Cardio Vascular Accident CVA
- 1. Critical Care Situations in Neurological Nursing Increased Intracranial Pressure Delirium CVA
- 2. Increased Intracranial Pressure: Skull as a “closed box” Brain tissue is 78% Intravascular blood is 12% Cerebrospinal fluid is 10 % About 1900 mL in adults Normally volume in = volume out
- 3. Normal ICP is 5-15 mmHg in pt. With HOB at 30 degrees. If sustained pressure above 20 mmHg herniation of the brain is likely, compressing the brainstem Body compensates for minor increases in ICP by increasing CSF absorption, decreased CSF production, as well as changing intracranial blood volume through increased venous outflow
- 4. Cerebral Perfusion Pressure: CPP This is the pressure of the blood flow into the cerebrum, which must be above 30 CPP = MAP - ICP Note the pressure-volume curve:
- 5. What are the factors that raise the ICP? Increased arterial blood pressure (note: MAP is the mean arterial pressure) Maximal constriction of vessels occurs at MAP of 150, maximal dilation at 50 Increased intra-abdominal and intrathoracic pressure (eg valsalva, cardiac) Posture (how high head is in relation to heart)
- 6. More factors that influence ICP Hyper and hypothermia Brain injury = swelling Low oxygen tension = cerebral vessel dilation Increased PaCO2 = cerebral vessel dilation Infection Masses Toxic substances in blood/brain tissue
- 7. Signs and Symptoms of Increased ICP Change in LOC: orientation, restlessness, clouded sensorium. Subtle or dramatic Change in Vital Signs: most important is watching for pattern. Cushing’s Triad (late sign): widening pulse pressure, bradycardia with full bounding pulse, and irregular respirations
- 8. More Signs and Symptoms Changes in pupil size, vision, symmetry, reactivity, as well as ocular and lid movement. Hemiparesis, or other changes in motor function Review decerebrate and decorticate posturing. Both serious, decerebrate is more ominous. Vomiting, headache.
- 9. Brief overview of treatment of Increased ICP Frequent assessment, with attention to subtle changes in LOC and neuro exam Very important to ACT EARLY when symptoms emerge, by the time symptoms are overt, pressure may be hitting the dangerous part of the curve. Maintain calm and non-stimulating environment (think: similar to “aneurysm precautions”) PaO2 at 100%, some physicians will aim for hyperventilatory state, some not. Do avoid excess PaCO2
- 10. Increased ICP Care, continued Team will want to address the cause, and treat it whenever possible (discuss) Debate about use of sedation (discuss pros and cons, situational considerations) Diuresis: osmotic and loop diuretics, watch I & O, note SIADH as serious problem Corticosteroids
- 11. Even More ICP care Maintain normothermia Avoid skin breakdown Maintain nutrition (discuss why) Maintain adequate CPP with BP stable and fairly normo-tensive (physician may have specific boundaries in mind) Maintain ICP as near normal as possible, moniter it.
- 12. CVA: Epidemiology CVA affects over 730,000 people in US yearly One of the top 3 causes of death in US Costs us (in indirect and direct cost) about 41 billion yearly Incidence doubles after age 55, CVA affects more men than women, and African Americans are at a higher risk as well.
- 13. More Epidemiology About 50% Stroke victims in US die About ½ Strokes in US are associated with hypertension 85% strokes occur at home About 50% stroke victims travel to ED by ambulance
- 14. Risk Factors for CVA~Mostly Modifiable Hypertension Heart disease Diabetes High cholesterol Smoking Alcohol and other drug use, esp cocaine Use of Oral Contraceptives History of Migraine Headache Elevated homocysteine Obesity and physical inactivity Diet
- 15. Cerebrovascular Disease that Predisposes to Stroke Cerebral Vessel Abnormalities : arteriosclerosis, aneurysms, arteritis, hypertension*, vasoconstriction Blood Flow Abnormalities : Stenosis, thrombi, emboli Blood Property Abnormalities : coagulation problems, viscosity
- 16. CVA Symptoms Sudden onset of focal neurological deficits, the deficits relate directly to the area of the brain that is affected: visual, motor, sensory, speech most common Talk about stroke scales and their usefulness: NIH full and short scale, the LAPSS—why it matters
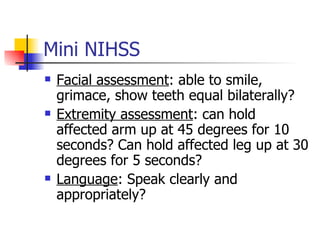
- 17. Mini NIHSS Facial assessment : able to smile, grimace, show teeth equal bilaterally? Extremity assessment : can hold affected arm up at 45 degrees for 10 seconds? Can hold affected leg up at 30 degrees for 5 seconds? Language : Speak clearly and appropriately?
- 18. Pathophysiology of Stroke Brain requires nearly constant supply of Oxygen and Glucose to function. Brain is about 2% of body mass, but uses about 20% of the blood pumped by your heart. Brain has little reserve Oxygen/glucose-therefore TIME IS BRAIN.
- 19. Ischemic Stroke (about 85%): Thrombus and Embolus (pictures) Densely ischemic central core : neuronal tissue undergoes rapid infarction Ischemic prenumbra : larger surrounding area that is compromised re circulation, but because of collateral circulation, tissue remains viable for a variable period of time (several hours)
- 20. Hemorrhagic Stroke: about 15% Hypertension, Aneurysm, malformed vessel, drug use are implicated Assessment findings alone are not definitive to differentiate. May find “worst HA ever, blood in CSF
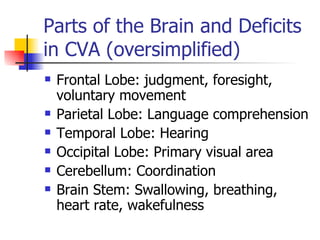
- 21. Parts of the Brain and Deficits in CVA (oversimplified) Frontal Lobe: judgment, foresight, voluntary movement Parietal Lobe: Language comprehension Temporal Lobe: Hearing Occipital Lobe: Primary visual area Cerebellum: Coordination Brain Stem: Swallowing, breathing, heart rate, wakefulness
- 22. A Few More Broca’s Area: speech Wernicke’s Area: speech comprehension Sensory Cortex: pain, heat, and other sensations Motor Cortex : movement
- 23. Diagnosis in Stroke: Essential to be correct~treatment differs Physical Assessment Labs: may see elevated Hgb and Hct if stroke is severe, EKG Blood sugar and electrolytes Stroke mimics hypoglycemia, migraine, seizure CT scan is important Evaluation needs to be rapid. NURSE should be patient advocate and make sure things are going on time:Because time is brain.
- 24. Guidelines for Emergency Stroke Management On arrival: EKG, blood sugar, Vital signs Physician evaluation: 10 minutes Stroke team notification: 15 minutes CT scan : 25 minutes CT interpreted: 45 minutes Drug administration: 60 minutes Monitored bed: 3 hours
- 25. Most Common Nursing Diagnoses (not all) Self care deficits – all Immobility Situational Low Self Esteem Injury, risk for Aspiration, risk for & Impaired swallow Body temp, risk for imbalanced Communication, impaired Unilateral Neglect
- 26. Thrombotic or Embolic Stroke tPA Activase to dissolve clot. 3 hour time window and not for hemorrhagic stroke. 0.9 mg/kg up to 90 mg. First 10% as bolus, rest given over 60 minutes. No ASA or heparin right now (discuss controversy) Manage BP Goal: 140/80 to 150/90 If hypertensive labetrol used (20-40 mg over 2 min), or sodium nitroprusside
- 27. Other Medications: ASA, heparin, anticonvulsants ASA, persantine: Some studies find that ASA given early prevents early recurrence of th/emb. Should be given if no clear diagnosis is possible (even at home before coming in) Anticonvulsants to prevent seizure (which would compound injury Heparin and low molecular weight heparin Some controversy in research findings: the little decrease in thrombus or embolus may be canceled out by the increased risk of intracranial bleeding. Review the use of these drugs, including appropriate lab values to monitor
- 28. Nursing Care Issues in Acute Treatment Keep temperature normal (discuss why) Prevent aspiration and choking while not starving the patient Prevent and assess for thromboembolism Prevent seizures, seizure precautions Assess for depression (common) Keep patient calm-avoid abrupt increases in ICP Aim for good CPP and ICP as close to normal as possible (discuss) Neuro assessment, report changes
- 29. Hemorrhagic Stroke Care Once this type of stroke is diagnosed, there are a few key differences in medical care. First, tPA, ASA, heparin, etc. are contraindicated (a main issue). Later, since 50% of hemorrhagic stroke victims go on to have a thrombotic or embolic stroke, they may be used with caution. Second, depending on the case, surgery may be indicated Third: a medication such as Amicar (an antifibrinolytic) may be used to facilitate a good clot at site of ruptured aneurysm
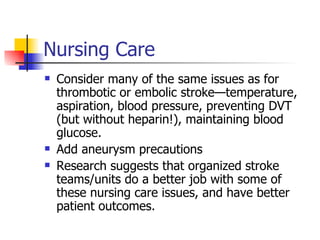
- 30. Nursing Care Consider many of the same issues as for thrombotic or embolic stroke—temperature, aspiration, blood pressure, preventing DVT (but without heparin!), maintaining blood glucose. Add aneurysm precautions Research suggests that organized stroke teams/units do a better job with some of these nursing care issues, and have better patient outcomes.
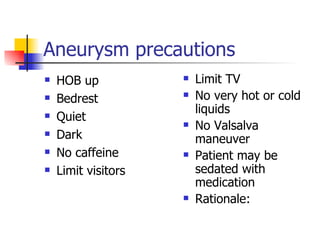
- 31. Aneurysm precautions HOB up Bedrest Quiet Dark No caffeine Limit visitors Limit TV No very hot or cold liquids No Valsalva maneuver Patient may be sedated with medication Rationale:
- 32. Prevention Issues Primary Prevention: work with public to facilitate limiting the modifiable risk factors prior to any illness developing Secondary Prevention: (early detection) Teach public that time is brain and symptoms of stroke to seek treatment for right away. Talk about ASA.
- 33. Tertiary Prevention ASA up to 300 mg/day, or persantine. (discuss research) Coumadin therapy esp if person has A fib. (not good if hemorrhagic stroke) Antihypertensive therapy Improve diet and exercise Carotid endarterectomy especially useful if over 70% blockage ACE inhibition Pravastatin or Simvastatin to decrease hypercholesterol states Stop smoking
- 34. Delirium: Basic Characteristics Disturbance of consciousness or cognition Usually reversible, with acute onset Usually secondary to some other condition or problem, such as intoxication, withdrawl, medical condition, severe stressors
- 35. Delirium: Assessment concerns Review MMS exam. In text. Scrutinize for underlying causes Orientation to time (1 st to go) Orientation to place Orientation to person (last to go) Distractability Ability to converse Level of Consciousness (alert, drowsy, stuporous, etc) Illusions, hallucinations (type, specific, timing) Awareness of own deficits
- 36. Nursing Intervention: Delirium Do what is appropriate to eliminate cause, includes careful assessment Safety: falls, wandering, Ivs/ NGs pulled out easily, may strike out in fear Meet physiologic needs: nutrition, hydration, sleep, appropriate level of stimulation, pain relief Judicious use of antipsychotic,antianxiety meds
- 37. Communication with Confused Person Short questions, instructions, with no “big” words. Be patient. Check for comprehension, give instructions more than once, not in condescending manner Face to face, normal tone, good light No “honey” “dearie” etc
- 38. Reality Orientation with Confused Person Clocks, calendars, cues placed prominently. Talk about it. Names on doors, big. Familiar routine, structure, staff Verbal reorientation to PPT as a natural part of conversation Read text for more interventions!!