Bacterial infections of the urinary tract
- 1. Bacterial Infections of the Urinary Tract MEHER RIZVI Associate Professor Department of Microbiology & Immunology
- 2. Objectives Discuss the clinical syndromes of Urinary Tract Infection (UTI) Enlist the bacteria most commonly involved in UTI Describe the pathogenesis of UTI Discuss the general features and virulence mechanisms of bacterial pathogens causing UTI viz: Escherichia coli, Pseudomonas aeruginosa, Staphylococcus saprophyticus Discuss various aspects of laboratory diagnosis of UTI viz: collection of a proper specimen, its processing and interpretation of results
- 4. Clinical syndromes • Cystitis • Pyelonephritis • Urosepsis • Urethritis Dysuria, frequency, urgency, suprapubic pain, hematuria Fever, flank pain, chills, nausea/vomiting Above symptoms, shock Discharge, itching, dysuria, frequency: Suspect STDs
- 5. Epidemiology of UTI Community acquired UTI Hospital acquired UTI: Most common health care associated infection (CAUTI) Worldwide: 150 million cases/ year Simple Complicated
- 6. Pyelonephritis 10%Cystitis 90% Complicated UTI Calculi/stones 2%
- 8. Host protective factors Normal flora in urethra Flushing mechanism of urine Acid pH of urine (4.6-6) ↑ Urea concentration ↑ Osmolality Acid vaginal pH (3.5-4.5) Systemic/local antibodies Inflammatory response mounted in bladder Flushing mechanism of urine
- 9. Host Risk factors Complicated UTI: If anatomic/ functional/ metabolic abnormalities of urinary tract present Pregnancy ( Incomplete emptying) Residual urine in bladder: Stone, Benign hypertrophy of prostate (BPH Men > 50 years ) Diabetes (Glucose in urine facilitates bacterial growth) Post-menopausal women ( Estrogen deficiency leads to ↑ vaginal pH Neurogenic bladder (Incomplete emptying) Renal failure/ renal transplantation In dwelling catheter (Biofilm production)- Most common cause of HAI termed as CAUTI Simple uncomplicated UTI Female gender (short and broad urethra) Infant boys (vesicular-ureteric reflux) Genetic susceptibility
- 10. • Both Gram-negative and Gram-positive bacteria cause UTI • Uropathogenic Escherichia coli (UPEC) cause majority of both uncomplicated and complicated UTIs • Escherichia coli • Klebsiella pneumoniae • Staphylococcus saprophyticus • Enterococcus faecalis • Group B Streptococcus • Proteus mirabilis • Pseudomonas aeruginosa • Staphylococcus aureus • Candida spp. • Escherichia coli • Enterococcus faecalis • Klebsiella pneumoniae • Candida spp • Staphylococcus aureus • Pseudomonas aeruginosa • Proteus mirabilis • Group B Streptococcus Uncomplicated UTI Complicated UTI Etiology
- 11. Prevalence of bacteria in UTI
- 12. Bacterial virulence factors Uropathogenic Escherichia coli • Somatic O antigens: (O2,O4,O6) • Capsule: pyelonephritis (inhibits phagocytosis) • P fimbriae: initiates attachment to uro- epithelial cells • Flagella: Motility allows the bacteria to ascend up to the bladder/ureter against urine flow • Haemolysins: In pyelonephritis damage renal epithelium • Cytotoxic necrotizing factor: Cytotoxic to bladder and renal epithelium Other Uropathogenic bacteria • Pili: for adherence • Capsule: Klebsiella pneumoniae • Haemolysin: Proteus mirabilis • Biofilm: Pseudomonas aeruginosa • Urease: Proteus mirabilis, S. saprophyticus, Klebsiella pneumonia • Protease:Pseudomonas aeruginosa • Proteus mirabilis: Urease enzyme splits urea to ammonia: → Urine is alkalinized: Damages renal epithelium → Complicated UTI Alkaline pH increases precipitation of calcium and phosphates → Stone/Calculi formation → Obstruction→Recurrent/Complicated UTI
- 13. Ascending and Descending UTI
- 14. Etiology Descending UTI S. aureus M. Tuberculosis Salmonella typhi Candida albicans Etiology Ascending UTI Escherichia coli Klebsiella pneumoniae Proteus mirabilis Ascending UTI Descending/ hematogenous UTI Source of uropathogens: Enteric bacteria from GI tract Source of pathogens: Blood stream
- 15. Complicated UTI- catheterized patient (CAUTI)
- 16. • Most common route • More common in women due to: • Short and wide urethra • Proximity to perineum. • If left untreated, can ascend to the ureters (esp. if vesiculo-reflex present) and to renal pelvis and renal parenchyma Ascending UTI Urethral commensals can ascend easily
- 17. • Haematogenous seeding less frequent than ascending infection • Common etiology: Bacteremia due to • Staphylococcus aureus • Salmonella typhi • Mycobacterium tuberculosis Descending UTI Hospital acquired UTI • Associated with lower urinary tract instrumentation • Catheterization • Cystoscopy
- 18. UTI occurs more often in females than males Escherichia coli is the most common cause of UTI in all settings The proportion of UTI caused by other species increases in recurrent or hospital acquired UTI KEY POINTS
- 19. Laboratory Diagnosis Early morning urine sample is best as has highest concentration of bacteria. Or Collect urine after 4 hrs of prior voiding ( To prevent false negative findings) Protocol: Collection of urine Transport to laboratory Screening tests Culture Antimicrobial sensitivity Sterile, wide mouthed screw capped container All samples for Culture & sensitivity (C/s) should be collected before instituting antimicrobial therapy
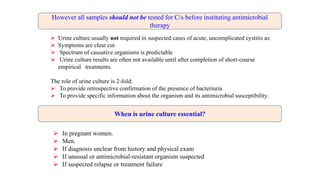
- 20. In pregnant women. Men. If diagnosis unclear from history and physical exam If unusual or antimicrobial-resistant organism suspected If suspected relapse or treatment failure Urine culture usually not required in suspected cases of acute, uncomplicated cystitis as: Symptoms are clear cut Spectrum of causative organisms is predictable Urine culture results are often not available until after completion of short-course empirical treatments. The role of urine culture is 2-fold: To provide retrospective confirmation of the presence of bacteriuria To provide specific information about the organism and its antimicrobial susceptibility. However all samples should not be tested for C/s before instituting antimicrobial therapy When is urine culture essential?
- 21. Collection of sample • Adult patient: Instructions Infants: Instructions to care giver • Wash external genitalia (Glans and labia) with soap and water. Do not use antiseptics! • Collect mid stream urine sample in sterile wide mouthed, screw capped container • Rationale: • First voided urine washes off commensals from distal urethra. • Midstream urine sample represents true bladder condition. • Non-invasive collection methods • Clean catch urine • Urine collection bags • Urine collection pads • Invasive collection methods • Suprapubic aspiration • In-out catheterization
- 22. Collection of sample from catheterized patient • Instructions to care giver
- 23. Laboratory processing of urine specimens: The patient’s urine sample should be transported and processed immediately (maximum within 2 hours of collection) If delay occurs: Samples should be stored in the refrigerator at 40C for a maximum of 24 hours Use Boric acid- a bacteriostatic preservative Rationale: Bacteria can multiply in urine and lead to false positive results (urine is a good culture media)
- 24. Screening of samples • Microscopy • Leucocyte esterase: • Rapid, sensitive dipstick method for detection of pus cells (pyuria). • Dipstick analysis: • Two in one method: Detects pyuria using leucocyte esterase and nitrite production for bacteriuria A wet mount of uncentrifuged urine specimen examined microscopically ( under high power) reveals the presence of pus cells, bacteria, erythrocytes, casts 6- 10 pus cells are considered significant (significant pyuria) and have to be correlated with the presence of significant bacteriuria
- 25. Culture • Media: Cysteine lactose electrolyte deficient medium (CLED) • Allows all bacteria to grow. • Semi quantitative count: A measured quantity of urine is taken with a calibrated sterile loop and cultured on CLED • Interpretation • 1-2 types of colonies: UTI present • ≥ 3 types of colonies: Contaminated sample. A repeat sample requested • Significant bacteriuria: 104 colony forming units (cfu) /ml in symptomatic patient (Kass Count) Suprapubic aspirate: Any bacterial count is significant!
- 26. CLED >3 types of conlonies: Contaminated sample Lactose fermenting colony cfu ≥ 104 Non-Lactose fermenting colony cfu ≥ 104 Non-Lactose fermenting: Proteus mirabilis: oxidase negative Pseudomonas aeruginosa: oxidase positive Lactose fermenting bacteria: Escherichia coli Klebsiella pneumoniae
- 27. • Asymptomatic bacteriuria: • Repeated positive urine culture (105cfu/ml) • Investigate & treat only pregnant women /early morning
- 28. Insignificant count 103 Significant count 104-105 Interpretation after 24 hour incubation at 370C • Bacterial Identification • Antimicrobial sensitivity done by automated system
- 29. Sterile pyuria • Large number of Pus cells observed in urine -: Pyuria • Culture repeatedly negative- Sterile pyuria • Interpretation: • Fastidious etiology. Organism does not grow on CLED • Cause: Mycobacterium tuberculosis • Chlamydia trachomatis • Virus e.g. adenovirus Clinical features of tubercular infection • Symptoms of bacterial cystitis • Symptoms of pyelonephritis • Unusual: Fever, weight loss, night sweats • Routine investigations: • Complete blood cell (CBC) count • Erythrocyte sedimentation rate (ESR) • C-reactive protein (CRP)
- 30. Laboratory Diagnosis: M. tuberculosis Serial early-morning urine cultures (at least 3) for acid-fast bacilli (AFB) are collected in a sterile flask. Reason: Mycobacteria are not excreted on all days and when excreted are present in small numbers. Diagnosis of kidney infection with Mycobacterium tuberculosis does not require counting of bacteria in the urine specimen. Any number is significant. Culture: Lowenstein Jensen Medium: Time taken- 4-8 wks Bactec 460- Time taken 2-3 days PCR: Most sensitive and specific- Species-specific IS6110 PCR test
- 31. Acute uncomplicated cystitis: Recommended agents Nitrofurantoin monohydrate / macrocrystals Trimethoprim-sulfamethoxazole Avoid in pregnancy Fosfomycin trometamol Acute uncomplicated cystitis: Alternative agents Fluoroquinolones Reserve for more serious conditions; avoid in pregnancy Beta-lactams Resistance varies by agent Treatment for UTI • Antibiotics to avoid in G6PD deficiency: • Nitrofurantoin • Fluoroquinolones • Sulfamethoxazole
- 32. Parenteral : In hospitalized patients with pyelonephritis ( community acquired ) Aminoglycoside Extended spectrum cephalosporin Fluoroquinolones 80 % of hospital acquired associated with catheterization. Multi resistant organisms such as MRSA and vancomycin resistant enterococci ( VRE ) cause UTI. MRSA: Vancomycin VRE: Linezolid Treatment: Acute uncomplicated pyelonephritis Treatment: Hospital acquired urinary Infections
Editor's Notes
- Primarily the term used is UTI. Viral and fungal causes are rare. This is the anatomical picture of the urinary tract. In which region can infection occur?
- Uropathogens such as UPEC survive by invading the bladder epithelium, producing toxins and proteases to release nutrients from the host cells. Proteus mirabilis produces urease, which hydrolyses urea to carbon dioxide and ammonia. This increases the urine pH and generates calcium crystals and magnesium ammonium phosphate precipitates,
- a | Uncomplicated urinary tract infections (UTIs) begin when uropathogens that reside in the gut contaminate the periurethral area (step 1) and are able to colonize the urethra. Subsequent migration to the bladder (step 2) and expression of pili and adhesins results in colonization and invasion of the superficial umbrella cells (step 3). Host inflammatory responses, including neutrophil infiltration (step 4), begin to clear extracellular bacteria. Some bacteria evade the immune system, either through host cell invasion or through morphological changes that result in resistance to neutrophils, and these bacteria undergo multiplication (step 5) and biofilm formation (step 6). These bacteria produce toxins and proteases that induce host cell damage (step 7), releasing essential nutrients that promote bacterial survival and ascension to the kidneys (step 8). Kidney colonization (step 9) results in bacterial toxin production and host tissue damage (step 10). If left untreated, UTIs can ultimately progress to bacteraemia if the pathogen crosses the tubular epithelial barrier in the kidneys (step 11). b | Uropathogens that cause complicated UTIs follow the same initial steps as those described for uncomplicated infections, including periurethral colonization (step 1), progression to the urethra and migration to the bladder (step 2). However, in order for the pathogens to cause infection, the bladder must be compromised. The most common cause of a compromised bladder is catheterization. Owing to the robust immune response induced by catheterization (step 3), fibrinogen accumulates on the catheter, providing an ideal environment for the attachment of uropathogens that express fibrinogen-binding proteins. Infection induces neutrophil infiltration (step 4), but after their initial attachment to the fibrinogen-coated catheters, the bacteria multiply (step 5), form biofilms (step 6), promote epithelial damage (step 7) and can seed infection of the kidneys (steps 8 and 9), where toxin production induces tissue damage (step 10). If left untreated, uropathogens that cause complicated UTIs can also progress to bacteraemia by crossing the tubular epithelial cell barrier (step 11).
- Uses: dental equipments, syringes, petri dishes,sutures, catheters
- Urine culture is generally not required in suspected cases of acute, uncomplicated cystitis because the spectrum of causative organisms is predictable and urine culture results are often not available until after completion of short-course empirical treatments. The role of urine culture is 2-fold: to provide retrospective confirmation of the presence of bacteriuria, which in the correct clinical setting confirms the diagnosis of UTI, and to provide specific information about the organism and its antimicrobial susceptibility. It is appropriate to obtain a culture (with susceptibility testing) of a pretreatment urine sample for women with suspected cystitis if the diagnosis is not clear from the history and physical examination, if an unusual or antimicrobial-resistant organism is suspected, if the episode represents a suspected relapse or treatment failure, or if the patient's therapeutic options are limited by medication intolerance. Pretreatment urine culture is also considered standard of care in pregnant women and men. Women presenting with classic symptoms of cystitis (dysuria, frequency) who do not have symptoms of possible alternative diagnoses or underlying complicating conditions may be treated for UTI without further testing. For such women, self-initiated therapy or "telephone clinic" provider-guided presumptive therapy may be appropriate (20). In a woman presenting with symptoms of acute cystitis, a positive urine dipstick result can help to confirm the diagnosis, but a negative dipstick result cannot rule out the diagnosis in a woman with a high pretest probability of cystitis (16, 21). Thus, a dipstick test is not necessary if the history is clearly diagnostic of UTI (particularly in women with symptoms akin to previous episodes). If the diagnosis is not clear-cut or if further complicating factors or alternative diagnoses emerges from the history, a more thorough and broad-based diagnostic evaluation should be conducted. Blood tests (including cultures) are not indicated in women with suspected cystitis unless they are needed to screen for alternative diagnoses suggested by the history or physical examination or to assess the status of a known underlying medical condition (e.g., diabetes mellitus). Up to 30% of women with acute pyelonephritis may have secondary bacteremia, and identification of the organism by blood culture can be helpful in cases where antibiotics are started in advance of the urine culture. Diabetic women and renal transplant recipients have a higher incidence of secondary bacteremia with UTI (22, 23).
- Women with cystitis should be treated with an appropriate antimicrobial agent. Before selecting a treatment regimen for women with presumed cystitis, ask about factors that may influence the choice of antimicrobial agent, including pregnancy and breast-feeding, other medications being taken, drug allergy history, recent antibiotic therapy, other recent infections or positive cultures, and recent travel. Also, whether there are any complicating factors should be determined because management of uncomplicated cystitis and pyelonephritis differs from that of complicated UTI. The IDSA has recently published updated guidelines for treatment of uncomplicated cystitis and pyelonephritis, specifically in premenopausal, nonpregnant women with no known urologic abnormalities or comorbid conditions (27). In addition to the usual concerns for efficacy and safety, the 2010 IDSA treatment recommendations for acute cystitis and pyelonephritis were guided by 2 important principles: the increasing prevalence of resistant organisms, and the potential for propagation of resistance (collateral damage) among normal host flora with the use of broad-spectrum antibiotics. No single agent was designated as the preferred regimen. Instead, agents are listed as recommended for first-line therapy (nitrofurantoin, TMP-SMX, pivemecillinam, and fosfomycin trometamol) and alternative agents (fluoroquinolones and beta-lactams). Treatment regimens for cystitis and pyelonephritis are listed in Tables 2 and 3, respectively. Each agent has its own caveats. Nitro-furantoin concentrates in the urine but has little tissue penetration and thus should be avoided if there is any possibility of pyelo-nephritis. A 5-day course of nitrofurantoin was as effective as a 3-day course of TMP-SMX in terms of both clinical and microbiological cure in a randomized trial (28). The main limitation to the use of TMP-SMX is the rising rate of resistance among uropathogens, especially outside the United States, and consistent evidence that in vitro resistance correlates with bacterial and clinical failures in at least 50% of women. However, the 4 studies reviewed by the IDSA guidelines committee showed that TMP-SMX remains an appropriate empirical treatment for acute uncomplicated cystitis in women when the local rate of resistance is known or expected to be < 20%. Fosfomycin is available in the United States but is rarely used. The recommended 3-g single dose may not be as efficacious as other recommended agents, and it should be not be used if pyelonephritis is suspected. Susceptibility data are not routinely reported for this drug, but surveys demonstrate that it retains activity against multidrug resistant uropath-ogens, such as extended-spectrum beta-lactamase–producing gram-negative organisms (29). Pivmecillinam, which is currently unavailable in the United States, is an extended-spectrum penicillin that is active against gram-negative organisms but is used only for treatment of UTI. Although efficacy rates are lower than those of the other recommended agents, its low resistance rates have made it a popular first-line choice in some European countries. The fluoroquinolones, ofloxacin, ciprofloxacin, and levofloxacin, are all highly efficacious in 3-day regimens but are recommended as alternative agents because they have a high propensity for collateral damage of the normal fecal flora. Increasing rates of fluoroquinolone resistance in certain areas suggest that these agents should be reserved for conditions other than acute cystitis. Beta-lactams in general have inferior efficacy, high collateral damage, and greater rates of adverse effects than other UTI antimicrobials and thus are also considered alternative agents. Pyelonephritis is a tissue-invasive disease, and the initial empirical regimen should be broad enough to ensure in vitro activity against the uropathogen. In all suspected cases, a urine culture would ideally be obtained for susceptibility testing before starting therapy so the initial empirical therapy can be tailored appropriately. The decision points in managing acute pyelonephritis include ruling out complicated infection (pregnancy, nephrolithiasis, obstruction) and then determining whether the patient can take oral antibiotics as an outpatient. If oral therapy is feasible, oral ciprofloxacin in a 7-day regimen is the preferred regimen if local resistance rates to the fluoroquinolones do not exceed 10%. The extended-release formulation of ciprofloxacin for 7 days or a once-daily dose of levofloxacin for 5 days can also be used, albeit the evidence is not as robust (27). TMP-SMX is also effective if the pathogen is susceptible, but in the absence of evidence to support short-course therapy a 14-day course is the official recommendation. If susceptibility of the uro-pathogen is not known, an initial single IV dose of ceftriaxone or a long-acting aminoglycoside is recommended before outpatient oral therapy. In a study comparing ciprofloxacin to TMP-SMX, an initial dose of IV ceftriaxone resulted in improved outcomes in women receiving TMP-SMX who had a resistant uropathogen. Oral beta-lactam agents are not recommended for treatment of pyelonephritis given inferior efficacy rates. In women being admitted for IV therapy, a broad-spectrum agent should be given until the susceptibilities of the organism are known. This can be achieved with a carbapenem agent, an aminoglycoside with or without ampicillin, or extended spectrum beta-lactam with or without an aminoglycoside, or another regimen chosen on the basis of local resistance patterns. Urinary analgesics for acute cystitis are appropriate in certain situations to speed resolution of bladder discomfort. The analgesic phenazopyridine is widely used but may cause nausea. Combination analgesics containing urinary antiseptics (methenamine, methylene blue), a urine-acidifying agent (sodium phosphate), and an antispasmodic agent (hyoscamine) are also available. Because these analgesics can mask the symptoms of antimicrobial failure, they are best used in patients with a clear diagnosis of cystitis. Patients with underlying complicating conditions are more likely to have a drug-resistant organism, to exhibit a poor response to antimicrobial therapy even when the urine organism is susceptible, and to develop complications if initial therapy for UTI is suboptimal. Broader-spectrum empirical therapy with agents to which resistance is least common and longer treatment durations are measures intended to blunt the negative effects of host compromise on treatment outcomes. In clinical trials of therapy for complicated UTI, oral fluoroquinolones were as effective as traditional iv regimens and as or even more effective than oral TMP-SMX or TMP (particularly for organisms resistant to TMP-SMX). However, resistance to fluoroquinolones among uropathogens is increasing worldwide. If the local prevalence of fluoroquinolone resistance exceeds 10%, another broad-spectrum antimicrobial should be considered, including an extended-spectrum cephalosporin with or without an aminoglycoside or a carbapenem. Combinations of a beta-lactam and a beta-lactamase inhibitor (e.g., ampicillin-sulbactam, ticarcillin-clavulanate, and piperacillin-tazobactam) could also be considered. The IDSA has issued evidence-based guidelines on the diagnosis, prevention, and treatment of CAUTI (18). The goal of limiting exposure to antimicrobial therapy and thus limiting selection pressure for resistant organisms is balanced by the awareness that microbial eradication requires a longer duration of therapy in patients with a urinary catheter. Seven days is the recommended duration of antimicrobial treatment for patients whose symptoms resolve promptly, and 10 to 14 days is recommended for patients with a delayed response. For those with CAUTI who are not severely ill, a 5-day regimen of levofloxacin may be considered (18). In pregnant women with symptomatic UTI, a urine culture and susceptibility testing should be performed. Empirical therapy with an oral antimicrobial agent that is safe for use in pregnancy should be given for 3 to 7 days for cystitis or 7 to 14 days for pyelonephritis. Antibiotic therapy should be adjusted on the basis of culture results.