Antileprotic drugs - drdhriti
- 1. Dr. D. K. Brahma Associate Professor Department of Pharmacology NEIGRIHMS, Shillong
- 2. Leprosy is caused by a slow-growing type of bacteria called Mycobacterium leprae (M. leprae) Also known as Hansen's disease, after the scientist who discovered M. leprae in 1873 - Dr. Gerhard Henrik Armauer Hansen of Norway Bears social stigma It primarily affects the skin, mucous membrane and the peripheral nerves Long Incubation period (3 – 5 years) Curable now – deformities/defects – may not reverse
- 3. Chaulmoogra oil Discovery of sulfonamides 1940 onwards 1. Sulfones – Dapsone ( DDS) 2. Phenazine derivative - Clofazimine 3. Antitubercular drugs - Rifampicin, Ethionamide 4. Other Antibiotics: Ofloxacin, Moxifloxacin, Minocycline and Clarithromycin
- 4. The simplest, oldest, cheapest, most active and most commonly used Diamino diphenyl sulfone (DDS) MOA: Leprostatic even at low concentration – higher conc. Arrests growth of may other bacteria Chemically related to Sulfonamides – same mechanism – inhibition of incorporation of PABA into folic acid (folic acid synthase) Specificity to M leprae – affinity for folate synthase Doses for acute infection – too toxic Activity: Used alone – resistance – MDT needed Resistance – Primary and Secondary (mutation of folate synthase – lower affinity) 2.5% to 40% Vs 20% Resistance However, 100 mg/day – high MIC -500 times and continued to be effective to low and moderately resistant Bacilli (low % of resistant patient) Persisters. Also has antiprotozoal action (Falciparum and T. gondii)
- 5. Pharmacokinetics: Complete oral absorption and high distribution (less CNS penetration) 70% bound to plasma protein – concentrated in Skin, liver, muscle and kidney Acetylated and glucoronidae and sulfate conjugated – enterohepatic circulation Half life 24-36 Hrs, but cumulative (1 – 2 weeks) ADRs: Generally Well tolerated drug (100 mg /day) Haemolytic anaemia (oxidizing property) - G-6-PD are more susceptible Gastric - intolerance, nausea, gastritis Methaemoglobinaemia, paresthesia, headache, mental symptoms and drug fever Allergic rashes, FDE, phototoxicity, exfoliative dermatitis and hepatotoxicity etc.
- 6. Sulfone syndrome: Starts after 4- 6 weeks of therapy, more common with MDT Symptoms: Fever, malaise, lymph node enlargement, desquamation of skin, jaundice and anemia – malnourished patients Management: stopping of Dapsone in severe cases, corticosteroid therapy Corticosteroids (prednisolone 40 – 60 mg/day) – severe cases – till reaction controlled – tapered over 8-12 weeks Dapsone contraindications: Severe anaemia and G-6-PD deficiency and hypersensitivity
- 7. A dye - Leprostatic and anti-inflammatory MOA: Interferes with template function of DNA in M. leparae Activity: Used alone resistance (1 -3 years) – but Dapsone resistance cases responds in 2 months (lag period) Kinetics: orally effective – accumulates in fat in crystalline form – entry to CSF poor – half life 70 days Used as component of MDT ADRs: - well tolerated Reddish-black discolouration of skin – exposed parts Discolouration of hair and body secretions, dryness of skin and itching, acneform eruptions and phototoxicity – conjunctival pigmentation GI symptoms: Enteritis with intermittent loose stool, abdominal pain, anorexia and weight loss – early and late symptoms Should be avoided in pregnancy and liver & kidney disease
- 8. Rifampicin: Cidal. 99.99% killed in 3-7 days, skin symptoms regress within 2 months Not satisfactory if used alone – persisters even prolonged treatment Included in MDT to shorten the duration of treatment and also to prevent resistance Not toxic and no induction of hepatic enzyme - dose as single dose only Should not be used in ENL and Reversal phenomenon Ofloxacin: all fluoroquinolones except ciprofloxacin are active. Used as alternative to Rifampicin – 22 daily doses Minocycline: Lipophillic - enters M leprae. Less marked effect than Rifampicin
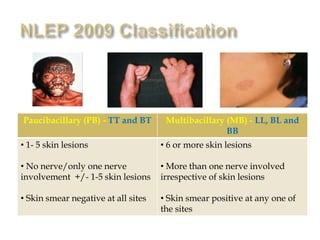
- 9. Granulomatous infection – skin,, mucous membrane and nerves Systems of Classification: 1st (Based on immune system of the patient): Mainly two types: lepromatous (sore on skin, nerves, and other organs) and tuberculoid (sore on skin) 2nd (Ridley-Jopling system – based on symptoms): Borderline tuberculoid leprosy (BL), Borderline lepromatous (BL), Borderline leprosy (BB) and Intermediate leprosy (I) For operational purposes: WHO Paucibacillary (>5 lesions): few bacilli and noninfectious – TT and BT and I Multibacillary (<5 lesions): large bacilli load and infectious – LL, BL and BB types Single lesion Paucibacillary: single lesion
- 10. Paucibacillary (PB) - TT and BT and I Multibacillary (MB) - LL, BL and BB • 1- 5 skin lesions • No nerve/only one nerve involvement +/- 1-5 skin lesions • Skin smear negative at all sites • 6 or more skin lesions • More than one nerve involved irrespective of skin lesions • Skin smear positive at any one of the sites
- 11. Initially (1982) – PBL Dapsone + Rifampicin for 6 Months and MBL – Dapsone + Rifampicin + Clofazimine – 2 years or till disease inactivity/smear negative – with added 5 years surveillance for MBL cases However, 12 years study (in 1994) – fixed duration for 6 months and 2 years was recommended – 12 million to 2.7 million and no resistance In 1999 – 6 months and 1 year recommended
- 12. Drug Paucibacillary (PB) Multibacillary (MB) Rifampicin 600 mg once a month Supervised 600 mg once a month Supervised Dapsone 100 mg daily self administered 100 mg daily self administered Clofazimine - 300 mg once a month Supervised 50 mg daily self administered Duration 6 Months 12 Months
- 13. Photo Courtesy: Dr. Anju R. Marak, SM&HO cum DLO and DMO-MCH, Ri-Bhoi District, Meghalaya
- 14. 1. Lepra Reaction Occurs in LL type (Type – III HSR) – coincides with institution of chemotherapy or intercurrent infection Arthus type of reaction – release of antigens from killed bacilli - may be mild, moderate and severe (ENL) Symptoms: enlarged lesions, become red (inflamed nodules and papules) and painful, new lesions – fever and other constitutional symptoms Treatment: Mild analgesics Mild: Clofazimine - 200 mg daily Moderate to severe-Steroids: 60 mg/day-Prednisolone - taper off in 2-3 months 2. Reversal reaction Occurs in TT and BL cases (Type II HSR) – delayed hypersensitivity to M. leprae antigens • Symptoms: Cutaneous ulceration, multiple nerve involvement with swollen and tender nerves – occurs suddenly even after completion of therapy …… Treatment: same as above
- 15. New Case detection Report
- 17. “The biggest disease today is not leprosy or tuberculosis, but rather the feeling of being unwanted, uncared for, and deserted by everybody.” – Mother Teresa Thank you