Hyponatremia
- 1. HYPONATREMIA
- 2. Hyponatremia is a serum sodium level below 135 mEq/L ETIOLOGY:- - Decreased total body water (dehydration) - Syndrome of inappropriate antidiuretic hormone. It may follow many forms of drug therapy e.g:- Chemotherapy, phenothiazines, morphine and barbiturates. - Inability of kidney to excrete sufficiently diluted urine.
- 3. - Hypovolemic hyponatremia:- Renal loss of sodium from diuretic use, daibetic glycosuria, aldosterone deficiency, intrinsic renal disease. External loss of sodium from vomitting, diarrhea, increased sweating, burns. - Euvolemic hyponatremia:- Sodium deficit result from syndrome of inappropriate antidiuretic hormone or the continuous secretion of antidiuretic hormone due to pain, emotions, medication.
- 4. - Hypovolemic hyponatremia:- Edematous disorders resulting in sodium deficits, congestive heart failure, cirrhosis of liver, nephrotic syndrome, acute and chronic renal failure. - Redistributive hyponatremia:- Pseudohyponatremia, hyperglycemia, hyperlipidemia. RISK FACTORS:- - Elderly, infants and small children - Vomitting, diarrhea, cardiac or renal disorders
- 5. - Addison’s disease - Patients on NPO and recieving IV infusion - Patients on potent diuretics without sodium replacement - Excessive perspiration - Less fluid intake. - Athletes and outdoor laborers.
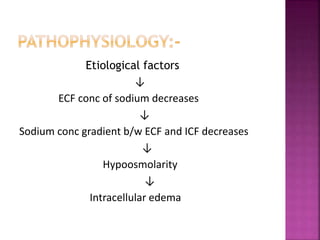
- 6. Etiological factors ↓ ECF conc of sodium decreases ↓ Sodium conc gradient b/w ECF and ICF decreases ↓ Hypoosmolarity ↓ Intracellular edema
- 7. ↓ (Osmosis) ↓ Water moves into cells ↓ Delayed membrane repolarisation ↓ Cerebral edema Uncorrected hypovolemic hyponatremia may result in shock from continued ECF volume loss.
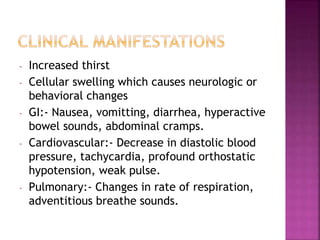
- 8. - Increased thirst - Cellular swelling which causes neurologic or behavioral changes - GI:- Nausea, vomitting, diarrhea, hyperactive bowel sounds, abdominal cramps. - Cardiovascular:- Decrease in diastolic blood pressure, tachycardia, profound orthostatic hypotension, weak pulse. - Pulmonary:- Changes in rate of respiration, adventitious breathe sounds.
- 9. - Neurologic:- Headache, apprehension, lethargy, confusion, slowed problem solving flat affect, dimnished muscle tone in extremities, decreased deep tendon reflexes, weakness and tremor. - Integumentary:- Dry skin, pale, dry mucus membranes. LABORATORY FINDINGS:- - Serum sodium<135mEq/L - Urine sodium<40mEq/L - Serum osmolarity<275mOsm/Kg
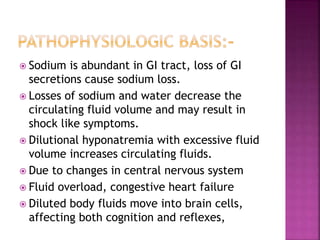
- 10. Sodium is abundant in GI tract, loss of GI secretions cause sodium loss. Losses of sodium and water decrease the circulating fluid volume and may result in shock like symptoms. Dilutional hyponatremia with excessive fluid volume increases circulating fluids. Due to changes in central nervous system Fluid overload, congestive heart failure Diluted body fluids move into brain cells, affecting both cognition and reflexes,
- 11. excitable membranes are less responsive to stimuli. - Decreased interstitial fluids - Results in hyonatremia, symptoms become apparent when the serum sodium is<125 mEq/L. - Body sodium losses result in decreased concentration of sodium in body fluids. MEDICAL MANAGEMENT:- Intake of fluids will be restricted to allow the sodium to regain balance.
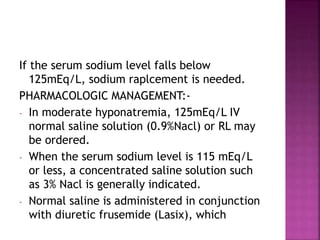
- 12. If the serum sodium level falls below 125mEq/L, sodium raplcement is needed. PHARMACOLOGIC MANAGEMENT:- - In moderate hyponatremia, 125mEq/L IV normal saline solution (0.9%Nacl) or RL may be ordered. - When the serum sodium level is 115 mEq/L or less, a concentrated saline solution such as 3% Nacl is generally indicated. - Normal saline is administered in conjunction with diuretic frusemide (Lasix), which
- 13. Increases urinary sodium loss and therefore reduces the risk of ECF volume expansion. Moreover, the urine excreted through frusemide induced diuresis has much less sodium than does the ECF, which raises serum sodium level. Drug therapy for hyponatremia from SIADH includes agents that antagonise ADH, such as demeclocycline and lithium. DIETARY MANAGEMENT:- Foods high in sodium are recommended. Grains, cheeses, meats.
- 14. Nsg dsis:- Hyponatremia r/t vomitting, diarrhea, gastric suctioning, burns, SIADH or surgery. Expected outcomes:- The nurse will monitor the client for sodium levels to return to 135mEq/l or above, the reduction of factors contributing to hyponatremia, fluid and electrolyte losses and replacement and symptoms of fluid and sodium imbalance. Implementation:- - Check v/s every 4-8 hrs.
- 15. - Monitor serum sodium and osmolality levels. (Serum sodium less than 125mEq/L indicates need for prompt medical care). - Fluid intake whether oral or IV should include sodium. If the patient is recieving 3% saline solution IV, the nurse observes s/s of hypervolemia eg- dyspnea, chest crackles and neck vein engorgement. - The nurse should irrigate NG tubes and wound sites with normal saline solution to prevent further sodium losses.
- 16. - Closely monitor intake and output. - Raise side rails and keep bed in low position when nurse is not providing direct care. - As seizures may develop the patient should be protected from injury during seizure and airway should be maintained.
- 17. THANK YOU