Integrated health & social care: service transformation supported by technology – Kent County Council: Alison Davis (NHS)
- 1. Alison Davis Director Integrated Care, North Kent 17th June 14 Integrated Health & Social Care: service transformation supported by technology
- 2. • Brief Introduction to the complexities of the Health and Social Care system in Kent • History of use of telehealth/telecare ,whole system demonstrator and what we learned • Current agenda including pioneer programme and Better Care Fund (BCF) • North Kent approach to the Integration of Health and Social Care Content
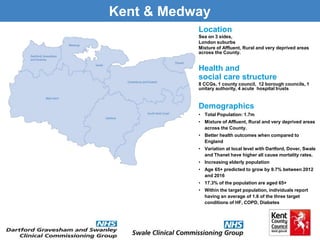
- 3. Kent & Medway Location Sea on 3 sides, London suburbs Mixture of Affluent, Rural and very deprived areas across the County. Health and social care structure 8 CCGs, 1 county council, 12 borough councils, 1 unitary authority, 4 acute hospital trusts Demographics • Total Population: 1.7m • Mixture of Affluent, Rural and very deprived areas across the County. • Better health outcomes when compared to England • Variation at local level with Dartford, Dover, Swale and Thanet have higher all cause mortality rates. • Increasing elderly population • Age 65+ predicted to grow by 9.7% between 2012 and 2016 • 17.3% of the population are aged 65+ • Within the target population, individuals report having an average of 1.6 of the three target conditions of HF, COPD, Diabetes
- 4. Advanced Assistive Technology in Kent 2004 The Kent Telecare Pilot 1100 users of enhanced Telecare Packages 93% felt more independent 93% also felt safer in their own homes Reduction in residential placements 2005 The Kent Telehealth Pilot One of the first in the UK to formally evaluate AAT and the benefits to the Health economy Reduction in A&E Attendances Reduction in unplanned Admissions £1800 average saving per patient over 6 months 2008 -2011 WSD (Telecare & Telehealth) Largest Randomised Control Trial in the World 6000 participants December 11 20% reduction unplanned admissions 15% reduction in A&E attendances 14% reduction in bed days 45% reduction in mortality rates. June 12 Telehealth reduces Hospital Admissions but unlikely to have a significant effect on costs. Feb 13 Telehealth did not improve quality of life Telecare has no significant impact on the use of other NHS or social care services
- 5. • A better quality of care, lower mortality rates and reduced unplanned hospital admissions are possible • Patients on the whole like this type of intervention and age is no barrier • Deploying appropriate technology at the appropriate time to the appropriate patient • Eligibility criteria and critical mass-technology alone does not bring the change – you need service transformation • Clinicians key to implementation and success • Education and training – skilled competent workforce • Need to Identify an appropriate procurement model to realise cost benefits What did we learn?
- 6. • NHS - over 1 million patient contacts every 36 hours • Increase in Long Term Condition – 1:3 people with a Long Term Condition • In England over 15 m people have a long term condition with numbers set to increase in the next 5 to 10 years, especially co-morbidity • People with long term conditions use 72% of inpatient beds, 68% of out-patient appointments and 55% of GP appointments • Treatment and care of those with LTCs account for 70% of the total health and social care spend in England, or almost £7 in every £10 spent • Deliver more for less – increasing demand and financial challenge The Challenge
- 7. I want……. …less time in hospital …independence …empowerment …own bed …prevention of exacerbation …in control …freedom …more time …understand own condition …fewer trips to see specialist
- 8. North Kent Vision “Transformation of the Health & social care system so that it works better for people, with a focus on promoting independence and self care, delivering the right care, right time, right place, providing seamless, integrated care for people, particularly those with complex needs” • Better access • Increased independence • More control • Improved care at home • Live and die safely at home • Shared care plans
- 9. “A single pooled budget for health and social care services to work more closely together in local areas, based on a plan agreed between the NHS and local authorities” 6 National conditions • Plans to be jointly agreed • Protection for social care services (not spending) • 7 day services in health and social care • Better data sharing between health and social care based on the NHS number • Assure joint approach to assessments and care planning, where funding is used for integrated packages of care there will be an accountable professional • Agreement on the consequential impact of changes in the acute sector Better Care Fund (BCF)
- 10. The Integrated Care & Support Pioneer Programme • 14 areas selected to lead on health and social care integration. • Support from the Department of Health and 40 national partners. • Responsibility to “barrier bust”. • Underpinned by the Better Care Fund.
- 11. Integrated Transformation Components Non Acute bed Provision: Consultant and GP support; Integrated Care Centres; Extra Care; Rehab Units; Community Hospital beds; Private Residential and Nursing bed provision Crisis Response Services: Access to Shared Anticipatory Care Plans by the ambulance service, enhanced rapid response ,enablement services and voluntary sector based crisis response services. Integrated Care Home support: Integrated teams including Consultant and GP support; Use of technology to Care Homes / Extra Care Housing providers. Integrated Equipment , DFGs, capital adaptations & assistive technologies at the front end of all the services video conferencing with clinicians and development of new pathways. Improved data sharing Promotion of the NHS umber, better health information, use of the health & social care information centre, patients accessing own health records. GPs linked to hospital data. Operating model: Integrated skill mix, assessors accessing integrated care direct: i.e. nurses accessing social care and case managers nursing care, skills for mental health, dementia/LD a Integrated Primary Care Teams 24/7 access to multi-disciplinary teams coordinated by the GP, inc mental health/dementia; risk stratifying patients; access to one shared care plan for patient and professionals Integrated Access: Integrated Locality Referral Unit; 7 days a week direct access and 24/7 crisis response ; Access to one shared care plan on an integrated platform. Integrated Discharge Teams: Across acute & community; 7 days a week working including Rapid Response; Enablement” Going Home Teams” “I can plan my care with people who work together to understand me and my carer(s), allow me control, and bring together services to achieve the outcomes important to me.”
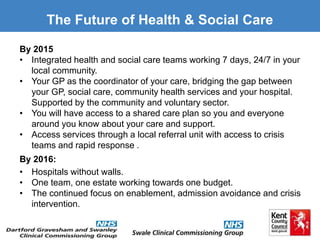
- 12. The Future of Health & Social Care By 2015 • Integrated health and social care teams working 7 days, 24/7 in your local community. • Your GP as the coordinator of your care, bridging the gap between your GP, social care, community health services and your hospital. Supported by the community and voluntary sector. • You will have access to a shared care plan so you and everyone around you know about your care and support. • Access services through a local referral unit with access to crisis teams and rapid response . By 2016: • Hospitals without walls. • One team, one estate working towards one budget. • The continued focus on enablement, admission avoidance and crisis intervention.
- 13. New Model of Delivery Primary Prevention Acute Care IntegratedDischargeTeam IntegratedPrimaryCareTeam Telehealth/ Care/ Medicine Shared care plans Psychological Liaison Discharge Nurses Case Management Discharge Planning Teams Pharmacy Specialist Services – for example Diabetologist & Respiratory Consultant Impact/RR Falls OT/ Physio Specialist Nurses Geriatricians Mental Health Enablement Twilight Ambulance 10K Population GP District Nurses 30K Population Dementia Adult Mental Health Health Visiting Case Management Community Pharmacy Single Point of Access LRU + LRMS
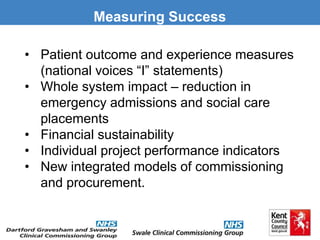
- 14. Measuring Success • Patient outcome and experience measures (national voices “I” statements) • Whole system impact – reduction in emergency admissions and social care placements • Financial sustainability • Individual project performance indicators • New integrated models of commissioning and procurement.
- 15. Any Questions?
Editor's Notes
- Success = someone knowing they don’t have to go to hospital as they can get the care they need at home.