2021 12 operational planning slide sharev4
- 1. Planning guidance 2022/23 Implications, actions and directions…what does it mean for primary care?
- 2. Ten priority areas Focus across all areas on : • Prevention of ill-health • Tackling of health inequalities • Enhancing productivity and value for money • Supporting broader social and economic development Workforce * COVID-19 response Elective care Urgent care Primary care Mental health and learning disability Population health management Digital Effective use of resources Integrated care boards Based on the proviso that COVID-19 infection rates return to low levels *At the time of publication level 4 incident level in place as a result of omicron variant Financial plan – revenue allocations- for one year; capital allocations - for three years All under continual review New target date for statutory arrangements- 1 July 2022 SYSTEM FOCUSSED
- 3. Workforce • Continued investment • New ways of working • Strengthening compassionate and inclusive culture COVID-19 • Vaccination programme • Care for patients with COVID Points to note • Whole system workforce plans to set out how to increase workforce • ARRS to deliver 26,000 roles to support creation of multidisciplinary teams • Accelerated introduction of new roles such as first contact practitioners and expanding advanced clinical practitioners • Suite of national GP recruitment and retention initiatives Impact on primary care • General practice and community pharmacy remain a key component of the infrastructure to deliver the vaccination programme • Activity of other primary care contractors is compromised by guidelines around infection control
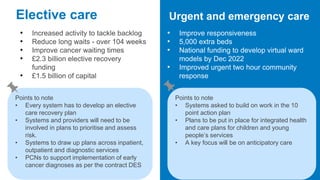
- 4. Elective care • Increased activity to tackle backlog • Reduce long waits - over 104 weeks • Improve cancer waiting times • £2.3 billion elective recovery funding • £1.5 billion of capital Urgent and emergency care • Improve responsiveness • 5,000 extra beds • National funding to develop virtual ward models by Dec 2022 • Improved urgent two hour community response Points to note • Every system has to develop an elective care recovery plan • Systems and providers will need to be involved in plans to prioritise and assess risk. • Systems to draw up plans across inpatient, outpatient and diagnostic services • PCNs to support implementation of early cancer diagnoses as per the contract DES Points to note • Systems asked to build on work in the 10 point action plan • Plans to be put in place for integrated health and care plans for children and young people’s services • A key focus will be on anticipatory care
- 5. Primary care • Improve timely access • Maximise the impact of investment to expand capacity • Drive integrated working at neighbourhood and place level • Digital first primary care by 2023/24 Community pharmacist consultation service - timescale Oct 2022 • Every opportunity to secure universal participation and to drive lower acuity of care from GP and NHS 111 • Supported by the impact and investment fund indicator for PCNs. • Community pharmacy to support delivery of care processes such as BP monitoring Network DES • Phased introduction of anticipatory care and personalised care • CVD diagnosis and prevention to be expanded Dental Services Focus on maximising clinically appropriate activity in light of infection control measures Targeting capacity to meet urgent care demand Points to note • Systems are to ensure the involvement of PCNs, community services and also community pharmacy. • Systems to support PCN recruitment including shared employment models • Expansion of number of GPs to continue • Promotion of community pharmacist consultation service to continue From July 2022- ICBs will become delegated commissioners for primary medical services (and in some cases dental, community pharmacy and optometry).
- 6. Mental health and learning disability services • Continued investment • Transform and expand community health services and improve access Population health management • Continued focus • Using data to redesign care pathways with a focus on improving access and health equity for underserved communities Points to note • PCNs asked to continue to use the mental health practitioner roles • Learning disabilities- Increase the rate of annual health checks to 75% by 2023/24 • Continue to improve the accuracy of coding on GP systems Points to note • By April 2023 - every system will have the technical capability for population health management • Will allow prediction and risk stratification • The system will also restore diagnosis, treatment and management of hypertension, AF and high cholesterol and diabetes. • Renewed focus on screening
- 7. Digital • Exploit potential of digital technologies • Achievement of a core level of digitisation in every service across systems • General practices to promote NHS App and NHS.UK to reach 60% of population by 2023 • Shared care record expansion, including social care • Provision of robust cyber security Resources • Return to pre-pandemic levels and beyond • Fully restore core services • Make in-roads to address elective backlog • ICB and partner objective to deliver financially balanced system
- 8. Establishment of ICBs Working together with local stakeholders across the ICS to develop a five year strategic plan Continued focus… • Five priority areas for tackling health inequalities • Population health management • Core20PLUS5 – approach to reducing health inequalities From July 2022- ICBs will become delegated commissioners for primary medical services (and in some cases dental, community pharmacy and optometry) . 2023/24- Dental, community pharmacy and optometry will all be delegated. Subject to the passage of the Health and Care bill
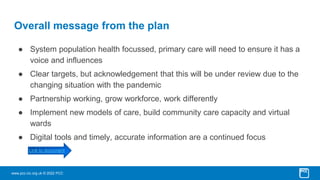
- 9. www.pcc-cic.org.uk © 2022 PCC Overall message from the plan ● System population health focussed, primary care will need to ensure it has a voice and influences ● Clear targets, but acknowledgement that this will be under review due to the changing situation with the pandemic ● Partnership working, grow workforce, work differently ● Implement new models of care, build community care capacity and virtual wards ● Digital tools and timely, accurate information are a continued focus Link to document
- 10. www.pcc-cic.org.uk © 2022 PCC ● Range of virtual courses being delivered over the coming months. See PCC events calendar for further details ● Visit our website for news, articles and how we can help you www.pcc- cic.org.uk ● Keep up to date with NHS news - sign up to our free weekly newsletters www.pcc-cic.org.uk/newsletters/