Adme
- 2. What Is pharmacokinetic? introduction How the human body act on the drugs? Pharmacokinetics is the quantitative study of drug movement in, through and out of the body. Intensity of effect is related to concentration of the drug at the site of action, which depends on its pharmacokinetic properties. Pharmacokinetic properties of particular drug is important to determine dose, the route of administration ,onset of action, peak action time, duration of action and frequency of dosing.
- 3. Pharmacokinetics has four component:- ABSORPTION 01 DISTRIBUTION02 METABOLISM 03 EXCRETION04
- 4. ABSORPTION • Absorption is the transfer of a drug from its site of administration to the blood stream . • Most of drugs are absorbed by the way of passive transport. • Intravenous administration has no absorption. • Fraction of administered dose and rate of absorption are important.
- 6. bioavailability • Bioavailability refers to the rate and extent of absorption of a drug. It is a measure of the fraction (F) of administered dose of a drug that reaches the systemic circulation in the unchanged form. • Bioavailability of drug injected i.v. is 100%, but is frequently lower after oral ingestion, because: - The drug may be incompletely absorbed -The absorbed drug may undergo first pass metabolism in intestinal wall and/or liver or be excreted in bile.
- 8. DISTRIBUTION • It is the passage of drug from the circulation to the tissue and site of its action. •The extent of distribution of drug depends on its lipid solubility, ionization at physiological pH (dependent on pKa), extent of binding to plasma and tissue proteins and differences in regional blood flow, disease like CHF, uremia, cirrhosis •Movement of drug - until equilibration between unbound drug in plasma and tissue fluids
- 9. Definition: Apparent Volume of distribution is defined as the volume that would accommodate all the drugs in the body, if the concentration was the same as in plasma. Expressed as: in Liters V = Dose administered IV/ Plasma concentration Total drug in body=1000mg Plasma drug concentration= 50mg/ml V=1000/50=20L Volume of Distribution (V)
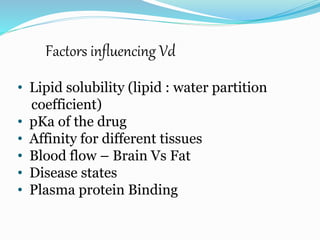
- 10. Factors influencing Vd • Lipid solubility (lipid : water partition coefficient) • pKa of the drug • Affinity for different tissues • Blood flow – Brain Vs Fat • Disease states • Plasma protein Binding
- 12. Brain and CSF Penetration Blood brain barrier (BBB): includes the capillary endothelial cells (which have tight junctions and lack large intracellular pores) and an investment of glial tissue, over the capillaries. A similar barrier is located in the choroid plexus. BBB is lipoidal and limits the entry of non-lipid soluble drugs (amikacin, gentamicin, neostigmine etc.). (Only lipid soluble unionized drugs penetrate and have action on the CNS)
- 13. METABOLISM Chemical alteration of the drug in the body . Aim: to convert non-polar lipid soluble compounds to polar lipid insoluble compounds to avoid reabsorption in renal tubules . Most hydrophilic drugs are less biotransformed and excreted unchanged – streptomycin, neostigmine and pancuronium etc. Biotransformation is required for protection of body from toxic metabolites
- 14. Results of Biotransformation Active drug and its metabolite to inactive metabolites – most drugs (ibuprofen, paracetamol, chlormphenicol etc.) Active drug to active product (phenacetin – acetminophen or paracetamol, morphine to Morphine-6-glucoronide, digitoxin to digoxin etc.) Inactive drug to active/enhanced activity (prodrug) – levodopa - carbidopa, prednisone – prednisolone and enlpril – enlprilat) . No toxic or less toxic drug to toxic metabolites (Isonizide to Acetyl isoniazide)
- 15. Phase- 1 phase -2 Phases of metabolism 01 Phase1 or non systemic metabolite may be active or inactive . 02 Phase2 or systemic metabolites are inactive
- 16. Phase -1 It includes oxidative ,reductive and hydrolytic biotransformation. The main purpose of it, to introduce a functional group into xenobiotic molecule to produce more water soluble compound. They do not sufficientlyproduce inactive metabolites but mainely tend to provide functional groups that can go to phase-2 reactions.
- 17. A. Reductive reaction 01 B. Hydrolytic reaction 02 C. Oxidative reaction 03 Types of phase-1 reaction
- 18. PAHASE-2 These are true detoxification reaction and are also known as conjugational reactions. It involves covalent attachment of small polar endogenous molecule such as sulfate, glycine etc to either unchanged drug or phase-1 product having suitable functional groups resulting in formation of highly water soluble conjugate tha are excreted by kidney. Enzymes involved in these reaction is tansferase which is mainly found in liver.
- 19. Glucuronic acid conjugation Sulfate conjugation Conjugation with glycine,glutamine and other amino acid ACETYLATION METHYLATION Glutathione or mercaptopuric acid conjugation
- 20. Factors affecting Biotransformation Concurrent use of drugs: Induction and inhibition. Genetic polymorphism. Pollutant exposure from environment or industry. Pathological status. Age
- 21. EXCRETION Excretion is a transport procedure which the prototype drug (or parent drug) or other metabolic products are excreted through excretion organ or secretion organ. Hydrophilic compounds can be easily excreted. Routes of drug excretion -: -Kidney -Biliary excretion - Sweat and saliva -Milk -Pulmonary
- 22. Hepatic Excretion Drugs can be excreted in bile, especially when the are conjugated with – glucuronic Acid Drug is absorbed → glucuronidated or sulfatated in the liver and secreted through the bile → glucuronic acid/sulfate is cleaved off by bacteria in GI tract → drug is reabsorbed (steroid hormones, rifampicin, amoxycillin, contraceptives) Anthraquinone, heavy metals – directly excreted in colon