CapstonePosterProject
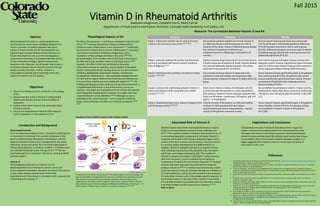
- 1. Vitamin D in Rheumatoid Arthritis Abstract Objectives Introduction and Background Physiological Aspects of RA Associated Role of Vitamin D Research: The Correlation Between Vitamin D and RA Implications and Conclusions References Fall 2015 Madysen Jourgensen, Elizabeth Harris, Molly Carroll Department of Food Science and Human Nutrition, Colorado State University, Fort Collins, CO. (Lang PO, Aspinall R, 2015)10 Purpose Methods Results Study 1: Determine whether serum vitamin D levels influence the recurrence rate of RA.6(1812-1816) RA remission patients divided into normal vitamin D (n=168) and vitamin D deficient groups (n=172) at baseline of the study. Vitamin D deficient group divided into vitamin D treatment (n=84) and non- treatment/control (n=88) groups. Followed for 24 months. Normal vitamin D group had lower recurrence rate (16.7%) of RA with a statistically significant difference (P=0.02) between recurrence rate in control group (29.5%). Difference between recurrence rate of vitamin D treatment group (19.0%) and control group was not statistically significant (P=0.11). Study 2: Discover whether RA activity and treatment success is correlated with serum vitamin D levels at time of diagnosis.3(1-8) Patients recently diagnosed with RA (n=37) had vitamin D levels measured at baseline of study. Patients divided into low and adequate vitamin D groups. RA activity observed in two groups for 12 months. Low vitamin D group had higher disease activity than adequate vitamin D group. Significantly lower remission rates (P<0.001) in low vitamin D group (16% remission) versus adequate vitamin D group (68% remission). Study 3: Determine the correlation of vitamin D levels and RA.7(1994-2001) Serum levels of active vitamin D measured in RA patients (n=130) and healthy control group (n=80). Disease activity compared to vitamin D status within RA group. Serum vitamin D levels significantly lower in RA patients than control group (P<0.01). RA patients with severe disease activity had significantly lower vitamin D levels compared to RA patients with moderate and low disease activity (P<0.01). Study 4: Examine the relationship between vitamin D status and incidence of RA using electronic health records.8(1475-1479) Most recent vitamin D status of individuals with RA (n=270) and non-RA controls (n=1,341) compared in final analysis. Vitamin D levels of groups analyzed with three cut-off values – continuous, <30 ng/mL, and <20 ng/mL – and compared. No correlation found between vitamin D status and RA development. Odds ratios RA vs. controls at continuous, <30 ng/mL, and <20 ng/mL vitamin D levels: 1.00, 0.98, 1.12. Study 5: Understand how serum vitamin D relates to RA and RA disease activity.9(246-250) Vitamin D levels of RA patients (n=181) and healthy controls (n=186) assessed with diet history questionnaires and serum measurements. Disease activity of RA patients evaluated as well. Serum vitamin D levels significantly lower in RA patients versus healthy controls (P<0.01), but disease activity not correlated to vitamin D levels in RA patients (P=0.129). Rheumatoid arthritis (RA) is a serious autoimmune disease that can cause severe disability. Research has shown a possible correlation between low serum vitamin D levels and the risk for developing RA and experiencing increased disease activity. Because it is known that vitamin D acts as an immunoregulatory component in the body, it is hypothesized that vitamin D may moderate an antigen-specific autoimmune response in RA. However, not all studies have shown a correlation between serum vitamin D and RA risk and disease activity; therefore, further research is encouraged to provide more knowledge about the relation of vitamin D to the disease. 1. Discuss the disease process, symptoms, and etiology of RA. 2. Discuss how the nutrient vitamin D could possibly relate to the disease process of RA and affect its symptoms. 3. Analyze what recent research has concluded about vitamin D and RA. 4. Discuss the implications of vitamin D/RA research and its importance in the treatment of RA. Rheumatoid Arthritis RA is an autoimmune disease that is classified by affecting five or more joints in the body. The synovial membrane of the joints is predominantly affected by inflammation, and this leads to corrosion of bones and cartilage which may cause deformity.1 Across the world, RA is the most widespread of inflammatory diseases. In America, it affects 1.5 million adults and 294,000 individuals under the age of 18.2(4403) RA can eventually lead to an individual’s demise by causing disability and early death.1 Vitamin D The biologically active form of vitamin D (1,25- dihydroxyvitamin D) contributes to calcium, bone and immunological homeostasis. Research has shown that vitamin D may reduce disease activity levels of RA while hypovitaminosis D has shown a correlation with increased risk of developing the disease.3(2) RA affects the synovium – a soft-tissue membrane lining the joint cavity.2(4403) Immune cells and the release of inflammatory cytokines create inflammation in this membrane.4(1-2) Eventually, the synovium thickens due to chronic inflammation,4(1) causing a restriction of movement, hindrance of ligaments, and a breakdown of the cartilage and bone in the joint.2(4403) RA generally begins in the smaller joints of the body, commonly in the feet and hands, and later moves to the larger joints.2(4404) However, the effects of RA are not limited to the joints. Inflammation known as vasculitis may be present in the blood vessels, limiting flow blood, causing ulcers on the skin and heart problems. Additionally, rheumatoid nodules – hard bumps resulting from inflammation – may eventually develop beneath the skin and on organs. Reduced bone density and osteoporosis can occur from mobility loss and inadequate vitamin D.4(2-6) The etiology and disease process of RA are not yet fully understood. It is hypothesized that factors in the environment, such as an infection, may begin the development of RA in those that already have the genetic predisposition; however, no antigen that may cause the disease can be identified.2(4404) Although no cure is available for RA, early treatment – such as disease modifying drugs, physical therapy, and diet, can moderate symptoms.2(4406- 4407) Multiple studies have shown that hypovitaminosis D may be linked to increased disease activity in those suffering from RA.5(61) This could be related to evidence that vitamin D can act as an immunoregulatory component in the body. Vitamin D receptors are located in the primary lymphoid organs, which consist of the bone marrow and the thymus, the chief centers for immune system development and differentiation. In addition, vitamin D receptors are found on several immune cells including mononuclear cells, dendritic cells, activated T and B cells, and antigen-presenting cells. The number of vitamin D receptors on helper T cells (CD4+ T cells) increases after their activation, further emphasizing the apparent involvement of vitamin D in an immune response.5(60) Multiple immune cells have even been found to have the ability to produce vitamin D.10(2045) In relation to autoimmunity, studies show that vitamin D may act primarily through the inhibition of Th1 cell proliferation, which are cells involved in the activation of many other immune cells in the antigen-specific response of the immune system. In the case of RA, vitamin D may inhibit Th1 cell differentiation and proliferation and therefore impede a resultant antigen-specific autoimmune response.5(61-62) Refer to figure 1. Rheumatoid Arthitis. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/arthritis/basics/rheumatoid.htm. Updated November 6, 2014. Accessed October 11, 2015. 2. Laberge M, Cataldo LJ, Alic M. Rheumatoid arthritis. In: Longe JL, eds. Gale Encyclopedia of Medicine. 5th ed. Vol. 7. Farmington Hills, MI: Gale Research Inc; 2015:4403-4408. 3. Franco M, Barchetta I, Iannuccelli C, et al. Hypovitaminosis D in recent onset rheumatoid arthritis is predictive of reduced response to treatment and increased disease activity: a 12 month follow-up study. BMC Musculoskelet Di. March 2015; 16 (53):1- 8. doi: 10.1186/s12891-015-0505-6. 4. Wordsworth P, Holden W. Rheumatoid arthritis. Encyclopedia of Life Sciences. Chichester, England: John Wiley & Sons Ltd; 2006:1- 8. 5. Cutolo M, Otsa K, Uprus M, Paolino S, Seriolo B. Vitamin D in rheumatoid arthritis. Autoimmun Rev. 2007; 7(1): 59-64. doi: 10.1016/j.autrev.2007.07.001. 6. Yang J, Liu L, Zhang Q, Li M, Wang J. Effect of vitamin D on the recurrence rate of rheumatoid arthritis. Exp Ther Med. 2015; 10(1): 1812-1816. doi: 10.3892/etm.2015.2747. 7. Hong Q, Xu J, Xu S, Lian L, Zhang M, Ding C. Associations between serum 25-hydroxyvitamin D and disease activity, inflammatory cytokines and bone loss in patients with rheumatoid arthritis. Rheumatology. 2014; 53(1): 1994-2001. doi: 10.1093/rheumatology/keu173. 8. Cote J, Berger A, Kirchner LH, Bili A. Low vitamin D level is not associated with increased incidence of rheumatoid arthritis. Rheumatol Int. 2014; 34: 1475-1479. doi: 10.1007/s00296-014-3019-x. 9. Matsumoto Y, Sugioka Y, Tada M, et. al. Relationships between serum 25-hydroxycalciferol, vitamin D intake and disease activity in patients with rheumatoid arthritis – TOMORROW study. Mod Rheumatol. 2014; 25(2): 246-250. doi: 10.3109/14397595.2014.952487. 10. Lang PO, Aspinall R. Can we translate vitamin D immunomodulating effect on innate and adaptive immunity to vaccine response? Nutrients. 2015; 7(3): 2044-2060. doi: 10.3390/nu7032044. Considerable amounts of research have been done in regards to vitamin D status and its relationship to the risk and severity of RA. Although most research has shown a positive relationship between vitamin D status and decreased RA activity, some studies have shown no correlation. Due to inconclusive evidence between studies, it is highly suggested that research continue on the topic of vitamin D status and its role in RA. Depiction of how vitamin D works in the immune system The active form of vitamin D is produced in the body through the action of sunlight, the liver, and the kidney. Through intracrine, paracrine, and endocrine signaling in immune cells, vitamin D can assist in both increasing a protective immune response and modulating an over-active immune response. Shown here, vitamin D impairs dendritic cell maturation via an intracrine pathway, inhibiting the proliferation of the helper T-cell and its release of inflammatory cytokines via a paracrine pathway.10(2047-2049)