Planning & orag.imaging services
- 1. PLANNING AND ORGANIZATION OF RADIOLOGY DEPARTMENT DR.N.C.DAS
- 2. GROWTH OF RADIOLOGY Several accidental coincidences lead to the discovery of X- rays by Wilhelm Conrad Roentgen in the year 1895. Since then a long-long way has been covered in this field. No medical science has seen such raid change as Radiology, especially in the past few decades. At the same time, No medical science has met the challenge as Radiology to move forward in an era of rapid change in medical technology.
- 3. PLANNING AND ORGANIZATION With rapid change in investigation technology, there is a continuous changing demand in the field of radio diagnosis and imaging service. Resulting in an advanced, and detailed systematic planning and organizing Having a foresight into future developments and requirements.
- 4. OBJECTIVE OF THE DEPARTMENT To provide comprehension high quality imaging service Establishment and confirmation of clinical diagnosis Providing high quality therapeutic radiology Commitment to training and research
- 5. PLANNING CONSIDERATIONS PLANNING PHYSICAL PLANNING STRATEGIC PLANNING VISIONARY PLANNING Development Planning Staffing Integration with Health Care Services Separate for indoor & out door service Addition of new technology Integration in health system Predict future requirement depending on past utilization Planned infrastructure Anticipate pattern of change Get most out of available space Plan imaging environment Incorporate information system and networking capability
- 6. PLANNING OF PHYSICAL FACILITIES PHYSICAL FACILITY LOCATION ENVIRONMENT ANCILLARY AREA ADMINISTRATIVE AREA FUNCTIONAL AREA SIZE AUXILLARY AREA
- 7. LOCATION Preferably in ground floor Away from main traffic Easy access to OPD, emergency and indoor SIZE Depends on the hospital size Types of services provided No. of machines to be installed ADMINISTRATIVE AREA Patient waiting area, reception Registration Counter Office of HOD Office of Nursing & technical staff Store for supplies Circulation space for movement of patients, staff, trolley and stretcher
- 8. SAFETY CONSIDERATION For Radiation Protection ALARA concept is used (As Low As Reasonably Achievable ) Plan Radio protection prior to construction. Promote awareness among doctors and staff. Awareness among patient and public, Demarcation of restricted areas to prevent radiation hazards like:- i)Acute and Chronic Skin ii)Somatic and Genetic iii)Deterministic (Not depending on does) iv)Stochastic (Depending on does of exposure)
- 9. PLAN RADIATION PROTECTION PROTECTION PATIENT PUBLIC STAFF Optimization of X-ray, CT does Patient Shielding, Thyroid Gonads breasts Minimize area of exposure Periodic quality control and calibration of X-ray machines - Deptt. away from main Traffic Good brick/ concrete wall 1.5 ft thick Lead covering 1.5 mm thick on wall. Hazzards signs & restricted area demarcation Radiation warning board or light in yellow colour Distance between control panel and unit minimum 3 mts. Radio protection aprons, lead gloves and mask. Use of radiation monitoring devices TLD badges/ films
- 10. PROTECTIVE MEASURES FOR RADIATION EMMISION Radiation is an energy emitted in the form of a beam of ‘X- rays which are risk involved to life, health or property when exposures is high. Radiation danger in X-Ray room is sweltered /scattered radiation. Radiation decreases in proportion to square of distance. Distance is important protection in X-Ray room. Metal cones and adjustable shutters are used to prevent sealtered radiation.
- 11. X-RAY ROOMS : Must be large enough for the equipment Should have at least one patient change cubicle accessible from outside the room Must locate the operator’s console where the primary beam will NEVER be directed towards it, but where the patient can be easily observed Must be able to accommodate large beds/trolleys, and any anaesthetic equipment likely to be used Must locate holes in floors for cables away from radiation beams, or be shielded Must have radiation warning signs on all doors Should have radiation warning lights outside for fluoroscopy, angiography and CT
- 12. DARK ROOM SAID TO BE THE LIFELINE OF A RADIOLOGY DEPARTMENT Minimal floor area of 100 sq ft Ceiling 11 ft high Cassette loading area Cassette unloading area Developing and film processing area Water tap Safe light (0 watt,3ft distance,color-red/amber/green) Ventillation, exhaust fan viii)Double door/self closing doors. ix)Pass boxes (light & x-ray proof) x)Walls lined with 1.6 mm lead equivalent. xi)Walls and roof painted black. xii)Floor-chemical/stain resistant. xiii)Equipments (benches, racks, hangers, tanks, immersion heaters) 2.Drying room 3.Record room 4.Patient preparation room 5.Reporting room (Can be modified as per dry film processing unit or digital imaging )
- 13. X-RAY ROOM CONSTRUCTION Shielding of wall of X-Ray room with lead equivalent of 1 mm. Concrete Wall - 8-12 cm thick Brick Wall - 12 to 15 cm thick Two important areas must be looked into Wall behind chest stand Wall of dark room Lead glass window between operator and X-ray tube Distance between X-ray table and control table should be as far as possible between 10 ft to 15ft.
- 14. PRINCIPLE OF MACHINE INSTALLATION X- Ray tube should never point towards the control unit. It should not point towards dark room. It should not point towards, door, window or towards corridor wall. Lead lying up to 4 ½ of wall of patient waiting space.
- 15. REGULATORY BODY Radiation protection rule 1971, under Atomic Energy Act 1962. Safety and protection body of the hospital and atomic energy regulatory board. Bhaba Atomic Research Centre. Disposal of Radio wastes as per norm. Radio monitoring equipments. Film/ TLD badges and monthly monitoring.
- 16. MRI AND C.T. ROOM Patient must not have any metals on body even dental fixtures, pace makers. No metal fixtures in the MRI Room. Non magnetic tables and trolley. Away from public passage, screen between control room and machine.
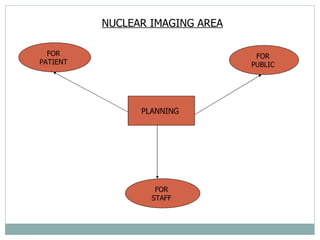
- 17. NUCLEAR IMAGING AREA PLANNING FOR PATIENT FOR PUBLIC FOR STAFF
- 18. HOT AREA - This area include receiving, diluting, holding, counting and issuing of radio isotopes. Floor and work surface should be non- porus All work to be done in glove box or under hood box Radio active level needs to be monitored Inter locking lead brick Lead gloves to be used while handling Separate toilet for radio active used patients
- 19. DIAGNOSTIC AREA All walls and doors to be painted with good quality washable paints. A portable contamination monitor with aural alarms to be used. Minimum furniture to be kept Adequate number of lead containers and inter looking lead bricks to be used. Ventilation fume hoods to be provided Drainage pipe should be directly connected to swearage SUPPORTING AREA Waiting area away from circulatory corridor Toilets separate for radio active and non radio active patients.
- 20. ELECTRICAL SUPPLY 3Phase electric supply Separate connections from main Generators/backup facilities-CPU WATER SUPPLY-continuous with heating equipments
- 21. FUNCTIONAL AREA The functional area have installation of all machines like MACHINES X-RAY MACHINES 5.8 mt x 3.3 mt ht ULTRA SOUND 25 sq mt CT SCAN 110-120 sq mt COLOR DOPPLER OPG MACHINE DARK ROOM MRI 125-130 sq mt MAMOGRAPHY 15-20 sq mt
- 22. AUXILLARY AREA AREAS PREPARATION ROOM JANITORS ROOM PATIENT TOILET PATIENT CHANGING ROOM DRYING ROOM PATIENT REST ROOM REPORTING DESK RECORD ROOM
- 23. ANCILLARY AREA ANCILLARY AREA CONSULTANT ROOM STAFF CHANGING ROOM TOILETS OLD RECORD & X-RAY ROOM LIBRARY SEMINAR ROOM ENVIRONMENT There should be public address system Back up electricity supply Proper ventilation and air change Air conditioning of machine rooms
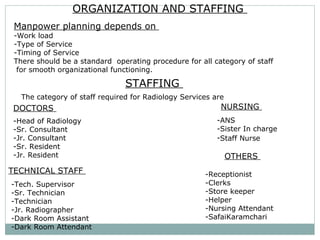
- 24. ORGANIZATION AND STAFFING Manpower planning depends on Work load Type of Service Timing of Service There should be a standard operating procedure for all category of staff for smooth organizational functioning. STAFFING The category of staff required for Radiology Services are DOCTORS Head of Radiology Sr. Consultant Jr. Consultant Sr. Resident Jr. Resident TECHNICAL STAFF Tech. Supervisor Sr. Technician Technician Jr. Radiographer Dark Room Assistant Dark Room Attendant NURSING ANS Sister In charge Staff Nurse OTHERS Receptionist Clerks Store keeper Helper Nursing Attendant SafaiKaramchari
- 25. ORGANOGRAM MEDICAL SUPERINTENDENT HOD (RADIOLOGY) ADMN. OFFICE OF HOD UDC/PA REGISTRATION CERK RECORD CLERK STORE KEEPER CLINICAL HEAD X-RAY UNIT TECH. ASSTT. DARK ROOM ASSITT. GROUP ‘D’ ATTENDANT HEAD CTVS TECH. STAFF NURSING STAFF GROUP ‘D’ HEAD MRI TECH. STAFF NURSING STAFF GROUP ‘D’ HEAD RADIOTHERAPY TECH. STAFF NURSING STAFF GROUP ‘D’ HEAD NUCLEARMED TECH. STAFF GROUP ‘D’ HEAD NURSING SISTER I/C STAFF NURSE GROUP ‘D’
- 26. EQUIPMENTS Procurement Installation Maintenance PROCUREMENT - All the equipments in the radiology department are technically very advance, sophisticated, sensitive and expensive but critical to patient care. -Hence a detail specification be made prior to purchase and installation . INSTALLATION Before installation the structure of the building and environmental aspect to be looked into. The images are obtained either by transmission of rays or emission of does of radio isotopes through the organ to be viewed, which reflects gamma rays picked by camera.
- 27. The various equipments in use are- X- ray Machines Ultrasound Machine Doppler Machine Computer assisted Tomography (CAT Scan) Magnetic Resources Imaging (MRI) Position Emission Tomography (PET) Mammography Nuclear Imaging System ACCESSORIES Cassettes X-ray, CT, MRI films Dyes, Apron, Gloves Hangers, Clips etc
- 28. FLUROSCOPY ULTRA SOUND MAMO GRAPHY CT_ SCAN MRI BONE DENSITO METER
- 29. EQUIPMENTS MAINTENANCE Daily Maintenance - Tech. staff Preventive Maintenance (AMC) Supplier Comprehensive Maintenance (CMC) Warranty and Guarantee Breakdown Maintenance Emergency Maintenance Maintenance helps in:- Reduction in down time Safety of equipment and man Credible cost effective service Increase equipment life
- 30. MANAGERIAL ISSUES (CONCEPT) Application of managerial tools to ensure effective and efficient running or functioning of the department. The concept of management is P – Planning - Infrastructure, manpower, equipments O – Organizing - Organ hierarchy, manpower, job responsibility L - Leading - Standard Operating Procedure I - Integrating - With other health care services C - Controlling - Maintenance, staff discipline, pilferage E - Evaluation - Level of staff and patient satisfaction and change in policy required.
- 31. MANAGEMENT ISSUES INPUT PROCESS OUTPUT ISSUES AT INPUT Registration Timing Any restriction in number Prior appointment Reception and information PROCESS Ensure trained manpower at machines Ensure functional status Correction of processing status Ensure part to be exposed Prevent mal practices and pilferage Training of staff Follow safety protocol for patient and staff Developing solutions & cassettes OUTPUT Quality of films Correct reporting, misinterpretation of report. Matching number in film and record Level of patient satisfaction The ultimate aim of any service is to achieve its desired objective with full satisfaction of both consumer and provider.
- 32. TYPES OF RADIATION HAZZARD ACUTE & SKIN REACTION HAZZARD SOMATIC & GENETIC DETERMINISTIC (Regular dose) STOCHASTIC (High dose)
- 33. RADIATION HAZARDS ACUTE EFFECT – Heavy dose in short period of time Cerebral-convulsions, blurring, headache Gastric-nausea, vomiting, colicky abdominal pain Blood- a plastic anemia, blood dyscrasias, marrow depression 2. CHRONIC EFFECT – Due to continuous short exposure Skin-loss of hair, burns, brittle nails, amputation fingers. Blood-anemia, leukemia, leucopenia. Eye-cataract, irido cyclitis. Others-Sterility, obesity, cancer.
- 34. RADIO PROTECTION PROTECTION FOR PATIENT FOR STAFF FOR PUBLIC
- 35. FOR PATIENT: Optimization of X-Ray/ CT dose. Shielding of patient parts (thyroid, breast, gonads) Lead aprons, gloves and goggles to be used while handling and positioning Unnecessary exposure to be avoided Periodic quality control and calibration of machines
- 36. FOR PUBLIC: Away from general traffic 4 ½ ft high lead covering of 10 mm thick on wall Warning board to be used (Restricted area) Yellow glow signs for radiation area
- 37. FOR STAFF: Adequate distance (3 mt) between machine and control panel Lead apron lead equivalent of 0.5 mm thick Gloves and goggles while positioning the patient Film/ TLD badges to be used Monitoring of radiation exposure every month
- 38. NEW DEVELOPMENTS 1.Picture archiving and Communication System A. More than 15years ago, the idea of Picture archiving and Communication System and a filmless Radiology department was conceived. B. In PACS, the images are acquired, read, communicated and stored digitally. C. HIS: PACS gets incorporated in HIS (Hospital Information system) so that other departments can access the images sitting in their work place. D. Computers or networks dedicated to : Storage Retrieval Distribution Presentation of images. E. Images are stored in an independent format. The most common format for image storage is DICOM (Digital Imaging and Communications in Medicine) .
- 39. NEW DEVELOPMENTS TELE RADIOLOGY 1. Hospitals like Narayan Hridayalay have managed to reach out to the remotest villages of Karnataka and Maharashtra through telemedicine and tele radiology. 2. Infact,a radiologist sitting in any part of the world can access the images of a patient in any other part of the world through PACS. 3. Implementation of PACS in a Radiology Department is not far away. 4. Era of Tele radiology is fast approaching.!
- 40. HOSPITAL ADMINISTRATION MADE EASY http//hospiad.blogspot.com An effort solely to help students and aspirants in their attempt to become a successful Hospital Administrator. hospi ad DR. N. C. DAS