Cardiovascular Anatomy.pptx
- 1. Cardiovascular Heart and Blood Vessels Dr. Adanwali Hassan Ahmed Rn-Mw, Medical doctor (MD), Health Officer (HO) Msc-Gyn/Obest.
- 2. Introduction • People always talk about the heart as the seat of control of emotions. • One important reference, however about the heart is that “without a functioning heart, there is no life”. The heart is a muscular organ that is essential for life because it pumps blood through the body. • Emotions are a product of brain function, not heart function but without the heart performing its functions efficiently, brain cells die within a short time! In this unit your knowledge of the structures and the organs in relations to the heart will be explored.
- 3. Objectives • At the end of this unit, you should be able to – Describe the location, size and shape of the heart – Highlight the functions of the heart – List the parts and functions of the pericardium – Contrast the three layers of the heart wall with respect to structure and function – With the aid of a well labeled diagram, describe the position of the heart. – With the aid of a well labeled diagram, describe the pathway for the flow of blood through the heart chambers and large vessels associated with the heart – Describe the vasculature of the heart with the aid of a diagram – Describe structural variations in some abnormalities of the heart and the vessels. – Explain what happens in pericardial effusion and pericarditis
- 4. The Pericardium • The pericardium is a protective sheath that encloses the heart, it has two parts: – The fibrous pericardium and – The serous pericardium. Pericardium: A serous membrane with two layers that surrounds the heart
- 5. Figure 1.1: The Heart and the Coverings
- 6. Cont--- Fibrous pericardium • The pericardium has an outer single-layered fibrous sac that encloses the heart and the roots of the great vessels, fusing with the adventitia of these vessels. • Its broad base overlies the central tendon of the diaphragm, with which it is inseparably blended, both being derived from the septum transversum. Adventitia: An enveloping or covering membrane or layer of body tissue Diaphragm: (anatomy) a muscular partition separating the abdominal and thoracic cavities; functions in respiration
- 7. Cont--- • The phrenic nerves lie on the surface of the fibrous pericardium and the mediastinal pleura is adherent to it, wherever the two membranes are in contact with each other. • The fibrous pericardium is connected to the back of the sternum by weak sternopericardial ligaments. Phrenic nerves: One of a pair of nerves that arises from cervical spinal roots and passes down the thorax to innervate the diaphragm and control breathing Mediastinal: The part of the thoracic cavity between the lungs that contains the heart and aorta and esophagus and trachea and thymus
- 8. Cont--- Serous pericardium • A serous layer lines the inside of the fibrous pericardium, where it is reflected around the roots of the great vessels to cover the entire surface of the heart, where it forms the epicardium. (The innermost of the two layers of the pericardium) • Between these parietal and visceral layers there are two sinuses: the transverse sinus and the oblique sinus of the pericardium.
- 9. Cont--- • The transverse sinus is a passage above the heart, between the ascending aorta and pulmonary trunk in front and the superior vena cava, left atrium and pulmonary veins behind. • The oblique sinus is a space behind the heart, between the left atrium in front and the fibrous pericardium behind, posterior to which lies the oesophagus. • It is through the transverse sinus that a temporary ligature is passed to occlude pulmonary trunk and aorta during pulmonary embolectomy and cardiac operations. Embolectomy: Surgical removal of an embolus (usually from an artery)
- 10. Cont--- • Nerve supply The fibrous pericardium is supplied by the phrenic nerve. The parietal layer of serous pericardium that lines it is similarly innervated, but the visceral layer on the heart surface is insensitive. Pain from the heart (angina) originates in the muscle or the vessels and is transmitted by sympathetic nerves. The pain of pericarditis originates in the parietal layer only and is transmitted by the phrenic nerve.
- 11. Cont--- • Blood supply Pericardial blood supply is derived from the internal thoracic artery, its pericardiophrenic and musculophrenic branches, bronchial arteries and the thoracic aorta. The veins drain into the azygos system. The azygos vein is a vein running up the right side of the thoracic vertebral column draining itself towards the superior vena cava. It connects the systems of superior vena cava and inferior vena cava and can provide an alternative path for blood to the right atrium when either of the venae cavae is blocked
- 12. Cont--- Pericardial drainage • A needle inserted in the angle between the xiphoid process and the left seventh costal cartilage and directed upwards at an angle of 45, towards the left shoulder, passes through the central tendon of the diaphragm into the pericardial cavity. • The creation of a small pericardial window surgically through the same route, or through the anterior end of the fourth intercostal space, provides more effective drainage.
- 13. Gross anatomy of the heart • The heart, slightly larger than a clenched fist, is a double, self-adjusting suction and pressure pump, the parts of which work in unison to propel blood to all parts of the body. • The right side of the heart (right heart) receives poorly oxygenated (venous) blood from the body through the SVC and IVC and pumps it through the pulmonary trunk and arteries to the lungs for oxygenation. • The left side of the heart (left heart) receives well- oxygenated (arterial) blood from the lungs through the pulmonary veins and pumps it into the aorta for distribution to the body.
- 14. Figure 1.2: The Anterior View of the Heart
- 15. Chambers of the heart The heart has four chambers: right and left atria and right and left ventricles. The atria are receiving chambers that pump blood into the ventricles (the discharging chambers). The synchronous pumping actions of the heart's two atrioventricular (AV) pumps (right and left chambers) constitute the cardiac cycle. The cycle begins with a period of ventricular elongation and filling (diastole) and ends with a period of ventricular shortening and emptying (systole).
- 16. Cont--- Two heart sounds are heard with a stethoscope: a lub (1st) sound as the blood is transferred from the atria into the ventricles and a dub (2nd) sound as the ventricles expel blood from the heart. The heart sounds are produced by the snapping shut of the one-way valves that normally keep blood from flowing backward during contractions of the heart.
- 17. Cont--- • The wall of each heart chamber consists of three layers, from superficial to deep: – Endocardium, a thin internal layer (endothelium and subendothelial connective tissue) or lining membrane of the heart that also covers its valves. – Myocardium, a thick, helical middle layer composed of cardiac muscle. – Epicardium, a thin external layer (mesothelium) formed by the visceral layer of serous pericardium.
- 18. Fig. 1.3: Wall of the heart
- 19. The 4 heart valves include the following: 1. Tricuspid valve. Located between the right atrium and the right ventricle. 2. Pulmonary valve. Located between the right ventricle and the pulmonary artery. 3. Mitral valve. Located between the left atrium and the left ventricle. 4. Aortic valve. The heart has four chambers: two atria and two ventricles. The right atrium receives oxygen-poor blood from the body and pumps it to the right ventricle. The right ventricle pumps the oxygen-poor blood to the lungs. The left atrium receives oxygen-rich blood from the lungs and pumps it to the left ventricle.
- 20. Contraction of the heart The walls of the heart consist mostly of myocardium, especially in the ventricles. When the ventricles contract, they produce a wringing motion because of the double helical orientation of the cardiac muscle fibers. This motion initially ejects the blood from the ventricles as the outer (basal) spiral contracts, first narrowing and then shortening the heart, reducing the volume of the ventricular chambers. Continued sequential contraction of the inner (apical) spiral elongates the heart, followed by widening as the myocardium briefly relaxes, increasing the volume of the chambers to draw blood from the atria.
- 21. Cont--- • The muscle fibers are anchored to the fibrous skeleton of the heart. • This is a complex framework of dense collagen forming four fibrous rings (L. anulifibrosi) that surround the orifices of the valves, a right and left fibrous trigone (formed by connections between rings), and the membranous parts of the interatrial and interventricular septa. The right and left fibrous rings of heart (annuli fibrosi cordis) surround the atrioventricular and arterial orifices.
- 22. Fig.1.4: The Musculature and Valves of the Heart
- 23. The fibrous skeleton of the heart: A. Keeps the orifices of the AV and semilunar valves patent and prevents them from being overly distended by an increased volume of blood pumping through them. B. Provides attachments for the leaflets and cusps of the valves. C. Provides attachment for the myocardium, which, when uncoiled, forms a continuous ventricular myocardial band that originates primarily from the fibrous ring of the pulmonary valve and inserts primarily into the fibrous ring of the aortic valve. Aortic valve: A semilunar valve between the left ventricle and the aorta; prevents blood from flowing from the aorta back into the heart
- 24. Cont--- D. Forms an electrical insulator, by separating the myenterically conducted impulses of the atria and ventricles so that they contract independently and by surrounding and providing passage for the initial part of the AV bundle of the conducting system of the heart. Myenteric: A plexus of unmyelinated fibers and postganglionic autonomic cell bodies in the muscular coat of the esophagus and stomach and intestines
- 25. Demarcations Externally, the atria are demarcated from the ventricles by the coronary sulcus (atrioventricular groove), and the right and left ventricles are demarcated from each other by anterior and posterior interventricular (IV) sulci (grooves). The heart appears trapezoidal from an anterior or posterior view, but in three dimensions it is shaped like a tipped-over pyramid with its apex (directed anteriorly and to the left), a base (opposite the apex, facing mostly posteriorly), and four sides. Demarcations: The boundary of a specific area
- 26. Cont--- • The apex of the heart: – Is formed by the inferolateral part of the left ventricle. – Lies posterior to the left 5th intercostal space in adults, usually approximately 9 cm (a hand's breadth) from the median plane. – Remains motionless throughout the cardiac cycle. – Is where the sounds of mitral valve closure are maximal (apex beat); the apex underlies the site where the heart beat may be auscultated on the thoracic wall.
- 27. Cont--- • The base of the heart: – Is the heart's posterior aspect (opposite the apex). – Is formed mainly by the left atrium, with a lesser contribution by the right atrium. – Faces posteriorly toward the bodies of vertebrae T6-T9 and is separated from them by the pericardium, oblique pericardial sinus, esophagus, and aorta. – Extends superiorly to the bifurcation of the pulmonary trunk and inferiorly to the coronary sulcus. – Receives the pulmonary veins on the right and left sides of its left atrial portion and the superior and inferior venacava at the superior and inferior ends of its right atrial portion.
- 28. Cont--- • The four surfaces of the heart are the: – Anterior (sternocostal) surface, formed mainly by the right ventricle. – Diaphragmatic (inferior) surface, formed mainly by the left ventricle and partly by the right ventricle; it is related mainly to the central tendon of the diaphragm. – Right pulmonary surface, formed mainly by the right atrium. – Left pulmonary surface, formed mainly by the left ventricle; it forms the cardiac impression in the left lung. • The heart appears trapezoidal in both anterior and posterior views. Trapezoid: A quadrilateral with two parallel sides
- 29. Cont--- • The four borders of the heart are the: – Right border (slightly convex), formed by the right atrium and extending between the SVC and the IVC. – Inferior border (nearly horizontal), formed mainly by the right ventricle and slightly by the left ventricle. – Left border (oblique, nearly vertical), formed mainly by the left ventricle and slightly by the left auricle. – Superior border formed by the right and left atria and auricles in an anterior view; the ascending aorta and pulmonary trunk emerge from this border and the SVC enters its right side. • Posterior to the aorta and pulmonary trunk and anterior to the SVC, this border forms the inferior boundary of the transverse pericardial sinus.
- 30. Cont--- • The pulmonary trunk, approximately 5 cm long and 3 cm wide, is the arterial continuation of the right ventricle and divides into right and left pulmonary arteries. • The pulmonary trunk and arteries conduct low- oxygen blood to the lungs for oxygenation. Pulmonary trunk: The artery that carries venous blood from the right ventricle of the heart and divides into the right and left pulmonary arteries
- 31. Figure 1.5: The Posterior View of the Heart
- 32. Vasculature of heart The blood vessels of the heart comprise the coronary arteries and cardiac veins, which carry blood to and from most of the myocardium. The endocardium and some subendocardial tissue located immediately external to the endocardium receive oxygen and nutrients by diffusion or microvasculature directly from the chambers of the heart. The blood vessels of the heart, normally embedded in fat, course across the surface of the heart just deep to the epicardium. Occasionally, parts of the vessels become embedded within the myocardium. The blood vessels of the heart are affected by both sympathetic and parasympathetic innervation.
- 33. Arterial supply of heart The coronary arteries, the first branches of the aorta, supply the myocardium and epicardium. The right and left coronary arteries arise from the corresponding aortic sinuses at the proximal part of the ascending aorta, just superior to the aortic valve, and pass around opposite sides of the pulmonary trunk. The coronary arteries supply both the atria and the ventricles; however, the atrial branches are usually small and not readily apparent in the cadaveric heart. The ventricular distribution of each coronary artery is not sharply demarcated.
- 34. Figure 1.6: The Blood Supply of the Heart
- 35. Cont--- • The right coronary artery (RCA) arises from the right aortic sinus of the ascending aorta and passes to the right side of the pulmonary trunk, running in the coronary sulcus. • Near its origin, the RCA usually gives off an ascending sinuatrial nodal branch, which supplies the SA node. • The RCA then descends in the coronary sulcus and gives off the right marginal branch, which supplies the right border of the heart as it runs toward (but does not reach) the apex of the heart
- 36. Cont--- • After giving off this branch, the RCA turns to the left and continues in the coronary sulcus to the posterior aspect of the heart. • At the posterior aspect of the crux (L. cross) of the heart—the junction of the interatrial and interventricular (IV) septa between the four heart chambers—the RCA gives rise to the atrioventricular nodal branch, which supplies the AV node. • The SA and AV nodes are part of the conducting system of the heart.
- 37. Cont--- • Typically, the RCA supplies: – The right atrium. – Most of right ventricle. – Part of the left ventricle (the diaphragmatic surface). – Part of the IV septum, usually the posterior third. – The SA node (in approximately 60% of people). – The AV node (in approximately 80% of people).
- 38. Cont--- • The left coronary artery (LCA) arises from the left aortic sinus of the ascending aorta, passes between the left auricle and the left side of the pulmonary trunk, and runs in the coronary sulcus. • In approximately 40% of people, the SA nodal branch arises from the circumflex branch of the LCA and ascends on the posterior surface of the left atrium to the SA node. • As it enters the coronary sulcus, at the superior end of the anterior IV groove, the LCA divides into two branches, the anterior IV branch (clinicians continue to use LAD, the abbreviation for the former term ―left anterior descending‖ artery) and the circumflex branch
- 39. Cont--- • The anterior IV branch passes along the IV groove to the apex of the heart. Here it turns around the inferior border of the heart and commonly anastomoses with the posterior IV branch of the right coronary artery. • The anterior IV branch supplies adjacent parts of both ventricles and, via IV septal branches, the anterior two thirds of the IVS. • In many people, the anterior IV branch gives rise to a lateral branch (diagonal artery), which descends on the anterior surface of the heart.
- 40. Cont--- • The smaller circumflex branch of the LCA follows the coronary sulcus around the left border of the heart to the posterior surface of the heart. • The left marginal branch of the circumflex branch follows the left margin of the heart and supplies the left ventricle. • Most commonly, the circumflex branch of the LCA terminates in the coronary sulcus on the posterior aspect of the heart before reaching the crux of the heart, but in approximately one third of hearts it continues to supply a branch that runs in or adjacent to the posterior IV groove.
- 41. Cont--- Typically, the LCA supplies: – The left atrium. – Most of the left ventricle. – Part of the right ventricle. – Most of the IVS (usually its anterior two thirds), including the AV bundle of the conducting system of the heart, through its perforating Interventricular ( IV) septal branches. – The SA node (in approximately 40% of people).
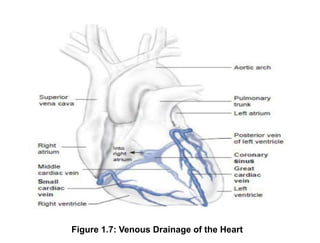
- 42. Venous drainage of the heart The heart is drained mainly by veins that empty into the coronary sinus and partly by small veins that empty into the right atrium. The coronary sinus, the main vein of the heart, is a wide venous channel that runs from left to right in the posterior part of the coronary sulcus. The coronary sinus receives the great cardiac vein at its left end and the middle cardiac vein and small cardiac veins at its right end. The left posterior ventricular vein and left marginal vein also open into the coronary sinus. coronary sinus: A short sinus receiving most of the veins of the heart; empties into the right atrium
- 43. Cont--- The coronary sinus (CS) refers to a collection of veins that join together to form a large blood vessel. • This vein is located between the left atrium and the left ventricle of the heart. • The heart is a vital organ and the central component of the circulatory system. The coronary sulcus, also known as the atrioventricular groove, is a groove that separates the atria and ventricles of the heart. It extends from the upper medial end of the third left costal cartilage to the middle of the right sixth chondrosternal joint.
- 44. Figure 1.7: Venous Drainage of the Heart
- 45. Cont--- • The great cardiac vein is the main tributary of the coronary sinus. • Its first part, the anterior interventricular vein, begins near the apex of the heart and ascends with the anterior IV branch of the LCA. • At the coronary sulcus it turns left and its second part runs around the left side of the heart with the circumflex branch of the LCA to reach the coronary sinus. • (An unusual situation is occurring here: Blood is flowing in the same direction within a paired artery and vein!) The great cardiac vein drains the areas of the heart supplied by the LCA.
- 46. Cont--- • The middle cardiac vein (posterior IV vein) accompanies the posterior interventricular branch (usually arising from the RCA). • A small cardiac vein accompanies the right marginal branch of the RCA. • Thus these two veins drain most of the areas commonly supplied by the RCA. • The oblique vein is the remnant of the embryonic left SVC, which usually atrophies during the fetal period, but occasionally persists in adults, replacing or augmenting the right SVC.
- 47. Cont--- • Some cardiac veins do not drain via the coronary sinus. • Several small anterior cardiac veins begin over the anterior surface of the right ventricle, cross over the coronary sulcus, and usually end directly in the right atrium; sometimes they enter the small cardiac vein. • The smallest cardiac veins (L. venae cordis minimae) are minute vessels that begin in the capillary beds of the myocardium and open directly into the chambers of the heart, chiefly the atria. • Although called veins, they are valveless (To control (flow)) communications with the capillary beds of the myocardium and may carry blood from the heart chambers to the myocardium.
- 48. Lymphatic drainage of the heart o Lymphatic vessels in the myocardium and subendocardial connective tissue pass to the subepicardial lymphatic plexus. o Vessels from this plexus pass to the coronary sulcus and follow the coronary arteries. o A single lymphatic vessel, formed by the union of various lymphatic vessels from the heart, ascends between the pulmonary trunk and left atrium and ends in the inferior tracheobronchial lymph nodes, usually on the right side.
- 49. Innervation of the heart The heart is supplied by autonomic nerve fibers from the cardiac plexus, which is often quite artificially divided into superficial and deep portions. This nerve network is most commonly described as lying on the anterior surface of the bifurcation of the trachea (a respiratory structure), since it is most commonly observed in dissection after removal of the ascending aorta and the bifurcation of the pulmonary trunk. However, its primary relationship is to the posterior aspect of the latter two structures, especially the ascending aorta. Innervation: The neural or electrical arousal of an organ or muscle or gland
- 50. Cont--- The cardiac plexus is formed of both sympathetic and parasympathetic fibers end route to the heart, as well as visceral afferent fibers conveying reflexive and nociceptive fibers from the heart. Fibers extend from the plexus along and to the coronary vessels and to components of the conducting system, particularly the SA node. The sympathetic supply is from presynaptic fibers, with cell bodies in the intermediolateral cell columns (IMLs) of the superior five or six thoracic segments of the spinal cord & postsynaptic sympathetic fibers, with cell bodies in the cervical and superior thoracic paravertebral ganglia of the sympathetic trunks.
- 51. Cont--- The post synaptic fibers traverse cardiopulmonary splanchnic nerves and the cardiac plexus to end in the SA and AV nodes and in relation to the terminations of parasympathetic fibers on the coronary arteries. Sympathetic stimulation causes increased heart rate, impulse conduction, force of contraction and at the same time, increased blood flow through the coronary vessels to support the increased activity. Adrenergic stimulation of the SA node and conducting tissue increases the rate of depolarization of the pacemaker cells while increasing atrioventricular conduction. Splanchnic nerves: Any of several nerves of the sympathetic part of the autonomic nervous system that innervate viscera and blood vessels Adrenergic: sympathomimetic
- 52. Developmental and microanatomy of the heart The cardiovascular system is functionally important in development. Most cells and organs in an embryo do very little except grow and differentiate—the brain, lungs, liver, digestive system, gonads, and kidneys all fall into this category. But the cardiovascular system has to do real work early on.
- 53. Cont--- The reason is that once the embryo has gotten thicker than 200 to 400 microns, the diffusion of nutrients, oxygen and carbon dioxide is inadequate to service an inner mass of very metabolically active cells. A circulatory system is needed to keep these cells from dying and it needs to do it by the middle of the fourth week of gestation (circa embryonic day 24). And this system has to work continuously while undergoing some serious remodeling. Microns: A metric unit of length equal to one millionth of a meter
- 54. Remodelling of the Cardiovascular System with Development • The cardiovascular system is radically remodeled several times during development.The system is revamped at least four times. – It starts out as an approximately bilateral system of contractile blood vessels. Parts coalesce at midline to form a single channel or central pump. – Parts of the contents regresses in the embryo, including some early renal structures (the mesonephros). As a result entire systems of veins (and some embryonic arteries) also regress.Virtually the entire posterior cardinal venous system gets re-absorbed
- 55. Cont--- – The heart gets split into two pumps.The right side basically pumps blood straight into the descending aorta (through the ductus arteriosus shunt).The left side pumps blood into the rapidly growing cranium and brain. – At birth the whole pattern of circulation has to be modified radically in a matter of minutes.The main objectives are to shut down the chorionic/placental circulation and open up the pulmonary circulation. Arteriosus: A blood vessel in a fetus that bypasses pulmonary circulation by connecting the pulmonary artery directly to the ascending aorta; normally closes at birth
- 56. The cardiovascular system is not just made up of splanchnic mesoderm. • The heart also gets a critical influx of cells from the neural crest. • These crest cells contribute to the formation of the endocardial cushions, which in turn are critical in converting a simple one-chamber pump into a complex two-chambered heart with sophisticated valves. • They may be called "neural" crest, but these cells have an almost miraculous ability to make different types of tissues (cranial skeleton, adrenals, neurons, glia, even muscles in the ciliary body). Splanchnic: Relating to or affecting the viscera Miracle: Any amazing or wonderful occurrence
- 57. Cont---- • The heart and arterial trunk are split into the adult compartments by six growing walls of tissue (septae). • Septum primum: This first septum grows down the middle of the common atrium and eventually fuses with tissues that surround the narrow lumen between the atrium and ventricle (there is only one atrium and one ventricle at this point in the 5th week of gestation).
- 58. Cont---- • Septum secundum: This slow growing second atrial septum grows parallel to the 1st septum, but is delayed by a couple of weeks. It is a more robust wall. Both the 1st and 2nd septums (septae) have big holes in them. • To make it rough on you the hole in the first septum is called the second hole or for formal types, the foramen secundum • The hole in the second septum is called the foramen ovale
- 59. Cont---- • AV septum/endocardial cushion: The endocardial cushions give rise to most of the cardiac skeleton that splits the atrial and ventricular sides of the heart. The cushions also build mitral and tricuspid valves. • Interventricular septum, muscular part: A septum can also form when a central region grows particularly slowly. – The surrounding tissue can bulge outward and fuse. This may be the mode by which the interventricular septum forms.
- 60. Cont---- • Interventricular septum, membranous part: May be you have felt this part of the septum in the Gross Lab, tucked out of sight in the aortic vestibule, maybe not. – When this membrane forms from a motley crew of cells from the endocardial cushions and the bulbar ridges, the heart is finally four-chambered.
- 61. Cont---- • Aortico-pulmonary septa, bulbar ridges: There is no pulmonary trunk at early stages, just one big common arterial outflow, called the truncus arteriosus, that delivers all blood to an aortic sac. Truncus: A bundle of modified heart muscle that transmits the cardiac impulse from the atrioventricular node to the ventricles causing them to contract
- 62. Heart development, also known as cardiogenesis, refers to the prenatal development of the heart. – This begins with the formation of two endocardial tubes which merge to form the tubular heart, also called the primitive heart tube. – The heart is the first functional organ in vertebrate embryos.
- 64. Microanatomy of the great vessels The cardiovascular system may be divided into four major components: the Heart, the Macrocirculation, the Microcirculation and the Lymph vascular system. Essentially, the macrocirculation comprises all vessels, both arteries and veins that would be visible to the eye. The vessels of the macrocirculation supply and drain a network of fine vessels interposed between them, the capillaries. This network is also called the capillary bed.
- 65. Cont---- • Water and other components of the blood plasma which exude from the blood vessels form the interstitial fluid, which is returned to the circulation by the lymph vascular system.
- 66. General Structure of Blood Vessels The histological appearances of vessels are different sizes (arterioles vs arteries) and different types (arteries vs. veins) are different from each other. ( seen these in the laboratory). These differences are the result of quantitative variations of a common structural pattern that can be seen in all blood vessels with the exception of capillaries, i.e. the division of the walls of the blood vessels into three layers or tunics. Arterioles: One of the small thin-walled arteries that end in capillaries
- 67. Cont---- 1. The Tunica intima: The innermost membrane of an organ (especially the inner lining of an artery, vein or lymphatic vessel) • Tunica intima limits the vessel wall towards the lumen of the vessel and comprises its endothelial lining (typically simple, squamous) and associated connective tissue. • Beneath the connective tissue, we find the internal elastic lamina, which delimits the tunica intima from the Tunica media. Tunics: An enveloping or covering membrane or layer of body tissue
- 68. Cont---- 2. The Tunica media The Tunica media is formed by a layer of circumferential smooth muscle and variable amounts of connective tissue. A second layer of elastic fibers, the external elastic lamina, is located beneath the smooth muscle. It delimits the tunica media from the tunica adventitia, which consist of mainly of connective tissues fibers. Tunica: An enveloping or covering membrane or layer of body tissue The tunica intima is the innermost tunica (layer) of an artery or vein. It is made up of one layer of
- 69. Cont---- 3. Tunica adventitia • The tunica adventitia blends with the connective tissue surrounding the vessel. • The definition of the outer limit of the tunica adventitia is therefore somewhat arbitrary. Blends: An occurrence of thorough mixing
- 70. Cont---- Vasa Vasorum Any small blood vessel ramifying on the outside of a major artery or vein • A blood vessel that supplies the vessel that supplies blood to the wall of the vessel. • it supplies nutrients to the blood vessel.
- 71. Fig. 1.8: Histology of a blood vessel.(showing layers of the blood vessel wall including the intima, media and adventitia)
- 72. Fig. 1.9: VARIATIONS OF VESSEL WALL STRUCTURES Arteries
- 73. Cont---- • All arterial vessels originate from either the pulmonary trunk (from the right ventricle) or the aorta (from the left ventricle). Specializations of the walls of arteries relate mainly to two factors: the pressure pulses generated during contractions of the heart (systole) and the regulation of blood supply to the target tissues of the arteries. • The tunica media is the main site of histological specializations in the walls of arteries. • Vessels close to the heart (aorta, pulmonary trunk and the larger arteries that originate from them) are elastic arteries.
- 74. Elastic arteries o The tunica intima of elastic arteries is thicker than in other arteries. o A layer of loose connective tissue beneath the endothelium (subendothelial connective tissue) allows the tunica intima to move independently from other layers as the elastic arteries distend with the increase in systolic blood pressure. o Distension of the walls is facilitated by concentric fenestrated lamellae of elastic fibres in a thick tunica media. o In adult humans, about 50 elastic lamellae are found in the tunica media of the aorta. Intima: The inner most membrane of an organ (especially the inner lining of an artery, vein or lymphatic vessel)
- 75. Cont--- o The energy stored in the elastic fibres of the tunica media allows elastic arteries to function as a "pressure reservoir" which forwards blood during ventricular relaxation (diastole). o Smooth muscle cells and collagen fibres are present between the layers of elastic fibres. o Both fibre types are produced by the smooth muscle cells.
- 76. Cont--- o Each elastic lamella forms together with interlamellar fibres and cells to form a lamellar unit. o The external elastic lamina is difficult to discern (understand) from other layers of elastic fibres in the tunica media. o The tunica adventitia appears thinner than the tunica media and contains collagen fibers and the cell types typically present in connective tissue. The internal elastic lamina or internal elastic lamella is a layer of elastic tissue that forms the outermost part of the tunica intima of blood vessels
- 77. Cont---- o The walls of these large arteries are so thick that their peripheral parts cannot derive enough oxygen and nutrients from the blood of the vessel that they form. o Larger vessels are therefore accompanied by smaller blood vessels which supply the tunica adventitia and, in the largest vessels, the outer part of the tunica media of the vessel wall. o The vessels are called vasa vasorum. o In macroscopic preparations vasa vasorum are visible as fine dark lines on the surface of the larger arteries.
- 78. Cont---- o The diameter of individual arteries decreases as we follow them further into the periphery. o However, their total diameter increases, which leads to a fall in blood pressure. Also, the properties of the elastic arteries have to some extent evened out differences in diastolic and systolic blood pressure. o The amount of elastic fibres in the tunica media decreases with these physiological changes.
- 79. Muscular arteries The tunica intima is thinner than in elastic arteries. Subendothelial connective tissue other than the internal elastic lamina is often difficult to discern. The internal elastic lamina forms a well- defined layer. • The tunica media is dominated by numerous concentric layers of smooth muscle cells. Fine elastic fibers and a few collagen fibers are also present. • The external elastic lamina can be clearly distinguished although it may be incomplete in places. The thickness and appearance of the tunica adventitia is variable.
- 80. Fig.1 Arterioles
- 81. Arterioles • Arterioles are arterial vessels with a diameter below 0.1 - 0.5 mm (different values in different textbooks). • Endothelial cells are smaller than in larger arteries, and the nucleus and surrounding cytoplasm may 'bulge' slightly into the lumen of the arteriole. • The endothelium still rests on an internal elastic lamina, which may be incomplete and which is not always well-defined in histological sections.
- 82. Cont---- • The tunica media consists of 1-3 concentric layers of smooth muscle cells. It is difficult to identify an external elastic lamina or to distinguish the tunica adventitia from the connective tissue surrounding the vessel. • The smooth muscle of arterioles and, to some extent, the smooth muscle of small muscular arteries regulate the blood flow to their target tissues. • Arterioles receive both sympathetic and parasympathetic innervation. • The final branching of the arterioles finally gives rise to the capillary network (microcirculation).
- 83. Capillaries • The sum of the diameters of all capillaries is significantly larger than that of the aorta (by about three orders of magnitude), which results in decreases in blood pressure and flow rate. • Also, capillaries are very small vessels. • Their diameter ranges from 4-15 μm.
- 84. Cont---- • The wall of a segment of capillary may be formed by a single endothelial cell. This results in a very large surface to volume ratio. The low rate of blood flow and large surface area facilitate the functions of capillaries in Providing nutrients and oxygen to the surrounding tissue, the absorption of nutrients, waste products and carbon dioxide, and the excretion of waste products from the body.
- 85. Cont---- • Three types of capillaries can be distinguished based on features of the endothelium. Continuous capillaries - are formed by "continuous" endothelial cells and basal lamina. The endothelial cell and the basal lamina do not form openings, which would allow substances to pass the capillary wall without passing through both the endothelial cell and the basal lamina. Both endothelial cells and the basal lamina can act as selective filters in continuous capillaries.
- 86. Cont---- Fenestrated capillaries -endothelial cell body forms small openings called fenestrations, which allow components of the blood and interstitial fluid to bypass the endothelial cells on their way to or from the tissue surrounding the capillary.
- 87. Cont---- • Discontinuous capillaries- are formed by fenestrated endothelial cells, which may not even form a complete layer of cells. The basal lamina is also incomplete. Discontinuous capillaries form large irregularly shaped vessels, sinusoids or sinusoid capillaries. They are found where a very free exchange of substances or even cells between bloodstream and organ is advantageous
- 90. Venules They are larger than capillaries. Small venules are surrounded by pericytes (A few smooth muscle cells may surround larger venules). The venules merge to form Small to medium-sized veins which contain bands of smooth muscle in the tunica media. The tunica adventitia is well developed. In some veins (e.g. the veins of the pampiniform plexus in the spermatic cord) the tunica adventitia contains longitudinally oriented bundles of smooth muscle. Venules: A minute vein continuous with a capillary
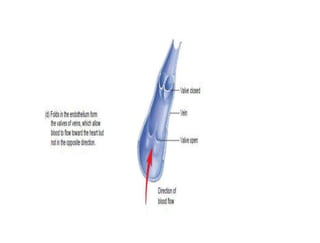
- 91. Cont--- • Aside from most veins in the head and neck, small to medium-sized veins are also characterized by the presence of valves. • The valves are formed by loose, pocket-shaped folds of the tunica intima, which extend into the lumen of the vein. • The opening of the pocket will point into the direction of blood flow towards the heart. One to three (usually two) pockets form the valve.
- 92. Cont--- • Blood flowing towards heart will pass the pockets. If the flow reverses, blood will fill the pockets which will occlude the lumen of the vein and prevent the return of blood into the part of the vein preceding the valve. • The ability of the valves to prevent backflow depends to some extent on the state of contraction (tone) of the smooth muscle in the wall of the vein.
- 94. Cont---- • The largest veins of the abdomen and thorax do contain some subendothelial connective tissue in the tunica intima, but both it and the tunica media are still comparatively thin. • Collagen and elastic fibres are present in the tunica media. • The tunica adventitia is very wide, and it usually contains bundles of longitudinal smooth muscle.
- 95. Cont---- • The transition from the tunica adventitia to the surrounding connective tissue is gradual. Valves are absent. • Vasa vasorum are more frequent in the walls of large veins than in that of the corresponding arteries - probably because of the lower oxygen tension in the blood contained within them.
- 97. Lymphatic system Parts of the blood plasma will exude from the blood vessels into the surrounding tissues because of transport across the endothelium or because of blood pressure and the fenestration of some capillaries (this process is partly counteracted by the higher osmotic pressure of the blood). The fluid entering tissues from capillaries adds to the interstitial fluid normally found in the tissue. The surplus of liquid needs to be returned to the circulation. Lymph vessels are dedicated to this unidirectional flow of liquid, the lymph.
- 98. Cont---- • Three types of lymph vessels can be distinguished based on their size and morphology 1. Lymph capillaries are somewhat larger than blood capillaries and very irregularly shaped. They begin as blind-ending tubes in connective tissue. Temporary openings in the endothelial lining of the lymph capillaries also allow the entry of larger particles into the lymph capillaries (lipid droplets, which are absorbed from the lumen of the gut do not enter blood capillaries, but enter the circulation via lymph vessels which are found in the villi of the ileum and jejunum).
- 99. Cont---- 2. Lymph collecting vessels which are larger and form valves but otherwise appear similar to lymph capillaries. The lymph is moved by the compression of the lymph vessels by surrounding tissues. The direction of lymph flow is determined by the valves. Lymph vessels empty intermittently into lymph nodes from which the lymph continues in efferent lymph vessels. Only very little lymph is returned from the limbs if they are immobilized, which illustrates the importance of muscular action in lymph transport.
- 100. Cont---- 3. Lymph ducts which contain one or two layers of smooth muscle cells in their wall (some textbooks call this layer the tunica media of lymph vessels). The walls of the lymph ducts are less flexible in the region of the attachment of the valves to the wall of the duct, which may give a beaded appearance to the lymph ducts. Peristaltic contractions of the smooth muscle contribute to the movement of lymph towards the heart in addition to the compression of the ducts by surrounding tissues.
- 101. Cont---- The largest lymph duct of the body, the thoracic duct, drains lymph from the lower half and upper left quadrant of the body and empties the lymph into the circulation by merging with the vascular system close to the junction of the left internal jugular and subclavian veins. That it is the largest lymph duct does not mean that it is a large vessel when compared to the large arteries and veins. It actually is not much larger (about 5mm in diameter) than one of the superficial forearm veins.
- 103. Clinical correlates i) Stroke or Cerebrovascular Accident Thrombi (clots) form on the walls of the left atrium in certain types of heart disease. If these thrombi detach or pieces break off from them, they pass into the systemic circulation and occlude peripheral arteries. Occlusion of an artery supplying the brain results in a stroke or cerebrovascular accident (CVA), which may affect vision, cognition or the motor function of parts of the body previously controlled by the now- damaged (ischemic) area of the brain.
- 104. Cont---- ii) Valvular Heart Disease o Disorders involving the valves of the heart disturb the pumping efficiency of the heart. o Valvular heart disease produces either stenosis (narrowing) or insufficiency. o Stenosis is the failure of a valve to open fully, slowing blood flow from a chamber. o Insufficiency or regurgitation, on the other hand, is failure of the valve to close completely, usually owing to nodule formation on (or scarring and contraction of) the cusps so that the edges do not meet or align.
- 105. Cont---- o This allows a variable amount of blood (depending on the severity) to flow back into the chamber it was just ejected from. o Both stenosis and insufficiency result in an increased workload for the heart. o Because valvular diseases are mechanical problems, damaged or defective cardiac valves can be replaced surgically in a procedure called valvuloplasty. o Most commonly, artificial valve prostheses made of synthetic materials are used in these valve-replacement procedures, but xenografted valves (valves transplanted from other species, such as pigs) are also used. The term xenograft refers to a tissue or organ that is derived from a species that is different from the recipient of the specimen. Heart valve disease occurs when one or more of the heart valves do not open or close properly.
- 106. Cont---- iii) Pulmonary valve stenosis • In pulmonary valve stenosis, the valve cusps are fused, forming a dome with a narrow central opening. • In infundibular pulmonary stenosis, the conus arteriosus is underdeveloped. • Both types of pulmonary stenoses produce a restriction of right ventricular outflow and may occur together. The degree of hypertrophy of the right ventricle is variable. Infundibular: Any of various funnel-shaped parts of the body (but especially the hypophyseal stalk)
- 107. Cont---- iv) Pulmonary valve incompetence If the free margins (lunules) of the cusps of a semilunar valve thicken and become inflexible or are damaged by disease, the valve will not close completely. An incompetent pulmonary valve results in a backrush of blood under high pressure into the right ventricle during diastole. Pulmonic regurgitation may be heard through a stethoscope as a heart murmur, an abnormal sound from the heart, produced in this case by damage to the cusps of the pulmonary valve.
- 108. Cont---- v) Aortic valve stenosis Aortic stenosis occurs when the aortic valve narrows and blood cannot flow normally. The condition may range from mild to severe. Over time, aortic valve stenosis causes your heart's left ventricle to pump harder to push blood through the narrowed aortic valve. vi) Aortic valve insufficiency Aortic regurgitation (AR), also known as aortic insufficiency, is a form of valvular heart disease in which the integrity of the aortic valve is compromised and leads to inadequate closure of the valve leaflets. A normal aortic valve is comprised of three semilunar cusps that attach to the aortic wall.
- 109. Cont---- vii) Echocardiography • Echocardiography (ultrasonic cardiography) is a method of graphically recording the position and motion of the heart by the echo obtained from beams of ultrasonic waves directed through the thoracic wall. • This technique may detect as little as 20 mL of fluid in the pericardial cavity, such as that resulting from pericardial effusion.
- 110. Cont---- • Doppler echocardiography is a technique that demonstrates and records the flow of blood through the heart and great vessels by Doppler ultrasonography, making it especially useful in the diagnosis and analysis of problems with blood flow through the heart, such as septal defects, and in delineating valvular stenosis and regurgitation, especially on the left side of the heart.
- 111. Cont---- An echocardiogram, or "echo", is a scan used to look at the heart and nearby blood vessels. It's a type of ultrasound scan, which means a small probe is used to send out high-frequency sound waves that create echoes when they bounce off different parts of the body.
- 112. Cont---- Viii) Coronary atherosclerosis • The atherosclerotic process, characterized by lipid deposits in the intima (lining layer) of the coronary arteries, begins during early adulthood and slowly results in stenosis of the lumina of the arteries • As coronary atherosclerosis progresses, the collateral channels connecting one coronary artery with the other expand, which may initially permit adequate perfusion of the heart during relative inactivity.
- 113. Cont---- • Despite this compensatory mechanism, the myocardium may not receive enough oxygen when the heart needs to perform increased amounts of work. • Strenuous exercise, for example, increases the heart's activity and its need for oxygen. • Insufficiency of blood supply to the heart (myocardial ischemia) may result in MI.
- 114. Cont---- ix) Slowly progressive coronary artery disease • In slow occlusion of a coronary artery, the collateral circulation has time to increase so that adequate perfusion of the myocardium can occur when a potentially ischemic event occurs. • Consequently, MI may not result. • On sudden blockage of a large coronary branch, some infarction is probably inevitable, but the extent of the area damaged depends on the degree of development of collateral anastomotic channels. • If large branches of both coronary arteries are partially obstructed, an extracardiac collateral circulation may be used to supply blood to the heart
- 115. Cont---- X) Transplantation • The patient‘s heart is removed by incisions through the aorta, pulmonary trunk and both atria. • The incision line through the right atrium leaves the two vena cava, the posterior wall of the atrium and the region of the SA node in situ. • The posterior part of the left atrium with the four pulmonary vein orifices is also left intact. • The donor heart is trimmed through the atria to match up with the remains of the patient‘s atria, although the lower end of the donor superior vena cava remains attached to the right atrium so that the donor heart retains its own SA node.
- 116. Cont---- • For combined heart–lung transplantation, the donor block is removed through the trachea, right atrium and aorta, and sutured to the recipient in that order.
- 117. END END
Editor's Notes
- The septum transversum is a thick mass of cranial mesenchyme, formed in the embryo, that gives rise to parts of the thoracic diaphragm and the ventral mesentery of the foregut in the developed human being and other mammals
- Pericardium: A serous membrane with two layers that surrounds the heart
- The oblique sinus is an inverted J-shaped reflection of the venae cavae and pulmonary veins. It lies behind the atria (particularly the left atrium), and in between left and right pulmonary veins
- Phrenic nerve: One of a pair of nerves that arises from cervical spinal roots and passes down the thorax to innervate the diaphragm and control breathing
- Wringing: Twist and press out of shape….. Ejects: Put out or expel from a place
- Atrioventricular….. semilunarResembling the new moon in shape
- What is the vena cava? The superior vena cava and inferior vena cava are very large veins that bring deoxygenated blood to your heart to get oxygen. Your inferior vena cava, your body's largest vein, carries oxygen-depleted blood back to your heart from the lower part of your body (below your diaphragm)
- Auricle: A small conical pouch projecting from the upper anterior part of each atrium of the heart
- sinoatrial node
- coronary sinus: A short sinus receiving most of the veins of the heart; empties into the right atrium. Tributary: (of a stream) flowing into a larger stream
- Remnant: A small part or portion that remains after the main part no longer exists…… augmenting: Enlarge or increase
- coronary sinus: A short sinus receiving most of the veins of the heart; empties into the right atrium… The venae cordis minimae (singular: vena cordis minima), meaning "smallest cardiac veins", also known as Thebesian veins
- Bifurcation: The place where something divides into two branches
- Nociceptive: Caused by or in response to pain
- Parasympathetic: Originates in the brain stem and lower part of the spinal cord; opposes physiological effects of the sympathetic nervous system: stimulates digestive secretions; slows the heart; constricts the pupils; dilates blood vessels
- Coalesce: Add together different elements
- Mesoderm: The middle germ layer that develops into muscle and bone and cartilage and blood and connective tissue..
- Interstitial: is dhexgalka
- Arterioles: One of the small thin-walled arteries that end in capillaries
- Circumferential: wareegsan… lamina: A thin plate or layer…. Delimits: kalabixin
- Concentric: Having a common center….. The internal elastic lamina or internal elastic lamella is a layer of elastic tissue that forms the outermost part of the tunica intima of blood vessels
- Pinocytosis:Process by which certain cells can engulf and incorporate droplets of fluid
- The pampiniform plexus is a network of veins arising from the testicular venous outflow. It begins in the scrotum and extends into the spermatic cord, then coalesces to form the gonadal vein, which travels through the inguinal canal and into the retroperitoneum
- Villi: A minute hairlike projection on mucous membrane
- The term clinical correlation is a broad concept and can incorporate medical concepts and clinical associations at multiple levels of detail. For example, they can be very superficial, such as the relationship of histology to a disease condition during a didactic lecture.
- A valvuloplasty (also called a valvotomy) is a minimally invasive structural heart disease treatment to open a narrowed heart valve. Narrowing of heart valves (valve stenosis) can restrict blood flow and cause symptoms such as chest pain or shortness of breath
- Semilunar: Resembling the new moon in shape
- MI Destruction of heart tissue resulting from obstruction of the blood supply to the heart muscle……………….. Anastomosis: A natural or surgical joining of parts or branches of tubular structures so as to make or become continuous
- Transplantation is a surgical procedure in which an organ/s, tissue or a group of cells are removed from one person (the donor) and surgically transplanted into another person (the recipient), or moved from one site to another site in the same person