BIOLOGY OF TOOTH MOVEMENT
- 1. DR SHEHNAZ JAHANGIR FIRST YEAR MDS DEPT. OF ORTHODONTICS NICDS 1
- 2. Introduction Tooth supporting tissues PhysiologicTooth Migration Tissue Response in Periodontium OrthodonticTooth Movements Optimal Orthodontic Force Theories of Orthodontic Mechanisms Tissue Response in Sutures Deleterious Effects of Orthodontic Force Post-treatment Stability Summary 2
- 3. Orthodontic treatment today comprises a wealth of removable and fixed appliances, sometimes in combination with extraoral ones. They all involve the use and control of forces acting on the teeth and adjacent structures. The principal changes from such forces are seen within the dentoalveolar system, resulting in tooth movements. 3
- 4. Other structures, such as sutures and the temporomandibular joint (TMJ) area, can also be influenced by means of dentofacial orthopedics. An optimal orthodontic force intends to induce a maximal cellular response and to establish stability of the tissue, whereas an unfavorable force does not result in a precise biological response and may initiate adverse tissue reactions. 4
- 5. During tooth movement, changes in the periodontium occur, depending on magnitude, direction, and duration of the force applied, as well as the age of the orthodontically treated patient. The periodontium consists of the investing and supporting tissues of the tooth. 5
- 6. It has been divided into two parts: • The Gingiva, whose main function is protection of the underlying tissues, and • The Attachment Apparatus, composed of the Periodontal Ligament, Cementum, and Alveolar Bone. Tooth movement requires changes in the gingiva, periodontal ligament, root cementum, and alveolar bone. 6
- 7. The gingiva is differentiated into the free and attached Gingiva. The free gingiva is in close contact with the enamel surface, and its margin is located 0.5 to 2 mm coronal to the cementoenamel junction after completed tooth eruption. The attached gingiva is firmly attached to the underlying alveolar bone and cementum by connective tissue fibers and is comparatively immobile in relation to the underlying tissue. 7
- 8. The predominant component of the gingiva is the connective tissue, which consists of collagen fibers, fibroblasts, vessels, nerves, and matrix. The fibroblast is engaged in the production of various types of fibers but is also instrumental in the synthesis of the connective tissue matrix. The collagen fibers are bundles of collagen fibrils with a distinct orientation.They provide the resilience and tone necessary for maintaining its architectural form and the integrity of the dentogingival attachment. 8
- 9. They are usually divided into the following groups • Circular fibers run in the free gingiva and encircle the tooth. • Dentogingival fibers are embedded in the cementum of the supraalveolar portion of the root and project from the cementum in a fanlike configuration into the free gingival tissue. 9
- 10. • Dentoperiosteal fibers are embedded in the same portion of the cementum as the dentogingival fibers but terminate in the tissue of the attached gingiva. • Transseptal fibers run straight across the interdental septum and are embedded in the cementum of adjacent teeth 10
- 11. The periodontal ligament (PDL), about 0.25 mm wide, is the soft, richly vascular and cellular connective tissue that surrounds the roots of the teeth and joins the root cementum with the lamina dura or the alveolar bone proper. In the coronal direction, the PDL is continuous with the lamina propria of the gingiva and is separated from the gingiva by the collagen fiber bundles, which connect the alveolar bone crest with the root (the alveolar crest fibers). 11
- 12. The true periodontal fibers, the principal fibers, develop along with the eruption of the tooth The orientation of the collagen fiber bundles alters continuously during tooth eruption.When the tooth has reached contact in occlusion and is functioning properly, they associate with the following well-oriented groups: alveolar crest fibers and horizontal, oblique, apical, and interradicular fibers. 12
- 13. The individual bundles have a slightly wavy course, which allows the tooth to move within its socket (physiologic mobility). The presence of a PDL makes it possible to distribute and resorb the forces elicited during mastication and is essential for movement of the teeth in orthodontic treatment. 13
- 14. The tissue response to orthodontic forces, including cell mobilization and conversion of collagen fibers, is considerably slower in older individuals than in children and adolescents. During physiologic conditions, collagen turnover in the PDL is much higher than that in most other tissues (e.g., twice as high as that of the gingiva). The high turnover has been attributed to the fact that forces on the PDL are multidirectional, having vertical and horizontal components. 14
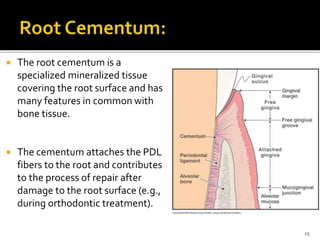
- 15. The root cementum is a specialized mineralized tissue covering the root surface and has many features in common with bone tissue. The cementum attaches the PDL fibers to the root and contributes to the process of repair after damage to the root surface (e.g., during orthodontic treatment). 15
- 16. The cementum contains no blood vessels, has no innervation, does not undergo physiologic resorption or remodeling, and is characterized by continuing deposition throughout life. During root formation a primary cementum is formed. After tooth eruption and in response to functional demands, a secondary cementum is formed that, in contrast to the primary cementum, contains cells. 16
- 17. 17
- 18. During the continuous formation of the primary cementum, portions of the principal fibers in the PDL adjacent to the root become embedded and mineralized. The Sharpey fibers in the cementum should be regarded as a direct continuation of the collagen fibers in the PDL. 18
- 19. Alveolar bone surrounds the tooth to a level approximately 1mm apical to the CEJ. The alveolar bone is covered with the periosteum, which is differentiated from the surrounding connective tissues and functions as an osteogenic zone throughout life. The alveolar bone is renewed constantly in response to functional demands by bone-forming osteoblasts and osteoclasts, cells involved in resorption 19
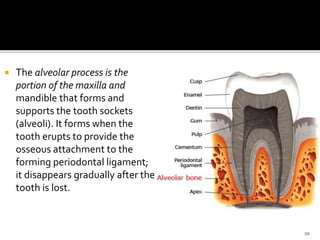
- 20. The alveolar process is the portion of the maxilla and mandible that forms and supports the tooth sockets (alveoli). It forms when the tooth erupts to provide the osseous attachment to the forming periodontal ligament; it disappears gradually after the tooth is lost. 20
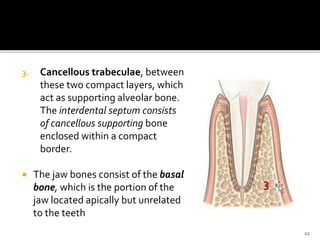
- 21. The alveolar process consists of the following: 1. An external plate of cortical bone formed by haversian bone and compacted bone lamellae, 2. The inner socket wall of thin, compact bone called the alveolar bone proper, which is seen as the lamina dura in radiographs. 2 1 21
- 22. 3. Cancellous trabeculae, between these two compact layers, which act as supporting alveolar bone. The interdental septum consists of cancellous supporting bone enclosed within a compact border. The jaw bones consist of the basal bone, which is the portion of the jaw located apically but unrelated to the teeth 3 22
- 23. Orthodontic tooth movement results in rapid formation of immature new bone. The type of bone through which the tooth is displaced must be considered in the orthodontic treatment plan. Tooth movements in a mesial or distal direction displace the roots through the spongiosa of the alveolar bone. When a tooth is moved into the reorganizing alveolus of a newly extracted tooth, remodeling is rapid because of the many differentiating cells present and the limited amount of bone to be resorbed. 23
- 24. On the contrary, movement of a tooth labially or lingually into the thin cortical plates should be undertaken with a high degree of caution, especially in adult patients, to avoid iatrogenic responses. 24
- 25. is weak, disorganized, and poorly mineralized bone. It is usually the first bone formed in response to orthodontic loading. Woven bone serves a crucial role in wound healing by (1) rapidly filling osseous defects, (2) providing initial continuity for fractures and osteotomy segments, and (3) strengthening a bone weakened by surgery or trauma. The functional limitations of woven bone are an important aspect of orthodontic retention and of the healing period following orthognathic surgery. 25
- 26. a strong, highly organized, well-mineralized tissue, makes up more than 99% of the adult human skeleton. When new lamellar bone is formed, a portion of the mineral component (hydroxylapatite) is deposited by osteoblasts during primary mineralization Secondary mineralization, which completes the mineral component, is a physical process (crystal growth) that requires many months. The full strength of lamellar bone that supports an orthodontically moved tooth is not achieved until about 1 year after completion of active treatment. This is an important consideration in planning orthodontic retention and in the postoperative maturation period that follows orthognathic surgery 26
- 27. is an osseous tissue formed by the deposition of lamellar bone within a woven bone lattice, a process called cancellous compaction. This process is the quickest means of producing relatively strong bone. Composite bone is an important intermediary type of bone in the physiologic response to orthodontic loading. It is the predominant osseous tissue for stabilization during the early process of retention or postoperative healing. 27
- 28. is a functional adaptation of lamellar structure to allow attachment of tendons and ligaments. Perpendicular striations, called Sharpey fibers, are the major distinguishing characteristics of bundle bone. Distinct layers of bundle bone usually are seen adjacent to the PDL along physiologic bone-forming surfaces. 28
- 29. 29
- 30. The teeth and their supporting tissues have a lifelong ability to adapt to functional demands and hence drift through the alveolar process, a phenomenon called physiologic tooth migration. Also well known clinically is that any change in the equilibrium of occlusal pressure, such as loss of a neighbouring or antagonistic tooth, may induce further tooth movement. The tissue reaction that occurs during physiologic tooth migration is a normal function of the supporting structures. 30
- 31. First time by Stein andWeinmann,1925, who observed that the molars in adults gradually migrate in a mesial direction. When the teeth migrate, they bring the supra-alveolar fiber system with them. Such movement implies remodeling of the PDL and alveolar bone. The turnover rate of the PDL is not uniform throughout the ligament, the cells being more active on the bone side than near the root cementum. 31
- 32. Osteoclasts are seen in scattered lacunae associated with the resorptive surface along the alveolar bone wall, toward which the tooth is moving; the number of cells is more numerous when tooth migration is rapid. The alveolar bone wall from which the tooth is moving away (depository side) is characterized by osteoblasts depositing nonmineralized osteoid, which later mineralizes in the deeper layer. 32
- 33. 33
- 34. Simultaneously, new collagen fibrils are produced on the bone surface. A slow apposition occurs on the cementum surface throughout life. The unmineralized precementum layer has special importance as a resorption-resistant “coating” layer, thus protecting the root surface during the physiologic migration. 34
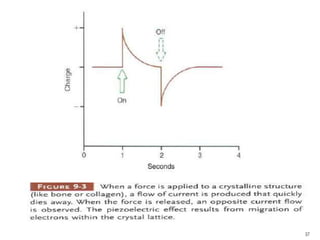
- 35. During masticatory function, the teeth and periodontal structures are subjected to intermittent heavy forces. When a tooth is subjected to heavy loads of this type, quick displacement of the tooth within the PDL space is prevented by the incompressible tissue fluid. Instead, the force alveolar bone bends in response. 35
- 36. In heavy function, individual teeth are slightly displaced as the bone of the alveolar process bends to allow this to occur, and bending stresses are transmitted over considerable distances. Bone bending in response to normal function generates piezoelectric currents that appear to be an important stimulus to skeletal regeneration and repair.This is the mechanism by which bony architecture is adapted to functional demands. 36
- 37. 37
- 38. Prolonged force, even of low magnitude, produces a different physiologic response- remodeling of the adjacent bone. 38
- 39. In 1905, Carl Sandstedt’s studies in dogs convincingly demonstrated that tooth movement is a process of resorption and apposition. He gave the first description of the glasslike appearance of the compressed tissue, termed hyalinization, which has been associated with a standstill of the tooth movement. In 1950s tooth movements attracted wider attention with Kaare Reitan’s classic study The initial tissue reaction incident to orthodontic tooth movement as related to the influence of function. Reitan used the dog as his experimental model but also extracted teeth from humans. 39
- 40. 40
- 41. Application of a continuous force on the crown of the tooth tooth movement within the alveolus narrowing of the periodontal membrane, particularly in the marginal are osteoclasts differentiate along the alveolar bone the cells increase in number and differentiate into osteoclasts and fibroblasts width of the membrane is increased by osteoclastic removal of bone in young humans after 30 to 40 hours Favourable conditions 41
- 42. orientation of the fibers in the periodontal membrane changes Arrangement of the ground substance changes fibroblasts not only are capable of synthesizing fibrous tissue and ground substance but also play an important role in the breakdown of connective tissue. These processes occur simultaneously 42
- 43. During the crucial stage of the initial application of force, compression in limited areas of the membrane frequently impedes vascular circulation and cell differentiation, causing degradation of the cells and vascular structures rather than proliferation and differentiation. The tissue reveals a glasslike appearance in light microscopy, which is termed hyalinization. It is caused partly by anatomic and partly by mechanical factors and is almost unavoidable in the initial period of tooth movement in clinical orthodontics. 43
- 44. Hyalinization represents a sterile necrotic area degeneration elimination of destroyed tissue establishment of a new tooth attachment 44
- 45. starts where the pressure is highest and the narrowing of the membrane is most pronounced, around bone spicules. It may be limited to parts of the membrane or extend from the root surface to the alveolar bone. Retardation of the blood flow disintegration of the vessel walls and degradation of blood elements The cells undergo a series of changes, swelling of the mitochondria and the endoplasmic reticulum continuing with rupture and dissolution of the cytoplastic membrane. 45
- 46. This leaves only isolated nuclei between compressed fibrous elements (pyknosis) and is the first indication of hyalinization. In hyalinized zones, the cells cannot differentiate into osteoclasts and no bone resorption can take place from the periodontal membrane. Tooth movement stops until the adjacent alveolar bone has been resorbed, the hyalinized structures are removed, and the area is repopulated by cells. A limited hyalinized area occurring during the application of light forces may be expected to persist from 2 to 4 weeks in a young patient .When bone density is high, the duration is longer. 46
- 47. The peripheral areas of the hyalinized compressed tissue are eliminated by an invasion of cells and blood vessels from the adjacent undamaged PDL hyalinized materials are ingested by the phagocytic activity of macrophages and are removed completely The adjacent alveolar bone is removed by indirect resorption by cells that have differentiated into osteoclasts on the surfaces of adjacent marrow spaces or, if the alveolar wall and the outer cortical bone are fused, on the surface of the alveolar process. 47
- 48. Reestablishment of the tooth attachment in the hyalinized areas starts by synthesis of new tissue elements as soon as the adjacent bone and degenerated membrane tissue have been removed. The ligament space is wider than before treatment started, and the membranous tissue under repair is rich in cells. 48
- 49. A side effect of the cellular activity during the removal of the necrotic hyalinized tissue is that the cementoid layer of the root and the bone are left with raw unprotected surfaces in certain areas that can readily be attacked by resorptive cells. Root resorption then occurs around this cell-free tissue, starting at the border of the hyalinized zone. 49
- 50. 50
- 51. The first sign of root resorption (initial phase) was defined as a penetration of cells from the periphery of the necrotic tissue where mononucleated fibroblast-like cells, stained negatively by tartrate-resistant acid phosphatase (TRAP), started removing the precementum/cementum surface. Root resorption beneath the main hyalinized zone occurred in a later phase during which multinucleatedTRAP-positive cells were involved in removing the main mass of necrotic PDL tissue and resorbing the outer layer of the root cementum. 51
- 52. When the movement is discontinued, repair of the resorbed lacunae occurs, starting from the periphery After the force has terminated, active root resorption by TRAP-positive cells in the resorption lacunae still was observed in areas where hyalinized tissue existed. After termination of force and in the absence of hyalinized necrotic tissue in the PDL, repair on the resorption lacunae occurred. The first sign was synthesis of collagenous fibrillar material by fibroblast-and cementoblast-like cells, followed by reestablishment of the new PDL. 52
- 53. 53
- 54. the PDL is considerably widened. The osteoclasts attack the bone surface over a much wider area. As long as the force is kept within certain limits or gentle reactivation of the force is undertaken, further bone resorption is predominantly direct . The fibrous attachment apparatus is reorganized by the production of new periodontal fibrils. When the application of a force is favorable, a large number of osteoclasts appear along the bone surface on the pressure side and tooth movement is rapid. 54
- 55. The main feature is the deposition of new bone on the alveolar surface from which the tooth is moving away (tension side). As proliferation starts, osteoid tissue is deposited on the tension side.The formation of this new osteoid depends to some extent on the form and thickness of the fiber bundles. The original periodontal fibers become embedded in the new layers of pre-bone, or osteoid, which mineralizes in the deeper parts. New bone is deposited until the width of the membrane has returned to normal limits, and simultaneously the fibrous system is remodeled. 55
- 56. Concomitantly with bone apposition on the periodontal surface on the tension side, an accompanying resorption process occurs on the spongiosa surface of the alveolar bone that tends to maintain the dimension of the supporting bone tissue. During the resorption of the alveolar bone on the pressure side, maintenance of the alveolar lamina thickness is ensured by apposition on the spongiosa surface. These processes are mediated by the cells of the endosteum, which cover all the internal bone surfaces and dental alveoli. 56
- 57. Basically, no great difference exists between the tissue reactions observed in physiologic tooth migration and those observed in orthodontic tooth movement. Because the teeth are moved more rapidly during treatment, the tissue changes elicited by orthodontic forces are more significant and extensive. Application of a force on the crown of the tooth leads to a response in its surrounding tissues, resulting in an orthodontic tooth movement, which depends on type, magnitude, and duration of the force. 57
- 58. Orthodontic forces comprise those that are meant to act on the PDL and alveolar process, Orthopedic forces are more powerful and act on the basal parts of the jaws. 58
- 59. 59
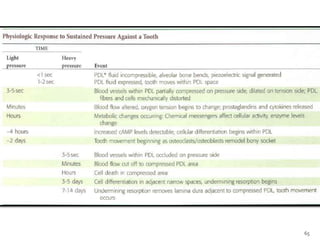
- 60. The heavier the sustained pressure, the greater should be the reduction in blood flow through compressed areas of the PDL, up to the point that the vessels are totally collapsed and no further blood flows Increasing the force against a tooth causes decreasing perfusion of the PDL on the compression side 60
- 61. 61
- 62. When light but prolonged force is applied to a tooth, blood flow through the partially compressed PDL decreases as soon as fluids are expressed from the PDL space and the tooth moves in its socket ( i.e.,i n a few seconds) 62
- 63. 63
- 64. 64
- 65. 65
- 66. When hyalinization and undermining resorption occur, an inevitable delay in tooth movement results. This is caused: i. by a delay in stimulating differentiation of cells within the marrow spaces, ii. because a considerable thickness of bone must be removed from the underside before any tooth movement can take place 66
- 67. 67
- 68. Not only is tooth movement more efficient when areas of PDL necrosis are avoided but pain is also lessened. Even with light forces, small avascular areas are likely to develop in the PDL and tooth movement will be delayed until these can be removed by undermining resorption. In clinical practice, tooth movement usually proceeds in a more stepwise fashion because of the inevitable areas of undermining resorption. Too much force is not helpful. 68
- 69. The key to producing orthodontic tooth movement is the application of sustained force. It means that the force must be present for a considerable percentage of the time, certainly hours rather than minutes per day. Animal experiments suggest that only after force is maintained for approximately 4 hours do cyclic nucleotide levels in the PDL increase, indicating that this duration of pressure is required to produce the "second messengers“ needed to stimulate cellular differentiation. 69
- 70. Continuous forces, produced by fixed appliances that are not affected by what the patient does, produce more tooth movement than removable appliances unless the removable appliance is present almost all the time. Removable appliances worn for decreasing fractions of time produce decreasing amounts of tooth movement. With removable appliances, patients are too unreliably compliant. 70
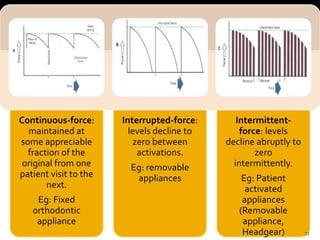
- 71. Duration of force has another aspect related to how force magnitude changes as the tooth responds by moving is known as force decay. From this perspective orthodontic force duration is classified by the rate of decay as: A. Continuous Forces B. Interrupted Forces C. Intermittent Forces 71
- 72. Continuous-force: maintained at some appreciable fraction of the original from one patient visit to the next. Eg: Fixed orthodontic appliance Interrupted-force: levels decline to zero between activations. Eg: removable appliances Intermittent- force: levels decline abruptly to zero intermittently. Eg: Patient activated appliances (Removable appliance, Headgear) 72
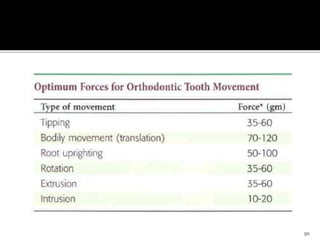
- 73. Direction of forces will result in different kinds of tooth movements. Both the amount of force delivered to a tooth and also the area of the PDL over which that force is distributed are important in determining the biologic effect. The PDL response is determined not by force alone, but by force per unit area, or pressure. Since the distribution of force within the PDL, differs with different types of tooth movement,it is necessary to specify the type of tooth movement for optimum force levels for orthodontic purposes. 73
- 74. Tipping of a tooth leads to a concentration of pressure in limited areas of the PDL. A fulcrum is formed, which enhances root movement in the opposite direction. 74
- 75. It results in the formation of a hyalinized zone slightly below the alveolar crest, particularly when the tooth has a short, undeveloped root. If the root is fully developed, the hyalinized zone is located a short distance from the alveolar crest. 75
- 76. Tipping of a tooth by light continuous forces results in a greater movement within a shorter time than that obtained by any other method. In most young orthodontic patients, bone resorption resulting from a moderate tipping movement usually is followed by compensatory bone formation.The degree of such compensation varies individually and depends primarily on the presence of bone-forming osteoblasts in the periosteum. 76
- 77. A torquing movement of a tooth involves tipping of the apex 77
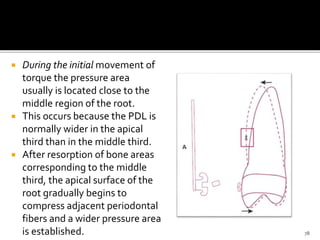
- 78. During the initial movement of torque the pressure area usually is located close to the middle region of the root. This occurs because the PDL is normally wider in the apical third than in the middle third. After resorption of bone areas corresponding to the middle third, the apical surface of the root gradually begins to compress adjacent periodontal fibers and a wider pressure area is established. 78
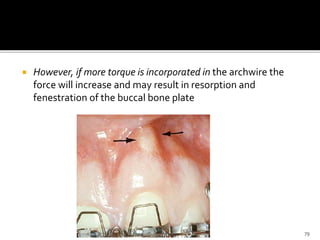
- 79. However, if more torque is incorporated in the archwire the force will increase and may result in resorption and fenestration of the buccal bone plate 79
- 80. Bodily tooth movement is obtained by establishing a couple of forces acting along parallel lines and distributing the force over the whole alveolar bone surface. This is a favorable method of displacement provided the magnitude of force does not exceed a certain limit 80
- 81. Rotation of a tooth creates two pressure sides and two tension sides and may cause certain variations in the type of tissue response observed on the pressure sides. Hyalinization and undermining bone resorption take place in one pressure zone, while direct bone resorption occurs in the other. 81
- 82. These variations are caused chiefly by the anatomy of the tooth and the magnitude of the force. The free gingival fiber groups are arranged obliquely from the root surface. Because these fiber bundles interlace with the periosteal structures and the whole supra-alveolar fibrous system, rotation also causes displacement of the fibrous tissue located some distance from the rotated tooth 82
- 83. Forces to produce rotation of a tooth around its long axis could be much larger than those to produce other tooth movements, since the force could be distributed over the entire PDL rather than over a narrow vertical strip. However, it is essentially impossible to apply a rotational force so that the tooth does not also tip in its socket, and when this happens, an area of compression is created just as in any other tipping movement. For this reason, appropriate forces for rotation are similar to those for tipping. 83
- 84. Extrusive movements ideally produce no areas of compression within the PDL, only tension. Even if compressed areas could be avoided, heavy forces risk “extraction” of the tooth. Varying with the individual tissue reaction, the periodontal fiber bundles elongate and new bone is deposited in areas of alveolar crest as a result of the tension exerted by these stretched fiber bundles . 84
- 85. In young individuals, extrusion of a tooth involves a more prolonged stretch and displacement of the supra-alveolar fiber bundles than of the principal fibers of the middle and apical thirds. If the tooth tipped at all while being extruded, areas of compression will be created. Extrusive forces, like rotation, should be of about the same magnitude as those for tipping. 85
- 86. Unlike extruded teeth, intruded teeth in young patients undergo only minor positional changes after treatment. Relapse usually does not occur, partly because the free gingival fiber bundles become slightly relaxed. 86
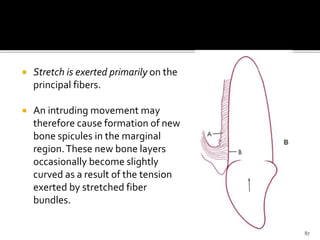
- 87. Stretch is exerted primarily on the principal fibers. An intruding movement may therefore cause formation of new bone spicules in the marginal region.These new bone layers occasionally become slightly curved as a result of the tension exerted by stretched fiber bundles. 87
- 88. Intrusion requires careful control of force magnitude. Light force is required because the force is concentrated in a small area at the tooth apex. A light continuous force, such as that obtained in the light wire technique, has proved favorable for intrusion in young patients. 88
- 89. In other cases the alveolar bone may be closer to the apex, increasing the risk for apical root resorption. If the bone of the apical region is fairly compact, as it is in some adults, a light interrupted force may be preferable to provide time for cell proliferation to start, and direct bone resorption may prevail when the arch is reactivated after the rest period. Intrusion may also cause changes in the pulp tissue such as vascularization of the odontoblast and pulpal edema Rearrangement of the principal fibers occurs after a retention period of a few months. 89
- 90. 90
- 91. An optimal force is based on proper mechanical principles, which enable the orthodontist to move teeth without traumatizing dental or paradental tissues, and without moving dental roots redundantly (round-tripping), or into danger zones (compact plates of alveolar bone) The classic definition of optimal force by Schwarz in 1932 was “the force leading to a change in tissue pressure that approximated the capillary vessels’ blood pressure, thus preventing their occlusion in the compressed periodontal ligament.” 91
- 92. According to Schwarz, forces below optimum produce no reaction, whereas forces above that level lead to tissue necrosis, thus preventing frontal resorption of the alveolar bone. Storey and Smith reported the same finding in 1952. o They studied distal movement of canines in orthodontic patients o suggested that there is an optimum range of pressure (150- 200 g) on the tooth-bone interface that produces a maximum rate of tooth movement. 92
- 93. The current concept of optimum force views it as an extrinsic mechanical stimulus that evokes a cellular response that aims to restore equilibrium by remodeling periodontal supporting tissues. This concept means that there is a force of certain magnitude and temporal characteristics (continuous v intermitted, constant v declining) capable of producing a maximal rate of tooth movement, without tissue damage, and with maximum patient comfort. The optimal force might differ for each tooth and for each patient. 93
- 94. Orthodontic tooth movement has been defined as the result of a biologic response to interference in the physiologic equilibrium of the dentofacial complex by an externally applied force. (Proffit) 3 theories have been proposed: 1. The Bone-BendingTheory, Farrar (1888) 2. The Biological ElectricityTheory, Bassett and Becker (1962) 3. The Pressure-TensionTheory, Sandstedt (1904), Oppenheim (1911), and Schwarz (1932) 94
- 95. Farrar first to suggest, 1888, alveolar bone bending plays a pivotal role in orthodontic tooth movement. Hypothesis later confirmed with the experiments of Baumrind in rats and Grimm in humans. 95
- 96. Orthodontic Appliance Activated Forces throughTooth All tissues nearby BONE BENDING Accelerated bone turnover and renewal of cellular & inorganic fractions Bone remain in deformed position 96
- 97. The force delivered to the tooth is dissipated throughout the bone by development of stress lines Further force application stimulus for altered biological responses of cells lying perpendicular to the stress lines. The altered activity of cells modifies the shape and internal organization of bone, to accommodate the exogenous forces acting on it. 97
- 98. Epker and Frost described the change in shape of the alveolar bone circumference resulting from stretching the PDL fibres. This fibre stretching decreases the radius of the alveolar wall, i.e, bending bone in the tension zone, where apposition of bone takes place. In areas of PDL tension, the interfacing bone surface assumes a concave configuration, in which the molecules are compressed, whereas, in zones of compressed PDL, the adjacent alveolar bone surface becomes convex. 98
- 99. It is postulated that in sites of compression in the PDL, it displays disorganization and diminution of fiber production. Here, cell replication decreases, as a result of vascular constriction. In contrast, in PDL tension sites, stimulation produced by stretching of fiber bundles results in an increase in cell replication. 101
- 100. Schwarz detailed the concept by correlating the tissue response to the magnitude of the applied force with the capillary blood pressure, and categorized it as four degrees of biologic effect: • First degree of biologic effect.The force is of such a short duration or so slight that no reaction whatsoever is caused in the periodontium. 102
- 101. • Second degree of biologic effect.The force is gentle; it remains below the pressure in the blood capillaries, i.e. less than 20 to 26 g for 1 cm2 of root surface, but it is nevertheless sufficient to cause resorption in the alveolar bone at the regions of pressure in the PDL. After the force ceases there will be anatomic and functional resolution of integrity of the PDL and alveolar bone without resorption of dental roots. 103
- 102. • Third Degree of Biologic Effect .The force is Fairly strong; sustaining increased pressure in the blood capillaries of the compressed PDL. At these areas suffocation of the strangled PDL develops, followed by resorption of the necrotic tissue, including the dental root surfaces. This resorption takes an impetuous course and attacks also those parts of the surface of the root, the vitality of which may be injured by the pressure. After the force ceases, there will be anatomic and functional resolution of integrity of the PDL and alveolar bone, with resorption of roots frequently progressing into the dentin. 104
- 103. • Fourth Degree of Biologic Effect.The force is strong, squeezing the strangled PDL, and the tooth touches the bone after the soft tissues are crushed. Alveolar bone resorption occurs in the periphery of the hyalinized PDL zones, as well as in bone marrow cavities near the compressed PDL. This situation is associated with a high risk of severe alveolar bone and root resorption, and damage to tissues of the dental pulp. In some cases, ankylosis of the tooth with the alveolar bone may occur. 105
- 104. Schwarz concluded “that the most favorable treatment is that which works with forces not greater than the pressure of blood capillaries.” He identified this pressure as 15–20 mm of Hg in man and most mammals, and calculated the optimal force level to be 20–26 g to 1 cm2 of root surface area, suggesting that these limits of pressure are critical, capable of generating a continuous resorption of alveolar bone in areas of pressure in the PDL. 106
- 105. Following Schwarz’s publication, Oppenheim worked further on tissue reactions in mature monkeys (Macaca rhesus) to applications of light and heavy forces (Oppenheim, 1944). He concluded that with light forces, osteoclasts are mobilized at a very fast pace and attack bone by a uniform superficial lacunar resorption.These cells, called “primary osteoclasts,” stayed active in the site for almost four days. 107
- 106. In contrast, the use of heavy forces resulted in crushing of the PDL, with a cut off in all its nutritional supplies, resulting in undermining resorption.The direction of bone resorption comes from unintended sources, with an inflow of osteoclasts from adjacent unaffected areas.These osteoclasts, called “secondary osteoclasts,” persist until the crushed PDL, bone and cementum are removed The hemorrhage formed by crushed blood vessels and found that the impaired nourishment along with encroachment of osteophytes and toxins from decomposed red blood cells lead to mobilization of osteoclasts from far off sites, called “tertiary osteoclasts” 108
- 107. He concluded that primary osteoclasts are the type, which is of great help to the orthodontist, and that only light forces can induce their production in abundance. Reitan (1960) concluded that the tissue changes observed were those of degeneration related to force per unit area, and that attempts should be made to minimize these changes. 109
- 108. Bien (1966), through his research on the effect of intrusive forces on mandibular incisors, recorded an oscillation of the force inside the dental socket, and named it the hydraulic damping effect. He identified three distinct, but interactive fluid systems present in paradental tissues: the vascular system, interstitial fluids, and cellular fluids. He used Reynold’s numbers to measure tooth oscillation and concluded that the low Reynold’s number observed for the tooth subjected to oscillations is due to predominance of viscous forces acting within the system. 110
- 109. He observed an escape of extracellular fluids from the PDL to the marrow spaces through the minute perforations in the alveolar wall. This phenomenon, occurring in the first stage of OTM, when PDL fibers are slack, depends mainly on size and number of alveolar bone perforations. The slack fibers become tightened once the extracellular fluids are exhausted. 111
- 110. Owing to the presence of interstitial fluid or ground substance throughout the PDL, and the fact that the PDL is extremely thin, when compared to the sizes of the dental root and alveolus, he related the behaviour of the PDL to that of the “squeeze film effect” proposed by Hays (1961). The presence of this film enables the tooth to withstand the heavy forces applied as part of orthodontic treatment or masticatory efforts. Once the force is released, replenishment of fluid occurs through recirculation of interstitial fluid and diffusion through capillary walls, restoring the equilibrium. 112
- 111. With application of high sustained forces, capillary pressure will not be sufficient enough to counteract the effect and thus to replenish the fluid back to equilibrium. In this stage, the randomly running PDL fibers, which crisscross the blood vessels, tighten-up, leading to compression, constriction of blood vessels, and leading to stenosis. This constriction point creates ballooning of the vessel wall above it, creating hydrodynamic pressure heads. 113
- 112. Drawing support from Bernoulli’s principle, Bien explained the creation of a pressure drop in areas of stenosed blood vessels, leading to gas formation and sub-atmospheric pressure. The gas bubbles formed might escape out of the capillaries and become lodged between bone spicules to create a favorable area for bone resorption. 114
- 113. 115
- 114. Controlled forces generated by various types of headgear and appliances for palatal expansion have shown cephalometric changes of the craniofacial morphology. The possibility of influencing the basal parts of the nasomaxillary complex is an open suture before any bony union (synostosis) has been established. Histologic studies on human maxillary sutures have shown that palatal suture closure usually starts during the third decade of life, although with large individual variations. After adolescence, closure was observed in most specimens, indicating a rapid increase in fusion during the third decade. 116
- 115. Sutures consist of a fibrous tissue with osteogenic layers on both surfaces. Sutures represent an extension of the periosteal layer of the bone and participate in the design of the bone by their remodeling capacity. The fiber system is mainly collagenous with a rapid synthesis and turnover. Elastic fibers are more frequent in sutures than in the PDL. The maturing suture tissue in the growing individual demonstrates changes with age that eventually end with a bony obliteration of the sutural space. 117
- 116. 118
- 117. The density and thickness of the fibrous component increase with age, and when growth ceases, bundles of fibers can be seen running transversely across the suture, increasing the mechanical strength of the joint. Osteogenesis tends to be restricted to areas of transversely densely arranged collagen bundles, a preliminary stage to bony bridgings. Because of the serpentine course of the suture, areas of tension and compression develop in the tissue 120 •Closure progresses more rapidly in the oral than in the nasal part of the palatal vault, and •the intermaxillary suture starts to close more often in the posterior than in the anterior part
- 118. The attempt to move an incisor orthodontically through the midpalatal suture in dogs was shown to be unsuccessful. The histologic analysis revealed that the suture had been dislocated in front of the orthodontically moved incisor. Eventually, the PDL and suture tissue became merged, demonstrating an apparently close similarity between the tissues of the two joint types. However, in dogs with a closed suture, the incisor could pass the sutural area without any impediment 121
- 119. Traction generated by orthopedic forces stimulate sutural growth, and widening of the midpalatal suture is a clinically well-documented procedure in orthodontics . The mechanical response to traction includes a widening of the suture and changes in the orientation of fiber bundles. 122
- 120. 123
- 121. A considerable increase of osteoblasts and an osteoid zone on both sutural bone surfaces indicate bone formation. The bone deposition accompanies traction, allowing the suture to recover a normal histologic picture. Experiments in vitro verify that mechanical tensile forces stimulate synthesis of structural proteins. Healing of a suture after rapid expansion may entail formation of bony bridges across the suture. 124
- 122. Rapid maxillary expansion is an orthopedic procedure that influence not only the midpalatal suture but also the circumaxillary sutural system. In such a palatal splitting, most of the resistance to separation results from the circumaxillary structures. Because posterior and anterior displacements of the maxilla (distraction) involve more sutures than displacements caused by palatal expansion, the resistance to separation consequently increases. Therefore, orthopedic forces have to be applied after surgical opening of suture. 125
- 123. 1.mobility and pain 2. effects on pulp 3. effects on root structure. 4. effects on alveolar bone height 126
- 124. Mobility and pain with heavy force, the greater amount of hyalinization and undermining resorption is expected and the greater mobility will be observed. orthodontic tooth movement is associated with the compression and tension of PDL cells which leads to the liberation of substances responsible for pain. 127
- 125. Effects on pulp a mild transient inflammation reactions in the pulp of at the beginning of treatment may be expected with optimal force levels. however if a tooth is subjected to heavy force, large increment of tooth movement in undermining resorption would cause disruption of an apical blood vessel and loss of vitality. 128
- 126. Effects on root structure. when orthodontic force is applied, there is usually an associated resorption of cementum of the root adjacent to hyalinized area. However, with extensive resorption, there is permanent loss of root structure, with shortening of root apex likely to occur. the use of heavy continous orthodontic force commonly leads to severe root resorption. 129
- 127. Murrell et al (1996) reported that removal of orthodontic forces produces significant changes in number and density of PDL blood vessels. Normalization of the periodontal vasculature was observed during an interval equivalent to the duration of orthodontic force application, and it has been suggested to be one of the main reasons for relapse of the end result of orthodontic treatment. 130
- 128. Yoshida et al (1999) evaluated the cellular repsonses involved in the relapse process of experimentally moved rat molars, and suggested that there will be rapid remodelling of the PDL and alveolar bone post-treatment which can be identified as the main cause of relapse. 131
- 129. Erespolsky et al in 2002 stated that various types of damage to teeth and pdl produced by orthodontic mechanotherapy healed more rapidly and extensively in functional teeth. During recovery period, the return of periodontal dimensions to normal values is regulated by the rate and direction of alveolar bone turn over. 132
- 130. Rapid advances made in all biological fields have enabled us to better understand the mechanisms involved in orthodontic tooth movement. It has become evident that at different stages of tooth movement, different combinations of cell-cell and cell-matrix interactions occur, which determine the nature of remodeling changes. The ongoing developments will move orthodontics closer to the goal of being optimal, where teeth are moved efficiently without causing discomfort to the patient or damage to the teeth and their supporting tissues. 133