Ear,Nose and throat Disorders...
- 1. Ear , Nose , and Throat disorder
- 2. Topics • Review of anatomy and physiology of the Ear Nose and Throat – • Nursing Assessment-History and physical assessment • Etiology, Path physiology, clinical manifestations, diagnosis, treatment modalities and medical & surgical nursing management of Ear Nose and Throat disorder: • External ear: deformities otalgia, foreign bodies, and tumors • Middle Ear- Impacted wax, Tympanic membrane perforation, otitis media , otoselerosis, mastoiditis, tumors • Inner ear-Meniere’s Disease, labyrinthitis, ototoxicity, tumors 2
- 3. • Upper airway infections- Common cold, sinusitis, ethinitis, rhinitis, pharyngitis, tonsilits and adenoiditis, peritonsilar abscess, laryngitis • Upper respiratory airway- epistaxis, • Nasal obstruction, laryngeal obstruction, cancer of the larynx • Cancer of the oral cavity • Speech defects and speech therapy • Deafness- • Prevention, control and rehabilitation • Hearing Aids, implanted hearing devices • Special therapies • Nursing procedures • Drugs used in treatment of disorders of Ear Nose and Throat Role of nurse Communicating with hearing impaired and muteness. 3
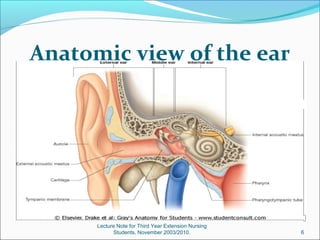
- 4. Anatomic and Physiologic Overview of Ear The ears are a pair of complex sensory organs located in the middle of both sides of the head (that attaches to the temporal bone of cranium) at approximately eye level. 4
- 5. Cont…d 5
- 6. Anatomic view of the ear Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 6
- 7. Anatomy of the external ear The external ear, housed in the temporal bone, includes the auricle (i.e., pinna) and the external auditory canal. The external ear is separated from the middle ear by a disklike structure called the tympanic membrane (i.e., eardrum). Auricle- the auricle, attached to the side of the head by skin, is composed mainly of cartilage, except for the fat and subcutaneous tissue in the earlobe. The function of auricle is to collects the sound waves and directs vibrations into the external auditory canal. 7
- 8. Cont…d 8
- 9. External Auditory Canal The external auditory canal is approximately 2.5 cm long. The lateral third is an elastic cartilaginous and dense fibrous framework to which thin skin is attached. The medial two thirds is bone lined with thin skin that contains hair, sebaceous glands, and ceruminous glands, which secrete a brown, wax like substance called cerumen (i.e., ear wax). The external auditory canal ends at the tympanic membrane. The ear’s self-cleaning mechanism moves old skin cells and cerumen to the outer part of the ear. 9
- 10. Anatomic view of the ear Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 10
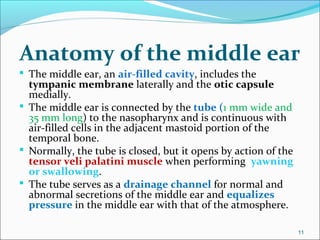
- 11. Anatomy of the middle ear The middle ear, an air-filled cavity, includes the tympanic membrane laterally and the otic capsule medially. The middle ear is connected by the tube (1 mm wide and 35 mm long) to the nasopharynx and is continuous with air-filled cells in the adjacent mastoid portion of the temporal bone. Normally, the tube is closed, but it opens by action of the tensor veli palatini muscle when performing yawning or swallowing. The tube serves as a drainage channel for normal and abnormal secretions of the middle ear and equalizes pressure in the middle ear with that of the atmosphere. 11
- 12. Tympanic Membrane The tympanic membrane (i.e., eardrum), about 1 cm in diameter and very thin, is normally pearly gray and translucent. The tympanic membrane consists of three layers of tissue: an outer layer, continuous with the skin of the ear canal; a fibrous middle layer; and an inner mucosal layer, continuous with the lining of the middle ear cavity. The tympanic membrane protects the middle ear and conducts sound vibrations from the external canal to the ossicles. 12
- 13. Ossicles The middle ear contains the three smallest bones (i.e., ossicles) of the body: - malleus, - incus, and - stapes. It has vibratory, resonance function and modify the external stimulus. The ossicles, which are held in place by joints, muscles, and ligaments, assist in the transmission of sound. 13
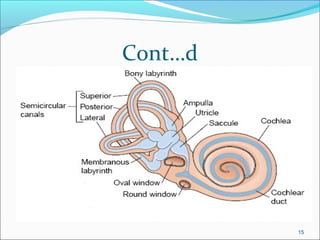
- 14. Anatomy of the inner ear The inner ear is housed deep within the temporal bone. The organs for hearing (i.e., cochlea) and balance (i.e., semicircular canals), as well as cranial nerves VII (i.e., facial nerve) and VIII (i.e., vestibulocochlear nerve), are all part of this complex anatomy. The cochlea and semicircular canals are housed in the bony labyrinth. The bony labyrinth surrounds and protects the membranous labyrinth, which is bathed in a fluid called perilymph. 14
- 15. Cont…d 15
- 16. Membranous Labyrinth The membranous labyrinth is composed of the utricle, the saccule, the cochlear duct, the semicircular canals, and the organ of Corti. The membranous labyrinth contains a fluid called endolymph. The three semicircular canals—posterior, superior, and lateral, which lie at 90-degree angles to one another—contain sensory receptor organs, arranged to detect rotational movement. These receptor end organs are stimulated by changes in the rate or direction of an individual’s movement. 16
- 17. Organ of Corti The organ of Corti is located in the cochlea, a snail- shaped, bony tube about 3.5 cm long with two and one-half spiral turns. The organ of Corti, also called the end organ for hearing, transforms mechanical energy into neural activity and separates sounds into different frequencies. 17
- 18. Function of the ears Hearing:- Hearing is conducted over two pathways: air and bone. Sounds transmitted by air conduction travel over the air- filled external and middle ear through vibration of the tympanic membrane and ossicles. Sounds transmitted by bone conduction travel directly through bone to the inner ear, bypassing the tympanic membrane and ossicles. Normally, air conduction is the more efficient pathway. (AC>BC) 18
- 19. Cont…d Sound conduction and transmission Sound enters the ear through the external auditory canal causes the tympanic membrane to vibrate. These vibrations transmit sound through the action of the ossicles to the oval window as mechanical energy. This mechanical energy is then transmitted through the inner ear fluids to the cochlea, stimulating the hair cells, and is subsequently converted to electrical energy. The electrical energy travels through the vestibulocochlear nerve to the central nervous system, where it is analyzed and interpreted in its final form as sound. 19
- 20. Assessment HEALTH HISTORY:- It includes all the components that are applied in other body system. Date of History. Identification. Chief compliant. History of present illness. History of past illness. Current health status (Current medication, addictive drugs and allergies). Family history. Psychosocial and personal history. 20
- 21. Physical Examination The external ear is examined by; Inspection of external ear :- for the presence of scar, lesion, symmetry, attachment, any abnormal discharge, color e.t.c. Tympanic membrane is inspected with an otoscope. Inspection of the middle ear with middle ear endoscopy. Direct palpation:- for tenderness, presence of malignancy, free movement, circulation, e.t.c. 21
- 22. Otoscopic examination To examine the external auditory canal and tympanic membrane, the otoscope should be held in the examiner’s right hand, in a pencil- hold position, with the bottom of the scope pointing up. Before inserting the otoscope it is important to straighten the external auditory canal by manipulation; Grasp the auricle firmly but gently and pull it upward, backward, and slightly away from the head in adult. Grasp the auricle firmly but gently and pull it down ward, backward, and slightly away from the head in Children. Proper otoscopic examination of the external auditory canal and tympanic membrane requires that the canal be free of large amounts of cerumen. The healthy tympanic membrane is pearly gray and is positioned obliquely at the base of the canal. 22
- 23. Cont…d Steady the hand against the patient’s head to avoid inserting the otoscope too far into the external canal. 23
- 24. Evaluation of gross auditory acuity A general estimation of hearing can be made by assessing the patient’s by; whisper test. Weber . Rinne tests 24
- 25. Whisper Test To exclude one ear from the testing, the examiner covers the untested ear with the palm of the hand. Then the examiner whispers softly from a distance of 1 or 2 feet from the unoccluded ear and out of the patient’s sight. The patient with normal acuity can correctly repeat what was whispered. 25
- 26. Weber Test (Lateralization Test) The Weber test uses bone conduction to test lateralization of sound. A tuning fork (ideally, 512 Hz), set in motion by grasping it firmly by its stem and tapping it on the examiner’s knee or hand, is placed on the patient’s head or forehead. A person with normal hearing will hear the sound equally in both ears or describe the sound as centered in the middle of the head. In cases of conductive hearing loss, such as from otosclerosis or otitis media, the sound is heard better in the affected ear. 26
- 27. Cont…d In cases of sensorineural hearing loss, resulting from damage to the cochlear or vestibulocochlear nerve, the sound lateralizes to the better-hearing ear. The Weber test is useful for detecting unilateral hearing loss. 27
- 28. Rinne Test In the Rinne test (pronounced rin-ay), the examiner shifts the stem of a vibrating tuning fork between two positions: 2 inches from the opening of the ear canal (i.e., for air conduction) and against the mastoid bone (i.e., for bone conduction). Normally, sound heard by air conduction is audible longer than sound heard by bone conduction. The Rinne test is useful for distinguishing between conductive and sensorineural hearing losses. With a conductive hearing loss, bone-conducted sound is heard as long as or longer than air-conducted sound, whereas with a sensorineural hearing loss, air-conducted sound is audible longer than bone conducted sound. 28
- 29. Cont…d 29
- 30. Cont…d Comparison of Weber and Rinne Tests 30
- 31. Diagnostic Evaluation 1. Audiometry { test to check the ability of hear sounds,} 2. Tympanogram {tympanometery is an examination used to test the condition of the middle ear and tympanic membrane} 3. Auditory brain stem response {ABR- is an extracted from ongoing electrical activity in the brain and recorded via electrodes placed on the scalp.} 4. Electronystagmography{ ENG- used to evaluate patients with dizziness, vertigo, or balance dysfunction or to record involuntary movements of the eyes caused by a condition known as nystagmus.} 5. Platform posturography{ TOB- TEST OF BLANCE} 6. Sinusoidal harmonic acceleration{ TO CHECK THE VESTBULAR FUNCTION} 7. Middle ear endoscopy 31
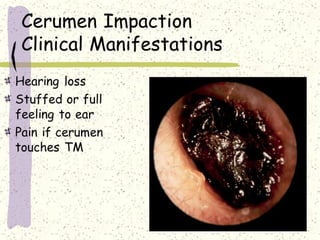
- 32. External Ear disorder 1. CERUMEN IMPACTION Cerumen normally accumulates in the external canal in various amounts and colors. Although wax does not usually need to be removed, impaction occasionally occurs, causing otalgia, a sensation of fullness or pain in the ear, with or without a hearing loss. Accumulation of cerumen is especially significant in the geriatric population as a cause of hearing deficit. 32
- 33. Accumulated cerumen (earwax) may become impacted due to use of cotton swabs to clean ears and may be a problem for some people. Cerumen becomes drier in elderly people, making impaction more likely. Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 33
- 34. Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 34
- 35. Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 35
- 36. Management o Cerumen can be removed by o Irrigation: (Unless the patient has a perforated eardrum or an inflamed external ear (i.e., otitis externa), particularly if it is not tightly packed in the external auditory canal). o Suction: Using any softening solution two or three times a day for several days is generally sufficient. Instilling a few drops of warmed glycerin, mineral oil, or half strength hydrogen peroxide into the ear canal for 30 minutes can soften cerumen before its removal. 36
- 37. Cont…d o Instrumentation. If the cerumen cannot be dislodge by these methods, instruments, such as a cerumen curette, aural suction, and a binocular microscope for magnification, can be used. Direct visual, mechanical removal can be performed on a cooperative patient by a trained health care provider.) o To prevent injury, the lowest effective pressure should be used. o Ceruminolytic agents, such as peroxide in glyceryl (Debrox), are available; however, these compounds may cause an allergic dermatitis reaction. 37
- 38. Foreign bodies Some objects are inserted intentionally into the ear by adults who may have been trying to clean the external canal or relieve itching or by children who introduce the objects. Other objects, such as insects, peas, beans, pebbles (Sand/stone), toys, and beads/droplet, may enter or be introduced into the ear canal. In either case, the effects may range from no symptoms to profound pain and decreased hearing. C/M –No symptoms, - Swelling, - Profound pain, - Decreased hearing, 38
- 39. Cont..d Management The three standard methods for removing foreign bodies are the same as those for removing cerumen: Irrigation: Foreign vegetable bodies and insects tend to swell; thus, irrigation is contraindicated., Suction, and Instrumentation. Usually, an insect can be dislodged by instilling mineral oil, which will kill the insect and allow it to be removed. In difficult cases, the foreign body may have to be extracted in the operating room with the patient under general anesthesia. 39
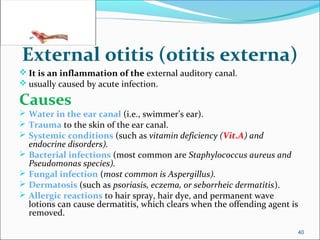
- 40. External otitis (otitis externa) It is an inflammation of the external auditory canal. usually caused by acute infection. Causes Water in the ear canal (i.e., swimmer’s ear). Trauma to the skin of the ear canal. Systemic conditions (such as vitamin deficiency (Vit.A) and endocrine disorders). Bacterial infections (most common are Staphylococcus aureus and Pseudomonas species). Fungal infection (most common is Aspergillus). Dermatosis (such as psoriasis, eczema, or seborrheic dermatitis). Allergic reactions to hair spray, hair dye, and permanent wave lotions can cause dermatitis, which clears when the offending agent is removed. 40
- 41. Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 41
- 42. Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 42
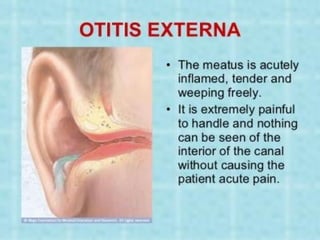
- 43. Cont…d Clinical Manifestations Pain, Discharge (yellow or green and foul smelling), Aural tenderness (usually not present in middle ear infections), Fever, Cellulitis, Lymphadenopathy, Pruritus, hearing loss, Feeling of fullness, Erythematous and edematous (otoscopic examination), In fungal infections, the hair like black spores may even be visible. 43
- 44. Cont…d Medical Management The principles of therapy are aimed at; relieving the discomfort, reducing the swelling of the ear canal, and eradicating the infection. Patients may require analgesics for the first 48 to 92 hours. Antibiotic ear drops Antifungal- clotrimazole ear drop 1% 2-3 times/d at least for 14 days. Avoid swimming & do not allow water to enter the ear. 44
- 45. Cont…d Nursing Management Nurses need to teach patients; not to clean the external auditory canal with cotton-tipped applicators, to avoid swimming, and not to allow water to enter the ear when shampooing or showering. A cotton ball can be covered in a water-insoluble gel such as petroleum jelly and placed in the ear as a barrier to water contamination. Infection can be prevented by using antiseptic otic preparations after swimming (eg, Swim Ear, Ear Dry). 45
- 46. Middle Ear disoder 1. Tympanic membrane perforation Causes Infection. Trauma (skull fracture, explosive injury, or a severe blow to the ear). Foreign objects (eg, cotton-tipped applicators, match pins, keys) that have been pushed too far into the external auditory canal. 46
- 47. Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 47
- 48. Cont…d Medical Management Most tympanic membrane perforations heal spontaneously within weeks after rupture. In the case of a head injury or temporal bone fracture, a patient is observed for evidence of cerebrospinal fluid leakage, otorrhea or rhinorrhea (a clear, watery drainage from the ear or nose), respectively. While healing, the ear must be protected from water. 48
- 49. Cont…d Surgical management Tympanoplasty (i.e., surgical repair of the tympanic membrane). Surgery is usually successful in closing the perforation permanently and improving hearing. 49
- 50. 2. Acute otitis media It is an acute infection of the middle ear, usually lasting less than 6 weeks. Acute otitis media is an inflammation and infection of the middle ear caused by the entrance of pathogenic organisms, with rapid onset of signs and symptoms. It is a major problem in children but may occur at any age. Causes Primarily Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Inflammation of surrounding structures (eg, sinusitis, adenoid hypertrophy). Allergic reactions (eg, allergic rhinitis). It is usually present in the middle ear, resulting in a conductive hearing loss. 50
- 51. Cont…d Clinical Manifestations Otalgia : ear pain (unilateral in adults) may awaken patient at night. Pain relieved after tympanic perforation. drainage from the ear (purulent exudate). Fever, headache Hearing loss (conductive hearing loss). The patient reports no pain with movement of the auricle. The tympanic membrane is erythematous and often bulging. 51
- 52. Diagnostic Evaluation Pneumatic otoscopy shows a tympanic membrane that is full, bulging, and opaque with impaired mobility (or retracted with impaired mobility). Cultures of discharge through ruptured tympanic membrane may suggest causative organism Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 52
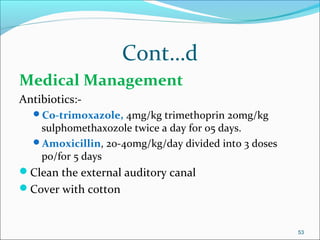
- 53. Cont…d Medical Management Antibiotics:- Co-trimoxazole, 4mg/kg trimethoprin 20mg/kg sulphomethaxozole twice a day for 05 days. Amoxicillin, 20-40mg/kg/day divided into 3 doses po/for 5 days Clean the external auditory canal Cover with cotton 53
- 54. Cont…d Surgical management An incision in the tympanic membrane is known as myringotomy or tympanotomy. The incision heals within 24 to 72 hours. Indication; For analysis of drainage (by culture and sensitivity testing). If pain persists. If episodes of acute otitis media recur and there is no contraindication, a ventilating, or pressure-equalizing tube may be inserted. The ventilating tube, which temporarily takes the place of the eustachian tube in equalizing pressure, is retained for 6 to 18 months. Ventilating tubes are more commonly used to treat recurrent episodes of acute otitis media in children than in adults. 54
- 55. Cont…d Complications Chronic OM Mastoiditis Meniningitis Brain abscess 55
- 56. Cont…d Comparison between AOE and AOM 56
- 57. 3. Serous otitis media Serous otitis media (i.e., middle ear effusion) implies fluid, without evidence of active infection, in the middle ear. Causes Children:- eustachian tube obstruction (negative pressure in the middle ear) Adults:- eustachian tube dysfunction (concurrent upper respiratory infection or allergy) -Radiation therapy. -Barotrauma(results from sudden pressure changes in the middle ear caused by changes in barometric pressure, as in scuba diving or airplane descent. - Carcinoma (eg, nasopharyngeal cancer). 57
- 58. Cont…d Clinical Manifestations Hearing loss (conductive hearing loss), Fullness in ear, Sensation of congestion, Popping and crackling noises, Dull tympanic membrane Diagnosis • Otoscope-dull TM, and air bubble shown in the middle ear. • Audiogram- to exclude conductive hearing loss. 58
- 59. Cont…d Management Myringotomy.( To relieve pressure or or drain fluid by incision) Tube may be placed to keep the middle ear ventilated. Corticosteroids. Valsalva maneuver (do cautiously). 59
- 60. 4. Chronic otitis media Chronic otitis media is the result of repeated episodes of acute otitis media causing irreversible tissue pathology and persistent perforation of the tympanic membrane. Chronic infections of the middle ear damage the tympanic membrane, destroy the ossicles, and involve the mastoid. The most common organisms are group A beta-hemolytic streptococci, S. pneumoniae, and H. influenzae. Other organisms may be present, such as Pseudomonas, Proteus, and Bacteroides species. 60
- 61. Cont…d Clinical Manifestations Presence of a persistent or intermittent, foul-smelling otorrhea . Pain is not usually experienced, except in cases of acute mastoiditis. Otoscopic exam; Perforated tympanic membrane. Cholesteatoma (an ingrowth of the skin of the external layer of the eardrum into the middle ear). Audiometric tests often show a conductive or mixed hearing loss. 61
- 62. Diagnostic Evaluation Air conductive hearing loss is present through audiometric tests. X-rays may show mastoid pathology, for example, cholesteatoma or haziness of mastoid cells. Culture of exudate from middle ear (through ruptured tympanic membrane or at time of surgery). Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 62
- 63. Cont…d Medical Management Suctioning of the ear. Instillation of antibiotic drops or application of antibiotic powder. Systemic antibiotics are usually not prescribed except in cases of acute infection. Dry the ear by wicking. 63
- 64. Cont…d Surgical management Tympanoplasty (most common surgical procedure). There are five types of tympanoplasties. Type I (myringoplasty)-closing the perforated TM, and it is the simplest. Types II through V-more extensive. Ossiculoplasty (surgical reconstruction of the middle ear bones-ossicles). Mastoidectomy (The objectives of mastoid surgery are to remove the cholesteatoma, gain access to diseased structures, and create a dry and healthy ear). 64
- 65. Cont…d Complications facial nerve palsy. Chronic mastoiditis. Meningitis. Brain abscess. 65
- 66. Inner Ear disorder Common compliant that individual with IED are; Dizziness (any altered sensation of orientation in space). Vertigo (the misperception or illusion of motion of the person or the surroundings). Most people with vertigo describe a spinning sensation or say they feel as though objects are moving around them. Ataxia (failure of muscular coordination due to vestibular system). Nystagmus (an involuntary rhythmic movement of the eyes). can be horizontal, vertical, or rotary. 66
- 67. 1. Motion sickness Motion sickness is a disturbance of equilibrium caused by constant motion (aboard a ship, while riding on a merry-go-round or swing, or in the back seat of a car) that over stimulate the vestibular system. Clinical Manifestations Sweating, Pallor, vertigo, Nausea, and Vomiting. These manifestations may persist for several hours after the stimulation stops. 67
- 68. Cont…d Management Over-the-counter antihistamines. dimenhydrinate (Dramamine) or meclizine hydrochloride (Bonine), Anticholinergic medications (scopolamine patch, promethazine, e.t.c.). Avoide potentially hazardous activities (operating heavy machinery, driving a car). 68
- 69. 2. Ménière’s disease Ménière’s disease is an abnormal inner ear fluid balance caused by a malabsorption in the endolymphatic sac. Ménière's disease (endolymphatic hydrops) is a chronic disease that involves the inner ear and causes a triad of symptoms—vertigo, hearing loss, and tinnitus. Ménière’s disease appears to be equally common in both genders. 69
- 70. Clinical Manifestations Sudden attacks occur, in which patient feels that the room is spinning (vertigo); may last 10 minutes to several hours. Dizziness, tinnitus, and reduced hearing occur on involved side. Headache, nausea, vomiting, and incoordination are present. Sudden motion of the head may precipitate vomiting. Irritability; other personality changes. After multiple attacks, tinnitus and impaired hearing may be continuous Lecture Note for Third Year Extension Nursing Students, November 2003/2010. 70
- 71. Cont…d Assessment and Diagnostic Findings Hx. P/E. Audiogram. Electronystagmogram. 71
- 72. Cont…d Pharmacologic therapy Antihistamines (meclizine (Antivert)). Tranquilizers (diazepam (Valium)). Antiemetics (promethazine (Phenergan)) suppositories. Diuretic therapy (eg, hydrochlorothiazide). Vasodilators (nicotinic acid, papaverine hydrochloride (Pavabid), and methantheline bromide (Banthine)). 72
- 73. Cont…d Surgical management Destructive surgery: Labyrinthectomy : recommended if the patient experiences progressive hearing loss and severe vertigo attacks so normal tasks cannot be performed; results in total deafness of affected ear. 73
- 74. 3. Labyrinthitis Labyrinthitis is an inflammation of the inner ear vestibular labyrinth system. It may be due to a viral or bacterial infection. Labyrinthitis, an inflammation of the inner ear. Causes Bacterial (complication of otitis media). Viral in origin (mumps, rubella, rubeola, and influenza) Viral illnesses of the upper respiratory tract. Herpetiform disorders of the facial and acoustic nerves (i.e., Ramsay Hunt syndrome). 74
- 75. Cont…d Clinical Manifestations sudden onset of incapacitating vertigo, Nausea, vomiting, various degrees of hearing loss, and tinnitus. 75
- 76. Cont…d Management Intravenous antibiotic therapy, Fluid replacement, Vestibular suppressant (meclizine) Antiemetic medications. Symptomatic for the viral one. 76
- 77. Anatomic and Physiologic overview of Nose Nose surface anatomy 77
- 78. Cont…d 78
- 79. Cont…d 79
- 80. Disorder of Nose 1. Epistaxis It is hemorrhage from the nose. It can be; A. Anterior Bleed Kiesselbach’s plexus vessels. Easy to locate and treatment. B. Posterior Bleed Larger vessels. Severe bleeding. Harder to locate and treatment. 80
- 81. Cont…d Etiology Dry cracked mucosal membrane Trauma Picking Blunt contact Forceful nose blowing sneezing HTN Chronic infection (AFI) Substance abuse Arteriosclerosis Liver disease Chronic bleeding disorder Leukemia Hemophilia Anticoagulant Rx 81
- 82. Cont…d Management Anterior Simple first aid Apply pressure for 5-10 minutes. Apply ice packs to nose & forehead. Sitting position leaning forward. Discourage swallowing blood. Medications Topical vasoconstrictors Cocaine Neo-Synephrine Adrenaline Nasal spray or on cotton swab held against bleeding site 82
- 83. Cont…d Sitting position leaning forward. 83
- 84. Cont…d Chemical cauterization Silver nitrate Gelfoam Topical anesthetic (pre-packing) Tetracaine Lidocaine Cocaine Nasal Packing -Anterior Petroleum gauze. 24-72 hours commonly. 84
- 85. Cont…d Nasal Packing -Posterior Pack both anterior & posterior for 2-5 days. Monitor for hypoxemia. Administer oxygen as ordered. Frequent oral hygiene. Administer narcotic analgesics as ordered. Monitor for complications. Toxic shock syndrome Otitis media Sinusitis 85
- 86. Cont…d Endoscopic Surgery Cauterizing bleeding vessel. Ligation of internal maxillary artery. 86
- 87. 2. Nasal Polyps It is a benign grapelike growth of mucous membrane. Form in areas of dependent mucous membrane. Usually bilateral. Stem-like base makes them moveable. It may enlarge and cause nasal obstruction. 87
- 88. Cont…d Management Medication; Topical corticosteroid nasal spray. Low-dose oral corticosteroids. Surgery; Polypectomy under local anesthesia. Nasal packing to control bleeding Avoid blowing nose 24-48 hours post removal of packing. Avoid straining at stool, vigorous coughing, strenuous exercise. Monitor for bleeding Frequent swallowing Visible blood at back of throat Laser surgery to remove polyps. May require multiple surgeries as polyps tend to recur. 88
- 89. 3. Deviated Septum May result from trauma May be present from birth Causes nasal obstruction Management Relief of airway obstruction. Repair visible deformity. Reshaping of nose by manipulation of septal cartilage by; Moving Rearranging Augmenting 89
- 90. Cont…d Surgery; Septoplasty or submucous resection. Rhinoplasty or surgical reconstruction of the nose. Post operatively; Bilateral Nasal packing for 72 hours. Temporary plastic splint for 3-5 days. Swelling subsides within 10-14 days. Normal sensation returns within several months. 90
- 91. 4. Rhinitis It is an inflammation of the mucous membranes of the nose. It has different classification; Based on duration, a) Acute b) Chronic Based on cause, a) Allergic rhinitis /hay fever /:due to allergy. b) Non-allergic rhinitis: following URTI (Bacteria and Viral). 91
- 92. 4.1. Acute Rhinitis (Coryza)or common cold Affects almost every one at some time and most often in the winter, with additional high incidence in early fall and spring. Cause Common etiology is virus. Rhinovirus Corona virus Adenovirus Influenza virus Parainfluenza virus Echovirus Coxsakiervirus Respiratory syncytial virus (RSV), Each virus may have multiple strains. For example, there are over 100 strains of rhinovirus, which accounts for 50% of all colds. 92
- 93. Cont…d It is highly contagious because virus is shed for about 2 days before the symptoms appear and after 3 days of the symptom. Common cold spread by; Droplet nuclei from sneezing. Contaminated hand or fomites. Secondary invasion by bacteria may cause; Pneumonia Acute bronchitis Sinusitis Otitis media 93
- 94. Cont…d Clinical manifestation Sneezing Nasal discharge (runny nose) Nasal obstruction Head ache Nasal congestion Chilliness Nasal itchiness Fever Shyness/nervousness Sore throat Malaise 94
- 95. Cont…d Medical management Usually self –limiting and lasts for about 1 week. Goal of management; 1. To relieve symptoms 2. Inhibit spread of the infection 3. Reduce risk of bacterial complication 95
- 96. Cont…d Adequate fluid intake. Encouraging rest. Preventing chilling. Increasing intake of vitamin C. Using expectorants as needed. Warm salt-water gargles soothe the sore throat. Nonsteroidal anti-inflammatory agents (NSAIDs) such as aspirin or ibuprofen. Antihistamines (chlorpheniramine maleate , diphenhydramine (Benadryl) Topical (nasal) decongestant ( e.g. oxymetazoline maleate (Afrin), phenylephrine (Neo-synephrine), pseudoephedrine (Sudafed) orally. Zinc lozenges may reduce the duration of cold symptoms if taken within the first 24 hours of onset. Amantadine (Symmetrel) or rimantadine (Flumadine) may be prescribed prophylactically. Antimicrobial agents (antibiotics) should not be used because they do not affect the virus or reduce the incidence of bacterial complications. 96
- 97. Cont..d Nursing Management; Perform hand hygiene often. Use disposable tissues. Avoid crowds during the flu season. Avoid individuals with colds or respiratory infections. Obtain influenza vaccination, if recommended (especially if elderly or diagnosed with a chronic illness) 97
- 98. 4.2. Chronic rhinitis A chronic inflammation of the nasal mucosal membrane characterized by increased nasal mucus. Cause Repeated acute infection or allergy. Vasomotor rhinitis (an instability of the autonomic nervous system caused by stress, tension , or some endocrine disorder). Chronic irritation by nasal drug 98
- 99. Cont…d Clinical manifestation no acute symptom. nasal obstruction (stuffiness). pressure in the nose. Polyp formation . Vertigo. 99
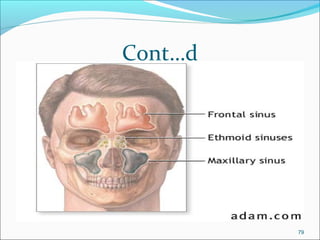
- 101. 5. Sinusitis It is an inflammation of the mucous membranes in the sinuses. Sinusitis can be; 1. Acute bacterial. 2.Sub acute. 3.Chronic. 101
- 102. 5.1. Acute Sinusitis The most common types of acute sinusitis are; Allergic. Usually seasonal. Viral. Acute bacterial (Streptococcus pneumonia, haemophilus influenza, beta hemolytic streptococcus, klebsiella pneumonia and various anaerobic organisms). 102
- 104. Cont…d In acute frontal and maxillary sinusitis, pain usually does not appear until 1 to 2 hours after awakening. It increases for 3 to 4 hours and then becomes less severe in the afternoon and evening usually this is due to increased drainage as result of gravity from standing during the day. Bloody or blood –tinged discharge from the nose in the first 24 to 48 hours. The discharge rapidly becomes thick, green, and copious, blocking the nose. 104
- 105. Cont…d Diagnosis Hx. P/E; Tenderness in the involved sinus, Hyperemic and edematous nasal mucosa, and The turbinate's are enlarged. X-ray examination Clouded sinus and fluid level is visible. 105
- 106. Cont…d Managements Aim is to relief a pain and shrinkage of the nasal mucosa. Medication Analgesics i.e. . Ibuprofen. Oral decongestant pseudoephedrine. Antibiotics i.e., Amoxicillin for 10 days to 14 days . Failure of the infection to respond to amoxicillin is an indication for aspiration of the maxillary sinus to take specimen for culture and sensitivity and to remove the accumulated secretion. Acute frontal sinusitis with pain, tenderness, and edema of the frontal or sphenoid sinus require hospitalization b/c of risk of intracranial complication or Osteomyelitis . High doses of IV antibiotic nasal decongestant or by spray is needed. 106
- 107. 5.2. Chronic Bacterial Sinusitis Chronic bacterial sinusitis develops when irreversible mucosa damage occurs. Damage car result from recurrent attacks of acute sinusitis or from suppurative sinusitis either being untreated or inadequately treated during the acute or sub acute phase. Etiology S.aureus H. influenza Anaerobes (Klebsiella) 107
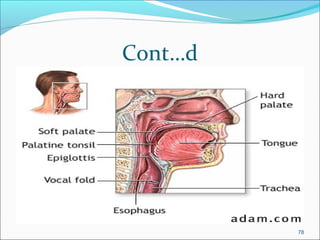
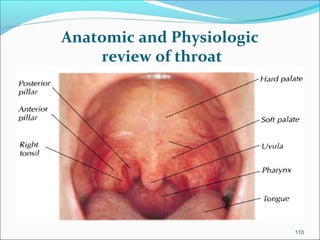
- 110. Anatomic and Physiologic review of throat 110
- 111. 1. Pharangitis 1.1. Acute pharyngitis Acute pharangitis is a febrile inflammation of the throat that is caused by 70% viral cause and 30% bacteria i.e. hemolytic streptococci, staphylococci. It is the most common throat inflammation. A severe form of acute pharangitis often is termed “Step throat” because of the frequency of streptococci as the causative organism. 111
- 112. Cont…d Clinical manifestation Dryness of the throat Fiery read throat and pharyngeal membrane and tonsils Sever pain which lead to difficulty in swallowing Enlarged and tender cervical lymph nodes Fever Malaise Sore throat Hoarseness cough Rhinitis 112
- 113. Cont…d Complication Sinusitis Otitis media Peritonsilar abscess Mastoiditis Cervical adenitis Rheumatic fever Rheumatic nephritis 113
- 117. 1.2. Chronic pharyngitis It is a persistent inflammation of the pharynx. It is common in adults who work or live in dusty surroundings, use their voice to excess, suffer from chronic cough, an habitually use alcohol and tobacco. Three types of chronic pharyngitis are recognized: • Hypertrophic:-general thickening and congestion of the pharyngeal mucous membrane • Atrophic: probably a late stage of the first type (the membrane is thin, whitish, glistening, and at times wrinkled) • Chronic granular (“clergyman’s sore throat”): characterized by numerous swollen lymph follicles on the pharyngeal wall. 117
- 118. Cont…d Clinical Manifestations; -a constant sense of irritation or fullness in the throat, - mucus that collects in the throat and can be expelled by coughing, and - difficulty swallowing. Medical Management; is based on -relieving symptoms, - avoiding exposure to irritants, and - correcting any upper respiratory, pulmonary, or cardiac condition that might be responsible for a chronic cough. Nasal sprays or medications containing ephedrine sulfate (Kondon’s Nasal) or phenylephrine hydrochloride (Neo-Synephrine). Antihistamine decongestant medications, such as Drixoral or Dimetapp, is taken orally every 4 to 6 hours. Anti-inflammatory and analgesic agent like Aspirin or acetaminophen. 118
- 119. Cont…d Nursing Management; avoid contact with others until the fever subsides. Alcohol, tobacco, second-hand smoke, and exposure to cold are avoided. The patient may minimize exposure to pollutants by wearing a disposable facemask. drink plenty of fluids. Gargling with warm saline solutions Lozenges will keep the throat moistened. 119
- 123. Cont…d Diagnosis Hx. P/E. Culture of tonsil swab. Audiometric examination (hearing loss). 123
- 124. Cont…d Treatment Benzantine penicillin Tonsillectomy Adenoidectomy Indication Repeated bout of tonsillitis. Respiratory obstruction. Hypertrophy of the tonsils and adenoids. Recurrent otitis media. Peritonsilar abscess. Mouth care may for comfort 124
- 126. 3. Laryngitis It is inflammation of the larynx. Predisposing factor /associated to; Voice abuse. Exposure to dust. Chemicals. Smoke and other pollutants. 126
- 127. Cont…d Etiology Almost alloys is a virus bacterial invasion may be Acute rhinitis or Naso pharyngitis. The onset of infection may be associated with exposure to sudden temperature change. Diet as deficiencies Lack of immunity Laryngitis is common in the winter and is easily transmitted. 127
- 131. “Teaching is an intimate contact b/n a more mature personality and less mature one which is designed to further the education of the latter.” (H.C.Morrison) 131
Editor's Notes
- Barotrauma(results from sudden pressure changes in the middle ear caused by changes in barometric pressure, as in scuba diving or airplane descent.
- Regardless of the cause, endolymphatic hydrops, a dilation in the endolymphatic space, develops. Either increased pressure in the system or rupture of the inner ear membranes occurs, producing symptoms of Ménière’s disease.
- The first episode is usually the worst; subsequent attacks, which usually occur over a period of several weeks to months, are less severe.
- Kiesselbach plexus vessels
- Allergic rhinitis /hay fever /
- Echovirus Coxsakiervirus
- Sore throat
- Frequent head cold