0 ratings0% found this document useful (0 votes)
39 viewsAcute Viral Hepatitis B Anggita Nur Aziza
Acute Viral Hepatitis B Anggita Nur Aziza
Uploaded by
Anggita Nur AzizaThis document describes a case of a 45-year-old male patient presenting with acute viral hepatitis B. The patient reports pain in the upper right abdomen, fever, nausea, vomiting, back and leg pain, loss of appetite, weight loss, and shortness of breath. A physical exam finds hepatomegaly and splenomegaly. Laboratory tests show elevated liver enzymes and the presence of HBsAg, consistent with acute hepatitis B. The patient is given IV fluids and medications to manage symptoms as the viral infection runs its course.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Acute Viral Hepatitis B Anggita Nur Aziza
Acute Viral Hepatitis B Anggita Nur Aziza
Uploaded by
Anggita Nur Aziza0 ratings0% found this document useful (0 votes)
39 views28 pagesThis document describes a case of a 45-year-old male patient presenting with acute viral hepatitis B. The patient reports pain in the upper right abdomen, fever, nausea, vomiting, back and leg pain, loss of appetite, weight loss, and shortness of breath. A physical exam finds hepatomegaly and splenomegaly. Laboratory tests show elevated liver enzymes and the presence of HBsAg, consistent with acute hepatitis B. The patient is given IV fluids and medications to manage symptoms as the viral infection runs its course.
Original Description:
Hepatitis B
Original Title
CASE 1
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
This document describes a case of a 45-year-old male patient presenting with acute viral hepatitis B. The patient reports pain in the upper right abdomen, fever, nausea, vomiting, back and leg pain, loss of appetite, weight loss, and shortness of breath. A physical exam finds hepatomegaly and splenomegaly. Laboratory tests show elevated liver enzymes and the presence of HBsAg, consistent with acute hepatitis B. The patient is given IV fluids and medications to manage symptoms as the viral infection runs its course.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
39 views28 pagesAcute Viral Hepatitis B Anggita Nur Aziza
Acute Viral Hepatitis B Anggita Nur Aziza
Uploaded by
Anggita Nur AzizaThis document describes a case of a 45-year-old male patient presenting with acute viral hepatitis B. The patient reports pain in the upper right abdomen, fever, nausea, vomiting, back and leg pain, loss of appetite, weight loss, and shortness of breath. A physical exam finds hepatomegaly and splenomegaly. Laboratory tests show elevated liver enzymes and the presence of HBsAg, consistent with acute hepatitis B. The patient is given IV fluids and medications to manage symptoms as the viral infection runs its course.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 28
ACUTE VIRAL HEPATITIS B
Anggita Nur Aziza
*
*
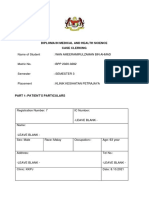
Name : Mr. Y
Age : 45 y.o
Sex : Male
Address : Sukajaya Kampung
Pinayungan RT 14 RW 06
Kecamatan Teluk Jambe Timur
Kabupaten Karawang
Occupation : Computer Labour
Religion : Muslim
Marital status : Married
Date of addmision : October 23
rd
2011
Taken from : Rengasdengklok
Pain in upper right abdomen
since 2 days before
hospitalized
Chief
complaint
Fever
Nausea and vomitting
Aches from back waist to
feet
Hasnt been defecated for 2
days
Additional
complaint
*
*Patient came with pain in upper right abdomen
since 2 days before hospitalized. It felt sharp,
continously, not radiating and day by day is
getting worse especially when the patient lying
down.
*Beside the pain, the patient also felt aches
from back waist to feet, nausea and vomitting,
and fever.
*Fever starts from 2 days before hospitalized, intermittent.
*Nausea and vomitting starts from 2 days before hospitalized,
vomitted about 2 times, food in its contain, blood (-)
*The aches from back waist felt since 1 days before
hospitalized, sharp, continously, worsened when the patient
is walking and sit down.
*Theres no pain and no dripping when he is urinating. The
patient hasnt been defecated since 2 days before
hospitalized. He also loss his appetite and loss weight since a
month ago.
*Dizziness, fatigue, cough, pain in chest are denied.
*Lately, patient said that the pain in abdomen and back waist
is decreased. But the patient feel shortness of breath since
last night, and swollen in his feet.
*
Same
condition (+)
Hypertension
(-)
Diabetes
mellitus (-)
Cardiovasular
(-)
Kidney (-) Allergy (-)
*
Same
condition (-)
Hypertension
(-)
Diabetes
mellitus (-)
Cardiovasular
(-)
Kidney (-) Allergy (-)
Had gone to puskesmas
2 days before
hospitalized and get
medicated
Herbal medicine (-)
Blood transfusion (+)
PAST MEDICAL
HISTORY
*
Smoke (-)
Alcohol (-
)
Tattoo (-)
Free sex
(-)
Narcotics
(-)
Injection
drugs (-)
He didnt
exercise
regularly
*
Severely ill
General
appearance
Compos
mentis
Conciousness
Vital
Sign
BP:
130/70
mmHg
RR:
24x/min
Temp:
37,5
0
c
HR:
120x/min
*
Head
Normocephaly
Eyes
Conjunctiva anemic -/-
Sclera icteric -/-
Ears
Normotia
Secret -/-
Serumen -/-
Nose
Sepeum deviation -
Secret -/-
Concha normal
Mouth
Dirty mouth -
Dry mouth -
Dry tongue -
Throat
Tonsils T1/T1
Faring hiperemis (-)
Neck
Lymph gland is not palpable
Thyroid gland is not palpable
JVP 5+2 cm
Inspection:
Symmetrical
Palpation:
Equal vocal fremitus
Percusion:
Sonor in both lung
Auscultation:
Vesicular breath sound in both
lung, no ronchi and wheezing
Inspection:
Ictus cordis is invisible, spider
nevi (-)
Palpation:
Ictus cordis is palpable at 5
th
ICS
LMCS
Percution:
no enlargment
Auscultation:
Regular I - II heart sound no
murmur and gallop
*
*
Inspection
Brown skin, bulging abdomen, icteric (-), caput meducae (-)
Palpation
Pain present on palpation at right hypochondrium region
Liver palpable 3 fingers under arcus costae, soft consistency, sharp
edge, flat surface, tenderness (-)
Spleen palpable at Schuffner 4, soft consistency, sharp edge, flat
surface, tenderness (-)
Shifting dullness (-)
Percussion
No pain present on abdominal percussion
Dullness
CVA (-)
Auscultation
Bowel sound (+). Arterial bruit (-), venous hum (-)
*
*Warm acrals
*Oedema
+ +
+ +
+ -
+ +
*
October 23rd 2011 Patient result Normal range
Hb 8.00 % 12 17 g%
Leukocyte 5.100/uL 5000-10.000/uL
Trombocyte 227.000 150.000-450.000
Ht 24 % 37-48 %
HbsAg + -
GDS 105 mg/dl 80-140 mg/dl
Ureum 66,2 mg/dl 10-45 mg/dl
Creatinine 1.39 mg/dl 0.4-1.5 mg/dl
Albumin 3,10 3.5-5.0 mg %
SGOT 56 < 40 u/l
SGPT 36 < 40 u/l
*
October 24th 2011 Patient result Normal range
Protein total 6,05 mg% 6.5 8.5 mg%
Albumin 3,22 mg% 3.5 5 mg%
Globulin 2,83 mg% 2.6 3.6 mg%
Total Bilirubin 0,68 mg/dl < 1.1 mg/dl
Direct Bilirubin 0,37 mg/dl < 0.6 mg/dl
Indirect Bilirubin 0,31 mg/dl < 0.5 mg/dl
SGOT 650 u/l < 40 u/l
SGPT 429 u/l < 40 u/l
*
October 25th
2011
Patient result Normal range
Ureum 33.3 10-45 mg/dl
Creatinin 1.30 0.4-1.5 mg/dl
*
Symptoms Signs Laboratory and others
Pain in upper right
abdomen
Fever
Nausea and vomitting
Aches form back waist
untill feet
Hasnt been defecated
for 2 days
Loss of appetite
Weight loss
Shortness of breath
Swollen in feet
Vital sign:
BP: 130/70 mmHg
HR: 120 x/min
RR: 24 x/min
T: 37.5
0
c
Abdomen:
Bulging abdomen
Hepatomegali and
splenomegali
sounds dull
Hb: 8.0 g%
Ht: 24 %
HbsAg: +
Ureum: 69 mg/dl
Creatinine: 1.94 mg/dl
Protein total : 6.05 %
Albumin: 3.10 mg%
Globulin: 2.83 mg%
Total bilirubin: 0.68 mg/dl
Direct bilirubin: 0.37
mg/dl
Indirect bilirubin: 0.31
mg/dl
SGOT: 650 u/l
SGPT: 429 u/l
*
1. Acute viral hepatitis B
2. Chronic hepatitis B
3. Acute non viral hepatitis B
4. Cirrhosis hepatis
5. Cholelithiasis
*
Acute viral hepatitis B
*
*Imunoserologic examination
*USG
*Urinalysis
*Liver biopsy
*
*IVFD RL 20 tpm
*IVFD Aminofusin hepar
*Ranitidin 2 x 1 amp
*Curcuma 3 x 1 tab
*Meloxicam 1 x 15 mg
*Alprazolam 1 x 0.5 mg
*Neurodex 2 x 1 tab
*Laxadin 2 x C II
*
Ad
fungsionam
: dubia ad
malam
Ad sanationam
: dubia ad
malam
Ad vitam :
dubia ad
bonam
You might also like
- Antepartum HemorrhageDocument21 pagesAntepartum HemorrhageNidhi SharmaNo ratings yet
- (D. J. Begley BSC, PHD, J. A. Firth MA, PHD, J. R. PDFDocument259 pages(D. J. Begley BSC, PHD, J. A. Firth MA, PHD, J. R. PDFali razaNo ratings yet
- DMDFDocument22 pagesDMDFsujal177402100% (1)
- Duty Report Er 23 07 2015Document25 pagesDuty Report Er 23 07 2015Auditya WidyasariNo ratings yet
- MR GoutyDocument25 pagesMR GoutyArvindan SubramaniamNo ratings yet
- Janiar, Female, 74 Yo, HCU 12Document11 pagesJaniar, Female, 74 Yo, HCU 12Melsa AprimaNo ratings yet
- Apriyanto Lifandy Desmy FadillahDocument38 pagesApriyanto Lifandy Desmy FadillahdesmyyNo ratings yet
- 9 December 2023 Obstructive Jaundice Ec Susp Hepatic TumorDocument13 pages9 December 2023 Obstructive Jaundice Ec Susp Hepatic Tumorkamilmarsal1No ratings yet
- Case Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaDocument39 pagesCase Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaFarella KartikaNo ratings yet
- Duty Report - Rosni (DR - Gari)Document9 pagesDuty Report - Rosni (DR - Gari)RudiErwinKurniawanNo ratings yet
- Duty Report - Rosni (DR - Gari)Document9 pagesDuty Report - Rosni (DR - Gari)RudiErwinKurniawanNo ratings yet
- Diploma in Medical and Health Science Case ClerkingDocument11 pagesDiploma in Medical and Health Science Case ClerkingWan AmeeramirulzamanNo ratings yet
- Case DM + HypertensionDocument27 pagesCase DM + Hypertensioncendy andestriaNo ratings yet
- Anamnesis: Autoanamnesis On March 22 ND 2017 Chief Complaint General Weekness 1 Day AgoDocument25 pagesAnamnesis: Autoanamnesis On March 22 ND 2017 Chief Complaint General Weekness 1 Day AgoTebeNo ratings yet
- Yulnova, Acute On CKD and Thrombocytopenia, Duty HannaDocument18 pagesYulnova, Acute On CKD and Thrombocytopenia, Duty HannaHanna GustinNo ratings yet
- Case Illustration: TH THDocument6 pagesCase Illustration: TH THdigimon666No ratings yet
- A Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaDocument34 pagesA Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaJobaer MahmudNo ratings yet
- Heri Sunoto, CKD CHF, Duty HannaDocument17 pagesHeri Sunoto, CKD CHF, Duty HannaHanna GustinNo ratings yet
- CR Piopneumothoraks Nicky FIXdDocument62 pagesCR Piopneumothoraks Nicky FIXdPutri RahmawatiNo ratings yet
- Upper GI BleedingDocument70 pagesUpper GI BleedingMia MusNo ratings yet
- Morning Report RakaDocument19 pagesMorning Report Rakaraka widhiartaNo ratings yet
- Case PresentationDocument20 pagesCase PresentationMohamad HafyfyNo ratings yet
- Duty Report Chronic Kidney Diseases, DM and GERD: Approach of Complexity ProblemDocument15 pagesDuty Report Chronic Kidney Diseases, DM and GERD: Approach of Complexity ProblemGiovina FajarNo ratings yet
- CFGVDocument28 pagesCFGVmyolie wuNo ratings yet
- Bedah 21 Nov 2022 + FU 19 Nov 22 + Patof.Document28 pagesBedah 21 Nov 2022 + FU 19 Nov 22 + Patof.maya_rosmariaNo ratings yet
- Sri Pertiwi, Syok Sepsis CAPDocument14 pagesSri Pertiwi, Syok Sepsis CAPLukman NurhakimNo ratings yet
- Imed Case 5Document11 pagesImed Case 5Shakshi RainaNo ratings yet
- Case Base DiscussionDocument19 pagesCase Base DiscussionNu JoeNo ratings yet
- NCP An - MVDocument7 pagesNCP An - MVMahendri Deayu PutriNo ratings yet
- LeptospirosisDocument19 pagesLeptospirosisFelicia adeline ChristianNo ratings yet
- Mastoera, Female, 87 Yo, HCU 8Document10 pagesMastoera, Female, 87 Yo, HCU 8Melsa AprimaNo ratings yet
- Duty ReportDocument12 pagesDuty ReportRudiErwinKurniawanNo ratings yet
- Case Conference February 1st 2018Document26 pagesCase Conference February 1st 2018Efan StiawanNo ratings yet
- Presentasi Kasus Dokter Arif Cynthia NataliaDocument26 pagesPresentasi Kasus Dokter Arif Cynthia NataliaIntan SorayaNo ratings yet
- Yetti, CAP Hipoxia, Duty HannaDocument18 pagesYetti, CAP Hipoxia, Duty HannaHanna GustinNo ratings yet
- Baru Titi Sumarni, Melena Uremic Bleeding, CKD Stage V, Oa GenuDocument15 pagesBaru Titi Sumarni, Melena Uremic Bleeding, CKD Stage V, Oa GenuherdianNo ratings yet
- Neli Pastinar, Penkes UE, RPGN, SLE, Duty HannaDocument19 pagesNeli Pastinar, Penkes UE, RPGN, SLE, Duty HannaHanna GustinNo ratings yet
- Morning Report Case: 17th Dec 2013Document22 pagesMorning Report Case: 17th Dec 2013SunardiasihNo ratings yet
- Vier Marleiny, Melena Gastropathy Nsaid, Duty HannaDocument19 pagesVier Marleiny, Melena Gastropathy Nsaid, Duty HannaHanna GustinNo ratings yet
- Syafrudin, Male, 58 Yo, MW 11: Chief Complaint: (Autoanamnesis and Alloanamnesis) Present Illness HistoryDocument14 pagesSyafrudin, Male, 58 Yo, MW 11: Chief Complaint: (Autoanamnesis and Alloanamnesis) Present Illness HistoryLukman NurhakimNo ratings yet
- Case Conference Sunday Night Shift, October 14 2018Document26 pagesCase Conference Sunday Night Shift, October 14 2018Hendra WardhanaNo ratings yet
- Liver Function Test FinalDocument98 pagesLiver Function Test FinalHussain Azhar100% (1)
- Wa0008.Document14 pagesWa0008.Mahendra NitharwalNo ratings yet
- Lapjag 10 Feb 2016 - AnemiaDocument25 pagesLapjag 10 Feb 2016 - AnemiamyoganoNo ratings yet
- MburiDocument11 pagesMburirahmaNo ratings yet
- Muhammad Nur, Penkes Ec SAE DD Hypoxia, Duty HannaDocument16 pagesMuhammad Nur, Penkes Ec SAE DD Hypoxia, Duty HannaHanna GustinNo ratings yet
- Kistiyanto - SIDA ToxoDocument13 pagesKistiyanto - SIDA ToxoAgung Pratama YudhaNo ratings yet
- Case DR SigitDocument71 pagesCase DR SigitandreNo ratings yet
- Intraoperatively Inadequate BlockMORBIDITY ProtocolDocument9 pagesIntraoperatively Inadequate BlockMORBIDITY Protocoldocv526No ratings yet
- Rheumatoid Arthritis LapsusDocument37 pagesRheumatoid Arthritis Lapsusderahmat dedyNo ratings yet
- Case CHF, Cap, DM Tipe 2 - Dr. Ruddy, SP - PDDocument34 pagesCase CHF, Cap, DM Tipe 2 - Dr. Ruddy, SP - PDMelisaNo ratings yet
- LAPORAN TUTORIAL Case 1 Kelompok B5 - Hepatitis SirosisDocument35 pagesLAPORAN TUTORIAL Case 1 Kelompok B5 - Hepatitis SirosisTutde SedanaNo ratings yet
- Morning Report YusmustiDocument9 pagesMorning Report YusmustiAfdhol FalahNo ratings yet
- AnasarcaDocument9 pagesAnasarcaKAMRAN AHMADNo ratings yet
- Uterine Myoma With Cystic DegenertionDocument17 pagesUterine Myoma With Cystic DegenertionMeizaNo ratings yet
- Duty DewiDocument13 pagesDuty DewiLukman NurhakimNo ratings yet
- MR BP Dan AsphyxiaDocument29 pagesMR BP Dan AsphyxiaRizky FajriNo ratings yet
- CC 22 Sept Pneumonia KolestasisDocument60 pagesCC 22 Sept Pneumonia KolestasisIka Juli2018No ratings yet
- Ny.T PEB Eng Tim Dinas 2Document23 pagesNy.T PEB Eng Tim Dinas 2arifsandroNo ratings yet
- Death Case: DR Levina DR Muhammad Fauzan AssegafDocument45 pagesDeath Case: DR Levina DR Muhammad Fauzan AssegafWiwik Puji LestariNo ratings yet
- Febrianto, Sepsis Ec HAP, PIS, Duty HannaDocument17 pagesFebrianto, Sepsis Ec HAP, PIS, Duty HannaHanna GustinNo ratings yet
- Nogales V Capitol Medical CenterDocument8 pagesNogales V Capitol Medical Centercha cha100% (1)
- 1 Historical ReviewDocument3 pages1 Historical ReviewNoraNo ratings yet
- ICDAS Chart ClujDocument2 pagesICDAS Chart Clujpiece_of_mindzz1969No ratings yet
- Phos 313 - Activity No 7 PhosDocument6 pagesPhos 313 - Activity No 7 PhosDIANA CAMILLE CARITATIVONo ratings yet
- L LocationDocument2 pagesL LocationZee MirzaNo ratings yet
- Indications and Risks of Vacuum Assisted Deliveries.: OriginalDocument2 pagesIndications and Risks of Vacuum Assisted Deliveries.: OriginalgagagigoNo ratings yet
- The Advantages and Disadvantages of Being A DoctorDocument2 pagesThe Advantages and Disadvantages of Being A DoctorSindi M. Dallashi100% (1)
- Your Baby, Your Way Taking Charge of Your Pregnancy, Childbirth, and Parenting Decisions For A Happier, Healthier Family by Jennifer MargulisDocument8 pagesYour Baby, Your Way Taking Charge of Your Pregnancy, Childbirth, and Parenting Decisions For A Happier, Healthier Family by Jennifer MargulisSimon and Schuster100% (1)
- PathReport4 PDFDocument4 pagesPathReport4 PDFGohar Ali UsmanNo ratings yet
- Interpersonal RelationshipDocument161 pagesInterpersonal Relationshipdhiren1529No ratings yet
- Labor and Birth ProcessesDocument54 pagesLabor and Birth Processesclccorner100% (1)
- GMC Claim Form How To File A ClaimDocument4 pagesGMC Claim Form How To File A ClaimtweetknotNo ratings yet
- Anesthesia For GeriatricDocument23 pagesAnesthesia For GeriatricTommy ArisandyNo ratings yet
- TOP 500 CPT® CODES For WOMEN'S HEALTH NURSE PRACTITIONERSDocument2 pagesTOP 500 CPT® CODES For WOMEN'S HEALTH NURSE PRACTITIONERSbritofernandezaNo ratings yet
- Death Claimant StatementDocument4 pagesDeath Claimant Statementcet.ranchi7024No ratings yet
- Peter B. Fodor MD FACS: 2080 Century Park East, Suite 710 Los Angeles, CADocument2 pagesPeter B. Fodor MD FACS: 2080 Century Park East, Suite 710 Los Angeles, CAPeter FodorNo ratings yet
- Unit - I: Introduction To Pediatric NursingDocument45 pagesUnit - I: Introduction To Pediatric Nursingbereket gashu100% (2)
- Cases Blank FormDocument6 pagesCases Blank FormIara CruzNo ratings yet
- Modified Duke's Criteria For Infective Endocarditis - Mnemonic - EpomedicineDocument5 pagesModified Duke's Criteria For Infective Endocarditis - Mnemonic - EpomedicineAsmaNo ratings yet
- NN.14.01 Sponge BathDocument3 pagesNN.14.01 Sponge BathBaban RajpurNo ratings yet
- Emergency RoomDocument2 pagesEmergency Roomharpreet kaur brar100% (1)
- Antenatal ExaminationDocument18 pagesAntenatal ExaminationMiu MiuNo ratings yet
- Pulp CappingDocument59 pagesPulp Cappingதிருவேங்கடம் கோபாலன்No ratings yet
- Midterm Lecture ExamDocument5 pagesMidterm Lecture ExamMartin Clyde100% (2)
- Lesson Plan On Episiotomy CareDocument7 pagesLesson Plan On Episiotomy Careanu aaNo ratings yet
- NCPDocument2 pagesNCPRicher John PolicarpioNo ratings yet
- Labreport AspxDocument1 pageLabreport Aspxazeemkhalid09876No ratings yet
- Concise CardiologyDocument354 pagesConcise CardiologyAtish_Mathur_9874No ratings yet