The Low-down on Lean
- 1. The “Low Down” on Lean Bonnie Brossart, CEO, Health Quality Council Debra Jane Wright, Executive Director, Learning and Implementation, Provincial Kaizen Promotion Office, Health Quality Council
- 2. What we hope to leave you with: A better understanding of the Saskatchewan health care system’s commitment to and early implementation of Lean methodology An increased familiarity with some of the most common Lean concepts and methods we are using in Saskatchewan
- 3. What is Lean? • Lean is a set of operating philosophies and methods that help create maximum value for patients by reducing waste including the waste of time waiting for service. It is often referred to as a learning and management system. • Way of managing and delivering health care, and a new way of relating to and working with patients as partners in their care. Source: www.betterhealthcare.ca
- 4. Why Lean, Why now, Why at such a scale?
- 5. A burning platform… • Unsafe health care – Estimates of one to two avoidable deaths per day in health system (extrapolation from Baker and Norton 2003 study) • Long waits for services - over 15,000 waiting more than 3 months for elective surgery in 2010 • Unrelenting expenditure growth in health care costs – Greater than 7% per annum from mid-1990s to late 2000s
- 6. a compelling vision… • “Patient First” must be embedded as a core value in health care. • Health care in Saskatchewan needs to function as a cohesive system. • Frontline providers must be empowered to deliver patient- and family- centred care.
- 7. …and disquiet with the status quo.
- 8. • Jönköping County (Jönköping, Sweden) • Southcentral Foundation (Alaska) • Virginia Mason Medical Center (Seattle, Washington) • Intermountain Healthcare (Salt Lake City, Utah) • National Health Service (England) • Veterans Health Administration (USA) • Kaiser Permanente (USA) Learning from high-performing, innovative systems greatly influenced our approach
- 9. • Develop and grow leaders for change • Commit to a consistent, rigorous, disciplined improvement methodology • Transparent measurement • Engage and mobilize people • Align processes, priorities • Spread (replicate) innovation Key “take aways” from these systems and their transformation efforts…
- 10. 2012: a new partnership emerged
- 11. Patient First Review: “Keep the Best, Fix the rest” “Fix” = Eliminating waste; waste is anything that does not add value in the eyes of the patient = LEAN Reducing walking Reducing waits Reducing inventory Eliminating defects
- 12. Our approach to making care safer and better • Set provincial health strategy collectively (Hoshin Kanri or Strategy Deployment) • Develop infrastructure to support and coordinate continuous improvement efforts • Build improvement science capability among our leaders & our entire health care workforce (40,000 strong), • Connect learning and doing with achieving health system priorities via Improvement Events • Working in partnership with patients and families
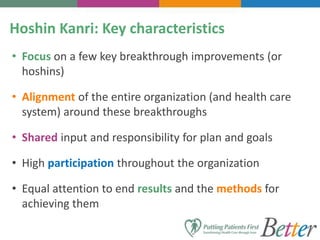
- 13. Hoshin Kanri: Key characteristics • Focus on a few key breakthrough improvements (or hoshins) • Alignment of the entire organization (and health care system) around these breakthroughs • Shared input and responsibility for plan and goals • High participation throughout the organization • Equal attention to end results and the methods for achieving them
- 14. Our approach to making care safer and better • Developing Infrastructure to Support and Coordinate Efforts (Establishing infrastructure) – Quality departments or units transitioned to Kaizen Promotion Offices in all RHAs, Cancer Agency, Ministry of Health, 3sHealth, eHealth – Presently over 100 employees in the health system dedicated to improvement – Creation of Provincial Kaizen Promotion Office (housed at HQC) – Consistent, standardized approach and use of Lean tools – Aim to have 1-2% of workforce with deepened capability to lead & do continuous improvement
- 15. • Building improvement capability among our leaders and health care workforce (40,000 strong) – Over 600 leaders (CEOs, VP, Directors, physicians and improvement staff) currently in Lean Leader Certification) • 83 certified to date • Over 40 physicians in training – Over 16,000 staff have completed Kaizen Basics course (on track to reaching all 40,000 by 2017) Our approach to making care safer and better
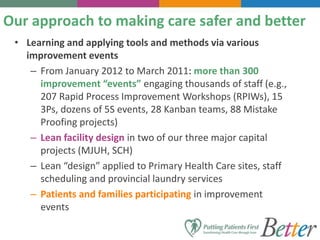
- 16. • Learning and applying tools and methods via various improvement events – From January 2012 to March 2011: more than 300 improvement “events” engaging thousands of staff (e.g., 207 Rapid Process Improvement Workshops (RPIWs), 15 3Ps, dozens of 5S events, 28 Kanban teams, 88 Mistake Proofing projects) – Lean facility design in two of our three major capital projects (MJUH, SCH) – Lean “design” applied to Primary Health Care sites, staff scheduling and provincial laundry services – Patients and families participating in improvement events Our approach to making care safer and better
- 18. Lean is about learning to see
- 19. A snapshot of our work • Built from direct observation on the Gemba • Identifies the steps in our work • Highlights where things tend to run amuck in the process (Starbursts) Value Stream Map
- 20. The Waste Wheel • Identifies opportunities for improvement • Generated by direct observation and by the staff who do the work Types of Waste
- 21. Making too much Doing too much Time on Hand Stock on Hand Movement of Things Movement of People Broken or defective Products/ Equipment All of which can be deemed as unnecessary distractions in our everyday work
- 22. Understanding Movement and Flow • Built from direct observation – by following patients, families, providers, medication, supplies, information and equipment. Spaghetti Diagram
- 23. Visual Controls Signals in our System • How can we make it easy to know what the right thing is every day Visual Controls
- 24. Mistake Proofing Devices Preventing errors and eliminating defects • Making it difficult to do the wrong thing and even better, making it impossible to do the wrong thing.
- 25. Mistake Proofing Understanding our Roles, Responsibilities & Tasks • Having clarity in who does what is helpful to ensure we are all working to our best ability to provide care for our patients. Standard Work (SW)
- 26. Daily Visual Management BoardsDaily Visual Management (DVM) Understanding our Collective Work • Making information visible • Identifying , talking about and testing ideas to improve your work on a daily basis
- 27. Personal Production Board Team Production Board Unit Level DVM Board Service Line Visibility Wall Cascading Communication • Making work visible across the multiple levels in our system
- 28. Regional Walls Provincial Walls Communication Cascades continue • To regional and organizational walls and up to a provincial walls on a quarterly basis
- 29. Lean is about learning to do
- 30. RPIW Try-storming change on the Gemba • Senior Leaders, managers, point of care staff from the area , and patients come together to test and implement improvement ideas over 5 days. Rapid Process Improvement Workshop (RPIW)
- 31. RPIW Eliminating Defects in our Work Senior Leaders and managers working together to identify and redesign mistake- prone situations, to ensure safe care for patients and providers. Mistake Proofing Project Team
- 32. RPIW Building, designing or redesigning a better future • 3P stands for Production Preparation Process and is a Lean method • Highly engaging and creative workshop to rethink what’s possible 3P Workshop
- 33. Managing Inventory • Built on the concept of just in time and visual cues, to make it easy to find, fill and reorder materials and supplies. Kanban Seminar
- 34. A well organized work place • Organizing and sustaining the orderliness of your workplace, to allow you to do your best work everyday. 5S Campaign
- 36. Leaders’ Impressions of SK’s Transformation “I wouldn’t want to be anywhere else…because I want to be part of this; I want to see it succeed. At a very personal level, it is the most satisfying thing I have ever been associated with.” Maura Davies, CEO, Saskatoon Health Region "The Saskatchewan Union of Nurses welcomes the opportunity for front-line care providers to have their voices heard…A focus on patient- and family-centred care using best practice evidence and Lean principles will improve the patient experience and return nursing to a rewarding career." Rosalee Longmoore, Past President , Saskatchewan Union of Nurses “I’m a lot less frustrated…I can see things happening in my community which is the whole purpose why I ever volunteered to be in a regional health authority in the first place.” Tina Rasmussen, Board Chair, Keewatin Yatthe Health Region
- 37. Staff’s experiences with Lean “That RPIW really proved what lean was all about; making small incremental improvements…When something doesn’t work, you try a different approach and get expertise from the people at the point of care and service. I love seeing the shared education that happens when we cross pollinate on rapid process improvement workshop teams.” Lisa White, Kaizen Promotion Office, Saskatoon Health Region “Each potential and true injury is treated and addressed as an opportunity for learning and prevention with frequent team huddles and transferring/lifting/repositioning (TLR) audits…This has been effective and inspired everyone to be more aware. Marie Legault Lalonde, Unit 3-2 Manager, Wascana Rehabilitation Centre
- 38. Saskatchewan’s Implementation of Lean We are cultivating the discipline required to stick to and be successful in attaining our ambitions
- 39. Saskatchewan’s Implementation of Lean Working differently means we are embracing the complexity of Saskatchewan’s health system and the challenges we face.
- 40. The commitment to and ambition of the health system to “thinking and acting as one” is unprecedented.
- 41. “When it comes to Lean, Saskatchewan hasn’t even hit kindergarten.” Maura Davies, President & CEO, Saskatoon Health Region And probably the most important lesson learned so far: Humility
- 42. Want to learn more?