DES Slideshare
- 1. Network Contract DES 2022/23 A summary of the DES for PCNs April 2022 Year four of a five year contract
- 2. www.pcc-cic.org.uk © 2022 PCC Priorities for 2022/23 ● Maintain stability for general practice ● Bolster investment in workforce and leadership ● Support the recovery of communities ● Ensure patients continue to receive timely, high quality care ● Builds on Investment and Evolution.
- 3. Additional roles reimbursement scheme • ARRS funding increased by £280m • 15 different roles available to support service delivery Workforce plans • 31 Aug 2022- updated plans for 22- 23 • 31 Oct 2022- updated plans 23-24 Points to note • On target to have achieved 21,000 FTE by March 2023 • Number of mental health practitioner (MHP) roles doubled (up to two MHPs where <100,000 patients) • MHP role broadened to include non clinical support to patients • Unclaimed funding- to be identified by 30 Sep 22- if PCN agrees estimate- the PCN will no longer have right to claim • Commissioner may allow other PCNs to bid • Core PCN funding of £1.50 per head maintained
- 4. Funding overview Payments based on list size 1 Jan 2022 list size 1 Jan 2022 • Extended hours access (1 April- 30 Sept) = £0.720 per PCN registered list size • Extended hours access (1 Oct- 31 Mar ‘23) = £3.764 per PCN registered list size • Care Home = £120 per bed per annum • Leadership and Management payment = £0.699 x PCN adjusted population per year • Core PCN funding of £1.50 per registered patient • Network participation payment to practices £1.761 per contractor weighted population
- 5. Enhanced Access 1 April 2022- 30 Sep 22- existing extended hours access continues Combines network DES extended access funding with CCG commissioned extended access services Draft enhanced access plan submitted to commissioners by 31 July 2022 Final version to be agreed by 31 Aug 2022 Service to include: • Bookable appointments outside core hours • 6.30pm-8pm weekday evenings • 9am-5pm Saturdays • These are then ‘network standard hours’ • Offer a range of general practice services in line with patient preference and need • Minimum 60 minutes per 1,000 PCN adjusted patients per week- no stipulation re appointment length £3.764 per PCN adjusted population to cover six months period (Oct 2022 – Mar 2023) Plan to demonstrate: • How PCN has engaged with patients • Services provided • What is the mix of appointments types (face to face and remote) • Proposed staffing / skill mix • Locations (a minimum equivalent to CCG extended access service) NB- How this will be delivered must be set out in the network agreement Service requirements - extended access
- 6. Enhanced Access Medication review and medicines optimisation Enhanced health in care homes (EHCH) PCNs must offer and deliver a volume of structured medication reviews determined and limited by the PCN’s clinical pharmacist capacity The PCN must demonstrate reasonable ongoing efforts to maximise that capacity PCN must • Deliver EHCH in the homes in its PCN area • Ensure a lead GP (or GPs)is agreed for each of the PCN’s aligned homes • Work with community service providers to establish a multi-disciplinary team • Have established protocols for information sharing, shared care planning • Deliver a ‘home round’- reviewing only those according to need not all home residents. • Create personalised care plans Service requirements
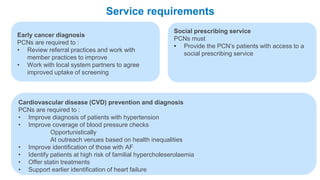
- 7. Enhanced Access Early cancer diagnosis PCNs are required to : • Review referral practices and work with member practices to improve • Work with local system partners to agree improved uptake of screening Social prescribing service PCNs must • Provide the PCN’s patients with access to a social prescribing service Service requirements Cardiovascular disease (CVD) prevention and diagnosis PCNs are required to : • Improve diagnosis of patients with hypertension • Improve coverage of blood pressure checks Opportunistically At outreach venues based on health inequalities • Improve identification of those with AF • Identify patients at high risk of familial hypercholeserolaemia • Offer statin treatments • Support earlier identification of heart failure
- 8. Enhanced Access Tackling neighbourhood inequalities PCNs are required to : • Identify and deliver an annual health check for patients with a learning disability (75% of patients aged 14 and over) • Identify and include all patients with severe mental illness and deliver health checks for 60% of these patients • Record the ethnicity of all patients registered with a PCN unless the patient chooses not to provide their ethnicity • Appoint a lead for tackling health inequalities • Develop a plan to tackle unmet needs of a population Anticipatory care PCNs must • PCNs must contribute to the delivery of ICS plans Service requirements Personalised care PCNs must • By 30 Sept 2022- work to offer and improve access to social prescribing to an identified cohort with unmet need • 1 October- must deliver the plan
- 9. Service requirements • All clinical staff complete e-learning refresher training for shared decision making (SDM) conversations. Investment and Impact Fund (IIF) Three domains • Prevention and tackling health inequalities • Providing high quality care • A sustainable NHS 36 indicators (up from 20 in 21/22) 1,153 points available £200 per point Achievement to be calculated after 31 March 2023
- 10. Useful links Useful Links ● Contract Specification- requirement and entitlements ● DES guidance ● DES ready reckoner ● DES IIF Summary ● DES IIF updated guidance ● Update to the GP Contract financial implications ● QOF Changes ● Weight Management ES ● PCN ECD guidance ● DES Adjusted populations calculator ● DES – Personalised care ● DES FAQ ● CVD Supplementary guidance
- 11. www.pcc-cic.org.uk © 2022 PCC PCC support ● Range of virtual courses being delivered over the coming months. See PCC events calendar for further details ● Visit our website for news, articles and how we can help you www.pcc- cic.org.uk ● Keep up to date with NHS news - sign up to our free weekly newsletters www.pcc-cic.org.uk/newsletters/