0 ratings0% found this document useful (0 votes)
215 viewsPleural Effusion
Pleural Effusion
Uploaded by
Wan HafizPleural effusions can be classified as transudates or exudates based on protein levels. Transudates have protein levels <25g/L while exudates are >35g/L. Common causes of transudates include heart failure and liver disease. Common causes of exudates include infection, malignancy, and inflammation. Pleural fluid analysis and Light's criteria can help distinguish between transudates and exudates. Management may involve drainage and pleurodesis to prevent recurrence.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Pleural Effusion
Pleural Effusion
Uploaded by
Wan Hafiz0 ratings0% found this document useful (0 votes)
215 views12 pagesPleural effusions can be classified as transudates or exudates based on protein levels. Transudates have protein levels <25g/L while exudates are >35g/L. Common causes of transudates include heart failure and liver disease. Common causes of exudates include infection, malignancy, and inflammation. Pleural fluid analysis and Light's criteria can help distinguish between transudates and exudates. Management may involve drainage and pleurodesis to prevent recurrence.
Original Description:
Pleural Effusion powerpoint
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Pleural effusions can be classified as transudates or exudates based on protein levels. Transudates have protein levels <25g/L while exudates are >35g/L. Common causes of transudates include heart failure and liver disease. Common causes of exudates include infection, malignancy, and inflammation. Pleural fluid analysis and Light's criteria can help distinguish between transudates and exudates. Management may involve drainage and pleurodesis to prevent recurrence.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
215 views12 pagesPleural Effusion
Pleural Effusion
Uploaded by
Wan HafizPleural effusions can be classified as transudates or exudates based on protein levels. Transudates have protein levels <25g/L while exudates are >35g/L. Common causes of transudates include heart failure and liver disease. Common causes of exudates include infection, malignancy, and inflammation. Pleural fluid analysis and Light's criteria can help distinguish between transudates and exudates. Management may involve drainage and pleurodesis to prevent recurrence.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 12
Pleural effusion
Transudate : < 25g/L
Exudate > 35g/L
Blood: hemothorax, pus : empyema, lymph with fat : cylothorax, air
and blood : heamopneumothorax
causes
Transudate , 25g/L
CHF
Constrictive pericarditis
Fluid overload
Hypoproteinaemia eg. Cirrhosis,
nephrotic syndrome, malabsorption
Hypothyroidism
Meigs syndrome (rt PE with ovarian
fibroma)
Exudate > 35 g/L
Infection : pneumonia, TB,
Malignancy : bronchogenic ca,mets,
lymphoma, mesothelioma
Inflammation: SLE, RA
Clinical features
Dyspnoea
Pleuritic chest pain
Decrease chest expansion
Stony dullness on percussion
Diminished breath sound
Tactile fremitus, VR are decrease or absent
Bronchial breathing above the effusion
Tracheal deviation to opposite side
Other CF to look for
Stigmata of chronic liver dz
Malignancy*/ TB : cachexia, clubbing, Lymphadenopathy, mastectomy
scar*, radiations mark*
Cardiac failure
Hypothyroidism
Rheumatoid arthritis
Butterfly rash in SLE
Ix
CXR :blunt costophrenic angle, dense shadows with concave upper
border (meniscus sign). Detected PE if volume more than 250ml/
300ml
Ultrasound: site for pleural tap
Pleural fluid analysis
Pleural biopsy ( if pleural fluid analysis is inconclusive or clinical
suspicion of malignancy or TB)
Where to do tapping?
Percussed upper border of the effusion
Tap 1-2 intercostal below it.
Infiltrate pleural with 5-10mL 1% of lidocaine
Attached a 21G and insert it just upper border of the ribs ( lower
border has the neurovascular bundles)
Draw 10-30mL of the pleural fluid and send to lab for the
biochemistry (protein, glucose, pH, LDH, amylase) , bacteriology (TB
culture, microscopy ad stain, auramine stain), cytology, immunology
(RF, ANA, complement)
Pleural fluid analysis
Gross appearances:
Clear, straw colored: transudate, exudate
Turbid, yellow: empyema, parapneumonic effusion
Hemorrhagic: pulmonary infarction, trauma
Cytology
Neutrophils ++ : parapneumonic effusion, PE
Lymphocytes ++ : malignancy, TB, RA, SLE, sarcoidosis
Multinucleated giant cells: RA
Lupus erythematosus cells: SLE
Clinical chemistry
Protein : <25 g/L transudate; > 35 exudate, 25-35 g/L if pleural fluid
proteins/serum protein > 0.5 the effusion is exudate
Glucose: < 3.3mmol/L : Empyema, malignancy, TB, RA, SLE
pH <7.2 : Empyema, malignancy, TB, RA, SLE
LDH high (pleural: serum > 0.6): Empyema, malignancy, TB, RA, SLE
Amylase high: pancreatitis, Ca, esophageal rupture
Immunology
RF: RA
Antinuclear AB: SLE
Complement low: RA, SLE, malignancy, infections
Lights criteria
To distinguish pleural transudate from exudate
Pleural fluid is exudate if one or more criteria are met:
Pleural fluid protein: serum protein > 0.5
Pleural fluid ldh: serum ldh ratio > 0.6
Pleural fluid ldh> 2/3 UL of normal serum ldh
Mx
Drainage by pleural tap or intercostal drain (chest tube). Removed
slowly (<2L/24h). CX: Pneumothorax
Pleurodesis: tetracycline, bleomycin, talc
Surgery: remove one pleural so they can stick with chest wall
Case Presentations
You might also like
- English For NursingDocument16 pagesEnglish For NursingMaria Apostu StylesNo ratings yet
- 1 Ineffective Peripheral Tissue PerfusionDocument1 page1 Ineffective Peripheral Tissue Perfusionjean_fabulaNo ratings yet
- Pat 2 Medsurg1Document20 pagesPat 2 Medsurg1api-300849832No ratings yet
- Pleural Effusion Case StudyDocument5 pagesPleural Effusion Case Studyjanice ianNo ratings yet
- Dr. H. Achmad Fuadi, SPB-KBD, MkesDocument47 pagesDr. H. Achmad Fuadi, SPB-KBD, MkesytreiiaaNo ratings yet
- Insulin EffectsDocument24 pagesInsulin Effectsvag taoNo ratings yet
- Pleural Effusion Case StudyDocument31 pagesPleural Effusion Case StudyHomework PingNo ratings yet
- Case 1 - Pneumonia (Final)Document4 pagesCase 1 - Pneumonia (Final)Joegie ArioNo ratings yet
- DB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaDocument5 pagesDB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaNeil Alcazaren かわいいNo ratings yet
- Community-Acquired Pneumonia: Bello, Mickaela Bianca A. Gumiran, NomerDocument37 pagesCommunity-Acquired Pneumonia: Bello, Mickaela Bianca A. Gumiran, NomerKristine-Joy Legaspi FrancoNo ratings yet
- GE BasavaDocument21 pagesGE BasavaAmalin PrãdhãñNo ratings yet
- Blunt Abdominal TraumaDocument65 pagesBlunt Abdominal TraumaAmit MishraNo ratings yet
- Case Presentation: Presented byDocument34 pagesCase Presentation: Presented byZahid AnwarNo ratings yet
- Obstructive Uropathy Secondary To Benign Prostatic HyperplasiaDocument74 pagesObstructive Uropathy Secondary To Benign Prostatic HyperplasiaGregory Litang100% (1)
- Benign Prostatic Hypertrophy: Pathophysiology and EtiologyDocument4 pagesBenign Prostatic Hypertrophy: Pathophysiology and EtiologyErnestomalamionNo ratings yet
- Occurs Most Often In:: Muscular DystrophyDocument4 pagesOccurs Most Often In:: Muscular DystrophyJiezl Abellano AfinidadNo ratings yet
- Pathophysiology of BPHDocument1 pagePathophysiology of BPHJerome Matthew Hautea Amorado0% (1)
- Rheumatic Heart Disease Short Case PresentationDocument1 pageRheumatic Heart Disease Short Case PresentationPrerna SehgalNo ratings yet
- Pathophysiology of EsophagusDocument36 pagesPathophysiology of EsophagusShivani Lal0% (1)
- Chronic Obstructive Pulmonary DiseaseDocument76 pagesChronic Obstructive Pulmonary DiseasedidinNo ratings yet
- CholelithiasisDocument3 pagesCholelithiasisMIlanSagittarius0% (1)
- Nursing Care PlanDocument2 pagesNursing Care Planusama_salaymehNo ratings yet
- Case Study PnuemoniaDocument10 pagesCase Study PnuemoniaKyle B. Nacionales Ü100% (1)
- Chronic GastritisDocument7 pagesChronic GastritisDivina AquinoNo ratings yet
- Tension Pneumothorax PDFDocument2 pagesTension Pneumothorax PDFClarissa Aileen Caliva AdoraNo ratings yet
- CholelithiasisDocument6 pagesCholelithiasismarkzamNo ratings yet
- Acute Gastroenteritis in Children: Prepared By: Prof. Elizabeth D. Cruz RN, ManDocument12 pagesAcute Gastroenteritis in Children: Prepared By: Prof. Elizabeth D. Cruz RN, ManChaii De GuzmanNo ratings yet
- Choledecholithiasis Case StudyDocument8 pagesCholedecholithiasis Case StudyYuuki Chitose (tai-kun)No ratings yet
- COPD Case StudyDocument23 pagesCOPD Case StudyXinyun XuNo ratings yet
- Right Sided Heart FailureDocument18 pagesRight Sided Heart FailureShaf Abubakar100% (1)
- Case Study MijaresDocument55 pagesCase Study Mijaresiura echinNo ratings yet
- The Correlation Between Disease Stage and Pulmonary Edema Assessed With Chest Xray in Chronic Kidney Disease PatientsDocument6 pagesThe Correlation Between Disease Stage and Pulmonary Edema Assessed With Chest Xray in Chronic Kidney Disease PatientsAnnisa RabbaniNo ratings yet
- Acute Appendicitis Group CDocument40 pagesAcute Appendicitis Group CHeart TolenadaNo ratings yet
- Chronic GastritisDocument37 pagesChronic GastritisBondu Babu007No ratings yet
- Summary of Intravenous FluidDocument1 pageSummary of Intravenous FluidHshalalalaNo ratings yet
- MI Case Study FinalDocument25 pagesMI Case Study FinalAlmaNo ratings yet
- Abruptio Placentae: ALCANTARA, Eduardo L. Ms. Analinda R. Sese, RN, MANDocument45 pagesAbruptio Placentae: ALCANTARA, Eduardo L. Ms. Analinda R. Sese, RN, MANinscenekivir100% (1)
- Systemic Inflammatory Response SyndromeDocument12 pagesSystemic Inflammatory Response SyndromeninapotNo ratings yet
- MDRTB Case StudyDocument35 pagesMDRTB Case StudyFejlean Angelica AntineoNo ratings yet
- DiarrheaDocument11 pagesDiarrheaMade DhamaNo ratings yet
- Drug Study Pyrantel & CefuroximeDocument2 pagesDrug Study Pyrantel & CefuroximeMikhael Briones ApasNo ratings yet
- Reflective Journal 1Document4 pagesReflective Journal 1api-365605511No ratings yet
- Nontoxic Nodular GoiterDocument9 pagesNontoxic Nodular GoiterKayshey Christine ChuaNo ratings yet
- Anal Canal: Fissure in Ano HaemorrhoidsDocument37 pagesAnal Canal: Fissure in Ano Haemorrhoidsyash shrivastavaNo ratings yet
- NSTEMIDocument33 pagesNSTEMIwaazalimahwahidNo ratings yet
- Pulmonary EdemaDocument14 pagesPulmonary EdemaRizzamwah Catague100% (1)
- Nursing Interventions CHFDocument3 pagesNursing Interventions CHFbanyenye25100% (1)
- Foreign Body Airway ObstructionDocument15 pagesForeign Body Airway ObstructionKristine Anne SorianoNo ratings yet
- Lupus NephritisDocument15 pagesLupus NephritisVilza maharaniNo ratings yet
- Discharge Plan EndoDocument3 pagesDischarge Plan EndoCharlayne AnneNo ratings yet
- Discharge PlanDocument1 pageDischarge PlanBernalene SyNo ratings yet
- Urinalysis: PurposeDocument6 pagesUrinalysis: PurposebobtagubaNo ratings yet
- Leprosy CHNDocument14 pagesLeprosy CHNPhillip ChingNo ratings yet
- Benign Febrile Convulsion (BFC)Document8 pagesBenign Febrile Convulsion (BFC)Raj-el Delacruz100% (1)
- Chronic Kidney Disease Secondary To Type 2 Diabetes MellitusDocument84 pagesChronic Kidney Disease Secondary To Type 2 Diabetes Mellituswar5No ratings yet
- Acute GastroenteritisDocument13 pagesAcute Gastroenteritismarjorie_11No ratings yet
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- The politics of hunger: Protest, poverty and policy in England, <i>c.</i> 1750–<i>c.</i> 1840From EverandThe politics of hunger: Protest, poverty and policy in England, <i>c.</i> 1750–<i>c.</i> 1840No ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- Pleural EffusionDocument51 pagesPleural EffusionMinhajul IslamNo ratings yet
- Brochure Health ProfessionsDocument12 pagesBrochure Health ProfessionsWan HafizNo ratings yet
- Research Nih 3399393Document15 pagesResearch Nih 3399393Wan HafizNo ratings yet
- Atoto CompilationDocument100 pagesAtoto CompilationWan HafizNo ratings yet
- Nihms 632585jjkjkDocument18 pagesNihms 632585jjkjkWan HafizNo ratings yet
- Diabetes Mellitus ComplicationDocument4 pagesDiabetes Mellitus ComplicationWan HafizNo ratings yet
- Hyponatremia (Essay)Document3 pagesHyponatremia (Essay)Wan HafizNo ratings yet
- DIabetes InsipidusDocument3 pagesDIabetes InsipidusWan HafizNo ratings yet
- Ligature Material in HangingDocument5 pagesLigature Material in HangingWan HafizNo ratings yet
- Efficacy of Fluorochrome Stain in The Diagnosis of Pulmonary Tuberculosis Co-Infected With HIV - B - K Prasanthi, AR Kumari - B - , Indian Journal of Medical Microbiology PDFDocument4 pagesEfficacy of Fluorochrome Stain in The Diagnosis of Pulmonary Tuberculosis Co-Infected With HIV - B - K Prasanthi, AR Kumari - B - , Indian Journal of Medical Microbiology PDFWan HafizNo ratings yet
- Where Seamless Living Is Abridged: Site Plan Location MapDocument2 pagesWhere Seamless Living Is Abridged: Site Plan Location MapWan HafizNo ratings yet
- 0730 Cunningham Fluids and Electrolytes 2012Document19 pages0730 Cunningham Fluids and Electrolytes 2012Wan HafizNo ratings yet
- A P: A M A: Utopsy Athology Anual and TlasDocument2 pagesA P: A M A: Utopsy Athology Anual and TlasWan HafizNo ratings yet
- Pupillary DisorderDocument19 pagesPupillary DisorderWan HafizNo ratings yet
- Preface: Hematopathology Book, The Editors Decided For A Major ReviDocument1 pagePreface: Hematopathology Book, The Editors Decided For A Major ReviWan HafizNo ratings yet
- What Is Tortuous Artery?? A Tortuous Artery Is One That Twists and Winds in A "Tortuous" PathDocument1 pageWhat Is Tortuous Artery?? A Tortuous Artery Is One That Twists and Winds in A "Tortuous" PathWan HafizNo ratings yet
- The Realities of The Armenia-Azerbaijan Conflict: "What Do I Know About Azerbaijan"Document1 pageThe Realities of The Armenia-Azerbaijan Conflict: "What Do I Know About Azerbaijan"Wan HafizNo ratings yet
- The Cranial NervesDocument4 pagesThe Cranial NervesRadhikaManamNo ratings yet
- In The Name of ALLAH, The Most Beneficent, The Most Gracious, The Most Merciful !Document24 pagesIn The Name of ALLAH, The Most Beneficent, The Most Gracious, The Most Merciful !Wan HafizNo ratings yet
- 1 Litre of Tears DiaryDocument18 pages1 Litre of Tears Diarykhairapanda95No ratings yet
- Zoology+Lecturer+Past+Papers+ MergedDocument30 pagesZoology+Lecturer+Past+Papers+ MergedDarshana WaghaniNo ratings yet
- StandardDocument3 pagesStandardjonh dickNo ratings yet
- Investigatory ProjectDocument8 pagesInvestigatory ProjectAiren LianNo ratings yet
- Final MSSQLDocument6 pagesFinal MSSQL8020 Sakshi100% (1)
- Holistic DevelopmentDocument16 pagesHolistic DevelopmentArtem ParriñasNo ratings yet
- WBCS GAZETTE OCT - CompressedDocument57 pagesWBCS GAZETTE OCT - CompressedHarsh RanjanNo ratings yet
- Tsunami MP 820 Series Datasheet Eol USDocument3 pagesTsunami MP 820 Series Datasheet Eol USArif RahmanNo ratings yet
- Tanesco Tanzania - Specification S24 MV Load Break Fuse Cutouts With Arc Chutes (2000)Document42 pagesTanesco Tanzania - Specification S24 MV Load Break Fuse Cutouts With Arc Chutes (2000)Anonymous AoUv7Gz100% (1)
- Problem of UnfruitfulnessDocument6 pagesProblem of UnfruitfulnessRockyNo ratings yet
- Cygnus Energy LNG News Weekly 14th May 2021Document23 pagesCygnus Energy LNG News Weekly 14th May 2021Sandesh Tukaram GhandatNo ratings yet
- Volvo Wheel LoaderDocument16 pagesVolvo Wheel LoaderHewa PCNo ratings yet
- 2008 NRL ReviewDocument250 pages2008 NRL ReviewU.S. Naval Research LaboratoryNo ratings yet
- Sight Words Worksheet Free 3rd Grade Word Search 1Document1 pageSight Words Worksheet Free 3rd Grade Word Search 1MUHAMMAD ZAIYAN BIN MOHAMAD ZAMRINo ratings yet
- Bhsa Inggris'Document5 pagesBhsa Inggris'Dwi NovianaNo ratings yet
- Perancangan Ringkasan RPT Sains Tingkatan 3 2022 - 2023Document2 pagesPerancangan Ringkasan RPT Sains Tingkatan 3 2022 - 2023RosmizaNo ratings yet
- Datsun Blue Bird Parts Catalog 410 411 1964 68Document20 pagesDatsun Blue Bird Parts Catalog 410 411 1964 68andrea100% (62)
- 2023 MISTRAL ATLAS DatasheetDocument2 pages2023 MISTRAL ATLAS DatasheetYaser TrujilloNo ratings yet
- By: Engr. Ronald John R. CajillaDocument1 pageBy: Engr. Ronald John R. CajillareynoldNo ratings yet
- Research Report 249: Transport and Road Research LaboratoryDocument23 pagesResearch Report 249: Transport and Road Research LaboratorydaraaamaaadiNo ratings yet
- Vegetation of California Fan Palm Oases On The San Andreas FaultDocument5 pagesVegetation of California Fan Palm Oases On The San Andreas FaultErsarsit GeaNo ratings yet
- Drop SocioEconomic ImpactDocument7 pagesDrop SocioEconomic ImpactChan ZyNo ratings yet
- Inmarsat Vocality Radio Over IPDocument8 pagesInmarsat Vocality Radio Over IPJorge CasaliNo ratings yet
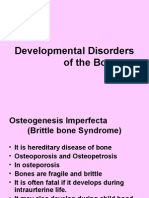
- Developmental Disorder of The BoneDocument14 pagesDevelopmental Disorder of The BoneArslan SiddiquiNo ratings yet
- Anaesthesia MDMS QuestionDocument54 pagesAnaesthesia MDMS QuestionDipesh ShresthaNo ratings yet
- Non Peza ClientsDocument15 pagesNon Peza ClientsDioscoro J. Jebulan100% (1)
- Roger Dunn Spring CatalogDocument52 pagesRoger Dunn Spring Catalogstig-rdNo ratings yet
- Đề tiếng Anh cấp 3Document5 pagesĐề tiếng Anh cấp 3dinhthien1016No ratings yet
- Textile Printers FESPA 09Document24 pagesTextile Printers FESPA 09Marco MaanNo ratings yet
- JD 5 Relay CatalogDocument3 pagesJD 5 Relay Catalogjimmy barusNo ratings yet