Age changes in prosthodontics
- 1. BY -: Dr. BARUN KANT MDS I3/6/2015 1
- 2. Introduction Defintion Scope of the problem Psychologic and psychiatric aspects of aging Aging and nutrition Oral aspects of aging Prosthetic diagnosis Complete denture construction Summary 3/6/2015 2
- 3. Because we are born ,we grow old and because grow old ,we die. It is unfortunate that the geriatric patients generally needs most of the necessary dental and medical services at an age when he is least able to tolerate them and possibly least able to afford them. Although fluoridation and other preventive measures will undoubtedly have an affect on the incidence of dental caries and the resultant tooth loss of our population ,the benefits to the geriatric patients of today are negligible . 3/6/2015 3
- 4. The prosthetic needs of our geriatric population are monumental and most probably will remain that way at least for the next generation. 3/6/2015 4
- 5. Gerontology(gerodontological society in 1959): “The branch of knowledge which is concerned with situations and changes inherent in increments of time ,with particular reference to post maturational stages.” 3/6/2015 5
- 6. In 1900 ,only 3.1 million , or one of every 25 ,Americans were 65 years of age or older . In 1984 ,27.9million ,or one of nine ,fell into this category. If present population trends continue ,those over 65 should account for 64.5 million ,or 21.2 %,of the population by the yer 2030. 3/6/2015 6
- 7. The majority of elderly persons in their younger retirements years are relatively healthy and not limited in activity ,even if they have a chronic illness . By the end of 8th and 9th decade of life ,the chances of being limited in activity and in the need of health services increases significantly. 3/6/2015 7
- 8. 0 10 20 30 40 50 60 male female male female black white Numberper100population 45-64 years 65 years and over 3/6/2015 8
- 9. The problems of adjusting to old age in our society is becoming extremely difficult owing to the high values placed on youth .,beauty ,and virility. Members of the medical and dental profession in some cases have fallen pray to these existing attitudes ,perhaps partially because of personal fears regarding their own aging process . 3/6/2015 9
- 10. For the aged themselves ,these are frustrating years . They realize that they are beyond their productive peak and many of their goals ,ideals ,ambitions, and hopes can never be attained . As certain physical attributes decline ,others becomes stronger . 3/6/2015 10
- 11. Memory may decline ,but judgment may improve with age . Experience ,being dependent on time ,inevitably increase with age . Retirees should be encouraged to participate in creative activities as long as they are able ,especially in the social ,economic ,and political life of their community . 3/6/2015 11
- 12. Lonely patients can turn to the dentist for aid in their ever ending struggle against illness and old age . Weekly and monthly appointments can become the most significant aspects of their lives . It gives them a reason for having to do something or go somewhere ,and they look forward to it . A sympathetic word when inserting dentures into the mouth often does wonders . 3/6/2015 12
- 13. Hardly elderly – many of our modern aged are in excellent physical and psycho logic condition . The senile aged syndrome –these people are disadvantaged physically and emotionally and may be described as handicapped ,chronically ill ,disabled ,infirm and truly aged . Between these two extremes are millions of elderly. 3/6/2015 13
- 14. Nutrition is one of the factors under human control that can influence the health of the aging . It is essential for the geriatric patient to retain an interest in food . He must be prevented ,because of dental difficulties ,from gradually changing his diet to softer foods that require little or no chewing and are easy to swallow . A lack of protein can result . 3/6/2015 14
- 15. A reduction of fats in the diet limits the deposition of cholesterol in the arterial walls . An adequate dentition ,either natural or artificial ,is not essential for sufficient food intake for maintaining a good nutritional balance during normal health. However ,an adequate dentition ,either natural or artificial, may be necessary to support the extra demands of illness and is definitely needed as an aid to the enjoyment of food. 3/6/2015 15
- 16. 3/6/2015 16
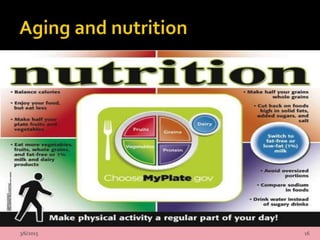
- 17. Nutritional guidelines for the patients undergoing removable prosthodontic treatment. Eat a variety of foods . Build diet around complex carbohydrates . Eat at least five serving of fruits and vegetables daily. Select fish, poultry ,lean meat,eggs,or dried peas and beans everyday. 3/6/2015 17
- 18. Consume four serving of calcium –rich food daily. Limit intake of bakery products high in fat and simple sugars . Limit intake of prepared and processed foods high in sodium and fat. Drink several glasses of water,juice ,or milk daily. 3/6/2015 18
- 19. Risk factors for malnutrition in patients with dentures Eating less than two meals per day , Difficulty chewing and swallowing . Unplanned weight gain or loss of more than 10 lb in the last 6 month. Undergoing chemotherapy or radiotherapy. Alcohol or drug abuse. Unable to shop for,cook for ,or feed oneself. 3/6/2015 19
- 20. Nutritional requirement of the elderly carbohydrates should compromise 45-65% of total calories. Fat should compromise 20-35% of total calories . Protein should compromise 10-35%of total calories . Fluid should compromise 30ml/kg/day or 1ml/kcal intake. 3/6/2015 20
- 21. Loss of teeth-due primarily to degeneration of periodontal structures. Attrition –rate is influenced by diet and masticatory habits (bruxism) Oral mucosa –loss of elasticity with dryness and atrophy .Tendency to hyperkeratosis . Gingivae-loss of stippling .edematous appearance .Keratinized layer thin or absent .Tissue friable or easily injured . 3/6/2015 21
- 22. 3/6/2015 22
- 23. 3/6/2015 23
- 24. Saliva –diminished function of salivary glands with relative or absolute xerostomia due to atrophy of cells lining the intermediate ducts .Xerostomia also result in abnormal taste sensation and stomatodynia. Tongue –atrophic glossitis ,probably due to concurrent vitamin B complex deficiency. Lips –angular chelitis is very common and is probably related to concurrent vitamin B complex deficiency. Chelitis due to dehydration . 3/6/2015 24
- 25. Contrary to the belief of many patients and some dentists ,the loss of teeth is not an inevitable consequence of growing old . Unfortunately there are many in the dental profession who are radical in their attitudes towards the elderly . Even when the loss of all the remaining natural teeth are inevitable ,they are too quick in diagnosing complete dentures . 3/6/2015 25
- 26. Although the patients no doubt will adapt better to complete dentures at an earlier age ,conservatism and the construction of partial, transitional ,or overdenture is the treatment of choice . It is better to retain the natural teeth for as long as possible and eventually accept the complete dentures with their decreased efficiency . 3/6/2015 26
- 27. The longer a patient retain some of his natural teeth ,the shorter the time he will be edentulous ,and better the residual ridges will be. Patients motivation cannot be underestimated The patient must realize his need for prosthetic treatment ,want dentures, accept the prosthesis ,and attempt to learn to use it . 3/6/2015 27
- 28. The dentist, in turn , must adapt his technique to fit the patient, perhaps changing his original diagnosis as treatment progresses ,and concern himself with the construction of a functional and comfortable prosthesis . 3/6/2015 28
- 29. Many times nothing is as important as good clinical judgment in prosthetic diagnosis for the geriatric patients . Complete denture should not be constructed if a patient is under extreme physical or mental stress . Too little treatment can be just as harmful as too much treatment . 3/6/2015 29
- 30. The majority of practicing dentists have probably seen wearers of old dentures with vulcanite or early acrylic dentures that actually float in the patient’s mouth. It is an error to try to talk to these geriatric patients into having new dentures constructed . 3/6/2015 30
- 31. An elderly person who has been without teeth for many years and has no desires for complete dentures is best left alone . If facial appearance is unimportant to these patients and being without teeth does not alter their personalities ,it is an error to convince them to have complete dentures constructed . 3/6/2015 31
- 32. Jamieson wrote that “fitting the personality of the aged patient is often more difficult than fitting the dentures to the mouth .” Older patients are often more irritable and demanding than younger patients . Geriatric patients should not be promised too much . 3/6/2015 32
- 33. It has been written and said many times that esthetics is unimportant or secondary in fabrication of dentures for the aged . The loss of tooth is a traumatic experience . Although we know that dentures can and do improve facial appearance ,dentist are not plastic surgeons . 3/6/2015 33
- 34. If the final dentures are not what the patients want or expects esthetically ,they may be immediately rejected . If the patient cannot be convinced to accept the dentures on esthetic grounds ,improved function and other features should be stressed . 3/6/2015 34
- 35. Impressions Prior to making edentulous impression for geriatric patients ,the denture bearing tissues must be thoroughly examined . Although it is true that age tolerate change badly and it is wise to avoid major changes ,this does not mean that new dentures should be under extended , no matter how short the patients old dentures were . 3/6/2015 35
- 36. The finished dentures should be as large as possible within the functional limitation of the patients with no impingement on functional borders. 3/6/2015 36
- 37. Vertical dimension The determination of vertical dimension in a young healthy individual is difficult. With the geriatric patients ,much more time and efforts are required to ensure an accurate physiologic recording . The interocclusal distance increases with age . 3/6/2015 37
- 38. It is claimed by some investigators that continuous eruption of the teeth will adequately maintain the vertical dimension . The falling-in of the lips ,due to loss of adequate support and muscle tone ,complicates the difficulty of determining vertical dimension. Geriatric patients needs more than the average 3-mm inter occlusal distance of the young adult with a full complement of teeth . 3/6/2015 38
- 39. If severe difficulty exists in the determination of vertical dimension ,the patient’s old dentures, if available ,can be used as a guide . In some elderly patients ,even though the vertical dimension is carefully and to the best of our knowledge correctly determined, “clicking” of the dentures may still occur because of muscular incoordination or habit. 3/6/2015 39
- 40. Centric relation The correct recording and duplication of centric relation is parmount to the success of complete denture . A prognathic position of the mandible with a resultant convenience eccentric bite is often acquired by the geriatric patients ,usually the result of a closed occlusal vertical dimension. 3/6/2015 40
- 41. The patients must be seated in an upright position ,if at all possible ,before centric relation can be recorded . Although many prosthodontics recommend a gothic arch or arrow point tracing for the determination of centric relation of the elderly ,the author favors interocclusal wax check bites after the initial tentative centric relation has been recorded by wax occlusal rims constructed on shellac ,gutta –percha ,or resin recording bases 3/6/2015 41
- 42. Posterior tooth selection The posterior teeth are responsible for the occlusion of a complete denture . The arrangement of the posterior teeth plays a significant part in the retention and stability of the dentures and the condition of the supporting tissues . Many prosthodontics recommend zero degree posterior teeth for the edentulous geriatric patients . 3/6/2015 42
- 43. Several non anatomic modification of posterior tooth forms constructed wholly or partially of chromium cobalt alloy are available that are claimed to be advantageous for patients with less than average closing pressure . And where it is necessary to reduce the force of the denture on the bearing surface during function. 3/6/2015 43
- 44. Hardy has designed blocks of upper and lower acrylic posterior teeth in which curved metal cutting blades are embedded. Although the chromium cobalt modification of posterior tooth are enjoying some degree of popularity ,they must be used with reservation and only in specially selected cases . 3/6/2015 44
- 45. 3/6/2015 45
- 46. Adjustment No matter how much care and skill are incorporated into the fabrication of complete denture ,their insertion is usually followed by irritation and trauma in varying degrees . The soft tissue pain threshold changes greatly after menopause and the male climacteric ,with an increase in the sensitivity ,which according toVinton ,frequently reaches the magnitude of 400%. 3/6/2015 46
- 47. The geriatric patients should be seen the day after insertion or, at the latest ,the second day If the patients is a new complete denture wearer ,mastication should not be attempted until the denture can be worn comfortably and speech presents no problems . During the adjustment visits ,the patients should be asked for pointing out areas of soreness . 3/6/2015 47
- 48. However ,patients are poor judges and usally cannot locate exact areas of discomfort . Geriatric patients can remove one or both dentures during the day if their mouth feel tired after the adjustment periods. If the patients is unable to care for his denture or is afraid to try because of the fear of dropping and breaking them ,oral hygiene will be entirely dependent on another person. 3/6/2015 48
- 49. Relines If the dentures of the geriatric patients must be relined because of the inability of the dentist to construct new denture for any reason, the existing jaw relation and the arrangement of the teeth must be satisfactory. 3/6/2015 49
- 50. Dental care of the aging patients presents a number of problem not encountered in younger patients . Most of these problems result from tissue changes that occur during aging.The dentist, especially the prosthodontics ,is in a strategic position to evaluate and correct many of the dietary and nutritional deficiencies that promote premature aging of tissues . 3/6/2015 50
- 51. Sharry J.P. : Complete denture prosthodontics. 3rd Ed. Mc Graw Hill Book Co., 1974. Sheldon Winkler: Essentials of complete denture prosthodontics 2nd Ed. Detroit Mich : Nutrition for the aging patient. J. Pros. Dent., 10 : 53-60, 1960. Perry C. : Nutrition for senescent denture patients. J. Pros. Dent., 11 : 73-78, 1961. Ramsay W.D. : Role of nutrition in conditions of edentulous patients. J. Pros. Dent., 23 : 130, 1970. Carl O Boucher: Boucher's ProsthodonticTreatment for Edentulous Patients (13th Edition) "Food Pyramids:What ShouldYou Really Eat?". www.hsph.harvard.edu. Retrieved 2009-12-25 Dental Clinics Of North America volume 49 number 2 april 2005: GERIATRICS: contemporary and future concerns 3/6/2015 51
- 52. 3/6/2015 52