CVD.pptx
- 1. Cardiovascular Disorders PROF DR AMINUDDIN SHEIKH
- 2. Overview • Coronary Artery Disease (CAD) – Arteriosclerosis – Atherosclerosis – Myocardial Infarction (MI) • Cardiac Arrhythmias – Sinus node abnormalities – Atrial conduction abnormalities – Cardiac arrest • Congestive Heart Failure (CHF) • Arterial Diseases – Hypertension • Shock
- 3. Diagnostic Tests for Cardiovascular Function • ECG – Monitors arrhythmias, MI, infection, pericarditis – Studies conduction activation and systemic abnormalities • Ausculation – Studies heart sounds using stethoscope • Exercise stress test – Assess general cardiovascular function – Checks for exercise-induced problems • Chest X-ray Film – Shows shape, size of heart – Evidence of pulmonary congestion associated with heart failure – Nuclear imaging
- 4. Diagnostic Tests • Cardiac Catheterization – Visualize inside of heart, measure pressure, assess valve and heart function – Determine blood flow to and from heart
- 5. Diagnostic Tests • Angiography – Visualization of blood flow in coronary artery – Obstruction assessed and treated • Basic catheterization • Balloon angioplasty
- 6. Diagnostic Tests • Doppler Studies – Assessment of blood flow in peripheral vessels – Microphone records sounds of blood flow • Can detect obstruction • Blood tests – Assess triglyceride and cholesterol levels – Electrolytes – Hb, hematocrit, cbcs • Arterial Blood Gas Determination – Essential for pts with shock, MI – Check current oxygen levels, acid-base balance
- 7. General Treatment Measures for Cardiac Disorders • Dietary modification • Regular exercise program • Quit smoking • Drug therapy
- 8. Drug Therapy • Vasodilators (Nitroglycerin) – Provide better balance of oxygen supply and demand in heart muscle – May cause low bp • Beta-blockers (Metoprolol or Atenolol) – Treats angina, hypertension, arrhythmias – Blocks beta1-adrenergic receptors in heart • Prevent epine from increasing heart activity
- 9. Drug Therapy • Calcium ion channel blockers – Block movement of calcium – Decrease heart contraction • Antiarrhytmatic for excessive atrial activity • Antihypertension and vasodilator • Digoxin – Treats heart failure – Increases efficiency of heart • Decreases conduction of impulses and HR • Increases contraction of heart – Pts must be checked for toxicity • Antihypertensive drugs – Decrease bp to normal levels – Include: • Adrenergic blocking agents • Calcium ion blockers • Diuretics • Angiotensin-converting enzyme (ACE) inhibitors – Used to treat hypertension, CHF, after MI
- 10. Drug Therapy • Adrenergic Blocking drugs – Act on SNS, block arteriole alpha adrenergic receptors, or act directly as vasodilator • ACE Inhibitors – Treat hypertension, CHF • Diuretics – Remove excess water, sodium ions – Block resorption in kidneys – Treat high bp, CHF
- 11. Drug Therapy • Anticoagulant – Decrease risk of blood clot formation – ASA decreases platelet adhesion – Block coagulation process • Cholesterol or lipid reducing drugs – When diet and exercise fail – Decrease LDL and cholesterol
- 12. CAD—Arteriosclerosis: Pathophysiology • General term for all types of arterial changes • Best for degeneration in small arteries and arterioles • Loss of elasticity, walls thick and hard, lumen narrows
- 13. CAD—Atherosclerosis: Pathophysiology • Presence of atheromas – Plaques • Consist of lipids, cells, fibrin, cell debris – Lipids usually transported with lipoproteins
- 15. Atherosclerosis--Pathophysiology • Analysis of serum lipids: – Total cholesterol, triglycerides, LDL, HDL • LDL – High cholesterol content – Transports cholesterol liver cells – Dangerous component • HDL – “good” – Low cholesterol content – Transports cholesterol cells liver
- 18. Atherosclerosis—Etiology • Age • Gender • Genetic factors • Obesity, diet high in cholesterol, animal fats • Cigarette smoking • Sedentary life style • Diabetes mellitus • Poorly controlled hypertension • Combo of BC pills and smoking
- 19. Atherosclerosis—Diagnostic Tests • Serum lipid levels • Exercise stress test • Radioisotope
- 20. Atherosclerosis—Treatment • Decrease cholesterol and LDL • Decrease sodium ion intake • Control primary disorders • Quit smoking • Oral anticoagulant • Surgical intervention – Percutaneous transluminal coronary angioplasty (PTCA) – Cardiac catheterization – Laser beam technology – Coronary artery bypass grafting
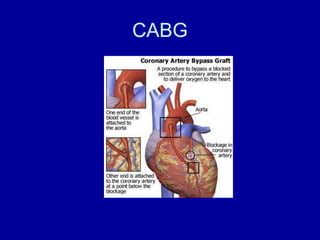
- 21. CABG
- 22. CAD: Myocardial Infarction— Pathophysiology • Coronary artery completely obstructed – Prolonged ischemia and cell death of myocardium • Most common cause is atherosclerosis with thrombus • 3 ways it may develop: – Thrombus obstructs artery – Vasospasm due to partial occlusion – Embolus blocks small branch of coronary artery • Majority involve L ventricle – Size and location of infarction determine severity of damage
- 24. MI—Pathophysiology • Function of myocardium contraction and conduction quickly lost – Oxygen supplies depleted • 1st 20 minutes critical • Time Line – 1st 20 min critical – 48 hrs inflammation begins to subside – 7th day necrosis area replaced by fibrous tissue – 6-8 weeks scar forms
- 26. MI—Signs and Symptoms • Pain – Sudden, substernal area – Radiates to L arm and neck – Less severe in females • Pallor, sweating, nausea, dizziness • Anxiety and fear • Hypotension, rapid and weak pulse (low CO) • Low grade fever
- 27. MI—Diagnostic Tests • ECG • Serum enzyme and isoenzyme test • High serum levels of myosin and troponin • Abnormal electrolytes • Leukocytosis • Arterial blood gases • Pulmonary artery pressure measure – Determines ventricular function
- 28. MI—Complications • Arrhythmias – 25% pts sudden death after MI • Due to ventricular arrhythmias and fibrillation – Heart block – Premature ventricular contraction (PVCs) • Cardiogenic shock • CHF
- 29. MI—Treatment • Rest, oxygen therapy, morphine • Anticoagulant • Drugs • Cardiac rehabilitation • Prognosis depends on site/size of infarct, presence of collateral circulation, time elapsed before treatment • Mortality rate in 1st year – 30-40% due to complications, recurrences
- 30. Cardiac Arrhythmias • Alteration in HR or rhythm • ECG monitors – Holter monitors • decreases efficiency of heart’s pumping cycle – Slight increase in HR increases CO – Very rapid HR prevents adequate filling in diastole – Very slow HR reduces output to tissues • Irregular contraction inefficient – Interferes with normal filling/emptying cycle
- 32. CA: Sinus Node Abnormalities • Brachycardia – Regular but slow HR • Less than 60 beats/min – Results from vagus nerve stimulation or PNS stimulation • Tachycardia – Regular rapid HR • 100-160 beats/min – SNS stimulation, exercise, fever, compensation for low blood volume
- 34. CA: Atrial Conduction Abnormalities • Premature Atrial Contractions (PAC) – Extra contraction or ectopic beats of atria – Irritable atrial muscle cells outside conduction pathway • Interfere with timing of next beat • Atrial flutter – HR 160-350 beats/min – AV node delays conduction • Slower ventricular rate
- 35. Treatment of CA • Cause should be determined and treated • Easiest to treat are those due to meds • SA node problems may require a pacemaker • Some may require defibrillators
- 37. Cardiac Arrest • Cessation of all activity in the heart • No conduction of impulses (flat line) • May occur b/c: – Excessive vagal nerve stimulation (decreases heart) – Drug toxicity – Insufficient oxygen to maintain heart tissue • Blood flow to heart and brain must be maintained to resuscitate
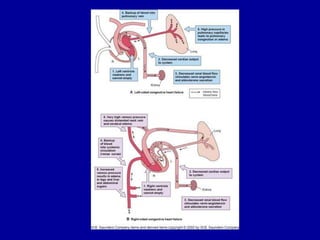
- 38. CHF—Pathophysiology • Heart unable to pump sufficient blood to meet metabolic needs of body • Complication • Acute or chronic • Results from – Problem in heart itself – Increased demands placed on heart – Combo • One side usually fails 1st
- 39. CHF—Pathophysiology • 1st compensation mechanism to maintain CO – Often aggravates instead of assists – Decreased flow to systemic circ • Kidneys increase renin, aldosterone secretion • Vasoconstriction (increase afterload) and increased blood vol (increased preload) = increased work load for heart – SNS increases HF and periph resistance – Dilatation of heart chambers, myocardium, hypertrophies
- 41. CHF—Pathophysiology • 2nd effect when heart cannot maintain pumping capability – Decrease in CO or SV • “forward effect” – “backup” congestion
- 43. CHF—Etiology • Causes of failure on affected side: – Infarction that impairs pumping ability or efficiency of conduction system – Valve defects – Congenital heart defects – Coronary artery disease
- 44. CHF—Etiology • Increased demands on heart cause failure – Depends on ventricle most adversely affected – Ex: Hypertension increases diastolic bp – Requires L ventricle to contract more forcibly to open aortic valve – Ex: Pulmonary disease – Damages lung caps, increases pulm resistance – Increase work load to R vent
- 46. CHF—Signs and Symptoms • Forward effects – Similar with failure on either side – Decrease blood supply to tissue and general hypoxia – Fatigue, weakness, dyspnea (breathlessness), cold intolerance, dizziness • Compensation mechanism – Indicated by tachycardia, pallor, daytime oliguira
- 47. CHF—Signs and Symptoms • Systemic backup effects of R-sided failure – Edema in feet, legs – Hepatomegaly, splenomegaly – Ascites – Acute R-sided failure • Increased pressure on SVC – Flushed face, distended neck veins, headaches, vision problems
- 48. CHF—Diagnostic Tests • Radiographs • Catheterization • Arterial blood gases
- 49. CHF—Treatment • Underlying problem should be treated • Decrease work load on heart • Prophylactic measures • Other methods – Diet – Drugs
- 50. Arterial Diseases: Hypertension— Pathophysiology • Increased bp • Insidious onset, mild symptoms and signs • 3 major categories – Essential (primary) – Secondary – Malignant • Can be classified as diastolic or systolic • Develops when bp consistently over 140/90 • Diastolic more important
- 52. Hypertension—Pathophysiology • Over long time, high bp damages arterial walls – Sclerosis, decreased lumen – Wall may dilate, tear • Aneurysm • Areas most frequently damaged: – Kidneys, brain, retina • End result of poorly controlled hypertension: – Chronic renal failure – Stroke – Loss of vision – CHF
- 53. Hypertension—Etiology • Increases with age • Males more freq and severe • Genetic factors • High sodium ion intake • Excessive alcohol • Obesity • Prolonged, recurrent stress
- 54. Hypertension—Signs and Symptoms • Asymptomatic in early stages • Initial signs vague, nonspecific – Fatigue, malaise, morning headache
- 55. Hypertension—Treatment • Treated in sequence of steps – Life style changes – Mild diuretics, ACE inhibitors – One or more drugs added • Pt compliance is an issue • Prognosis depends on treating underlying problems and maintaining constant control of bp
- 56. Shock (Hypotension) • Results from decreased circulating blood vol – General hypoxia – Low CO
- 57. Classification and Mechanisms of Shock Type Mechanism Hypovolemic loss of blood or plasma Cardiogenic Decreased pumping capability of heart Anaphylactic Systemic vasodilation due to severe allergic reaction Septic Vasodilation due to severe infection Neurogenic Vasodilation due to loss of SNS and vaso-motor tone
- 59. Shock—Pathophysiology • Bp decreases when blood vol, heart contraction, or periph resistance fails • Low CO, microcirculation – = decreased oxygen, nutrients for cells • Compensation mechanism – SNS, adrenal medulla stimulated – Renin secreted – Increased secretion of ADH – Secretion of glucocorticoids – Acidosis stimulates respiration
- 61. Shock—Pathophysiology • Complications of decompensation of shock – Acute renal failure – Adult respiratory distress syndrome (ARDS) – Hepatic failures – Hemorrhagic ulcers – Infection of septicemia – Decreased cardiac function
- 62. Shock—Etiology • Hypovolemic shock – Loss of blood, plasma • Burn pts, dehydration • Cardiogenic shock – Assoc w/ cardiac impairment • Distributive shock – Blood relocated b/c vasodilation • Anaphylactic shock • Neurogenic shock • Septic shock – Severe infection
- 63. Shock—Signs and Symptoms • 1st signs – Shock, thirst, agitation, restlessness – Often missed • 2nd signs – Cool, moist, pale skin; tachycardia; oliguria – Compensation – Vasoconstriction • Direct effects – Decrease bp and blood flow – Acidosis • Prolonged – Decreased responsiveness in body – Compensated metabolic acidosis progresses to decompensated – Acute renal failure – Monitoring
- 64. Shock—Treatment • Primary problem must be treated • Hypovolemic shock – Whole blood, plasma, electrolytes, bicarbonate required • Anaphylactic shock – Antihistamines, corticosteroids • Septic – Antimicrobials, glucocorticoids • Maximize oxygen supply • Epine reinforces heart action and vasoconstriction • Dopamine, dubutamine increase heart function • Good prognosis in early stages • Mortality increases as irreversible shock develops