8.mid
- 2. 2
- 3. Previous questions • Minimal invasive dentistry Apr 2010, 2014 3
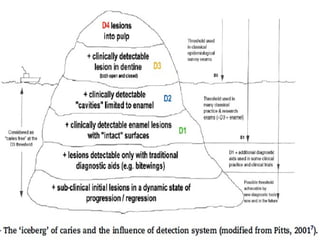
- 4. Contents • Introduction • Definition • History • Principles of MID • Motives for minimal invasive dentistry • Caries diagnostic aids • Iceberg of caries • Potential factors 4
- 5. • Cavity design principles • Minimal invasive preparation techniques ART Chemo-mechanical caries removal Air- abrasion Sono-abrasion Lasers Ozone therapy Polymer cutting instruments Silver diamine fluoride • Conclusion • References 5
- 6. INTRODUCTION • Prevention, remineralization and minimal intervention for the placement and replacement of restorations. • The ultimate goal of minimal intervention is to extend the life of restored teeth with as less intervention as possible. • When operative care is indicated, it should be aimed at “PREVENTION OF EXTENSION” rather than “EXTENSION FOR PREVENTION”. 6
- 7. DEFINITION • Minimum Invasive Dentistry (MID) can be defined as a philosophy of professional care, concerned with the first- occurrence, earliest detection and earliest possible cure of disease on micro (molecular) levels, followed by minimal invasive and patient friendly treatment in order to repair irreversible damages caused by such disease. (FDI Commission, 2002) 7
- 8. 8 Prevention and treatment of dental caries lesions forming in enamel pits and fissures can be challenging because of factors such as the "hidden caries" phenomenon, types of materials to use, methods of bonding restorative materials, and concerns for conserving tooth structure.
- 9. 9 Recent trends in caries prevention Recent trends in oral prevention Recent advances in HIV diagnosis Recent trends in Preventive dentistry • Fluorides • ART • Caries Vaccine • Xylitol • Ozone • Replacement therapy • Antibacterial and antimicrobial agents • Caries detection methods • Tretinoin Biofilm • DNA Vaccine and Oral cancer preventi on • Ora sure • Ora quic k Recent Advances in pit and fissure sealants • Microscopic identification • Cultures • PCR • Genetic analyses • Enamel matrix derivatives • Bisphosphonate s • Photodynamic therapy • Local antimicrobial delivery systems Recent trends in periodontal disease prevention • Fluoride releasing sealants • ACP-pit & fissure sealants. • Glass ionomers as sealants. • Moisture tolerant pit & fissure sealants. • Etch- free pit & fissure sealants. • Pen type handling of sealants. • Fissure sealants with color change technology. • Nano composites as sealants. •Harshpriya et al, recent trends in preventive dentistry-A review; SRM University dental journal, 2011;2(3):23 2-237
- 10. HISTORYHISTORY 1900 - 'Extension for Prevention': G.V.Black 1912 - Hyatt introduced Prophylactic Odontomy 1951 - Dr. J. Tim Rainey introduced Air Abrasion 1954 - Bunocore introduces Acid etching 1964 - Bowen introduced Resin 1980’s – ART & Caridex 10
- 11. • 1998 - Carisolv • 1999 - Dr.Hugo & Mosele introduce caries excavation by Sonoabrasion • 2000 - Baysan & Lynch - introduced Ozone Therapy for arresting dental caries. • 2004 onwards - Dr Lawrence proposes genetically modified organisms to prevent caries. • Frietas describes the application of concept of Nanodentistry to treat dental caries Dentistry has moved beyond the surgical approach Now - heal a carious lesion, at least in its early stages 11
- 12. Principles of Minimal Intervention Dentistry 1. Modification of the oral flora / Reduction of cariogenic bacteria 2. Patient education 3. Remineralization of non-cavitated lesions (early lesions) of enamel and dentin 4. Minimal surgical intervention of cavitated lesions / Disease control 5. Repair rather than replacement of defective restorations 12
- 13. MOTIVES FOR MID • Early diagnosis of lesions and accurate risk assessments are available. • The extensive knowledge on caries progression rates . • Adhesive restorative materials and techniques promote less removal of healthy tissues . • High risk for Iatrogenic effects. 13
- 14. CARIES DIAGNOSTIC AIDS 1. Visual Method 2. Visual – Tactile method 3. Elective Temporary Tooth Separation 4. Magnification 5. Radiographic method 6. Laser fluorescence method 7. Fiber-optic transillumination method (FOTI) 8. Electrical conductive method 9. Ultra Violet illumination method 14
- 15. 10.Endoscope / Videoscope 11.Dye penetration method 12.Iodide Penetration 13.Multi-Photon Imaging 14.Infrared Thermography 15.Infrared Fluorescence 16.Ultra sonic imaging 15
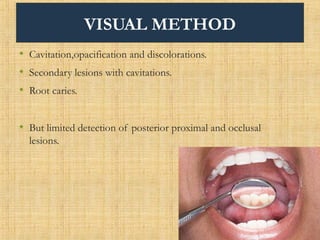
- 16. VISUAL METHOD • Cavitation,opacification and discolorations. • Secondary lesions with cavitations. • Root caries. • But limited detection of posterior proximal and occlusal lesions. 16
- 17. VISUAL - TACTILE METHOD • Determining roughness or softness of the tooth surface with a sharp explorer. • May transmit cariogenic bacteria from one site to another • May produce irreversible traumatic defects in potentially remineralisable non-cavitated lesions of enamel and dentin. 17
- 18. Mechanical binding of on explorer tip in a fissure may not be because of caries but due to other causes like. a. Shape of the fissure b. Sharpness of explorer: A sharp explorer has a diameter of 200microns c. Force of application 18
- 19. ELECTIVE TEMPORARY TOOTH SEPARATION • Elastomeric separating modules (separators) (Rimmer and Pits 1990) • Diagnosis of caries in proximal smooth surface 19
- 20. Magnification • Essential aid to diagnose small cavities & initial lesions • High reproducibility of results 20
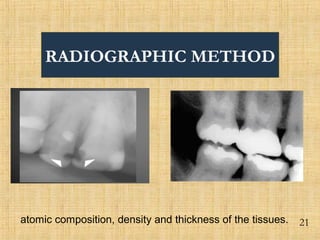
- 21. RADIOGRAPHIC METHOD 21atomic composition, density and thickness of the tissues.
- 22. 22
- 23. 23 Advantages: 1.The depth of a lesion 2.Relation between the lesion and the pulp of the tooth. 3.Aproximal lesions. 4.Non-invasive method while probing may cause a break of the enamel covering a subsurface lesion. 5.Lasting documentation.
- 24. LIMITATIONS: 1. Two dimensional image of three-dimensional object. 2. Under estimations or over estimations due to projection errors. 3. Radiolucency cannot be judged whether this is due to caries or resorption or any other defect. 4. Proximal secondary caries on the more apical part of a restoration may not be detected. 24
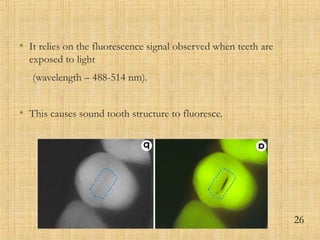
- 25. Laser fluorescence method Quantitative Light Induced fluorescence (QLF) method • Diagnostic tool for in vivo and in vitro quantitative assessment of dental caries, plaque, calculus, staining. • images are captured into the computer and stored in an image database. • Optional quantitative analysis tools enable the user to quantify parameters like mineral loss, lesion depth, lesion size, stain size and severity with high precision and repeatability. 25
- 26. • It relies on the fluorescence signal observed when teeth are exposed to light (wavelength – 488-514 nm). • This causes sound tooth structure to fluoresce. 26
- 27. • It is a two step method - The first step involves image acquisition with CCD camera. - The second step involves image analysis, using the software. 27
- 28. DIAGNODENT • It is the chair side, battery powered quantitative diode laser fluorescence device. • It measures the fluorescence of bacterial products within carious lesions 28
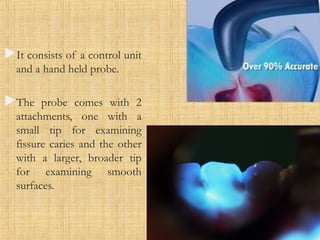
- 29. It consists of a control unit and a hand held probe. The probe comes with 2 attachments, one with a small tip for examining fissure caries and the other with a larger, broader tip for examining smooth surfaces. 29
- 30. FIBER OPTIC TRANS ILLUMINATION (FOTI) • It works under the principle that since a carious lesion has a lowered index of light transmission, an area of caries appears as a darkened shadow that follows the spread of decay through the dentine. 30
- 31. 31 ADVANTAGES No hazards of radiation Simple and comfortable for the patients Lesions which cannot be diagnosed radiographically can be diagnosed by this method Less time consuming DISADVANTAGES Permanent records are difficult to maintain as in radiographs Difficult to locate probe in certain areas
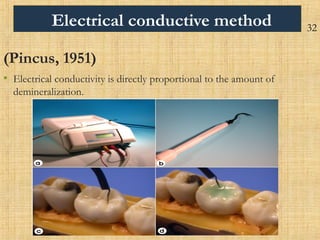
- 32. Electrical conductive method (Pincus, 1951) • Electrical conductivity is directly proportional to the amount of demineralization. 32
- 33. ADVANTAGES: •Very effective in detecting early pit and fissure caries •It can monitor the progress of caries during caries control programme. DISADVANTAGES: •It can only recognize demineralization and not caries specifically. •Presence of enamel cracks may lead to false positive diagnosis 33
- 34. The observation of the colouring can be qualitative or quantitative. Qualitative assessment is observation for colour difference and quantitative assessment is determination of the intensity of colour. Both fluorescent and non fluorescent dyes have been used for staining the porous carious lesion. 34 CARIES DETECTOR DYES
- 35. • “Procion” and “Calcein” dyes stain enamel lesions. • Basic fuchsine red stain was developed to differentiate between 2 layers of carious dentin. . 35
- 37. 37
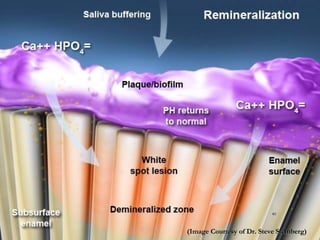
- 38. POTENTIAL FACTORS 1. Deminerlization – Remineralization cycle 2. Adhesion in restorative dentistry 3. Biomimetic restorative material 38
- 39. 39
- 40. (Image Courtesy of Dr. Steve Steinberg)(Image Courtesy of Dr. Steve Steinberg) 40
- 41. (Image Courtesy of Dr. Steve Steinberg)(Image Courtesy of Dr. Steve Steinberg) 41
- 42. Adhesion in restorative dentistry Two forms of adhesion are available; i. Micromechanical union between tooth surface and restorative material - beveling the enamel cavity margin and then etching with phosphoric acid. ii. Chemical adhesion - result of an ion exchange between glass ionomer cement and tooth structure both enamel and dentine 42
- 43. Biomimetic Restorative Materials “Imitation of nature” :- should in some way reproduce one or more natural phenomena within a biologic situation, the material will be biocompatible and not be rejected by adjacent vital tissues Glass ionomer cement Other materials - Resin – based composite. A layered combination of resin – based composites and GICs applied with a technique called lamination. 43
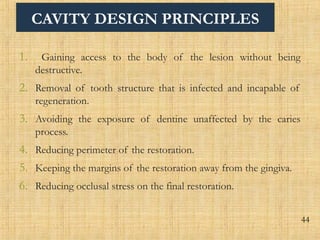
- 44. CAVITY DESIGN PRINCIPLES 1. Gaining access to the body of the lesion without being destructive. 2. Removal of tooth structure that is infected and incapable of regeneration. 3. Avoiding the exposure of dentine unaffected by the caries process. 4. Reducing perimeter of the restoration. 5. Keeping the margins of the restoration away from the gingiva. 6. Reducing occlusal stress on the final restoration. 44
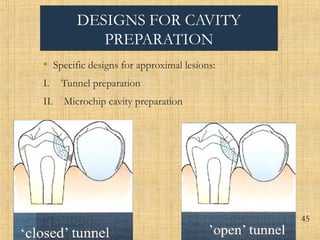
- 45. DESIGNS FOR CAVITY PREPARATION • Specific designs for approximal lesions: I. Tunnel preparation II. Microchip cavity preparation . 45 45
- 46. DESIGNS FOR CAVITY PREPARATION III. Minibox cavity preparation IV. Full box cavity preparation. 46
- 47. MINIMALLY INVASIVE PREPARATION TECHNIQUES • Atraumatic restorative treatment (ART) • High / Low speed bur • Chemomechanical Caries removal • Air abrasion • Laser • Ozone Technology • Polymer Cutting Instruments • Silver Diamine Fluoride (AG (NH3)2F) 47
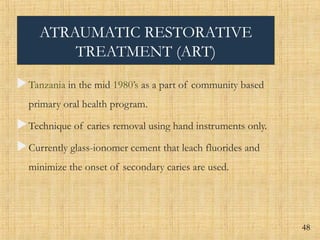
- 48. ATRAUMATIC RESTORATIVE TREATMENT (ART) Tanzania in the mid 1980’s as a part of community based primary oral health program. Technique of caries removal using hand instruments only. Currently glass-ionomer cement that leach fluorides and minimize the onset of secondary caries are used. 48
- 49. 49
- 50. 50
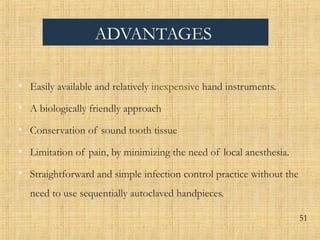
- 51. ADVANTAGES • Easily available and relatively inexpensive hand instruments. • A biologically friendly approach • Conservation of sound tooth tissue • Limitation of pain, by minimizing the need of local anesthesia. • Straightforward and simple infection control practice without the need to use sequentially autoclaved handpieces. 51
- 52. • Chemical adhesion of GIC. • Leaching of fluoride from GIC. • Ease of repairing defects in restoration • Low cost • Non-threatening oral procedure. • No noise from a drill. • Greatest advantage of ART is that it makes possible to reach people who otherwise never would have received any oral care. 52
- 53. LIMITATIONS • Its use is limited to small and medium sized one surface lesions because of low wear resistance and strength of GIC. • Hand fatigue from the use of hand instruments over long periods • Hand mixing might produce a relatively unstandardized mix of GIC 53
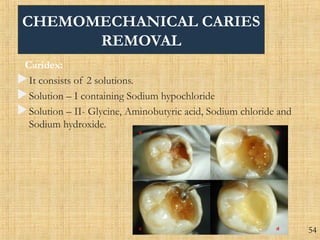
- 54. CHEMOMECHANICAL CARIES REMOVAL Caridex: It consists of 2 solutions. Solution – I containing Sodium hypochloride Solution – II- Glycine, Aminobutyric acid, Sodium chloride and Sodium hydroxide. 54
- 55. ADVANTAGES Reduced need for local anaesthesia Conservation of sound tooth structure Reduced risk of pulpal exposure Well suited for anxious and medically compromised patients as well as for the child patients. LIMITATIONS: Large volumes of solution were needed and the procedure was slow (10-15 minutes) 55
- 56. CARISOLV • It is in the form of Pink gel which can be applied to the carious lesion with specially designated hand instruments. • It is marketed in 2 syringes, • 1.Sodium hypochloride • 2.pink viscous gel which contains aminoacids lysine, leucine, glutamic acid togetherwith CMC (Carboxymethyl cellulose) to make it viscous and is readily visible in use. 56 Mediteam in Sweden , January, 1998
- 57. ADVANTAGES: The system is much easier to use than Caridex As it involves gel rather than liquid there is better contact with the carious lesion. When complete caries removal is achieved by this technique the cavity surface has been shown to be as sound as that remaining after conventional drilling. LIMITATIONS: Rotary and hand instruments may still be needed for removal of tissue or material other than degraded dentine collagen. 57
- 58. ENZYMES • (Goldsberg and Keil, 1989) successfully removed soft carious dentine using bacterial Achromobacter Collagenase, which did not affect the sound dentin layer beneath the lesion. • Enzyme pronase, a non-specific proteolytic enzyme originating from Streptomyces griseus to help remove carious dentine. 58
- 59. SILVER DIAMINE FLUORIDE Ag+ (Silver ions) plus Protein (Bacterial proteins and proteins from infected carious dentine) leading to instant coagulation and form Silver protein Bacterial enzymes (Trypsin, Collagenase), consisting of proteins, are inhibited, thus further denaturation of dentine collagen is prevented Stops degeneration of affected into infected dentine Fluoride assists in the remineralisation of affected dentine 59
- 60. AIR ABRASION • Dr.Robert Black , 1950’s introduced • Dr. J. Tim Rainey was able to improve and combine this technology with the use of modern adhesive restorative material. • Air abrasion devices include cart, table top and handheld models. • Operator controls are either mechanical or digital. 60
- 61. • Some systems (e.g. AIR – FLOW Prep K1) capture the Al2O3 powder stream in H2O spray to reduce the pollution which increases comfort of operation. • When highly energized abrasive particles are directed at healthy enamel and dentin the kinetic energy is absorbed by the substrate and cuts or abrades rapidly. • kinetic cavity preparation. 61
- 62. ADVANTAGES OF AIR – ABRASION Non – traumatic treatment No chipping and micro fracturing Decreased thermal build up Less invasive procedure that preserves more natural tooth structure. 62
- 63. DISADVANTAGES Non-contact based modality, leading to significant risk of cavity over preparation and inadequate carious dentin removal. Spread of aluminum oxide powder particles around the dental operatory. Impaired indirect view because abrasive particles collect on mirror rapidly blocking the viewing surfaces. 63
- 64. SONO ABRASION Recent advances have demonstrated the use of high speed ultrasonic's with abrasive tips for the purpose of cavity preparation High frequency sonic air scaler, modified abrasive tips Oscillate in sonic region of 6.5 kHz Air cooled with water: 20-30 mL/min 64
- 65. LASERS Maiman in 1960. • Lasers are devices that produce beams of Coherent and very high intensity light. Lasers are used in the treatment of soft tissues and modification of hard tooth structures. 65
- 66. Lasers that are currently being investigated for more selective hard tissue ablation include • Er : YAG and Nd : YAG. • CO2 lasers. • Excimer lasers with U.V. emission. • Holmium lasers • Dye enhanced laser ablation. 66
- 67. ADVANTAGES • Laser radiation has proved to be a safe and effective treatment modality for caries removal and cavity preparation, and the reduced need for anesthesia is considered an advantage. LIMITATIONS • Expensive • Huge size of the equipment 67
- 68. OZONE TECHNOLOGY • Ozone (O3) is an energized form of oxygen. • It is now a proven fact that 10 seconds application of ozone gas at a concentration of 2200ppm could eliminate 99% of the carious micro flora. • For the therapeutic purposes, ozone can be produced in a controlled manner using electrical units. 68
- 69. 69
- 70. Indications • Primary pit and fissure caries • To treat primary root carious lesions • Early carious lesions around crowns and bridges Advantages • Ozone therapy kills more than 99% of microorganisms in caries. • It oxidizes caries and speeds up remineralization • Ozone does not cause allergic reaction. • Microorganisms do not develop resistance to ozone. 70
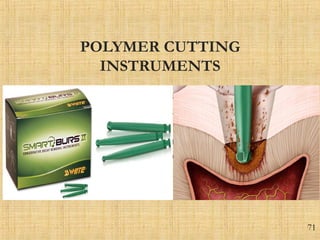
- 71. POLYMER CUTTING INSTRUMENTS • Metal and diamond burs cut decayed and healthy dentin indiscriminately. Innovative polymer instruments have been designed to differentiate between these two structures, they are able to remove softened dentin, but cannot cut hard, healthy dentin. 71
- 72. CONCLUSION • The 21st century of dentistry surely belongs to the 'preventive' paradigm. Minimal intervention approach accompanies up-to-date caries diagnosis and risk assessment before arriving at a treatment decision. • The minimal intervention philosophy could be fruitfully incorporated into contemporary preventive and public health dentistry. • we should be engaged in treating 'CARIES' and not the 'CAVITY' anymore. 72
- 73. REFERENCES Norman o harris. preventive dentistry 2009 Joel M. White, M.S, W. Stephan Eakle. Rationale and treatment approach in minimally invasive dentistry. JADA, Vol. 131, June 2000. Pg: 13S-19S. FDI Policy Statement. Minimal Intervention in the Management of Dental Caries. Adopted by the FDI General Assembly: 1 October 2002 – Vienna, Austria Mount GJ. Minimal Intervention: A new concept for operative dentistry. Quintessence Int 2000:31:527-533 Bennett T. Amaechi. Emerging technologies for diagnosis of dental caries: The road so far. JOURNAL OF APPLIED PHYSICS 105, 102047 ; 2009. 73
- 74. M. Ganesh and Dhaval Parikh. Chemomechanical caries removal (CMCR) agents: Review and clinical application in primary teeth. Journal of Dentistry and Oral Hygiene 2011; 3(3);34-45. Pitts NB. Diagnostic methods for caries: what is appropriate when? J Dent 1991 Dec; 19(6):377-82. Vivek S Hegde, Roheet A Khatavkar. A new dimension to conservative dentistry. Air Abrasion. J Conserv Dent 2010: 13(1); 4-8. Sumita Bhagwat, Deepil Mehta Bur ….no more. Non rotary methods of cavity preparation. Scientific Journal Vol. II – 2008 Iain A. Pretty. Review Caries detection and diagnosis: Novel technologies. Journal of dentistry 34 (2006) 727 – 739. 74
- 75. • LJ Walsh. The current status of laser applications in dentistry. Australian Dental Journal 2003; 48 :( 3):146-155. • www.midentistry .com • Banerjee A, Watson TF, Kidd EA. Dentine caries excavation: a review of current clinical techniques. Br Dent J 2000 May 13; 188(9):476-82. • Beeley JA, Yip HK. Stevenson AG. Chemochemical caries removal: a review of the techniques and latest developments. Br Dent J. 2000 Apr 22; 188(8):427-30. • Harshpriya et al, recent trends in preventive dentistry-A review; SRM University dental journal, 2011;2(3):232-237 75
- 76. THANK YOU 76