Approach to pitiutary diseases
- 1. Anatomy of the Pituitary Gland
- 2. Pituitary Hormones ➢ Anterior Pituitary ▪ Thyroid Stimulating Hormone (TSH) ▪ Adrenocorcticotropic Hormone (ACTH) ▪ Growth Hormone (GH) ▪ Follicle Stimulating Hormone (FSH) ▪ Luteinizing Hormone (LH) ▪ Prolactin (Prl) ➢ Posterior Pituitary ▪ Arginine Vasopressin (AVP) ▪ Oxytocin
- 3. Hypothalamic Hormones ▪ Thyrotropin Releasing Hormone (TRH) ▪ Corticotropin Releasing Hormone (CRH) ▪ Growth Hormone-Releasing Hormone (GHRH) ▪ Growth Hormone Release Inhibiting Hormone (Somatostatin) ▪ Gonadotropin Releasing Hormone (GnRH) ▪ Prolactin Release Inhibiting Hormone (Dopamine)
- 4. The Hypothalamic- Pituitary Axes
- 5. Lesions of Hypothalamic Pituitary Axis Hypothalamic (hypothalamic or pituitary stalk disease) vs. Primary Pituitary Disease ▪ Acquired Defects: Tumors (inc. Pit. Adenomas), Trauma, Irradiation, Inflammatory/Infiltrative d/s, Vascular d/s (inc. Apoplexy), Empty Sella, Primary Neoplastic d/s, Metastatic d/s, Metabolic d/s and Functional d/s. ▪ Congenital Embryopathic Defects: Kallman’s syndrome, Pituitary Aplasia, Anencephaly, Midline defects. ▪ Genetic Defects: Hypothalamic / Pituitary Hormone Gene Defects and Hormone Receptor Gene Defects.
- 6. Clinical Manifestations of Lesions of Hypothalamic Pituitary Axis ➢ Mass effects: Headaches, Visual Field and CN III-VI Defects, Obstructive Hydrocephalus, CSF Rhinorrhea, Hypothalamic Syndromes (DI, SIADH, thirst/ appetite/ satiety/ sleep/ temperature regulation), Frontal/ Temporal Lobe Dysfunction ➢ Endocrine Effects: ▪ Hypopituitarism: TSH/ ACTH/ GH/ LH-FSH/ Prolactin ▪ Hyperpituitarism: TSH/ ACTH/ GH/ LH-FSH/ Prolactin
- 7. Mass Effects of Pituitary Lesions
- 8. Organization of visual fibers at the Optic Chiasm
- 9. Pituitary Adenoma With Involvement Of Left Oculomotor Nerve
- 10. Pituitary Tumor
- 12. Pituitary Apoplexy w/ OC compression
- 13. Clinical Manifestations of Lesions of Hypothalamic Pituitary Axis ➢ Mass effects: Headaches, Visual Field and CN III-VI Defects, Obstructive Hydrocephalus, CSF Rhinorrhea, Hypothalamic Syndromes (DI, SIADH, thirst/ appetite/ satiety/ sleep/ temperature regulation), Frontal/ Temporal Lobe Dysfunction ➢ Endocrine Effects: ▪ Hypopituitarism: TSH/ ACTH/ GH/ LH-FSH/ Prolactin ▪ Hyperpituitarism: TSH/ ACTH/ GH/ LH-FSH/ Prolactin
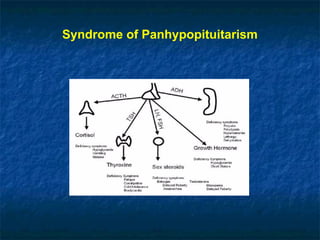
- 14. Syndrome of Panhypopituitarism ➢ Progressive loss of Anterior Pituitary function: FSH/LH and GH; TSH; ACTH. ➢ Hypopituitarism with DI is suggestive of Hypothalamic etiology.
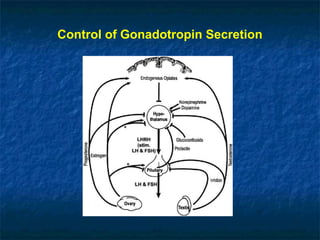
- 16. Control of Gonadotropin Secretion
- 17. Syndrome of Panhypopituitarism ➢ FSH / LH deficiency: ▪ In women: Oligo-amenorrhea, Infertility, “Post-menopausal” symptomatology, Bone loss. ▪ In Men: Decreased Libido, ED, Gynecomastia with loss of secondary sexual characteristics, Bone loss. ▪ Labs: Gonadotropins inappropriately low for E2 in women and T in men.
- 18. Syndrome of Panhypopituitarism ➢ GH deficiency in Adults: ▪ Symptoms: Reduced muscle mass and decreased exercise performance, Increased abdominal adiposity, Decreased psychosocial well being. ▪ Signs: Central adiposity, thin dry skin, Decreased muscle strength. ▪ Labs: Hyperinsulinemia, Dyslipidemia, “Low-normal” IGF-1 with inadequate response on Insulin tolerance test/ L-Dopa test/ L-Arginine test.
- 19. Syndrome of Panhypopituitarism ➢ GH deficiency in Children: ▪ GH deficiency (especially prior to onset of puberty) leads to growth retardation/ short stature. ▪ Thyroid and Corticosteroid replacement are necessary for GH action in patients with panhypopituitarism.
- 20. Syndrome of Panhypopituitarism ➢ TSH deficiency: ▪ Symptoms: Fatigue, Cold intolerance, Lethargy, Constipation, Diminished appetite, Weight gain, Hoarseness of voice, Menorrhagia. ▪ Signs: Bradycardia, Hypothermia, Pale/ cool/ dry skin, dry hair, “hung up” DTRs, stupor/ coma in severe cases. ▪ Labs: “Low-normal” TSH with low Free T4, Abnormal TRH Stimulation test, Hyponatremia in severe cases.
- 21. Syndrome of Panhypopituitarism ➢ ACTH deficiency: ▪ Symptoms: Weakness, Fatigue, Nausea/ Vomiting, Weight loss ▪ Signs: Pale skin with inability to tan, Postural Hypotension. ▪ Labs: Mineralocorticoid function is preserved, Low AM cortisol, +/- ACTH Stimulation test, Poor pituitary ACTH reserve on Insulin tolerance test/ CRH stimulation test/ Metyrapone test.
- 22. Maintenance Medications for Hypopituitarism
- 23. Empty Sella Syndrome ➢ Defects in diaphragma sella allowing herniation of arachnoid membrane into the hypophyseal fossa thereby leading to transmission of ICP and compressing the pituitary against the walls of the sella. ➢ Primary vs. Acquired (Surgery, Radiation therapy, Infarction) ➢ Pituitary function is usually normal +/- mild elevations of Prolactin.
- 25. Clinical Manifestations of Lesions of Hypothalamic Pituitary Axis ➢ Mass effects: Headaches, Visual Field and CN III-VI Defects, Obstructive Hydrocephalus, CSF Rhinorrhea, Hypothalamic Syndromes (DI, SIADH, thirst/ appetite/ satiety/ sleep/ temperature regulation), Frontal/ Temporal Lobe Dysfunction ➢ Endocrine Effects: ▪ Hypopituitarism: TSH/ ACTH/ GH/ LH-FSH/ Prolactin ▪ Hyperpituitarism: TSH/ ACTH/ GH/ LH-FSH/ Prolactin
- 26. Pituitary Adenoma ➢ Microadenomas are < 10mm. ➢ Macroadenomas are ≥ 10mm. ➢ Majority are monoclonal and not malignant. ➢ May or may not be functional. ➢ Mass effects and hypopituitarism may be present irrespective of functional status. ➢ Functioning (secretes hormones) vs. non-functioning
- 27. Prevalence of Pituitary Tumors
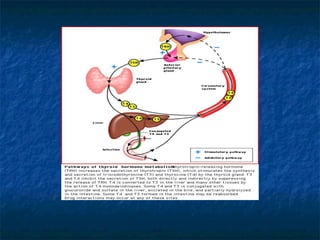
- 28. The Thyroid Axis
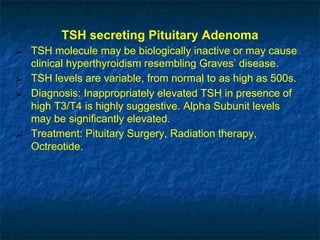
- 29. TSH secreting Pituitary Adenoma ➢ TSH molecule may be biologically inactive or may cause clinical hyperthyroidism resembling Graves’ disease. ➢ TSH levels are variable, from normal to as high as 500s. ➢ Diagnosis: Inappropriately elevated TSH in presence of high T3/T4 is highly suggestive. Alpha Subunit levels may be significantly elevated. ➢ Treatment: Pituitary Surgery, Radiation therapy, Octreotide.
- 30. FSH/LH secreting Pituitary Adenoma ➢ No characteristic syndrome of hormone excess is seen. ➢ Occasionally- ▪ In Men: +/- testicular enlargement, hypogonadal symptoms. ▪ In Women: +/- hypogonadal signs and symptoms. ➢ Treatment: Pituitary surgery, Radiation therapy.
- 31. Neuroendocrine regulation of the HPA axis
- 32. ACTH secreting Pituitary Adenoma (Cushing’s Disease) ➢ Accounts for about 60-70% of cases of Cushing’s syndrome. ➢ Symptoms: Fatigue, Weight gain, Easy bruising, Headaches, Irregular menses, Psychiatric symptoms from depression to frank psychosis. ➢ Signs: Plethoric “Moon facies”, ”Buffalo hump”, Central adiposity with thin extremities, Hyperpigmentation, Hypertension, Hirsuitism, Acne, Purple striae, Proximal myopathy.
- 33. ACTH secreting Pituitary Adenoma (Cushing’s Disease) ➢ Labs: IFG/IGT, Hypokalemia and Alkalosis, Leukocytosis, Lymphopenia, Bone loss on DXA. ➢ Diagnosis : Elevated 24 hour urinary free cortisol and/or lack of suppression by low dose dexamethasone, Elevated ACTH levels, Ectopic ACTH syndrome ruled out. ➢ Treatment: Pituitary surgery, Medical therapy as temporizing measure, Radiation therapy
- 34. GH secreting Pituitary Adenoma (Acromegaly) ➢ “Acral” and “facial” growth in Adults (once the epiphyses of long bones are fused). ➢ 40% may co-secrete Prolactin. ➢ Symptoms: Headaches, Arthralgias, Fatigue, Hyperhidrosis, entrapment neuropathies, Sleep Apnea, Deepening of voice, Impotence in men, irregular menses in women.
- 35. GH secreting Pituitary Adenoma (Acromegaly and Gigantism) ➢ Signs: “Coarsening” of facial features, enlarged hands and feet secondary to soft tissue hypertrophy, oral malocclusion and increased spacing between teeth, Moist “doughy” skin, increased heel pad thickness, Hypertension, Goiter. ➢ Labs: IFG/IGT, +/- elevated Prolactin, Hypogonadism. ➢ Diagnosis: Elevated IGF-1, Abnormal GTT. ➢ In children, gigantism occurs because of accelerated linear growth (growth plates haven’t fused yet)
- 36. Diseases associated with Acromegaly ■ DM ■ Arthritis and carpal tunnel syndrome secondary to hypertrophy of joint cartilage ■ Hypogonadism ■ Sleep Apnea ■ HTN, LVH ■ Colon Polyps
- 42. Prolactin secreting Pituitary Adenoma ➢ Most common Pituitary lesion. ➢ Majority are microprolactinomas, few are macroprolactinomas. ➢ E2 stimulates lactotroph proliferation. ➢ Note: Physiologic elevation of Prolactin is seen in pregnancy. ➢ Idiopathic Prolactinoma: When the etiology is unclear. A subset of these patients may have macroprolactinemia.
- 43. Prolactin secreting Pituitary Adenoma ➢ Prolactin >200ng/ml is consistent with Prolactinoma ➢ Prolactin <50ng/ml is often secondary to physiologic causes. ➢ Prolactin 20-100ng/ml may be secondary to pituitary stalk compression by tumors not actively secreting Prolactin.
- 44. Prolactin secreting Pituitary Adenoma ➢ Clinical Presentation: Signs and Symptoms of hypogonadism (especially amenorrhea and infertility in pre-menopausal women) +/- galactorrhea (especially in women) and gynecomastia (in men) +/- tumor mass effects. ➢ Diagnosis: Elevated Prolactin levels in the presence of Pituitary lesion on imaging and other causes of Hyperprolactinemia ruled out.
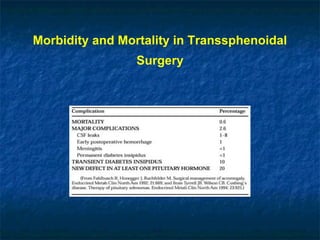
- 47. Morbidity and Mortality in Transsphenoidal Surgery
- 48. Posterior Pituitary and AVP Secretion
- 49. Variables influencing Plasma AVP ➢ Osmotic: Plasma Osmolality (Water balance) ➢ Hemodynamic: Volume and Pressure sensing ➢ Others: Emesis, Hypoglycemia
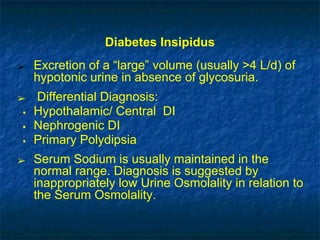
- 50. Diabetes Insipidus ➢ Excretion of a “large” volume (usually >4 L/d) of hypotonic urine in absence of glycosuria. ➢ Differential Diagnosis: ▪ Hypothalamic/ Central DI ▪ Nephrogenic DI ▪ Primary Polydipsia ➢ Serum Sodium is usually maintained in the normal range. Diagnosis is suggested by inappropriately low Urine Osmolality in relation to the Serum Osmolality.
- 51. Causes of Diabetes Insipidus
- 52. Diabetes Insipidus Clinical Features: ➢ Central DI: Relatively abrupt onset of symptoms, Preference for cold liquids, Polyuria and Thirst persisting through the night. ➢ Nephrogenic DI: Lithium, Demeclocycline use, Hypokalemia, Hypercalcemia. ➢ “Psychogenic” Polydipsia: Erratic course, Symptoms exacerbated during stress, Minimal disruption of sleep (lack of nocturia), Underlying psychiatric disease.
- 53. Treatment of DI ➢ Adequate water replacement is essential to avoid metabolic complications. ➢ Central DI: DDAVP (Selective action on antidiuretic V2 receptors, minimal on pressor V1 receptors) ➢ Nephrogenic DI: Thiazide leading to greater proximal tubular reabsorption of glomerular filtrate.
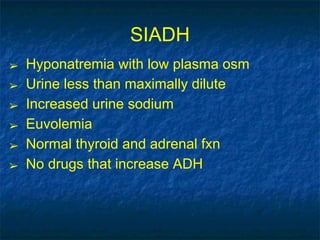
- 54. SIADH ➢ Hyponatremia with low plasma osm ➢ Urine less than maximally dilute ➢ Increased urine sodium ➢ Euvolemia ➢ Normal thyroid and adrenal fxn ➢ No drugs that increase ADH
- 55. Thyroid Disease Sheri Gillis Funderburk, MD
- 56. Thyroid ■ Physiology ■ Hypothyroidism ■ Thyroiditis ■ Hyperthyroidism ■ Thyroid Nodules ■ Thyroid Cancer
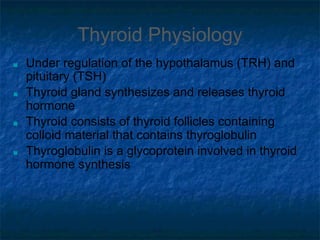
- 57. Thyroid Physiology ■ Under regulation of the hypothalamus (TRH) and pituitary (TSH) ■ Thyroid gland synthesizes and releases thyroid hormone ■ Thyroid consists of thyroid follicles containing colloid material that contains thyroglobulin ■ Thyroglobulin is a glycoprotein involved in thyroid hormone synthesis
- 58. Thyroid Hormone ■ T4 and to lesser extent T3 is released from thyroid gland ■ Majority T3 is produced peripherally by deiodination of T4 ■ Majority T4 and T3 is bound to thyroid binding globulin (TBG) and albumin ■ T4 is bound more tightly than T3 to TBG ■ Only the free hormone is active ■ T3 has higher affinity for thyroid receptor ■ T3 is the more active thyroid hormone
- 60. Thyroid Hormone
- 61. Thyroid ■ T3 uptake ■ Indirect measurement of free T4 ■ Constant x T3 resin Uptake x Total T4 ■ Inverse relationship with TBG (in situations whn TBG is high (pregnancy, OCP use), then T3U will be low. ■ T3U is inversely proportional to the percentage of total T4 that is protein-bound
- 62. Thyroid ■ TBG ■ Increased ■ Congenital ■ Estrogen ■ Contraceptive, replacement, pregnancy ■ Hypothyroidism* ■ Decreased ■ Congenital ■ Androgens ■ Liver failure ■ Nephrotic syndrome ■ Malnutrition ■ Hyperthyroidism* ■ Sick patients ■ glucocorticoids
- 63. Lab values in different scenarios ↑↓↓↓Protein binding ↓↓↓Hypothyroidism ↓↑↑↑ Protein binding ↑↑↑Hyperthryoidism T3RUTotal T3Total T4
- 64. Hypothyroidism ■ Primary ■ Secondary ■ Pituitary disease ■ follow free T4, TSH unreliable ■ Tertiary ■ Hypothalamic disease ■ Sarcoidosis, tumor, radiation ■ Resistance to thyroid hormone ■ Rare ■ Abnormal binding of thyroid hormone to receptor ■ High TSH and T3/T4 +/- signs hypothyroidism
- 65. Hypothyroidism ■ Symptoms ■ Nonspecific ■ Modest weight gain ■ Cold intolerance ■ Constipation ■ Dry skin ■ Fatigue ■ Constipation ■ Menstrual irregularities ■ Muscle aches ■ Signs ■ Dry skin/hair ■ Nonpitting edema ■ Thick lips or tongue ■ Slow relaxation phase of DTR (“hung up reflex”) ■ Thinning lateral aspect of eyebrows
- 67. Primary Hypothyroidism ■ Hashimoto’s ■ Most common cause hypothyroidism ■ Women>men ■ Incidence increases with age ■ Autoimmune destruction of thyroid gland ■ Associated with positive anti-TPO and/or anti-thyroglobulin antibody ■ Slowly progressive ■ May coexist with other autoimmune diseases
- 68. Hashimoto’s ■ Labs ■ High TSH, low Total T4, total T3, T3 resin Uptake, and free T4; positive thyroid peroxidase and/or anti thyroglobulin antibodies ■ We don’t usually measure free T3 ■ Treatment ■ Thyroxine replacement ■ T4 vs T3 ■ Subclinical hypothyroidism ■ Modestly elevated TSH with normal T4/T3 ■ Indications for treatment ■ Hypercholesterolemia ■ Symptoms consistent with hypothyroidism
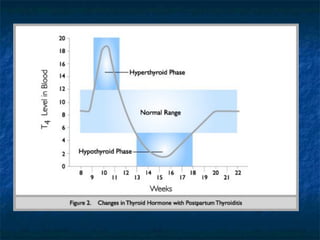
- 70. Post Partum Hypothyroidism ■ Recovery phase ■ Self limiting ■ Can reoccur with future pregnancies ■ Positive Thyroid Peroxidase antibodies associated with increase risk of later developing permanent hypothyroidism
- 71. Primary Hypothyroidism (other) ■ Iatrogenic/Drugs ■ Thyroidectomy ■ Radioablation ■ Anti-thyroid medications ■ Lithium, Amiodarone, Interferon ■ Frequently underlying autoimmune process ■ Iodine deficiency ■ Rare in well-developed countries ■ Dyshormonogenesis ■ Rare ■ Enzymatic defect in biosynthesis ■ Leads to hypothyroidism and goiter
- 72. Myxedema Coma ■ End stage severe longstanding hypothyroidism ■ Endocrinology emergency ■ Elderly ■ Hypothermia, bradycardia, hypotension ■ Predisposing condition ■ Cold, infection, trauma, CNS depressants
- 73. Myxedema Coma ■ Treatment ■ Supportive care ■ correction hypothermia, treat underlying illness, IV fluids with glucose ■ IV thyroid replacement ■ Corticosteroids
- 75. Hypothyroidism ■ Miscellaneous ■ Dosing T4 ■ Elderly vs young ■ Start at 25ug and titrate up ■ 1.5ug/kg body weight ■ Treat TSH within normal range ■ Exception secondary/tertiary hypothyroidism-free T4 upper end of normal ■ Consider R/O adrenal insufficiency ■ Primary vs secondary hypothyroidism
- 76. Hypothyroidism in Pregnancy ■ Thyroid Binding Globulin (TBG) increases with pregnancy ■ Pregnant women with underlying thyroid disease often unable to increase thyroid hormone production ■ Patient given instruction as soon as pregnancy confirmed increase dose by 30% ■ Some evidence hypothyroidism in 1st trimester associated with mental disability in offspring ■ Goal TSH in pregnancy is less than in non-pregnant patients (< 2)
- 77. Differential for thyroiditis: low uptake on scan ■ Infectious ■ Acute (suppurative)-fungal, parasite, bacterial, PCP, rare ■ Subacute: usually viral in origin (granulomatous: de Quervain’s)--tender gland ■ Painless (non post-partum) ■ Amiodarone-Induced ■ Radiation Induced ■ Traumatic ■ Autoimmune: painless ■ Chronic Lymphocytic (Hashimotos) ■ Postpartum
- 78. Subacute Thyroiditis ■ Often history viral illness ■ Neck tenderness ■ During recovery phase transient period hypothyroidism lasting weeks to several months ■ Usually transient ■ Positive antibodies associated with increased risk of developing primary hypothyroidism
- 79. Stages of subacute and postpartum thyroiditis ■ Hyperthyroid phase occurs first, usually in first 3 months after the viral illness or pregnancy and thyroid pain ■ Followed by several weeks of a transitory phase when euthyroidism occurs ■ Followed by a hypothyroid phase for several months ■ Followed by a Recovery phase when the patient returns to euthyroidism
- 81. Subacute Thyroiditis ■ Labs ■ TSH, Total T4 and T3 resin Uptake or free T4, total T3, and thyroid antibodies ■ ESR: high ■ Serum thyroglobulin: high in all forms thyroiditis ■ Imaging ■ Uptake and Scan: low uptake
- 82. Subacute Thyroiditis ■ Treatment ■ Depending on stage ■ Beta blockers ■ Anti inflammatory ■ High dose PTU (decrease peripheral conversion T4→ T3) ■ Steroids ■ Thyroid hormone
- 83. Hyperthyroidism ■ Thyrotoxicosis ■ Excess thyroid hormone from any cause ■ Low TSH +/- elevated T4/T3 ■ Radioactive Iodine uptake and scan helps to differentiate various forms
- 84. Hyperthyroidism ■ Grave’s Disease ■ Subacute Thyroiditis ■ Post-Partum Thyroiditis ■ Lymphocytic thyroiditis ■ Acute Thyroiditis ■ Toxic Adenoma ■ Toxic Multinodular Goiter ■ Iodine induced ■ IV contrast, iodine containing supplements ■ Factitious ■ Excess Beta HCG from molar pregnancy or choriocarcinoma ■ Struma ovarii ■ TSH producing pituitary adenoma ■ Medications ■ Amiodarone, lithium, interferon
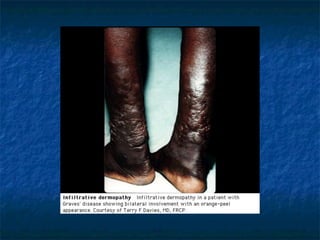
- 85. Hyperthyroidism ■ Symptoms ■ Palpitations ■ Anxiety ■ Weight loss/gain ■ Polyphagia ■ Heat intolerance ■ Increased frequency BM ■ Tremulous ■ Difficulty concentrating ■ Menstrual irregularities ■ Signs ■ Goiter ■ Thyroid bruit* ■ Resting tremor ■ Lid lag ■ Proptosis* ■ Tachycardia/atrial fibrillation ■ Widened pulse pressure ■ Proximal myopathy ■ Neck tenderness ■ Dermopathy* ■ Warm/moist skin
- 86. RAIU: most useful test in the differentiatal dx of thyrotoxicosis ■ High uptake ■ Graves: diffuse pattern ■ Toxic Multinodular Goiter: irregular patern ■ Solitary Toxic Adenoma: increased in one area of thyroid ■ Low Uptake ■ Factitious: low thyroglobulin levels ■ Iodine-Induced ■ Thyroiditis: have high thyroglobulin levels; may have high ESR or antibodies, depending on cause
- 87. Grave’s Disease ■ Most common cause hyperthyroidism (60-70%) ■ Autoimmune activation TSH receptor ■ Thyroid Stimulating Immunoglobulin ■ Familial ■ Women > Men ■ Associated with other autoimmune diseases ■ Vitiligo, Pernicious Anemia, Myasthenia Gravis, Addison’s disease, TIDM ■ Anti-TPO and Anti-Thyroglobulin antibodies may also be present ■ May have positive Thyroid stimulating immunoglobulins and/or positive Thyroid receptor antibodies
- 88. Grave’s Disease ■ Triad ■ Thyroid bruit, dermopathy, proptosis are all pathognomonic ■ Labs ■ Suppressed TSH, elevated T4 and/or T3, increased T3 uptake ■ Imaging ■ Uptake and scan ■ Increased, diffuse uptake
- 93. Grave’s Disease: Treatment ■ Anti-thyroid medications ■ PTU ■ Inhibits synthesis thyroid hormone ■ Decreases peripheral conversion T4 → T3 ■ Does not block release preformed thyroid hormone ■ Side effects ■ Agranulocytosis, hepatitis, urticaria ■ 18-24 months treatment to decrease chance of relapse ■ Preferred pretreatment in surgery
- 94. Grave’s Disease: Treatment ■ Anti-thyroid medication ■ Methimazole ■ Inhibits synthesis only ■ Preferred treatment prior to RAI ■ Same side effects as PTU ■ Cross reactivity ■ Beta Blocker ■ Symptomatic relief ■ Decrease peripheral conversion T4→T3
- 95. Grave’s Disease ■ Treatment ■ Radioactive iodine ■ Exacerbation of hyperthyroidism and eye disease ■ Pretreatment drug of choice is methimazole (hold 5-7 days prior to RAI) ■ Hypothyroidism wanted/potential side effect ■ Iodine: used in severe thyrotoxicosis or storm ■ Blocks release thyroid hormone ■ Wolf Chaikoff Effect (Escape) ■ Surgery ■ Rarely used ■ Pretreatment indicated with PTU/Iodine ■ Major complications are hypothyroidism, hypoparathyroidism, damage to recurrent laryngeal nerve
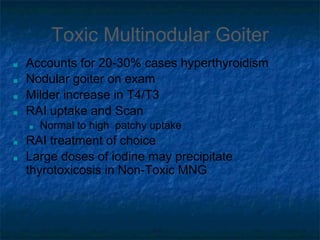
- 97. Toxic Multinodular Goiter ■ Accounts for 20-30% cases hyperthyroidism ■ Nodular goiter on exam ■ Milder increase in T4/T3 ■ RAI uptake and Scan ■ Normal to high patchy uptake ■ RAI treatment of choice ■ Large doses of iodine may precipitate thyrotoxicosis in Non-Toxic MNG
- 98. Toxic Adenoma ■ AKA Plummer’s Disease ■ 3-5% toxic adenoma ■ Caused by solitary hyperfunctioning nodule ■ Nodule may be palpable on exam ■ Low TSH with elevated T4 and/or T3 ■ RAI uptake and scan ■ Normal to high uptake ■ Solitary hot nodule ■ Remainder glands suppressed ■ RAI treatment of choice
- 99. Hyperthyroidism due to Iodine ■ Iodine Induced ■ Jod Basedow ■ Underlying thyroid pathology ■ Self limiting ■ History IV contrast obtained within several weeks of onset or pt is on Amiodarone ■ Low TSH, elevated T4, typically normal T3 ■ Low RAI uptake ■ Pretreatment ■ Symptomatic relief
- 100. Hyperthyroidism due to Meds ■ Medications ■ Lithium ■ Amiodarone ■ Type I vs Type II ■ Increased thyroid hormone production vs destructive thyroiditis ■ Often difficult to differentiate ■ Treatment (depending on Type I vs II) ■ Discontinue amiodarone ■ Anti-thyroid medications (Type 1), steroids (type II), beta-blocker, surgery
- 101. Hyperthyroidism: other causes ■ Factitious ■ Low TSH ■ Low RAI uptake ■ Decreased thyroglobulin ■ Elevated in thyroiditis ■ Molar Pregnancy and Choriocarcinoma ■ Stimulatory effect of hCG, which structurally resembles TSH ■ Struma Ovarii ■ Ectopic thyroid tissue ■ RAI uptake and scan ■ Uptake in pelvis and no uptake in neck ■ TSH producing pituitary adenomas ■ Extremely rare ■ Suspect with elevated T4/T3 and normal/high TSH
- 102. Apathetic Hyperthyroidism ■ Seen in the elderly ■ Thyrotoxicosis without the adrenergic manifestations ■ Appear depressed, often diagnosed with mxyedema ■ Weight loss, atrial fibrillation, CHF, muscle weakness ■ Often Toxic MNG underlying disorder
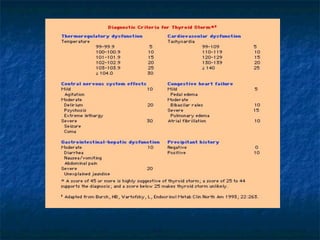
- 104. Hyperthyroidism Emergency ■ Thyroid Storm ■ Decompensated form of severe thyrotoxicosis ■ Uncommon, life threatening condition ■ Precipitating event ■ ex. Infection, trauma, surgery, DKA ■ Fever, tachycardia, neurological abnormalities, hypertension followed by cardiovascular collapse ■ Treatment ■ Anti-thyroid medications, iodine, steroids, B-blockers, control hyperthermia
- 106. Sick Euthyroid Syndrome ■ Seen in critically ill patients ■ Low TSH, free T4, and T3 ■ Elevated Reverse T3* ■ No treatment
- 108. Thyroid Nodule ■ Extremely common ■ Approximately 50% patients over 65 will have at least 1 thyroid nodule on US ■ Incidentaloma
- 110. Thyroid Nodules ■ Benign ■ Non toxic Goiter ■ Not associated with inflammation or neoplastic process ■ Causes ■ Majority unknown ■ Iodine deficiency ■ Iodine excess ■ Dyshormonogenesis ■ Radiation ■ Cyst ■ Adenoma ■ Thyroiditis
- 111. Thyroid Nodule ■ Carcinoma ■ Papillary ■ Follicular ■ Anaplastic ■ Medullary ■ Lymphoma ■ Metastatic
- 113. Thyroid Cancer ■ Treatment ■ Surgery ■ Radioactive iodine to ablate any remnant thyroid tissue ■ Thyroid replacement after surgery and RAI ■ Suppression of TSH without overt hyperthyroidism ■ Follow Up ■ Physical Exam ■ TFTs including Thyroglobulin ■ Thyrogen whole body scan ■ Ultrasound