Vinter o&p2013
- 1. Christina Vinter MD, PhD Department of Gynaecology and Obstetrics Odense University Hospital University of Southern Denmark Lifestyle intervention during pregnancy
- 2. Today´s presentation • Types of lifestyle intervention • RCT • Systematic reviews and metaanalysis • IPD metaanalysis • Weight loss prior to conception • Future perspectives
- 3. Fertility Childhood AdulthoodPostpartum Fertility Embryo Fetus Pregnancy Infertility Miscarriage Congenital anomalies Stillbirth Fetal growth Monitoring GDM Preeclampsia Thromboembolism Infections Thromboembolism Low breastfeeding rate Weight retention Childhood obesity Obesity Metabolic syndrome Delivery Induction of labour Instrumental delivery Cesarean delivery Anaesthetic compl. Intrapartum monitoring Sebire et al 2001, Chu et al 2007, Metwally et al 2008, Heslehurst et al 2008, Stothard et al 2009, Ovesen et al 2011, Nøhr et al 2012
- 4. Gestational Weight Gain (Institute of Medicine 2009) Prepregnancy BMI category Total weight gain Underweight (< 18.5 kg/m2 ) 12.5-18 kg Normal-weight (18.5-24.9 kg/m2 ) 11.5-16 kg Overweight (25.0-29.9 kg/m2 ) 7-11.5 kg Obese (≥ 30.0 kg/m2 ) 5-9 kg IOM: Weight gain during pregnancy: reexamining the guidelines, 2009
- 5. Intervention in pregnancy + Pregnancy is a ”window” of opportunities + Women concerned with the health of their baby + Frequent contact with health care professionals -9 months of pregnancy / a life with obesity -Two lifes to consider - Potential harm for the infants
- 7. Evaluation of intervention • Gestational Weight Gain (GWG) • >/< IOM weight gain recommendations • Maternal outcomes • Neonatal outcomes • Metabolic parameters • Psychological parameters • Long term outcomes
- 8. “Globesity” World Health Organization: • Worldwide obesity has more than doubled since 1980 • In 2008 over 200 million men and 300 million women were obese • 43 million children under the age of five were overweight in 2010 • Obesity is preventable
- 9. • RCT, BMI>30, n= 50 • 10 times individual 1h dietary counseling with dieticians • Reduction in GWG: 6.6 vs 13.3 kg, p=0.002 • No effect on clinical outcomes Denmark Wolff S et al, Int J Obes, 2008
- 10. • RCT, BMI>29, n= 205 • 1) Normal care 2) Brochure 3) Intervention • Intervention: 4 group sessions with a midwife, focus on energy intake and expenditure, healthy food pyramid • Significant reduction in GWG: normal care 13.5kg vs brochure 9.5kg vs intervention 10.6kg • Level of anxiety significantly decreased in intervention group and increased in normal care group • No effect on obstetric and neonatal outcomes Belgium Bogaerts et al, Int J Obesity, 2012
- 11. • RCT, BMI>25, n=132 • Continuity of care provider Weight monitoring Short dietary intervention Psychology assistance when needed • Reduction in GWG: 7.0 vs 13.8 kg, p<0.0001 Reduction in GDM: 6% vs 29%, p<0.04 Australia Quinlivan JA et al, Aust NZJ Obstet Gynecol, 2011
- 12. • RCT, BMI 20-40, n=401 • Low intensity behavioral intervention One face-to-face visit Mailed material Individual graphs of weight gain • Significant reduction in exceeding IOM recommendations: 40.2% vs 52.1%, p=0.003 In normal weight women only! No effect in overweight and obese women USA Phelan S et al, Am J Clin Nutr, 2011
- 13. The LiP (Lifestyle in Pregnancy) Study: A randomized controlled trial of lifestyle intervention in 360 obese pregnant women Vinter C, Jensen DM, Ovesen P, Beck-Nielsen H, Jorgensen JS. Diabetes Care, 2011
- 14. Ringkjøbing Ribe Vejle Århus Fyn BMI > 30 Danish National Board of Health 2012N= 402.955
- 15. The LiP (Lifestyle in Pregnancy) Study: A randomized controlled trial of lifestyle intervention in 360 obese pregnant women. Aim To study the clinical effects of diet and physical activity during pregnancy among Danish obese women Inclusion BMI 30-45, age 18-40 years Exclusion Diabetes, major medical disorders, non Danish-speaking, multiple pregnancy, prior serious obstetric complications including preterm birth Vinter C, Jensen DM, Ovesen P, Beck-Nielsen H, and Jorgensen JS. Diabetes Care, 2011
- 16. Diet • Individual face-to-face diet counseling sessions 4 times during pregnancy • Gestational weight gain 5 kilos
- 17. Physical activity • 30-60 min of daily physical activity • Free membership in fitness center • Aerobic classes 1 h weekly • Coaching in small groups • Pedometer • Activity calender
- 19. GA 35 Intervention n=144 Control n=148 P GWG (kg) 7.0 (4.7-10.6) 8.6 (5.7-11.5) 0.014 GWG < 5 kilos 41 (28.5%) 30 (20.3%) 0.102 GWG < 9 kilos 93 (64.6%) 79 (53.4%) 0.052 Gestational Weight Gain (GWG)
- 20. Obstetric and neonatal outcomes Vinter C et al, Diabetes Care, 2011
- 21. What to do?
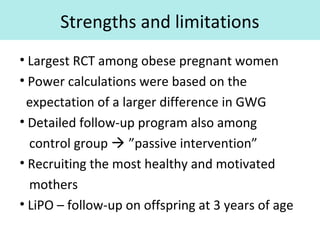
- 22. Strengths and limitations • Largest RCT among obese pregnant women • Power calculations were based on the expectation of a larger difference in GWG • Detailed follow-up program also among control group ”passive intervention” • Recruiting the most healthy and motivated mothers • LiPO – follow-up on offspring at 3 years of age
- 24. PubMed ResultsItems 1 -10 of 10 (Display the 10 citations in PubMed) • 1. Antenatal interventions for reducing weight in obese women for improving pregnancy outcome. Furber CM, McGowan L, Bower P, Kontopantelis E, Quenby S, Lavender T. Cochrane Database Syst Rev. 2013 Jan 31;1:CD009334. doi: 10.1002/14651858.CD009334.pub2. Review • 2. Interventions to reduce or prevent obesity in pregnant women: a systematic review. Thangaratinam S, Rogozińska E, Jolly K, Glinkowski S, Duda W, Borowiack E, Roseboom T, Tomlinson J, Walczak J, Kunz R, Mol BW, Coomarasamy A, Khan KS. Health Technol Assess. 2012 Jul;16(31):iii-iv, 1-191. doi: 10.3310/hta16310. Review. • 3. A systematic review investigating healthy lifestyle interventions incorporating goal setting strategies for preventing excess gestational weight gain. Brown MJ, Sinclair M, Liddle D, Hill AJ, Madden E, Stockdale J. PLoS One. 2012;7(7):e39503. doi: 10.1371/journal.pone.0039503. Epub 2012 Jul 5. Review. • 4. Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomised evidence. Thangaratinam S, Rogozinska E, Jolly K, Glinkowski S, Roseboom T, Tomlinson JW, Kunz R, Mol BW, Coomarasamy A, Khan KS. BMJ. 2012 May 16;344:e2088. • 5. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: systematic review and meta-analysis. Oteng-Ntim E, Varma R, Croker H, Poston L, Doyle P. BMC Med. 2012 May 10;10:47. Review. • 6. Antenatal exercise to improve outcomes in overweight or obese women: A systematic review. Sui Z, Grivell RM, Dodd JM. Acta Obstet Gynecol Scand. 2012 May;91(5):538-45. Epub 2012 Feb 28. • 7. Antenatal dietary interventions in obese pregnant women to restrict gestational weight gain to Institute of Medicine recommendations: a meta-analysis. Quinlivan JA, Julania S, Lam L. Obstet Gynecol. 2011 Dec;118(6):1395-401. doi: 10.1097/AOG.0b013e3182396bc6. Review. • 8. Systematic review of clinical trials on dietary interventions to prevent excessive weight gain during pregnancy among normal weight, overweight and obese women. Tanentsapf I, Heitmann BL, Adegboye AR. BMC Pregnancy Childbirth. 2011 Oct 26;11:81. doi: 10.1186/1471- 2393-11-81. Review • 9. Behavioural interventions for weight management in pregnancy: a systematic review of quantitative and qualitative data. Campbell F, Johnson M, Messina J, Guillaume L, Goyder E. BMC Public Health. 2011 Jun 22;11:491. doi: 10.1186/1471-2458-11-491. Review. • 10. Changing diet and physical activity to reduce gestational weight gain: a meta-analysis. Gardner B, Wardle J, Poston L, Croker H. Obes Rev. Systematic reviews on intervention
- 25. Effects of interventions in pregnancy on maternal weight and obstetric outcomes: metaanalysis of randomised evidence • BMJ 2012 • Study selection: 44 RCT (7278 women) evaluating any dietary or lifestyle intervention to influence maternal weight and pregnancy outcomes • Diet – physical activity – mixed approach Thangaratinam S et al. BMJ 2012
- 26. Mean difference in gestational weight gain (kg) with dietary and lifestyle interventions in pregnancy . Thangaratinam S et al. BMJ 2012;344:bmj.e2088 ©2012 by British Medical Journal Publishing Group
- 27. Relative risk of effect on size for gestational age with dietary and lifestyle interventions in pregnancy . Thangaratinam S et al. BMJ 2012;344:bmj.e2088 ©2012 by British Medical Journal Publishing Group
- 28. Relative risk of effects of weight management interventions in pregnancy on maternal outcomes. Thangaratinam S et al. BMJ 2012;344:bmj.e2088
- 29. Fig 7 Relative risk of effects of weight management interventions in pregnancy on fetal and neonatal outcomes. Thangaratinam S et al. BMJ 2012;344:bmj.e2088 ©2012 by British Medical Journal Publishing Group
- 30. Effects of interventions in pregnancy on maternal weight and obstetric outcomes: metaanalysis of randomised evidence Conclusion: •Dietary and lifestyle intervention in pregnancy are effective in reducing GWG without adverse effect on the risk of SGA •Dietary intervention was associated with the greatest reduction in GWG •Intervention significantly reduced the risk of preeclampsia •Quality of evidence: Moderate for GWG Low for clinical outcomes Thangaratinam S et al. BMJ 2012
- 31. Systematic review of clinical trials on dietary interventions to prevent excessive weight during pregnancy among normal weight, overweight and obese women • BMC Pregnancy and childbirth, 2011 • Study selection: 13 RCT (1434 women), normal weight, overweight and obese women • Evaluating any dietary intervention to influence maternal weight gain and secondarily child and maternal outcomes Tanentsapf I et al, BMC Pregnancy and childbirth, 2011
- 32. Tanentsapf I et al, BMC Pregnancy and childbirth, 2011
- 33. Systematic review of clinical trials on dietary interventions to prevent excessive weight during pregnancy among normal weight, overweight and obese women Conclusion: •Dietary intervention in pregnancy are effective in decreasing GWG, but not preventing excessive GWG (IOM). •No significant difference in weight retention 6 weeks postpartum, but at 6 months postpartum •Dietary intervention had no significant effect on birthweight or maternal outcomes •Low methodological quality of included studies Tanentsapf I et al, BMC Pregnancy and childbirth, 2011
- 34. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: systematic review and meta-analysis • BMC Medicine, 2012 • Study selection: 13 RCT , 6 non-RCT, overweight and obese women (excluding NW only) • Evaluating any antenatal dietary, activity, behavior or lifestyle intervention to improve maternal and perinatal outcomes Oteng-Ntim E et al, BMC Medicine, 2012
- 35. Forest plot of randomised trials investigating the effect of lifestyle advice versus standard care on gestational weight gain (kg). Oteng-Ntim E et al, BMC Medicine, 2012
- 36. Forest plot of randomised trials investigating the effect of lifestyle advice versus standard care on risk of gestational diabetes. Oteng-Ntim E et al, BMC Medicine, 2012
- 37. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: systematic review and meta-analysis Conclusion: •Antenatal intervention in overweight and obese pregnant women is associated with restricted GWG •A trend towards a reduction in GDM •Studies of low to medium quality - findings should be interpreted with caution •Further metaanalysis not needed •Large-scale well-designed prospective trials Oteng-Ntim E et al, BMC Medicine, 2012
- 38. Overall conclusion • Lifestyle intervention restricts gestational weight gain • Conflicting results on the effect on maternal and neonatal outcomes • No major adverse effect (stillbirth, SGA) • Level of evidence is low • Long-term maternal and offspring follow-up is needed
- 39. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population-based study Adjusted odds ratios for adverse pregnancy outcomes for those who gained 3 or more BMI units (~10 kg) during an average of 2 years – Pre-eclampsia 1.78 (95% CI 1.52–2.08) – Gestational hypertension 1.76 (1.39–2.23) – Gestational diabetes 2.09 (1.68–2.61) – Caesarean delivery 1.32 (1.22–1.44) – Stillbirth 1.63 (1.20–2.21) – LGA infants 1.87 (1.72–2.04) Eduardo Villamor, Sven Cnattingius, Lancet 2006
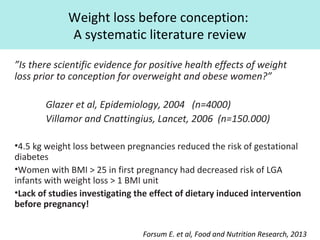
- 40. Weight loss before conception: A systematic literature review ”Is there scientific evidence for positive health effects of weight loss prior to conception for overweight and obese women?” Glazer et al, Epidemiology, 2004 (n=4000) Villamor and Cnattingius, Lancet, 2006 (n=150.000) •4.5 kg weight loss between pregnancies reduced the risk of gestational diabetes •Women with BMI > 25 in first pregnancy had decreased risk of LGA infants with weight loss > 1 BMI unit •Lack of studies investigating the effect of dietary induced intervention before pregnancy! Forsum E. et al, Food and Nutrition Research, 2013
- 42. Ongoing studies TOP study, Denmark Fit for Delivery, Norway ETIP, Norway LIMIT, Australia SPRING, Australia Healthy Moms, USA MOM trial, Canada ………………….
- 43. "Effects of weight management interventions on maternal and fetal outcomes in pregnancy: Individual patient data (IPD) meta-analysis of randomised trials and model based economic evaluation (iWIP)" Women's Health Research Unit Centre for Primary Care and Public Health Blizard Institute Barts and The London School of Medicine and Dentistry
- 44. Project’s overview • Maternal obesity and excess weight gain in pregnancy are associated with maternal and fetal complications in pregnancy and in the long term. • HTA report published in 2012 (Thangaratinam et al. 2012) on diet and lifestyle interventions showed that weight management interventions in pregnancy are effective in reducing maternal weight gain compared to standard care, with diet based interventions most effective. • The findings were based published studies. However, the effects of weight management interventions in women with varied pre pregnancy weight, ethnicity, age and socioeconomic status was difficult to ascertain. Furthermore, the relationship between the amount of weight change in pregnancy and risk of maternal and fetal complications was not known. • To address the above gaps in evidence, project team have established a Collaborative Network of researchers who have conducted studies on weight management interventions in pregnancy. As to the date The Network has access to around 5000 individual patient data from 16 datasets. • By pooling the individual data together, we will be able to estimate with increased confidence, the differential effects if any of the weight management interventions in various groups, allowing us to target the population that needs the most support for a beneficial outcome. It will also generate recommendations on optimal weight gain in pregnancy to minimise maternal and fetal complications and the cost effectiveness of these interventions.
- 45. Project’s objectives and design MAIN OBJECTIVES: The primary objective will be to determine the differential effects of weight management interventions in pregnancy by: i) BMI ii) age iii) ethnicity iv) parity and v) physical and mental medical conditions like diabetes and depression on: a) maternal weight gain and b) composite pregnancy outcome of maternal and fetal complications. DESIGN: Individual patient data (IPD) meta analysis of randomised trials
- 46. Contact details Project Lead: Professor Shakila Thangaratinam s.thangaratinam@qmul.ac.uk Project’s Co-ordinator: Ms Ewelina Rogozinska e.a.rogozinska@qmul.ac.uk Project’s details http://blizard.qmul.ac.uk/research-dissemination/756- iwip.html
- 48. Future perspectives • Should interventions be considered prepregnant to be able to alter short term obstetric and neonatal outcomes? • Nature, duration and intensity of such intervention? • Further research is necessary to identify such interventions and what benefits these confer on health and wellbeing in later life clinical implication and implementation
- 49. Thank you for the attention! christina.vinter@rsyd.dk
Editor's Notes
- We know a lot about obesity in pregnancy and the maternal and neonatal complications it may confer. All phases of reproduction are influenced by obesity. Problems with infertility, miscarriage, congenital anomalies, stillbirth and especially in pregnancy serious problems with GDM and preeclampsia. Obese mothers deliver large babies and seen from a larger health perspective it is of great concern that obese mothers have large infants, these infants grow up with increased risk of developing obesity in childhood and in later life – and then we have the viscous cycle of obesity from generation to generation.
- However, when it comes to handling the problems with obesity in pregnancy we actually only have very little evidence. Management of obesity in pregnancy includes recommendations of appropriate weight gain. In 2009 we had the American IOM recommendations. Based on epidemiological studies they suggest that obese women should gain 5-9 kg, but there is not sufficient evidence to suggest specific GWG recommendations within the obesity classes, which means that they have not distinguished between BMI of 30 and 50 fx. Newer large epidemiological studies from Sweden and USA have suggested that for women in the higher obesity classes GWG below these IOM recommendations may be associated with more favorable outcomes for both mother and child.
- A new phenomenon has been suggested “Globesity” since problems with obesity allover the world is seen with such increased incidence. WHO claims that:…………. Prevention is our special interest
- The intervention included one face-to-face visit; weekly mailed materials that promoted an appropriate weight gain, healthy eating, and exercise; individual graphs of weight gain; and telephone-based feedback
- GWG was calculated as weight at the last visit before delivery minus baseline weight measured in early pregnancy. Mean GWG in intervention group was 7 kg and 8.6 kg in the control group. That was a statistically significant difference. Our optimistic aim of limiting GWG to 5 kg was fulfilled in 28/20%. We also looked at those who restricted GWG as withing the IOM recommendations: 64/53%. Is that a success? Some will mean. On the other hand, with a selected group of highly motivated and otherwise healthy pregnant women, participating in a lifestyle intervention trial it is of concern that 35% of our women actually exceeded general GWG recommendations?
- So, all these struggles and not very optimistic results and very sad p values
- Power calculations were based on the expectation of a larger difference in GWG between groups than we actually found. This should be considered in the conclusions regarding clinical effects of intervention. We speculate that the close follow up in the control group in itself had a behavioral influence on the GWG. Therefore our control group might rather be characterized as a “passive intervention group”. Such cross-over from the control group could explain some of the small differences between our groups.
- Obesity pregnancy intervention, systematic review within the last two years
- Fig 3 Mean difference in gestational weight gain (kg) with dietary and lifestyle interventions in pregnancy Compared with control women there was an overall reduction in GWG of 1.4kg, with the largest reduction in weight seen in the diet intervention group.
- Fig 5 Relative risk of effect on size for gestational age with dietary and lifestyle interventions in pregnancy There was a trend towards decresed risk of LGA, but the difference was not significant. The risk of SGA was not altered with intervention – this is one of the major concerns with intervention, but there was no increased risk of SGA or other adverse outcomes.
- Fig 6 Relative risk of effects of weight management interventions in pregnancy on maternal outcomes The overall effect of intervention led to a 26% reduction of preeclampsia whereas all other outcomes were not associated with an overall decreased risk. However, for the diet intervention alone, compared to controls, there was a significant reduction in both preeclampsia, PIH, GDM and preterm delivery.
- Fig 7 Relative risk of effects of weight management interventions in pregnancy on fetal and neonatal outcomes Based on 15 studies you see the forest plot for fetal and neonatal outcomes. The metaanalysis showed a trend towards reduction in intrauterine deaths and a significant decreased risk of shoulder dystocia in intervention group.
- 150.000 women, swedish data. Association between prepregnancy BMI from first to second pregnancy Suggesting a causal relation between being overweight and the risk of adverse pregnancy outcomes.
- Collaboration Sweden, Norway, Iceland and Denmark
- Paradoxically, at a time of high public health priority, there is a research gap regarding the effectiveness of lifestyle intervention. In terms of the magnitude of the problems there is a need of better evidence
- UPBEAT: U K P regnancy B etter E ating and A ctivity T rial DALI study ETIP, Exercise training in pregnancy LIMIT study MOM trial Canada
- Dr. Hobel, California US, archives from his mother from 1933. 5 cents. Do not overeat.
- To determine any epigenetic changes a long term follow-up in the offspring should be considered