Burns.pptx
- 1. BURNS
- 2. Definition • Burns are a result of the effects of thermal injury on the skin and other tissues • Human skin can tolerate temperatures up to 42-440 C (107-1110 F) but above these, the higher the temperature the more severe the tissue destruction • Below 450 C (1130 F), resulting changes are reversible but >450 C, protein damage exceeds the capacity of the cell to repair
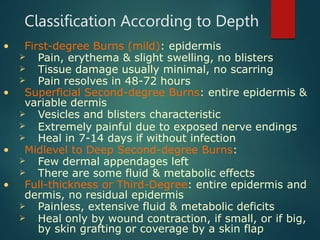
- 3. Classification According to Depth • First-degree Burns (mild): epidermis Pain, erythema & slight swelling, no blisters Tissue damage usually minimal, no scarring Pain resolves in 48-72 hours • Superficial Second-degree Burns: entire epidermis & variable dermis Vesicles and blisters characteristic Extremely painful due to exposed nerve endings Heal in 7-14 days if without infection • Midlevel to Deep Second-degree Burns: Few dermal appendages left There are some fluid & metabolic effects • Full-thickness or Third-Degree: entire epidermis and dermis, no residual epidermis Painless, extensive fluid & metabolic deficits Heal only by wound contraction, if small, or if big, by skin grafting or coverage by a skin flap
- 4. Burn Photos Mild Burn 2nd degree Burn 1 hr 2nd degree Burn 1 day 2nd degree Burn 2 days
- 5. Classification According to Extent • Mild: 10% • Moderate: 10-30% • Severe: > 30% • Hospitalization for > 10% of body surface area Infant Rule of Nines (for quick assessment of total body surface area affected by burns) Anatomic structure Surface area Head 18% Anterior Torso 18% Posterior Torso 18% Each Leg 14% Each Arm 9% Perineum 1%
- 6. Kinds of Burns • Scald Burn: most frequent in home injuries; hot water, liquids and foods are most common causes; above 65o C, cell death • Flame Burn: due to gasoline, kerosene, liquified petroleum gas (LPG) or burning houses • Chemical Burn: common in industries and laboratories but may also occur at home; acid is more common than alkali • Electrical Burn: worse than the other types; with entrance and exit wounds; may stop the heart and depress the respiratory center; may cause thrombosis and cataracts • Radiation Burn: from X-ray, radioactive radiation and nuclear bomb explosions
- 7. Burn Photos Scald Burns Flame Burns
- 8. Burn Photos Chemical (Acid) Burns Radiation (Flash) Burns
- 9. Burn Photos Electrical Burns Entrance Wounds Entrance wound of electrical burns from an overheated tool Severe swelling peaks 24-72 hrs after Electrical Burns Exit Wounds Electrical burns mummified 1st 2 fingers later removed
- 10. Physiological Response • Typically, biphasic response • The initial period of hypofunction manifests as: (a) Hypotension, (b) Low cardiac output, (c) Metabolic acidosis, (d) Ileus, (e) Hypoventilation, (f) Hyperglycemia, (g) Low oxygen consumption and (h) Inability to thermoregulate • This ebb phase occurs usually in the first 24 hours and responds to fluid resuscitation • The flow phase, resuscitation, follows and is characterized by gradual increases in (a) Cardiac output, (b) Heart rate, (c) Oxygen consumption and (d) Supranormal increases of temperature • This hypermetabolic hyperdynamic response peaks in 10-14 days after the injury after which condition slowly recedes to normal as the burn wounds heal naturally or surgically closed by applying skin grafting
- 11. Pathologic Features • Zone of coagulation (necrosis): Superficial area of coagulation necrosis and cell death on exposure to temperatures >450 (primary injury) • Zone of stasis (vascular thrombosis): Local capillary circulation is sluggish, depending on the adequacy of the resuscitation, can either remain viable or proceed to cell death (secondary injury) • Zone of hyperemia (increased capillary permeability)
- 12. Burn Pathophysiology: Edema • Injured tissue Increased permeability of entire vascular tree loss of water, electrolytes and proteins from the vascular compartment severe hemoconcentration • Protein leakage resultant hypoproteinemia, increased osmotic pressure in the interstitial space • Decreased cell membrane potential cause inward shift of Na+ and H2O cellular swelling • In the injured skin, effect maximal 30 min after the burn but capillary integrity not restored until 8-12 hours after, usually resolved by 3-5 days • In non-injured tissues, only mild and transient leaks even for burns >40% BSA
- 13. Burn Pathophysiology: Cardiac • Cardiac output decreases due to: 1) Decreased preload induced by fluid shifts 2) Increased systemic vascular resistance caused by both hypovolemia and systemic catecholamine release 3) A myocardial depressant factor has been described that impairs cardiac function • Cardiac output normal within 12-18 hours, with successful resuscitation • After 24 hours, it may increase up to 2 ½ times the normal and remain elevated until several months after the burn is closed
- 14. Burn Pathophysiology: Blood • The red-cell mass decreases due to direct losses • Immediate, 1-2 hours after, and delayed, 2-7 days postburn, hemolysis occurs due to damaged cells and increased fragility • Anemia within 4-7 days is common and expected, typically, will persist until wound healing occur; depressed erythropoietin levels documented • Early mild thrombocytopenia (sequestration) followed by thrombocytosis (2-4x normal) and elevated fibrinogen, factor V and factor VIII levels commonly by end of the 1st week • A “normal” platelet or fibrinogen level may be an early sign of disseminated intravascular coagulation • Persistent thrombocytopenia is associated with poor prognosis -- suspect sepsis
- 15. Burn Pathophysiology: Metabolic • Severe catabolism with breakdown of muscle protein for gluconeogenesis as acute response • Prostaglandins and cytokines implicated in increased core temperature of 1-20 C and in initiating acceleration of nitrogen catabolism • Plasma levels of catecholamines, glucagon and cortisol all increase, maximal in patients with 50-60% TBSAB, while insulin and thyroid hormone levels decrease • Hypermetabolic response may approach 200% of BMR remaining elevated for months after burn closed • Early enteral feeding associated with lessening of the hypermetabolic response
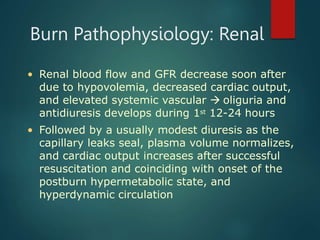
- 16. Burn Pathophysiology: Renal • Renal blood flow and GFR decrease soon after due to hypovolemia, decreased cardiac output, and elevated systemic vascular oliguria and antidiuresis develops during 1st 12-24 hours • Followed by a usually modest diuresis as the capillary leaks seal, plasma volume normalizes, and cardiac output increases after successful resuscitation and coinciding with onset of the postburn hypermetabolic state, and hyperdynamic circulation
- 17. Burn Pathophysiology: Immunologic • Mechanical barrier to infection is impaired because of skin destruction • Immunoglobulin levels decreased as part of general leak and leukocyte chemotaxis, phagocytosis, and cytotoxic activity impaired • The reticuloendothelial system's depressed bacterial clearance is due to decreases in opsonic function • These changes, together with a non-perfused, bacterially-colonized eschar overlying a wound full of proteinaceous fluid, put the patient in a significant risk for infection
- 18. First Aid Measures in Burns Extinguish flames by rolling in the ground, cover child with blanket, coat or carpet After determining airway is patent, remove smoldering clothes and constricting accessories during edema phase in the 1st 24-72 hours after Brush off remaining chemical if powdered or solid then wash or irrigate abundantly with water Cover burn wounds with clean, dry sheet and apply cold (not iced) wet compresses to small injuries; significant burns (>15-20% BSA) decreases body temperature which contraindicates use of cold compress dressings If burn caused by hot tar, mineral oil to remove it
- 19. Outpatient Management • For 1st and 2nd degree burns less than 10% BSA • Blisters should be left intact and dressed with silver sulfadiazine cream • Dressings should be changed daily washing with lukewarm water to remove any cream left
- 21. Recommendations for Hospitalization 1. Total burns >10% BSA or >2% full thickness, halved for <2 or >40 yr 2. Hands, face, feet or genitalia involved 3. Evidence or suspicion of inhalation injury 4. Associated injuries present 5. Suspicion that burn inflicted 6. Burn is infected 7. Burn circumferential 8. History of prior medical illness 9. Patient is comatose 10.Patient or family unable to cope with situation
- 22. Hospital Management 1. General assessment and cardiopulmonary stabilization 2. Resuscitation 3. Establishment of IV lines and blood studies 4. Wound care and infection control 5. Pain relief and psychological support 6. Nutritional support 7. Physical Therapy/Occupational Therapy
- 23. Airway compromise? Respiratory distress? Circulatory compromise? Intubation, 100% O2 IV access, fluids Multiple trauma? Yes No Evaluate & treat injuries Burns >15% or complicated burns? Yes No Burn care, tetanus prophylaxis, analgesia IV access; fluid replacement Circumferential full thickness burns? Escharotomy Yes Yes No No
- 24. Initial Procedures • Fluid infusion must be started immediately • NGT insertion to prevent gastric dilatation, vomiting and aspiration • Urinary catheter to measure urine output • Weight important and has to be taken daily • Local treatment delayed till respiratory distress and shock controlled • Hematocrit and bacterial cultures necessary
- 25. Fluid Resuscitation • For most, Parkland formula a suitable starting guide (4 ml Ringer’s Lactate/kg body weight/% BSA burned), ½ to be given over 1st 8 hr from time of onset while remaining over the next 16 hr • During 2nd 24 hr, ½ of 1st day fluid requirement to be infused as D5LR • Oral supplementation may start 48 hr after as homogenized milk or soy-based products given by bolus or constant infusion via NGT • Albumin 5% may be used to maintain serum albumin levels at 2 g/dl • Packed RBC recommended if hematocrit falls below 24% (Hgb <8 g/dl) • Sodium supplementation may be needed if burns greater than 20% BSA
- 26. Inhalation Injury • Three syndromes: 1. Early CO poisoning, airway obstruction & pulmonary edema major concerns 2. ARDS usually at 24-48 hrs or much later 3. Pneumonia and pulmonary emboli as late complications (days to weeks) • Assessment: 1. Observation (swelling or carbonaceous material in nasal passages 2. Laboratory determination of carboxyhemoglobin and ABGs • Treatment: 1. Maintain patent airway by early ET intubation, adequate ventilation and oxygenation 2. Aggressive pulmonary toilet and chest physiotherapy
- 27. Infection Control • Tetanus prophylaxis: 250-500 IU TIG or 3000 units equine ATS ANST IM; Toxoid also • Antibiotic of choice is one that will include Pseudomonas in its spectrum; most frequent pathogens in burns are Staphylococcus aureus, Pseudomonas aeruginosa and the Klebsiella- Enterobacter species • Topical therapy: 0.5% Silver nitrate dressing Mafenide acetate or Sulfacetamide acetate cream Silver sulfadiazine cream Povidone-iodine ointment Gentamicin cream or ointment
- 28. Pain Relief and Adjustment • Important to provide adequate analgesia, anxiolytics and psychological support to: a) Reduce early metabolic stress b) Decrease potential for posttraumatic stress syndrome c) Allow future stabilization and rehabilitation • Family support patient through grieving process and help accept long-term changes in appearance
- 29. Nutritional Support • Shriners Burn Institute at Galveston, Texas Guidelines for Caloric Intake Infants 1000 kcal/m2 BSA burned + 2100 kcal/m2 total BSA 2-15 years 1300 kcal/m2 BSA burned + 1800 kcal/m2 total BSA Adolescents 1500 kcal/m2 BSA burned + 1500 kcal/m2 total BSA
- 30. Complications of Burns • Burn Shock • Pulmonary complications due to inhalation injury • Acute Renal Failure • Infections and Sepsis • Curling’s ulcer in large burns over 30% usually after 9th day • Extensive and disabling scarring • Psychological trauma • Cancer called Marjolin’s ulcer, may take 21 years to develop
- 31. THANK YOU