Audit Training ©
- 1. Clinical Audit Workshop May 2011
- 2. Today’s schedule Housekeeping
- 3. Objectives for the session
- 7. Designing and running an audit
- 8. Exercise
- 9. Action plans and change
- 11. Ground Rules First namesPhones off (or on silent) please You can ask questions at any timeDon’t need to put your hand up
- 12. Objectives By the end participants should:1. Understand the principles of clinical audit.2. Have some basic clinical audit design skills.
- 13. Introductions In pairs – introduce your partner with Their name and role Where they live/work Why they’re here todayOne thing they’re very proud of
- 14. Three dimensions of healthcare qualityStructure- resources, physical settings. Process- How knowledge is used (technical), Relationships(the interpersonal). 3. Outcome - the change in service user’s health. (Avedis Donabedian,1966)
- 15. Why do we look at healthcare quality? To improve how we practice : provide better careTo improve how we deliver care: provide a better service
- 16. Task - What is ‘Clinical Audit’? In your groups – write a definition of ‘clinical audit’
- 17. Nominate one person to feed back
- 18. You have 3 minutes What is Clinical Audit?The ‘official’ definition is“A quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change” National Institute for Health and Clinical Excellence, 2002
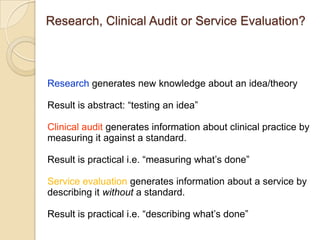
- 19. Research, Clinical Audit or Service Evaluation? Research generates new knowledge about an idea/theoryResult is abstract: “testing an idea” Clinical audit generates information about clinical practice bymeasuring it against a standard. Result is practical i.e. “measuring what’s done”Service evaluation generates information about a service by describing it without a standard. Result is practical i.e. “describing what’s done”
- 20. The Clinical Audit CycleSelect Topic Set Standard/criteriaRe-audit Introduce change Collect dataAnalyse and derive action points
- 21. Task - The Clinical Audit Race2 Teams. 15 cards show stages of the audit cycle. Put them in order them on the floor - show the audit cycle Task is over when the first team declares the (right) answer.
- 23. The Clinical Audit CycleSelect Topic Set Standard/criteriaRe-audit Introduce change Collect dataAnalyse and derive action points
- 24. Four key things for your projectAimObjectivesAudit standard Audit criteria
- 25. Writing an Aim and ObjectivesOne aim: To ensure procedure X is completed on admission to ward Y Objectives should deliver the aim:Develop a clinical audit of procedure XUse this to measure to what extent X is done on ward YWrite and implement action plan to ensure X is always done Conduct re-audit of X in 2012
- 26. Measurement of practice against a standardAn audit standard is a statement of the level of care/practice expected. All service users have a STORM suicide and self injury assessment within 12 hours of their admission to an adult ward. It should be as unambiguous as possible: “All service users are assessed for potential self harm on admission to a hospital” What kind of assessment, where and when?
- 27. Each audit standard is measured with criteria1. What That is the exact process/outcome 2. How much75, 95 or 100% of the time?3. What not Exceptions and why they are For quantitative audit, criteria will usually beNumerical: Times, Doses, Scores Categories: Yes/No/Don’t know
- 28. Example criteria All service users have a STORM suicide and self injury assessment within 12 hours of their admission to an adult ward.Audit Criteria: A complete STORM suicide and self injury assessment is done within 12 hours of admission This should occur for 100% of eligible admissions to the adult wardsExceptions – any service user discharged within 12 hours of admission any service user who has was admitted to another ward and has been inpatient for at least 12 hours Data collected could be either categorical (Yes or No) or numerical (hrs to completion)
- 29. Methods of Data CollectionQuantitative Data collection tool/proforma (or a spreadsheet)Numerical data: results, dates, dosages, times. Qualitative Questionnaire, interview, focus groups. Experiences, attitudes, beliefs, meanings, behaviours.Take care about what you’re asking - ethics
- 30. Designing data collection Keep it simple Paper audits - don’t exceed one sheet (2 sides) if possible Or collect it directly onto a spreadsheet or we will provide a SNAP web survey tool Keep a list of all eligible and all reviewed cases Minimise the amount of personal information you collectMaintain the 6 Caldicott Principles Ask us for help with design
- 31. 23
- 32. Questionnaires Postal, web or e-mailShort and simple as possible. Clear instructions for respondents. Question types - open/closed, scalar. Least intrusive questions first Layout – clear headings, minimum 10pt fontPlain English, avoid clinical/NHS jargonPilot
- 33. Interviews Structured, semi structured orunstructuredOne to one or group Face to face or ‘phoneEthics may be an issue – what are you asking? Need a detailed record of responses Rich data but time/effort intensive Design and execution is skilled task so pleaseask for advice.
- 34. Pilot StudiesDo a small pilot study of 2- 3 cases before the main project :It will:Test your criteriaShow up any practical problems with data collection
- 35. SamplingAn appropriate sample is the number of cases needed to ensure your audit is representative of practice. Random– choosing xnumbers from a list Time Period – all cases from 1 week or 6 months.Cluster – all cases from one team/ward/locality. Rapid Cycle – small numbers (20 - 50), repeated quickly
- 36. Prospective or retrospective? Prospective(collecting data on practice as it happens) avoids bias from incomplete records but: People may alter their behaviour if their being watched (known as The Hawthorne Effect).Retrospective (collecting data on previous practice) is often quicker and easier but:Open to bias from the quality/completeness of the records.
- 37. Is my audit design any good?Is it valid?Validity the extent to which the audit measures what it is supposed to. Valid audit measures things accurately. Is it reliable?Reliability means you’d get the same result if the audit was repeated on the same sample. Reliable audit would get the same result.
- 38. Re-audit Once your audit is complete you should schedule a re-audit to consolidate any action. This should be part of your action plan and be fairly prompt, usually within 3-6 months.Other prompts for a re-audit might include: Your original audit/action plan hasn’t worked
- 39. Significant alterations to your team/service
- 40. Significant staff turnover in your team/service
- 41. New standards publishedProject ChecklistChoose your topicBuild your 4 elements – Aim, Objectives, Standard, CriteriaRegister it with the Audit and Research DepartmentCollect the dataAnalyse the data and reportImplement any action pointsRe-audit when appropriate
- 42. ExerciseScenario: You are concerned patients with bi-polar disorder are not having their physical health checks. You want to ensure they receive physical health checks as detailed in NICE Clinical Guideline Number 38. In your group, write the following An audit aim and objectives to support it.Audit criteria and any exceptions.Methodology – qualitative or quantitative data, data source(s), sampling strategy,pro/retrospective. Feedback in 25 minutes.
- 43. Thinking about changeWhat year did you get your first mobile phone? Other peopleAction plans
- 44. Data analysis and presentationAnalysing and presenting findings is the first step of any action/change process. When you do this keep the following in mind:Your results should make sense to the intended audience. Avoid elaborate data analysis – this won’t make your findings any more credible Conclusions and actions should reflect and be proportionate to your findings. Active dissemination/marketing of the results/report/action plan is essential
- 45. Successfully changing what healthcare professionals do is difficult and requires both skill and commitment. Before writing action plans it’s worth considering what any change in practice actually entails: Carl Lewin (c1947) used the following model for change: This may help you think about how to plan both your project and any action needed from it. UnfreezeChange Re-freeze
- 46. Healthcare professionals are by definition skilled, knowledgeable and highly autonomous people who work in organisations composed of their peers, other professionals and service users. Responses to any proposed change are personal. Some things that inform how you or I might respond to change are: Awareness and knowledge – Do they know what you’re proposing and why? Motivation – What would motivate people to change? Acceptance and beliefs – Does this fit with their values/beliefs? Skills/Knowledge – Can they actually do what needs to be done? Practicalities – Do they have the resources to change? External Environment – Are there other priorities/competing demands?
- 47. Adaptation of InnovationE. Rogers c1967
- 48. Mobile phones – When did you get one? 19912011200020051995
- 49. Action PlansAction plans are widely used in the NHS. Some suggestions for writing action point/plans include: Consult as widely as possible before writing your action plan. Consider the other people involved i.e. whose got an interest & what is that interest? Consider the resource implications – can the Trust afford your proposed actions? Scale is significant – bigger changes may be harder to implement Dissemination – your Business Unit, the A & R Committee and who/where else?Review - Are the action points really feasible and implementable?
- 51. Clinical Audit Resourceshttp://www.rcpsych.ac.uk/pdf/clinauditChap1.pdfhttp://www.nice.org.uk/usingguidance/implementationtools/auditadvice/audit_advice.jsphttp://www.hqip.org.uk/clinical-audit-handbook/http://www.hqip.org.uk/clinical-audit-resources-3/http://www.wales.nhs.uk/sites3/Documents/501/Practical_Clinical_Audit_Handbook_v1_1.pdfStatistics resources - random numbers http://www.randomizer.org/form.htm -http://www.graphpad.com/quickcalcs/index.cfmChange and innovation in the NHS http://www.institute.nhs.uk/option,com_quality_and_service_improvement_tools/Itemid,5015.htmlhttp://www.sdo.nihr.ac.uk/managingchange.htmlhttp://www.tin.nhs.uk/leadership/change-management-workbookshttp://www.nice.org.uk/media/D33/8D/Howtochangepractice1.pdf
- 52. Summation of today Definition of clinical audit.The clinical audit cycle.Four things you need to build an audit Design issues/skills.Written a simple clinical audit.Action plans and change
- 53. Suggested Personal Development Plan linkagesCore Dimension 2: Personal and People DevelopmentLevels 1 Contribute to own personal development 2 Develop own skills and knowledge and provide information to others to help their development 3 Develop oneself and contribute to the development of others Core Dimension 4: Service Improvement Levels 1 Make changes in own practice and offer suggestions for improving services 2 Contribute to the improvement of services Core Dimension 5: Quality Levels 1 Maintain the quality of own work2 Maintain quality in own work and encourage others to do so3 Contribute to improving quality4 Develop a culture that improves qualityIK2: Information collection and analysis Level 2 Gather, analyse and report a limited range of information IK3: Knowledge and information resources Level 1 Access, appraise and apply knowledge and information G2: Development and Innovation Level 1 Appraise, concepts, models, methods, practices, products and equipment developed by others.
- 54. Please tell the group one thing that you’ve learnt todayThank you