Immunity. Basic princeples of humoral and cellular immune response.
- 1. Basic principles of humoral and cellular immune reaction Irene Tereshchenko 2nd Medical Faculty Charles University in Prague
- 2. Immunity Immunity is the ability of human body to resist almost all kinds of organisms and toxins that tends to damage the tissues and organs. → Fungi, Protozoans, Bacteria and viruses are all potential pathogens. Immune Response - reaction of the cells and fluids of the body to the presence of a substance which is not recognized as a constituent of the body itself.
- 3. 1. Pre-immune mechanisms Ag penetrates tissues (vasodilatation, edema) Adsorption of the Ag to immune tissue 2. Immune mechanisms migration of APCs in T-or B-zone peripheral organs of the immune system Processing of Ag: Stage 1 – Endocytosis of Ag Stage 2 - cleavage (processing) Stage 3 - expression of degraded particles Ag at the MTC in complex with MHC I or MHC II Stage 4 – presenting to TH 3. Suppression of the immune response (Autoimmune diseases can run) 4. Immunological memory Mechanism of IR
- 4. Goal: to stop pathogens from entering the body → Skin – acts as a barrier to invasion → Sweat – has chemicals which can kill different pathogens. → Tears - have lysozyme which has powerful digestive abilities that render antigens harmless. → Saliva – also has lysozyme. → Mucus - can trap pathogens, which are then sneezed, coughed, washed away, or destroyed by chemicals. → Stomach Acid – destroys pathogens First line of defense
- 5. If a pathogen is able to get past the body's first line of defense, and an infection starts, the body can rely on it's second line of defense. → First there is a non-specific response (phagocytosis) followed by an INFLAMMATORY RESPONSE. Second line of defense Phagocytosis = ingestion + digestion of pathogens.
- 6. →Cell-mediated immunity is a type of immunity when body develops large number of lymphocytes which are specifically activated against foreign agent. →These activated or sensitized lymphocytes have the ability to attach to a foreign agent and to destroy it. →CI is composed of sensitized T-lymphocytes. Cellular Immunity
- 7. →In process of developing of CI phagocytic cells involved in the expulsion of pathogens from the intercellular space. →Phagocytic cells attack pathogens and destroy them. On intracellular level macrophages are the main cell protectors which have specific receptors - Ig, through which they effect on the pathogen. →Its aim is to combine phagocytosis and specific antibodies to fight pathogenic environment. Cellular Immunity
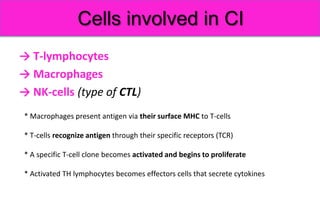
- 8. → T-lymphocytes → Macrophages → NK-cells (type of CTL) Cells involved in CI * Macrophages present antigen via their surface MHC to T-cells * T-cells recognize antigen through their specific receptors (TCR) * A specific T-cell clone becomes activated and begins to proliferate * Activated TH lymphocytes becomes effectors cells that secrete cytokines
- 9. → Protein Pathogen processed and converted into peptide to bind a MHC molecules on APC to be presented on T-cell AG Processing and presentation
- 10. → TH-cells express IL-2 receptors and secrete cytokines including IL-2 → IL-2 auto activate TH-cells → APC release IL-I which acts on both APC and TH-cell to promote their activation → All mentioned interactions lead to activation of mature TH-cells → Mature TH-cells proliferate and differentiate into effectors antigen specific TH-cells releasing cytokines → Some of them become memory cells which provide secondary immune response → Cytokine released from activated TH-cells activate macrophages, NK and B- cells T-cells activation
- 11. → Activated CD8 TC-cells proliferate and differentiate into a clone of effectors cells CTLs → Effectors CTLs kill target cells i.e. nucleated cells (expressing MHC-I) infected with viruses, tumor cells or graft cells T-cells activation
- 12. → Activated TH-cells (TH1) secrete IFN-γ which activates macrophages and increase their ability to kill ingested intracellular pathogens → The process of activation of macrophages, NK cell and cytotoxic T-cells, infiltration and proliferation of inflammatory cells, stimulated by cytokines released from TH-cells (TH1) is important protective mechanism against intracellular pathogen Macrophage activation
- 13. Cytokines stimulate other effectors cells of CMI and humoral immune response and mediate the following: 1. Attract monocytes, macrophages and lymphocytes to the site 2. Activate macrophages to kill intracellular microbes 3. Promote activity of CD8 CTLs which directly kill virus infected cells, tumour cells, and graft rejection 4. They activate NK cells increasing their cytotoxic functions 5. Stimulate B-cells to differentiate into plasma cells that secret antibodies
- 14. Sometimes the second line of defense is still not enough and the pathogen is then heading for the body's last line of defense. The immune system recognizes, attacks, destroys, and remembers each pathogen that enters the body. It does this by making specialized cells and antibodies that render the pathogens harmless. For each type of pathogen, the immune system produces cells that are specific for that particular pathogen. Third line of defense
- 15. →The humoral response is carried out by antibodies which are produced by Plasma cells. →Plasma cells are derived from activated B-cells that are produced in the bone marrow. →Humoral immunity promotes the development of normal operation antibodies. →The aim of bacteria and viruses (pathogens) – is to enter the cell to destroy it →The principle of action of antibodies is the interruption of receptor linkages between the pathogen and the cell. →The result is to breakdown of interaction between pathogen and cells due to blocking it by the effector molecule or antibody. Humoral Immunity
- 16. Antibodies An antibody (Ab) is a protein produced by B cells that is used by the immune system to identify and neutralize foreign objects such as bacteria and viruses. → Agglutination: Enhances phagocytosis and reduces number of infectious units to be dealt with → Opsonization: Coating antigen with antibody enhances phagocytosis → Neutralization: blocks adhesion of bacteria and viruses to mucosa. Also blocks active site of toxin → Activation of complement → Inflammation: Disruption of cells by complement/C-reactive protein attracts phagocytic and other defensive immune system cells → AB-dependent cell-mediated cytotoxicity: Ab attached to target cells cause destruction by non-specific immune cells
- 18. Immunoglobins Monomer → The most common, represents 75-80% of serum Ig. → The only antibody capable of crossing the placenta to give passive immunity to the fetus. → Has longest half-life (23 days) among of all Igs. → Activates complement → Stimulates chemotaxis → Antigen receptor on surface B cells (together with IgM). → Activate basophils and mast cells to produce antimicrobial factors. → Bound to surface of mast cells and basophils → Destroys parasitic worms and participates in allergies IgG IgD IgE SS-bond
- 19. → Present in body secretions → Provides protection against proliferation of microorganisms in this fluid → Aids in defense against microbes and foreign molecules penetrating body via cell linings of these cavities. → Provides passive immunity to infants through mothers breast milk Dimer (trimer) IgA Immunoglobins
- 20. Immunoglobins Pentamer → First Ig class produced in a primary response to an Ag → Found on surface on B cells (together with IgD) → Ag receptor of B cells → Has 10 antigen-binding sites → More effective at stimulating complement →The FC receptors on phagocytes bind IgM (opsonization) IgM
- 21. Interferons (IFNs) are proteins made and released by host cells in response to the presence of pathogens such as viruses, bacteria, parasites or tumor cells. They allow for communication between cells to trigger the protective defenses of the immune system that eradicate pathogens or tumors. ϒ-IFNs are produced by NK cells that activate macrophages (Type II IFNs) NK cells ϒ-IFNs Macrophage activation Whereas, α and β IFNs are produced by virus infected cells that activate NK cells. (Type I IFNs) Virus infected cells α, β IFNs NK cell activation Interferons
- 22. → The complement system helps the ability of Ab and phagocytic cells to clear pathogens from an organism. → It is part of the innate immune system (not adaptable, doesn’t changes during lifetime). → The complement system consists of a number of small proteins found in the blood, in general synthesized by the liver, and normally circulating as inactive precursors (pro-proteins). When stimulated by one of several triggers, proteases in the system cleave specific proteins to release cytokines and initiate an amplifying cascade of further cleavages. Complement system
- 23. → The Microbial antigen is ingested by an APC and partially digested. → Fragments from microbe bind with the MHC II to form a MHC II /Ag complex on the surface of the APC Humoral Immunity
- 24. → TH-cell, specific for the presented antigen, binds to the MHC II/Ag complex Humoral Immunity
- 25. → TH-cell then activates an appropriate B cell by releasing IL-2 to it. Humoral Immunity *IL-2 – growth factor for T and B cells
- 26. → The interaction between the TH-cell and the B-cell causes the B- cell to differentiate into Plasma cells and memory cells. Humoral Immunity
- 27. Memory Cells Memory T Cell → an infection fighting cell Memory B cell → an antibody producing cell Memory cells do not react right away but are held in reserve for later infections. The secondary response that is carried out by memory cells is different in 3 ways. → Memory cells produce antibodies that bind with greater affinity to their antigens than the antibodies produced in the initial response. → The response time is much vaster than the primary response → A greater number of antibodies are produced.
- 28. Lymphicytos – organism fighting infection G-вирус М-бактерия A-бактерия Proteins CD4 CD8 indexes shows the condition of CI State of secondary immunodeficiency Rheumatic process 17.12.2013
- 29. 25.02.2014