting On Digestive System of AnimalsSunil100% (4)
- Drugs Acting On Genitourinary System of AnimalsDocument44 pagesDrugs Acting On Genitourinary System of AnimalsSunilNo ratings yet
- Drugs Acting On Haematopoietic System of AnimalsDocument28 pagesDrugs Acting On Haematopoietic System of AnimalsSunil100% (1)
- Mycotoxins in Animal HealthDocument103 pagesMycotoxins in Animal HealthSunil100% (3)
- Toxicokinetics DynamicsDocument76 pagesToxicokinetics DynamicsSunil100% (1)
- Mercury Lead Arsenic Cadmium ToxicityDocument171 pagesMercury Lead Arsenic Cadmium ToxicitySunilNo ratings yet
- ZOOTOXINSDocument72 pagesZOOTOXINSSunil86% (7)
- Systemic Veterinary Pharmacology in A NutshellDocument165 pagesSystemic Veterinary Pharmacology in A NutshellSunil100% (1)
- Trematodes of Wild BirdsDocument5 pagesTrematodes of Wild BirdsSunilNo ratings yet
- LATHYRISM AND PHOTOSENSiTIZATIONDocument33 pagesLATHYRISM AND PHOTOSENSiTIZATIONSunilNo ratings yet
- Classification of AmphibiansDocument22 pagesClassification of AmphibiansSunil100% (1)
- AntiConvulsants Drugs in Brief PDFDocument28 pagesAntiConvulsants Drugs in Brief PDFSunilNo ratings yet
- Extinct and Endangered Animals OF INDIADocument8 pagesExtinct and Endangered Animals OF INDIASunil100% (2)
- Cestodes of Wild Birds PDFDocument5 pagesCestodes of Wild Birds PDFSunil100% (1)
- Pharmaco EconomicsDocument49 pagesPharmaco EconomicsSunil100% (1)
- 3CR12 Data Sheet 2021Document1 page3CR12 Data Sheet 2021Elcio VilanculoNo ratings yet
- Group 3 GunpowderDocument13 pagesGroup 3 GunpowderBrielle Shai CruzNo ratings yet
- Product Brochure Riken Keiki SP-220Document4 pagesProduct Brochure Riken Keiki SP-220Anticristh6666No ratings yet
- Chemical Process Industries (Reviewer)Document78 pagesChemical Process Industries (Reviewer)Emier VillanuevaNo ratings yet
- State-Of-The-Art Reverse Osmosis Desalination PDFDocument77 pagesState-Of-The-Art Reverse Osmosis Desalination PDFJaime MoralesNo ratings yet
- Rice and Einkorn Wheat Husks Reinforced Poly (Lactic Acid) (PLA)Document14 pagesRice and Einkorn Wheat Husks Reinforced Poly (Lactic Acid) (PLA)Sharol Nathalia Garzon SerranoNo ratings yet
- Activity No 2 - PHENOLDocument4 pagesActivity No 2 - PHENOLpharmaebooks100% (4)
- 04042016000000A Avesta 2205 Covered ElectrodesDocument1 page04042016000000A Avesta 2205 Covered Electrodesmeckup123No ratings yet
- Research Framework FormDocument2 pagesResearch Framework FormMohd Hafiz AhmadNo ratings yet
- GTL TechnologyDocument24 pagesGTL Technologychaitanya_scribd100% (1)
- 009 - Pages From (Library of Physico-Chemical Property Data) Carl L (Version 1)Document10 pages009 - Pages From (Library of Physico-Chemical Property Data) Carl L (Version 1)SHAILENDRANo ratings yet
- PSA 50 Paper PDFDocument5 pagesPSA 50 Paper PDFshashi kant kumarNo ratings yet
- 15.1 Bronsted-Lowry Acids and BasesDocument6 pages15.1 Bronsted-Lowry Acids and BasesPatricia de LeonNo ratings yet
- Welding Low Alloy SteelsDocument14 pagesWelding Low Alloy SteelsNanda Al Alif100% (1)
- EN15376Document1 pageEN15376Ganciarov MihaelaNo ratings yet
- Grade 9 Day 2 TB Dqas 2nd QuarterDocument10 pagesGrade 9 Day 2 TB Dqas 2nd QuarterKwen Ann OrtigzNo ratings yet
- IB Chemistry HL Topic4 Questions 1.: O C H H ODocument21 pagesIB Chemistry HL Topic4 Questions 1.: O C H H OKhang Thinh TRANNo ratings yet
- As Chemistry Unit 2 NotesDocument26 pagesAs Chemistry Unit 2 Notesizzy 12100% (1)
- Penyerahan Dan Penilaian TugasanDocument3 pagesPenyerahan Dan Penilaian TugasanKumaResan SubramaniamNo ratings yet
- Oxalic Acid - C2H2O4 - PubChemDocument61 pagesOxalic Acid - C2H2O4 - PubChemMuhamad Risky 'chan'No ratings yet
- SOPs For ChemicalsDocument7 pagesSOPs For ChemicalselizasunderNo ratings yet
- Pharmaceutical and Medicinal Organic Chemistry Lab: Unit OutcomesDocument8 pagesPharmaceutical and Medicinal Organic Chemistry Lab: Unit OutcomesJUDYANN PINEDANo ratings yet
- 1 WeldingDocument52 pages1 WeldingAYUSH PATRANo ratings yet
- One Bath One Stage Dyeing of Polyester / Cellulosic Blends.Document31 pagesOne Bath One Stage Dyeing of Polyester / Cellulosic Blends.sanjay shettiNo ratings yet
- 1950 Barton A N D Mugdan-Vinyl Chloride: J.S.C.I., 6g, March, 7Document5 pages1950 Barton A N D Mugdan-Vinyl Chloride: J.S.C.I., 6g, March, 7Evan Afrista Wiokartina PurbaNo ratings yet
- AlplexDocument2 pagesAlplexWHWENNo ratings yet
- Organic Chemistry: Exercise - I Exercise - Ii Exercise-Iii Exercise Iv Answer KeyDocument39 pagesOrganic Chemistry: Exercise - I Exercise - Ii Exercise-Iii Exercise Iv Answer KeyRaju SinghNo ratings yet
- SINTESIS SURFAKTAN METIL ESTER SULFONAT DARI METIL ESTER MINYAK BIJI KARET (Havea Brasiliensis) MELALUI REAKSI SULFONASI DENGAN PENGARUH VARIASI KATALISDocument6 pagesSINTESIS SURFAKTAN METIL ESTER SULFONAT DARI METIL ESTER MINYAK BIJI KARET (Havea Brasiliensis) MELALUI REAKSI SULFONASI DENGAN PENGARUH VARIASI KATALISAffiano AkbarNo ratings yet
- Concrete and PlasticsDocument14 pagesConcrete and PlasticsYna Marie GutierrezNo ratings yet