CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- 2. COPD is also known as chronic obstructive lung disease (COLD), chronic obstructive airway disease (COAD), chronic airflow limitation (CAL) and chronic obstructive respiratory disease (CORD) Chronic obstructive pulmonary disease (COPD) refers to chronic bronchitis and emphysema, a pair of two commonly co-existing diseases of the lungs in which the airways become narrowed. This leads to a limitation of the flow of air to and from the lungs causing shortness of breath.
- 3. In COPD, less air flows in and out of the airways because of one or more of the following: The airways and air sacs lose their elastic quality. The walls between many of the air sacs are destroyed. The walls of the airways become thick and inflamed. The airways make more mucus than usual, which tends to clog them.
- 5. It is the 4th leading cause of mortality and 12th leading cause of disability in the united states. In 2020 COPD is the 3rd leading cause of death.
- 6. 1)Smoking 2) Occupational exposures- exposure to workplace dusts found in coal mining, gold mining, and the cotton textile industry and chemicals such as cadmium, isocyanates, and fumes from welding have been implicated in the development of airflow obstruction. 3) Air pollution 4) sudden airway constriction in response to inhaled irritants, 5) Bronchial hyperresponsiveness, is a characteristic of asthma.
- 7. 6)Genetics-Alpha 1-antitrypsin deficiency is a genetic condition that is responsible for about 2% of cases of COPD. In this condition, the body does not make enough of a protein, alpha 1-antitrypsin. Alpha 1- antitrypsin protects the lungs from damage caused by protease enzymes, such as elastase and trypsin, that can be released as a result of an inflammatory response to tobacco smoke.
- 8. NUTRITION INFECTIONS SOCIO ECONOMIC STATUS AGING POPULATION
- 9. Abnormal inflammatory response of the lungs due to toxic gases. Responseoccurs in the airways ,parenchyma & pulmonary vasculature. Narrowing of the airway takes place Destruction of parenchyma leads to emphysema.
- 10. Destruction of lung parenchyma leads to an imbalance of proteinases/antiproteinases. (this proteinases inhibitors prevents the destructive process) Pulmonary vascularchanges Thickening of vessels Collagen deposit Destruction of capillary beds. Mucus hypersecretion(cilia dysfunction,airflow limitation,corpulmonale(RVF)) Chronic cough and sputum production
- 11. Chronic cough Sputum production Wheezing Chest tightness Dyspnoea on exertion Wt.loss Respiratory insufficiency Respiratory infections Barrel chest- chronic hyperinflation leads to loss of lung elasticity.
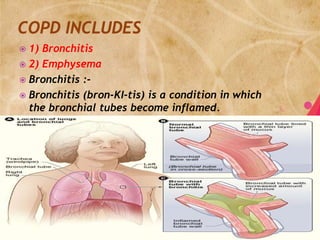
- 12. 1) Bronchitis 2) Emphysema Bronchitis :- Bronchitis (bron-KI-tis) is a condition in which the bronchial tubes become inflamed.
- 13. acute (short term) and chronic (ongoing). Infections or lung irritants cause acute bronchitis. Chronic bronchitis is an ongoing, serious condition. It occurs if the lining of the bronchial tubes is constantly irritated and inflamed, causing a long-term cough with mucus.
- 14. Chronic bronchitis: It is defined as the presence of cough and sputum production for atleast 3 months.
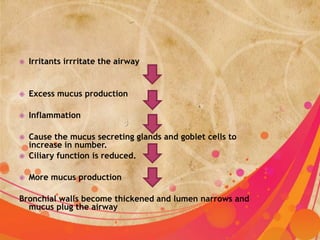
- 15. Irritants irrritate the airway Excess mucus production Inflammation Cause the mucus secreting glands and goblet cells to increase in number. Ciliary function is reduced. More mucus production Bronchial walls become thickened and lumen narrows and mucus plug the airway
- 16. Alveoli adjacent tto the bronchioles may become damaged and fibrosed. Alter function of alveolar macrophages. infection
- 17. sore throat, fatigue (tiredness), fever, body aches, stuffy or runny nose, vomiting, and Diarrhea persistent cough cough may produce clear mucus shortness of breath
- 18. coughing, wheezing, and chest discomfort. The coughing may produce large amounts of mucus. This type of cough often is called a smoker's cough.
- 19. History - medical history •Whether you've recently had a cold or the flu •Whether you smoke or spend time around others who smoke •Whether you've been exposed to dust, fumes, vapors, or air pollution -
- 20. Mucus -to see whether you have a bacterial infection chest x ray, lung function tests, CBC ABG analysis
- 21. MEDICAL MANAGEMENT SURGICAL MANAGEMENT NURSING MANAGEMENT
- 22. IMPROVE VENTILLATION 1. BRONCHO DILATORS LIKE BETA2 AGONISTS(ALBUTEROL),ANTICHOLINERGIC S(IPRATROPIUM BROMIDE-ATROVENT). 2. METHYLXANTHINES(THEOPHYLLINE,AMIN OPHYLLINE) 3. CORTICOSTEROIDS 4. OXYGEN ADMINISTRATION
- 23. REMOVE BRONCHIAL SECRETION PROMOTE EXERCISES CONTROL COMPLICATIONS IMPROVE GENERAL HEALTH
- 24. BULLECTOMY BULLAE ARE ENLARGED AIRSPACES THAT DO NOT CONTRIBUTE TO VENTILLATION BUT OCCUPY SPACE IN THE THORAX,THESE AREAS MAY BE SURGICALLY EXCISED LUNG VOLUME REDUCTION SURGERY IT INVOLVES THE REMOVAL OF A PORTION OF THE DISEASED LUNG PARENCHYMA.THIS ALLOWS THE FUNCTIONAL TISSUE TO EXPAND. LUNG TRANSPLANTATION
- 25. ASSESSMENT PHYSICAL EXAMINATION DIAGNOSIS INTERVENTION
- 26. IMPAIRED GAD EXCHANGE RELATED TO DECREASED VENTILLATION AND MUCOUS PLUGS INEFFECTIVE AIRWAY CLEARENCE RELATED TO EXCESSIVE SECRETION AND INEFFECTIVE COUGHING ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATION ACTIVITY INTOLERENCE RELATED TO INADEQUATE OXYGENATION AND DYSPNOEA
- 27. IMBALANCED NUTRITION LESS THAN BODY REQUIREMENT RELATED TO REDUCED APPETITE,DECREASED ENERGY LEVEL AND DYSPNOEA DISTURBED SLEEP PATTERN RELATED TO DYSPNOEA AND EXTERNAL STIMULI RISK FOR INFECTION RELATED TO INEFFECTIVE PULMONARY CLEARENCE
- 29. Definition:-Emphysema is defined as enlargement of the air spaces distal to the terminal bronchioles, with destruction of their walls of the alveoli. Pathology : As the alveoli are destroyed the alveolar surface area in contact with the capillaries decreases. Causing dead spaces (no gas exchange takes place)
- 30. Leads to hypoxia. In later stages: CO2 elimination is disturbed and increase in CO2 tension in arterial blood causing Respiratory acidosis (Decrease pulmonary blood flowis increased forcing the RV to maintain high B.P. in PA.)
- 31. Centrilobular-Therespiratory bronchiole (proximal and central part of the acinus) is expanded. The distal acinus or alveoli are unchanged. Occurs more commonly in the upper lobes.
- 32. Panlobular-The entire respiratory acinus, from respiratory bronchiole to alveoli, is expanded. Occurs more commonly in the lower lobes, especially basal segments, and anterior margins of the lungs.
- 33. a) History b) PFT c) Spirometry-to find out airflow obstruction. d) ABG analysis e) CT scan of the lung. f) Screening of alpha antitrypsin deficiency g) X-ray radiography may aid in the diagnosis.
- 34. MEDICAL MANAGEMENT SURGICAL MANAGEMENT NURSING MANAGEMENT
- 35. IMPROVE VENTILLATION 1. BRONCHO DILATORS LIKE BETA2 AGONISTS(ALBUTEROL),ANTICHOLINERGIC S(IPRATROPIUM BROMIDE-ATROVENT). 2. METHYLXANTHINES(THEOPHYLLINE,AMIN OPHYLLINE) 3. CORTICOSTEROIDS 4. OXYGEN ADMINISTRATION
- 36. REMOVE BRONCHIAL SECRETION PROMOTE EXERCISES CONTROL COMPLICATIONS IMPROVE GENERAL HEALTH
- 37. BULLECTOMY BULLAE ARE ENLARGED AIRSPACES THAT DO NOT CONTRIBUTE TO VENTILLATION BUT OCCUPY SPACE IN THE THORAX,THESE AREAS MAY BE SURGICALLY EXCISED LUNG VOLUME REDUCTION SURGERY IT INVOLVES THE REMOVAL OF A PORTION OF THE DISEASED LUNG PARENCHYMA.THIS ALLOWS THE FUNCTIONAL TISSUE TO EXPAND. LUNG TRANSPLANTATION
- 38. ASSESSMENT PHYSICAL EXAMINATION DIAGNOSIS INTERVENTION
- 39. IMPAIRED GAD EXCHANGE RELATED TO DECREASED VENTILLATION AND MUCOUS PLUGS INEFFECTIVE AIRWAY CLEARENCE RELATED TO EXCESSIVE SECRETION AND INEFFECTIVE COUGHING ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATION ACTIVITY INTOLERENCE RELATED TO INADEQUATE OXYGENATION AND DYSPNOEA
- 40. DISTURBED SLEEP PATTERN RELATED TO DYSPNOEA AND EXTERNAL STIMULI RISK FOR INFECTION RELATED TO INEFFECTIVE PULMONARY CLEARENCE IMBALANCED NUTRITION LESS THAN BODY REQUIREMENT RELATED TO REDUCED APPETITE,DECREASED ENERGY LEVEL AND DYSPNOEA
- 41. Respiratory insufficiency Respiratory failure Pneumonia Pneumothorax Pulmonary artery hypertension.
- 42. TAKEYOUR MEDICATIONS REGULARLY AS PRESCRIBED,IF YOU HAVE ANY DOUBT RING YOUR HOSPITAL. EXERCISEREGULARLY EVERYDAY OR ELSE ATLEAST 4 OUT OF 7 DAYS.
- 50. THANK YOU!