Australianhighcommission
- 1. + Introduction to Mental Health Australian High Commission – Feb 2016 Welcome
- 2. + Outline of PresentationOutline of Presentation What is mental health? Facts & Figures Who experiences mental distress? Some common mental health conditions A Case Study. Helpful and Unhelpful Responses. Q&A
- 4. + Filmmaker
- 5. + Trainer
- 6. + Gained First Class Honours at University
- 7. + But also…But also… I have a serious mental health condition and have been a service user for over 30 years.
- 8. + What is Mental Health? “Mental health is defined as a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.” (World Health Organisation) “A person’s condition with regard to their psychological and emotional well-being” (Dictionary Definition)
- 9. + Who has mental healthWho has mental health? EVERYBODY!
- 10. +
- 11. + 5 a day – mental health5 a day – mental health Connect Developing relationships with family, friends, colleagues and neighbours will enrich your life and bring you support Be active Sports, hobbies such as gardening or dancing, or just a daily stroll will make you feel good and maintain mobility and fitness Be curious Noting the beauty of everyday moments as well as the unusual and reflecting on them helps you to appreciate what matters to you Learn Fixing a bike, learning an instrument, cooking – the challenge and satisfaction brings fun and confidence Give Helping friends and strangers links your happiness to a wider community and is very rewarding.
- 12. + 1 in 4 experiences mental distress 1 in 200 goes to hospital. Mixed anxiety and depression most common experience (9-12%) UK has one of the highest rates of self-harm in Europe. 2% have phobias that need treatment. 2-3% have diagnosed OCD 87% of people with a mental health problem will have experienced some form of discrimination. Some Facts and Figures aboutSome Facts and Figures about Mental HealthMental Health
- 13. + Facts & FiguresFacts & Figures People who have mental health problems are more likely to: • Experience isolation / exclusion: 9 out of 10 people with mental health problems do not go out or apply for jobs due to the stigma • Receive dismissive or disrespectful treatment They feel most discriminated against by their family (36%), followed by their employers (35%), neighbours (31%) and friends (25%) (survey by Rethink 2008) • Not have a valued role or job More than half of all employers asked would not hire someone with a known mental disorder (survey by The Shaw Trust 2009) • Experience poverty and social deprivation (More than 50% of people with mental health problems have poor social contact, as defined by the Oslo Social Support Scale, compared with 6% of the general population)
- 14. + Who experiences mental distress?
- 15. + What is Normal?What is Normal? Telepathy 45% Ability to predict the future 45% Hypnotism 42% Life after death 39% Faith healing 39% Ghosts 31% Alien abduction 70% U.F.O‘s 35% A Gallup survey (1995) found the following rates of belief: •Studies find it hard to differentiate between ‘normal’ and ‘deluded’ people
- 16. +
- 17. +
- 18. + Some Mental Health CategoriesSome Mental Health Categories Mood (affective disorders) Depression Bi-polar affective disorder Eating Disorders Anorexia nervosa Bulimia nervosa Personality Disorders Psychotic Disorders Schizophrenia
- 19. + Some Facts and Figures aboutSome Facts and Figures about Mental HealthMental Health 1 in a 100 have the diagnosis of schizophrenia/psy chosis 1 in a 100 have the diagnosis of Bipolar Disorder 1 in 10 have the diagnosis of Personality Disorder
- 20. + DepressionDepression •Feelings of sadness & hopelessness •Losing interest in things •Feeling numb •Tiredness •Sleep Problems •Work & relationships affected •Poor concentration •Negative self-view •Social withdrawal
- 21. + Depression (cont’d)Depression (cont’d) ‘That’s the thing about depression: a human being can survive almost anything, as long as s/he sees the end in sight. But depression is so insidious and it compounds daily, that it’s impossible to ever see the end. The fog is like a cageThe fog is like a cage without a key.’without a key.’ Elizabeth Wurtzel, Prozac Nation “Depression turned my body, mind and soul into concrete; procrastination turned my heart into a block of dirty ice.” Dolly Sen, The World is Full of Laughter.
- 22. + Some ways people look afterSome ways people look after depressiondepression Meditation Exercise Therapy or Counselling Arts/Creativity Medication Identifying Triggers Relaxation Exercises Social support/Peer Support Challenging negative thinking Resolving Issues
- 23. + AnxietyAnxiety
- 24. + AnxietyAnxiety In 2013, there were 8.2 million cases of anxiety in the UK.
- 25. + Ways to help anxietyWays to help anxiety Self Care talking to someone you trust breathing exercises shifting your focus listening to music reassuring thoughts physical exercise keeping a diary eating a healthy diet complementary therapies joining a support group Treatments Talking therapies CBT Medication Applied Relaxation Therapy Mindfullness
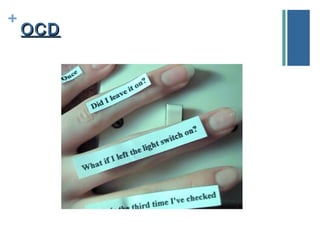
- 27. + OCDOCD
- 28. + What is OCD?What is OCD? OCD causes severe anxiety in those affected. OCD involves both obsessions and compulsions that take a lot of time and get in the way of important activities the person values.
- 30. +
- 32. + What is an eating disorder?What is an eating disorder? Eating disorders are a range of conditions that can affect someone physically, psychologically and socially. They include anorexia, bulimia and binge eating disorder. Over 725,000 men and women in the UK are affected by eating disorders. Young women are most likely to develop an eating disorder, particularly those aged 12 to 20, but older women and men of all ages can also have an eating disorder. Children as young as seven can develop anorexia and there is a greater proportion of boys in this younger age group. Eating disorders claim more lives than any other mental health condition – one in will die prematurely
- 33. + Eating Disorders – waysEating Disorders – ways forwardforward Psychological Treatment Self help/ Peer Support /Support Groups Family Therapy Nutritional Counselling Finding other ways to cope with difficult emotion Self-image work Arts & Creativity
- 34. + Eating Disorders ResourcesEating Disorders Resources https://www.b-eat.co.uk/
- 35. + Does not mean a split personality To get the diagnosis there has to be both the presence of delusion and hallucination. Schizophrenia and PsychosisSchizophrenia and Psychosis
- 36. + PsychosisPsychosis Decreased motivation Lack of emotion Poor concentration Inability to experience pleasure in things you once enjoyed e.g. golf/socialising Avoiding social situations Reduced speech Neglecting personal appearance
- 37. + PsychosisPsychosis Hallucinations: seeing, hearing or smelling things that are not there e.g. auditory hallucination of voices (which the sufferer may respond to) Delusions: firmly held beliefs which are untrue i.e. you are Jesus or a member of royalty/you are being controlled by an outside force. Thought disorder: confused thoughts or speech which do not make any sense.
- 38. + Is hearing voices always a sign of a psychiatric condition?
- 39. + Studies have found that between four and 10 per cent of people across the world hear voices. Between 70 and 90 cent of people who hear voices do so following traumatic events. Voices can be male, female, without gender, child, adult, human or non-human. People may hear one voice or many. Some people report hearing hundreds, although in almost all reported cases, one dominates above the others . Voices can be experienced in the head, in the ears, outside the head, in some other part of the body, or in the environment. Voices often reflect important aspects of the hearer’s emotional state – emotions that are often unexpressed by the hearer.
- 40. + Hearing Voices - exerciseHearing Voices - exercise
- 43. + BipolarBipolar Mania (cont’d)Mania (cont’d) Thinking they possess all abilities and powers High energy on no sleep Easily distracted, cannot concentrate Impaired judgment Wildly impulsive Reckless, despite the consequences Hallucinations Totally uninhibited Giving away cherished valuables Unending pursuit of pleasures/substance abuse
- 44. + BipolarBipolar Depression (cont’d)Depression (cont’d) Irritable Cannot experience pleasure Loss of interests Appetite and weight changes Sleep – restless, excessive, insomnia Lack of concentration Memory Problems
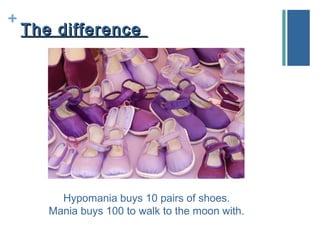
- 45. + Bipolar DisorderBipolar Disorder The difference between bipolar 1 and Bipolar 2 is severity of the ‘high’ and ‘low’ experiences. Bipolar 1 is more severe, the person experiences mania/severe depression. Bipolar 2 means the person experiences hypomania. The difference between the two is not clear cut. If the person is at risk from harm, or has developed psychosis, this is seen as mania. Rapid Cycling: Going from high to low, or vice versa, without periods of normality.
- 46. + The differenceThe difference Hypomania buys 10 pairs of shoes. Mania buys 100 to walk to the moon with.
- 47. + Bipolar Disorder - ResourcesBipolar Disorder - Resources http://www.bipolaruk.org.uk/
- 48. + DisclosureDisclosure Before support can be offered, the student has to disclose, but many students with mental health difficulties don’t. The main reason is fear of discrimination.
- 49. + Some FearsSome Fears Being teased or harassed by others Being assumed to be a less productive student Having fewer opportunities Being treated as more vulnerable than others or as having everything (anger, excitement, time off sick, or a grievance) associated with your mental health problem. Having to work harder to gain the same respect. Thought of as being dangerous
- 50. + You shouldn’t do it…You shouldn’t do it…
- 51. +
- 52. + Case Study - BipolarCase Study - Bipolar Male, in mid 20s, very recently diagnosed, has not had his condition for more than a year, no support in place. One day started talking over colleagues, being inappropriate, giving away his money, tells people he is God. Takes a break, gets better, but does not want to return to job because of embarrassment. What do you do?
- 53. + Case Study One - PsychosisCase Study One - Psychosis Female – mature student, discloses her mental health When well is a good student, punctual and involved, excellent attendance and high achiever. When her psychosis is present: hears loud and negative voices, becomes withdrawn, paranoid, stops attending classes Misses assignments. Becomes suicidal. What do you do?
- 54. + Some Responses to Self-HarmSome Responses to Self-Harm If injury is severe, go to A&E ❏ refraining from telling young person to stop, as this can make things worse. ❏ explaining your role and the limits of your confidentiality; ❏ giving information/education about self-harm and causes in a straightforward and matter of fact manner ❏ being aware that the person may be feeling guilty and ashamed; ❏ being aware of the stigma associated with self-harm; ❏ being non-judgmental; ❏ treating young person with respect; ❏ listening empathetically with a view to joint problem solving; ❏ providing reassurance that problems can be solved.
- 55. + What the organisation can doWhat the organisation can do Have a strong mental health policy Have good support services develop a culture where everyone is treated with respect and dignity and issues such as bullying and harassment are not tolerated develop a culture where open and honest communication is encouraged and support and mutual respect are the norm. Encouraging an ethos where staff know that it is OK to talk about mental health and that it is safe to disclose their own mental health conditions.
- 56. + Helpful ResponsesHelpful Responses Try to remain calm. Think about body language. Be as gentle and non-critical as you can. Do not make judgments. What they are feeling is their unique experience and you should refrain from giving your opinions or views Let the person know that you want to help Listen quietly and reflectively to what they have to say - let them express their worries and tell you how they see life.
- 57. + Helpful ResponsesHelpful Responses Ask how you can help? If the person is in delusion or denial, don’t try to argue them out of it. But don’t agree with them either. Example: “I am rotting, can you smell it? I can smell it.” One possible response: “I can’t smell anything. I don’t think you are rotting. But I can see you are upset by that. Do you want to talk to someone about it? Try and come up with ways with the person to reduce fear.
- 58. + Fear…Fear… Think about these experiences as fear free What is paranoia without fear? What are voices without fear? What is anxiety without fear? Can you have a panic attack without fear?
- 59. + Helpful ResponsesHelpful Responses Make meetings/spaces/emails feel safe. Warmness/lack of harshness. Example: Dolly, you didn’t come in last week. You must come in, otherwise this be reported and you might lose your place on the course. Could have been phrased: Dolly, how you doing? I noticed you didn’t come in last week. Are things ok? I hear you struggling with things. Do you want to come in for an informal, relaxed chat, so we can talk through any difficulties you may have, and see how we can work this through together. You are missed. Take care
- 60. + Helpful ResponsesHelpful Responses Be a bit of a hog Hopeful Honest Open Gentle
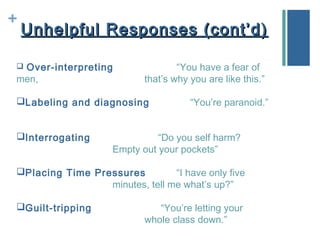
- 61. + Unhelpful Responses (cont’d)Unhelpful Responses (cont’d) Over-interpreting “You have a fear of men, that’s why you are like this.” Labeling and diagnosing “You’re paranoid.” Interrogating “Do you self harm? Empty out your pockets” Placing Time Pressures “I have only five minutes, tell me what’s up?” Guilt-tripping “You’re letting your whole class down.”
- 62. + Unhelpful ResponsesUnhelpful Responses Blaming “It’s all your own fault.” Getting Aggressive “Can’t you ever do anything right?” Moralising “This is just a sign of weakness, you need to do this…” Advising without trust and validation Not accepting another’s feelings “I don’t know why you are so depressed.”
- 64. + Thank you for your time! Dolly Sen dollysen70@hotmail.com http://www.dollysentraining.com
Editor's Notes
- .
- Source: Foresight report, the government think-tank. Its Mental Capital and Wellbeing report, which was compiled by more than 400 scientists, proposes a campaign modelled on the nutrition initiative, to encourage behaviour that will make people feel better about themselves.
- Stimga Shout Survey (Time to Change – source)
- Everyone can, no one is immune, affects all ages, backgrounds, ethnicities, cultures. Mental health is not black & white. People who have mh conditions are not the opposite to those who don’t have a label. Think of it as a spectrum. You can use any condition. 20% of adolescents may experience a mental health problem in any given year.1 50% of mental health problems are established by age 14 and 75% by age 24.2 10% of children and young people (aged 5-16 years) have a clinically diagnosable mental problem3, yet 70% of children and adolescents who experience mental health problems have not had appropriate interventions at a sufficiently early age.4 - See more at: https://www.mentalhealth.org.uk/statistics/mental-health-statistics-children-and-young-people#sthash.pzDmNvRT.dpuf A fifth of people over 65 experience depression. There are 44 million people with dementia worldwide. Loneliness is the biggest killer of older people.
- Other kinds of disorders: developmental disorders, conduct disorders, organic disorders, stress disorders, brain injuries.
- Won’t talk about causes very much Psychiatry isn’t pure science.
- Talk about my experience on ocd ward.
- Ask: do people recover from schizophrenia? 20% complete recovery, 40% some form of significant recovery. Is it a life-long condition? Other symptoms – thought disorder, flat emotion, paranoia
- What are delusions?
- Give my bus example.
- Also add what’s it like
- Wellness Recovery Action Plan
- Why are they not helpful